Abstract
OBJECTIVE
NEUROG3 plays a central role in the development of both pancreatic islets and enteroendocrine cells. Homozygous hypomorphic missense mutations in NEUROG3 have been recently associated with a rare form of congenital malabsorptive diarrhea secondary to enteroendocrine cell dysgenesis. Interestingly, the patients did not develop neonatal diabetes but childhood-onset diabetes. We hypothesized that null mutations in NEUROG3 might be responsible for the disease in a patient with permanent neonatal diabetes and severe congenital malabsorptive diarrhea.
RESEARCH DESIGN AND METHODS
The single coding exon of NEUROG3 was amplified and sequenced from genomic DNA. The mutant protein isoforms were functionally characterized by measuring their ability to bind to an E-box element in the NEUROD1 promoter in vitro and to induce ectopic endocrine cell formation and cell delamination after in ovo chicken endoderm electroporation.
RESULTS
Two different heterozygous point mutations in NEUROG3 were identified in the proband [c.82G>T (p.E28X) and c.404T>C (p.L135P)], each being inherited from an unaffected parent. Both in vitro and in vivo functional studies indicated that the mutant isoforms are biologically inactive. In keeping with this, no enteroendocrine cells were detected in intestinal biopsy samples from the patient.
CONCLUSIONS
Severe deficiency of neurogenin 3 causes a rare novel subtype of permanent neonatal diabetes. This finding confirms the essential role of NEUROG3 in islet development and function in humans.
Permanent neonatal diabetes (PNDM), defined as diabetes diagnosed within the first 6 months of life, is a rare condition with an estimated incidence of 1 in 260,000 live births (1). PNDM encompasses a number of different monogenic disorders (2,3). Despite recent advances in the understanding of the molecular basis of PNDM, the genetic cause remains to be identified in approximately 40% of patients (4).
Pancreas development is coordinated by a complex interplay of signaling pathways and transcription factors that determine early pancreatic specification as well as the latter differentiation of exocrine and endocrine lineages (5,6). Developmental abnormalities ranging from pancreas agenesis and hypoplasia to selective endocrine hypoplasia have been involved in a minority of cases of PNDM, including homozygous or compound heterozygous mutations in six genes: IPF1 (6), PTF1A (7), GLIS3 (8), PAX6 (9), RFX6 (10), and NEUROD1 (11). Genes encoding other pancreatic transcription factors are thus obvious candidates for PNDM of unknown etiology.
The basic helix-loop-helix (bHLH) transcription factor NEUROG3 plays a central role in the early specification of the endocrine pancreas. Neurog3-null mice fail to generate any pancreatic endocrine cells and die of diabetes within a few days after birth (12). In addition, NEUROG3 controls the developmental pathway of gut epithelial stem cells destined to become endocrine cells (13). Homozygous NEUROG3 missense mutations in humans have been recently associated with a rare form of congenital malabsorptive diarrhea characterized by the lack of enteroendocrine cells (enteroendocrine cells dysgenesis or enteric anendocrinosis) (14). Neonatal diabetes was not reported, but two of three patients developed diabetes by the age of 8 years. Further studies suggested that the mutations were hypomorphic rather than null, and it was proposed that the residual activity was sufficient to preclude glucose intolerance, at least during the first years of life (15).
We report a patient with compound heterozygous mutations in NEUROG3 and a novel subtype of permanent neonatal diabetes associated with severe malabsorptive diarrhea. Introduction of the mutant proteins to chick embryonic gut endoderm showed that both mutations were functional null, supporting the hypothesis that the severity of the NEUROG3 deficiency is reflected in the severity of the β-cell defect and hence the age of presentation with diabetes.
RESEARCH DESIGN AND METHODS
This study was conducted in accordance with the Declaration of Helsinki and approved by the local ethics committee. Written informed consent was obtained from the parents/guardians of the patients.
NEUROG3 gene analysis.
The single coding exon of NEUROG3 was PCR-amplified in three overlapping fragments, sequenced on an ABI 3730 sequencer (Applied Biosystems, Warrington, UK), and compared with accession number NM_020999 using Mutation Surveyor v3.24 (SoftGenetics, State College, PA).
Clinical studies.
Intestinal biopsies were obtained by flexible endoscopy. Immunohistochemical assays for chromogranin A were carried out in formalin-fixed, paraffin-embedded biopsy samples of intestinal tissue using the S-ABC (streptavidin–biotin–peroxidase complex) technique and commercially available antibodies (BioGenex). Archival samples from a 4-year-old child with nonspecific GI symptoms (abdominal pain) were used as control samples.
