Abstract
The water-soluble vitamin biotin is essential for normal cellular functions and its deficiency leads to a variety of clinical abnormalities. Mammals obtain biotin from exogenous sources via intestinal absorption, a process mediated by the sodium-dependent multivitamin transporter (SMVT). Chronic alcohol use in humans is associated with a significant reduction in plasma biotin levels, and animal studies have shown inhibition in intestinal biotin absorption by chronic alcohol feeding. Little, however, is known about the cellular and molecular mechanisms involved in the inhibition in intestinal biotin transport by chronic alcohol use. These mechanisms were investigated in this study by using rats and transgenic mice carrying the human full-length SLC5A6 5′-regulatory region chronically fed alcohol liquid diets; human intestinal epithelial Caco-2 cells chronically exposed to alcohol were also used as models. The results showed chronic alcohol feeding of rats to lead to a significant inhibition in carrier-mediated biotin transport events across jejunal brush border and basolateral membrane domains. This inhibition was associated with a significant reduction in level of expression of the SMVT protein, mRNA, and heterogenous nuclear RNA. Chronic alcohol feeding also inhibited carrier-mediated biotin uptake in rat colon. Studies with transgenic mice confirmed the above findings and further showed chronic alcohol feeding significantly inhibited the activity of SLC5A6 5′-regulatory region. Finally, chronic exposure of Caco-2 cells to alcohol led to a significant decrease in the activity of both promoters P1 and P2 of the human SLC5A6 gene. These studies identify for the first time the cellular and molecular parameters of the intestinal biotin absorptive processes that are affected by chronic alcohol feeding.
Keywords: transporter, SMVT, uptake, promoter, vitamin
biotin, a member of the B family of vitamins, is essential for normal cellular functions, growth, and development. The vitamin (a carboxyl carrier) acts as a cofactor for five carboxylases, four of which are located in the mitochondria and one in the cytoplasm (24, 25, 51). These carboxylases play a critical role in a variety of metabolic reactions that include gluconeogenesis, fatty acid synthesis, and amino acid catabolism (24, 25, 51). Biotin has also been shown to play a role in regulating gene expression (38). Deficiency of biotin leads to a variety of clinical abnormalities that include growth retardation, neurological disorders, and dermatological abnormalities (52). Biotin deficiency of varying degrees has been reported in a substantial number of patients with chronic alcoholism (5, 11), patients on long-term parenteral nutrition, individuals with inborn errors of biotin metabolism, and patients receiving long-term therapy with anticonvulsant agents (12, 19, 20, 26, 44).
All mammals, including humans, cannot synthesize biotin; rather they obtain the vitamin from exogenous sources via absorption in the intestinal tract. The human gut is exposed to two sources of biotin: dietary biotin (which is mainly absorbed in small intestine) and biotin released by the microflora of large intestine (which produces a significant amount of the vitamin) and is absorbed in that region (6, 53). Previous studies from our laboratory and others have utilized different small intestinal and colonic tissue/cellular preparations to show the involvement of an efficient Na+-dependent carrier-mediated process (39, 45). Subsequent studies have shown that whereas transport of biotin across the brush border membrane (BBM) and basolateral membrane (BLM) of the polarized enterocytes are both carrier mediated; the former but not the latter process is sodium dependent (43, 45). Other studies have shown that the involved intestinal biotin uptake system can also transport the structurally and functionally unrelated nutrients, pantothenic acid (a water-soluble vitamin) and lipoic acid (an important metabolic substrate for redox regulation of cell functions); for this reason the transporter has since been called the sodium-dependent multivitamin transporter (SMVT). Molecular identity of the SMVT system and the 5′-regulatory region (promoters) of its gene (SLC5A6) have been determined by cloning from a number of species [human, rat, rabbit, and mouse (gene accession no. AY572835)] and have been characterized (7, 32, 33, 37). We have also characterized different aspects of transcriptional and posttranscriptional regulation of the intestinal biotin uptake process and the involved SMVT system (30, 36). Finally, studies from our laboratory utilizing gene-specific [small interfering RNA (siRNA)] knockdown approach have established a predominant role for the SMVT system in intestinal biotin uptake (3).