A mixed meal test, consisting of 7 mL/kg Boost HP (Mead-Johnson) ingested over 2 min, was performed in the proband after an overnight fast. Insulin was not administered on the morning of the test and parenteral nutrition was withdrawn 48 h before the test. Venous blood was collected in EDTA with 50 µmol aprotinin (Trasylol, Bayer Pharmaceuticals) per milliliter of blood for hormonal assays at times 0 and 90 min. C-peptide was measured using a chemiluminescence immunoassay (Roche Diagnostics). Glucagon was measured by radioimmunoassay as previously described (16).
A standard oral glucose tolerance test with 75 g of glucose was undertaken in the parents of the patient after an overnight fast.
Functional studies.
The mutant protein isoforms were functionally characterized both in vitro and in vivo. Their ability to bind to an E-box element in the NEUROD1 promoter was investigated using a luciferase/Renilla reporter assay. In ovo electroporation of chicken embryos was used to further characterize the endocrine-inducing activity of wild-type and mutant NEUROG3 (see Supplementary Methods).
RESULTS
Case report.
The proband is a Chilean female of Spanish descent. She was born to nonconsanguineous parents at 37 weeks gestation with intrauterine growth retardation (birth weight 1910 g [−3.1 SDS for sex and gestational age]) and presented with nonprogressive nonketotic moderate hyperglycemia (120–180 mg/dL) on the first day of life. Insulin treatment was started on day 20 because of the persistence of hyperglycemia in the range 150–250 mg/dL. She has been on continual insulin since several attempts to discontinue insulin led to hyperglycemia >200 mg/dL, even in the face of severe diarrhea (see below). She has excellent metabolic control on NPH insulin twice a day plus a rapid-acting analog (lispro) before meals, with HbA1c usually <6.5% on insulin doses of 0.4–0.8 U/kg/day.
In addition to diabetes, she developed severe malabsorptive diarrhea as soon as significant enteral feedings were introduced. Diarrhea has required long-term mixed enteral and parenteral nutrition. Discontinuation of parenteral nutrition at the age of 2 years led to severe failure to thrive and ataxia. Brain computed tomography (CT) scan was normal. Because both resolved after the reintroduction of night-time parenteral nutrition, vitamin E deficiency secondary to malabsorption was considered the most likely cause of her neurologic symptoms. Despite extensive work-up, the cause of the diarrhea in this patient remained elusive. Abdominal CT scans repeatedly showed mild intestinal dilation and a macroscopically normal pancreas. Fecal elastase concentration was normal. Intestinal mucosa structure appeared normal after standard staining with hematoxylin-eosin.
The patient is currently 5 years old. Diarrhea remains her major problem, and she continues to pass 3 to 4 high-volume liquid stools daily. She takes regular home diet and an oral nutritional supplement (Pediasure) and receives night-time parenteral nutrition three times a week. Both weight (17.3 kg) and height (107.3 cm) are appropriate for her age. Her last HbA1c was 6.1%. Her daily insulin requirements are ∼0.8 and 0.4 U/kg per day on days with and without parenteral nutrition, respectively. Additional clinical details are in the Supplementary Data.
Molecular genetic findings.
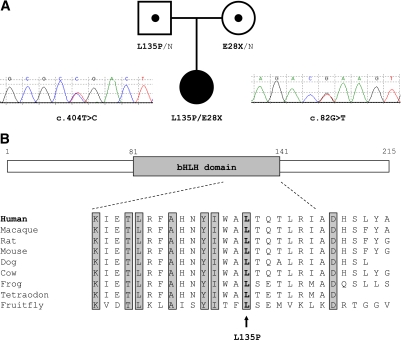
Two heterozygous mutations in NEUROG3 were identified (Fig. 1A). The maternally inherited c.82G>T mutation introduces a premature stop codon predicted to produce a truncated protein lacking the bHLH and the transactivation domain (p.E28X). The paternal c.404T>C mutation results in the substitution of proline for leucine at position 135 (p.L135P), which lies toward the end of the bHLH domain of NEUROG3 and is highly conserved across species (Fig. 1B). These variants have not been previously reported and were not present in 334 Caucasian control chromosomes.
FIG. 1.
A: Electropherograms and family pedigree showing inheritance of NEUROG3 mutations. Squares represent men, and circles represent women subjects. The black-filled symbol denotes the patient with neonatal diabetes, and the dot-filled symbols represent the unaffected heterozygous carriers. Genotype is shown underneath each symbol; N denotes the wild-type allele. B: Schematic organization of NEUROG3 protein. Numbers refer to the amino acids bordering the functional domains. The conservation across species of various residues within or nearby the bHLH domain is shown. (A high-quality color representation of this figure is available in the online issue.)
Clinical studies.
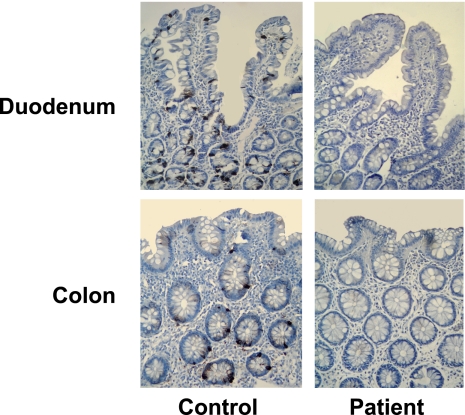
After the identification of the NEUROG3 mutations, intestinal biopsy samples were reinvestigated for the presence of enteroendocrine cells. Staining for chromogranin A revealed a complete absence of enteroendocrine cells in both the small bowel and the colon (Fig. 2). To better characterize the pancreatic function in the patient, a mixed meal test was performed, which showed a stimulated C-peptide level at 90 min of 546 pmol/L. Glucagon concentration was below the detection threshold of the assay both at fasting and after the mixed meal test.
FIG. 2.
Endoscopically resected intestinal mucosa from the patient and a control subject. Enteroendocrine cells can normally be identified by staining the preparation for chromogranin A (left panels). No immunohistochemical reactivity was seen either in the duodenal or in the colonic tissue from the patient (right panels). (A high-quality digital representation of this figure is available in the online issue.)
Both heterozygous parents denied diarrhea or any other gastrointestinal complaints and had normal glucose tolerance.
NeuroG3-induced transactivation of a NeuroD1 reporter construct.
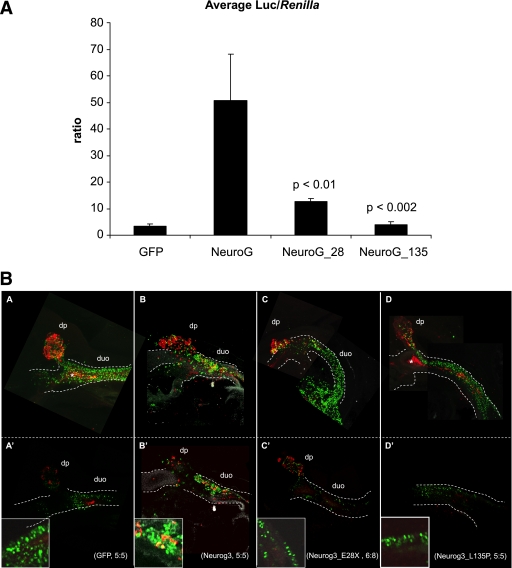
A NeuroD1 promoter-driven luciferase reporter gene was cotransfected with different NeuroG3 constructs into P19 cells, with SV40-driven renilla as internal standard (Fig. 3A), as previously reported (15). Wild-type NeuroG3 activity showed a 10- to 20-fold induction of Luc/renilla activity, compared with GFP vector alone.
FIG. 3.
A: Transactivation of the NEUROD1 promoter by wild-type (WT) and mutant NEUROG3 proteins in P19 cells. E28X activity is reduced to ∼25% compared with WT (P < 0.01 using a two-tailed Student t test), whereas L135P does not show activity over the vector control. Surprisingly, residual activity is seen when comparing E28X with the vector control (P < 0.00002). B: Whole-mount immunohistochemical detection of green fluorescent protein (GFP; green) and glucagon (red) in chicken embryos electroporated with WT and mutant NEUROG3 plasmids. WT NEUROG3 (B and B’), introduced into FoxA2 expressing endoderm of the prospective duodenum of 13–15 somite chicken embryos, induces the development of glucagon-expressing endocrine cells that delaminate from the duodenal epithelium, whereas control embryos (A and A’), or embryos expressing E28X (C and C’) and L135P (D and D’) mutants, do not develop such cells. A, B, C, and D show three-dimensional projections of the duodenum (duo) and dorsal pancreas (dp), whereas A’, B’, C’, and D’ show single optical sections from the same embryos. (A high-quality digital representation of this figure is available in the online issue.)
The NeuroG3L135P variant had no detectable activity. Surprisingly, NeuroG3E28X was capable of activating the NeuroD1 reporter, albeit at greatly reduced levels compared with NeuroG3 alone (Fig. 3A). Because a less severe truncation containing the first 124 amino acids is completely inactive (17), we speculated that overexpression conditions might lead to reduced fidelity of the introduced stop codon. However, Western blot analysis with Neurog3 antibodies detected 1 mg wild-type NeuroG3 programmed nuclear extract but failed to detect 20 mg NeuroG3E28X programmed extract so we estimate potential read-through of the nonsense codon to be less than 5%.
In vivo analysis by in ovo electroporation of chicken endoderm.
Previous studies have shown ectopic endocrine cell formation when NeuroG3 is electroporated into the chicken endoderm at Hamburger and Hamilton (HH) stage 12–15 (18). Electroporations with wild-type NeuroG3 confirmed delaminating and hormone expressing cells (Fig. 3B) identified outside the normal pancreas, whereas electroporation with nGFP alone had no detectable effect on the chicken endoderm (Fig. 3B). Electroporation with NeuroG3E28X failed to induce any endocrine cells in 6 of 8 embryos, whereas only a minuscule fraction of the total number of GFP+ cells expressed glucagon in the remaining two embryos (Fig. 3B). Such cells, which also are seen occasionally in vector controls, might be the result of electroporating cells that were already committed to endocrine fate. No ectopic endocrine cells were found in the NeuroG3L135P variant. We therefore conclude that NeuroG3L135P has no activity and NeuroG3E28X has very limited or no activity.
DISCUSSION
We report the first case of PNDM caused by biallelic NEUROG3 mutations. In keeping with the expression pattern of NEUROG3, the patient not only presented with neonatal diabetes but also developed severe diarrhea secondary to the lack of enteroendocrine cells.
Inactivation of Neurog3 in mice resulted in severe hyperglycemia and dehydration soon after birth (12), which highlights its central role during pancreatic endocrine specification. These knockout mice had a macroscopically normal pancreas, but islets of Langerhans were not identified on standard histological analysis. Furthermore, no hormone-containing cell could be detected by immunohistochemistry. The importance of Neurog3 in the control of endocrine differentiation can also be seen in the gut, where all kinds of gastrointestinal cells are derived from stem cells residing in the base of the intestinal crypts. In mice, intestinal enteroendocrine cells cannot differentiate without the expression of Neurog3 (13).
Enteroendocrine cell dysgenesis has previously been described in three patients with homozygous R93L or R107S NEUROG3 missense mutations (14). Interestingly, none presented with neonatal diabetes. However, the two patients who survived beyond early childhood developed persistent hyperglycemia by 8 years and were diagnosed with type 1 diabetes although a detailed characterization of the diabetic phenotype was not reported. Functional studies on these mutations revealed that the resulting protein products were hypomorphic and retained certain residual activity, which could contribute to precluding glucose intolerance during the first years of life (15). In addition, it has been proposed that NEUROG3 may differentially bind to specific cofactors in the intestinal and pancreatic progenitor cells (19).
The lack of detectable glucagon suggests that there are no α-cells, whereas the detectable C-peptide levels (and excellent metabolic control) suggest the presence of at least some β-cells. Neurog3 is required for both α- and β-cell development in mice, but the two cell types appear at different stages of embryonic development. Whereas α-cells appear during a narrow window in the early phase of pancreatic development, β-cells appear later, after the secondary transition (20). Thus β-cells develop from a much larger pool of progenitors and in larger numbers. It is possible that the minute residual activity of NEUROG3 (or an alternative bHLH factor) is capable of sustaining limited β- but no α-cell formation, because the larger pool of progenitors available for β-cell development partly compensates for the reduced proendocrine activity of NEUROG3. Alternatively, a redundant, NEUROG3-independent pathway may result in the production of at least some β-cells, as has previously been suggested (19).
This is a rare cause of PNDM. No mutations in NEUROG3 were reported in 13 patients with neonatal or childhood-onset antibody-negative type 1 diabetes (21) or in an additional 35 patients with permanent neonatal diabetes of unknown cause (unpublished data) (22).
Heterozygous mutations in NEUROD1, encoding another bHLH transcription factor that play a main role in the development of the endocrine pancreas, have been associated with autosomal dominant diabetes (23). This raised the hypothesis that mutations in NEUROG3 may also lead to the development of maturity-onset diabetes of the young (MODY) or late-onset familial diabetes. Two studies have failed to confirm this (24,25). Both parents in this study have a heterozygous null mutation in NEUROG3 and normal glucose tolerance (aged 30 and 35 years). It seems, therefore, unlikely that heterozygous mutations in NEUROG3 contribute significantly to MODY.
In conclusion, our study shows that recessive null mutations in NEUROG3 may cause a rare form of neonatal diabetes with intestinal anendocrinosis. This confirms the important role that NEUROG3 plays in the endocrine pancreas in humans and suggests a differential requirement for NEUROG3 gene dosage in enteroendocrine development versus pancreatic function.
ACKNOWLEDGMENTS
This work was funded by the European Union FP6 Integrated programme 2006-2010 EURODIA (LSHM-CT-2006-518153) and the Wellcome Trust (grants 067463/Z/2/Z and 083270/Z/07/Z). O.R.-C. was supported by an Ayuda para contratos post-Formación Sanitaria Especializada from the Instituto de Salud Carlos III (FIS CM06/00013). J.N.J. was supported by the Juvenile Diabetes Research Foundation Grant 10-2008-580. S.E. is employed as a core member of staff within the National Institute for Health Research–funded Peninsula Clinical Research Facility. A.T.H. was a Wellcome Trust Research Leave Fellow.
No potential conflicts of interest relevant to this article were reported.
O.R.-C. researched data, contributed to discussion, wrote and reviewed and edited the article. J.N.J. researched data and contributed to discussion. M.I.H. researched data and reviewed the article. E.C. researched data and reviewed the article. S.E., P.S., and A.T.H. contributed to discussion and reviewed and edited the article.
Parts of this study were presented in abstract form at the 8th Joint Lawson Wilkins Pediatric Endocrine Society/European Society for Paediatric Endocrinology Meeting, New York, New York, 9–12 September 2009.
The authors thank Emma Edghill (Institute of Biomedical and Clinical Science, Peninsula Medical School, Exeter, U.K.) and Javiera Torres and Ignacio Duarte (Department of Pathology, School of Medicine, Pontificia Universidad Católica, Santiago, Chile) for technical support. The authors are grateful to Karsten Skole Marckstrøm and Violeta Georgieva Tsonkova and to Mark Kalisz (Hagedorn Research Institute, Gentofte, Denmark) for critical discussions and technical help.
Footnotes
This article contains Supplementary Data online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db10-1008/-/DC1.
REFERENCES
- 1.Slingerland AS, Shields BM, Flanagan SE, et al. Referral rates for diagnostic testing support an incidence of permanent neonatal diabetes in three European countries of at least 1 in 260,000 live births. Diabetologia 2009;52:1683–1685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aguilar-Bryan L, Bryan J. Neonatal diabetes mellitus. Endocr Rev 2008;29:265–291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Greeley SA, Tucker SE, Worrell HI, Skowron KB, Bell GI, Philipson LH. Update in neonatal diabetes. Curr Opin Endocrinol Diabetes Obes 2010;17:13–19 [DOI] [PubMed] [Google Scholar]
- 4.Edghill EL, Flanagan SE, Patch AM, et al. Neonatal Diabetes International Collaborative Group Insulin mutation screening in 1,044 patients with diabetes: mutations in the INS gene are a common cause of neonatal diabetes but a rare cause of diabetes diagnosed in childhood or adulthood. Diabetes 2008;57:1034–1042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oliver-Krasinski JM, Stoffers DA. On the origin of the beta cell. Genes Dev 2008;22:1998–2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stoffers DA, Zinkin NT, Stanojevic V, Clarke WL, Habener JF. Pancreatic agenesis attributable to a single nucleotide deletion in the human IPF1 gene coding sequence. Nat Genet 1997;15:106–110 [DOI] [PubMed] [Google Scholar]
- 7.Sellick GS, Barker KT, Stolte-Dijkstra I, et al. Mutations in PTF1A cause pancreatic and cerebellar agenesis. Nat Genet 2004;36:1301–1305 [DOI] [PubMed] [Google Scholar]
- 8.Senée V, Chelala C, Duchatelet S, et al. Mutations in GLIS3 are responsible for a rare syndrome with neonatal diabetes mellitus and congenital hypothyroidism. Nat Genet 2006;38:682–687 [DOI] [PubMed] [Google Scholar]
- 9.Solomon BD, Pineda-Alvarez DE, Balog JZ, et al. Compound heterozygosity for mutations in PAX6 in a patient with complex brain anomaly, neonatal diabetes mellitus, and microophthalmia. Am J Med Genet A 2009;149A:2543–2546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith SB, Qu HQ, Taleb N, et al. Rfx6 directs islet formation and insulin production in mice and humans. Nature 2010;463:775–780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rubio-Cabezas O, Minton JA, Kantor I, Williams D, Ellard S, Hattersley AT. Homozygous mutations in NEUROD1 are responsible for a novel syndrome of permanent neonatal diabetes and neurological abnormalities. Diabetes 2010;59:2326–2331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gradwohl G, Dierich A, LeMeur M, Guillemot F. Neurogenin3 is required for the development of the four endocrine cell lineages of the pancreas. Proc Natl Acad Sci USA 2000;97:1607–1611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jenny M, Uhl C, Roche C, et al. Neurogenin3 is differentially required for endocrine cell fate specification in the intestinal and gastric epithelium. EMBO J 2002;21:6338–6347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang J, Cortina G, Wu SV, et al. Mutant neurogenin-3 in congenital malabsorptive diarrhea. N Engl J Med 2006;355:270–280 [DOI] [PubMed] [Google Scholar]
- 15.Jensen JN, Rosenberg LC, Hecksher-Sørensen J, Serup P. Mutant neurogenin-3 in congenital malabsorptive diarrhea. N Engl J Med 2007;356:1781–1782 [DOI] [PubMed] [Google Scholar]
- 16.Taheri S, Ghatei M, Bloom S. Measurement of gut hormones in plasma. Methods Mol Biol 2006;324:213–233 [DOI] [PubMed] [Google Scholar]
- 17.Rosenberg LC, Lafon ML, Pedersen JK, et al. The transcriptional activity of Neurog3 affects migration and differentiation of ectopic endocrine cells in chicken endoderm. Dev Dyn 2010;239:1950–1966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grapin-Botton A, Majithia AR, Melton DA. Key events of pancreas formation are triggered in gut endoderm by ectopic expression of pancreatic regulatory genes. Genes Dev 2001;15:444–454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martin MG, Wu SV, Cortina G. Mutant neurogenin-3 in congenital malabsorptive diarrhea. N Engl J Med 2007;356:1781–1782 [DOI] [PubMed] [Google Scholar]
- 20.Johansson KA, Dursun U, Jordan N, et al. Temporal control of neurogenin3 activity in pancreas progenitors reveals competence windows for the generation of different endocrine cell types. Dev Cell 2007;12:457–465 [DOI] [PubMed] [Google Scholar]
- 21.Nocerino V, Colombo C, Bonfanti R, Iafusco D, Barbetti F. Mutations in IAPP and NEUROG3 genes are not a common cause of permanent neonatal/infancy/childhood-onset diabetes. Diabet Med 2009;26:660–661 [DOI] [PubMed] [Google Scholar]
- 22.Edghill EL, Minton JA, Groves CJ, et al. Sequencing of candidate genes selected by beta cell experts in monogenic diabetes of unknown aetiology. JOP 2010;11:14–17 [PubMed] [Google Scholar]
- 23.Malecki MT, Jhala US, Antonellis A, et al. Mutations in NEUROD1 are associated with the development of type 2 diabetes mellitus. Nat Genet 1999;23:323–328 [DOI] [PubMed] [Google Scholar]
- 24.del Bosque-Plata L, Lin J, Horikawa Y, et al. Mutations in the coding region of the neurogenin 3 gene (NEUROG3) are not a common cause of maturity-onset diabetes of the young in Japanese subjects. Diabetes 2001;50:694–696 [DOI] [PubMed] [Google Scholar]
- 25.Kim SH, Warram JH, Krolewski AS, Doria A. Mutation screening of the neurogenin-3 gene in autosomal dominant diabetes. J Clin Endocrinol Metab 2001;86:2320–2322 [DOI] [PubMed] [Google Scholar]