Chronic alcohol consumption in humans is associated with a significant reduction in plasma biotin levels (5, 11), a finding that has been reproduced in rats fed alcohol chronically (46). Chronic alcohol feeding of rats was also found to be associated with a significant inhibition in the transepithelial, carrier-mediated biotin absorption process compared with absorption in pair-fed control animals (46). However, little is known about either molecular mechanism(s) involved in this inhibition of biotin uptake by chronic alcohol feeding or about the membrane site of the inhibition in the polarized enterocytes (BBM vs. BLM). We addressed these issues in the present investigation using small and large intestinal preparations isolated from rats fed an alcohol liquid or control rats pair fed an isocaloric liquid diet without alcohol. We also used transgenic mice carrying the human full-length SCL5A6 5′-regulatory region (which encompasses promoters P1 and P2 of this gene) that we have previously generated and characterized (37), to further confirm that the effect of chronic alcohol feeding is, at least in part, exerted at the transcriptional level. Furthermore, we extend the study to the human intestine by examining in Caco-2 cells (a human intestinal cell line) 1) the effect of ethanol on biotin uptake and 2) the mechanism of ethanol's effect on biotin uptake.
MATERIALS AND METHODS
Materials
[3H]Biotin (specific activity 30 Ci/mmol; radiochemical purity > 98%) was obtained from American Radiolabel (ARC, St. Louis, MO). Nitrocellulose filters (0.45-μm pore size) were purchased from Millipore (Fisher Scientific, Pittsburgh, PA). Unlabeled biotin and other chemicals including molecular biology reagents were obtained from commercial vendors and were of analytical grade.
Chronic Alcohol Feeding of Rats
Male Wistar rats (Charles River, Wilmington, MA) weighing ∼120 g (∼14 wk old) were housed at the Animal Core of the National Institute on Alcohol Abuse and Alcoholism-funded Southern California Research Center for ALPD (Alcoholic Liver and Pancreatic Disease) and Cirrhosis at University of Southern California. The experimental protocol was approved by the animal use committees of the Veterans Affairs Medical Center at Long Beach, CA, and the University of Southern California, Los Angeles, CA. Rats were fed Lieber-DeCarli (21) ethanol-liquid diet (that provides 36% of total calories from ethanol) (Bio-Serv, Frenchtown, NJ); control rats were pair fed the same liquid diet but without ethanol (maltose-dextrin replaced ethanol isocalorically). After 2 and 4 wk of chronic alcohol feeding, rats were euthanized; the jejunum was removed and BBM vesicles (BBMV) and BLM vesicles (BLMV) were isolated. An additional portion of the jejunum was stored at −80°C in TRIzol (Invitrogen, Carlsbad, CA) for determination of mRNA and heterogenous nuclear RNA (hnRNA) levels of SMVT transporters in later stage.
Preparation of Rat Jejunal BBMV and BLMV and Transport Studies
Two alcohol-fed rats and their two pair-fed controls were euthanized with ketamine and their jejunum was removed, flushed with ice-cold saline solution, and the mucosa was scrapped and pooled. BBMV were isolated on the same day from alcohol-fed rats and their pair-fed controls by a divalent cation (Mg2+) chelation method, whereas BLMV were isolated from fresh jejunal tissue by a Percoll-gradient differential centrifugation method. Both of these methods have been well established in our laboratory and also been widely used by others (8, 9, 13, 16, 42, 43, 48). These freshly isolated BBMV and BLMV were preloaded with a buffer of (in mM) 280 mannitol and 20 HEPES in pH 7.4. Uptake studies were carried out by incubating vesicles (10 s; initial rate) (40) in a buffer of 100 mM NaCl, 80 mM mannitol, 20 mM HEPES, pH 7.4, and in the presence of 0.5 μCi (250 nM) [3H]biotin. Transport studies were performed at 37°C according to a rapid-filtration technique described previously (40).
Preparation of Rat Colonic Sheets and Uptake Investigation
The colons of rats fed alcohol chronically and their pair-fed controls were removed and flushed with an ice-cold saline buffer solution. These flushed colons were cut open longitudinally and two adjacent 1-cm pieces (sheets) were then prepared from the mid portion and immediately incubated in Krebs-Ringer buffer (KR buffer) as described by us previously (15) (in mM: 133 NaCl, 4.93 KCl, 1.23 MgSO4, 0.85 CaCl2, 5 glucose, 5 glutamine, 10 HEPES, 10 MES, pH 7.4) in the presence of 0.5 μCi (25 nM) [3H]biotin. The colonic sheets were incubated at 37°C for 5 min (initial rate, data not shown) for uptake process. Uptake was stopped by aspiration of the incubation solution followed by addition of fresh 5 ml of ice-cold KR buffer. The colonic sheets were then washed again with ice-cold KR buffer, digested with 1 N NaOH, and neutralized with 10 N HCl, and radioactivity was counted in a Beckman Coulter LS6500 multipurpose liquid scintillation counter.
Western Blot Analysis
Western blot analysis was performed on purified BBM protein isolated from the jejunum of alcohol-fed and control pair-fed rats. Sixty micrograms of BBM proteins were resolved onto premade 4–12% Bis-Tris minigel (Invitrogen) as described before (4, 29, 30). After electrophoresis, proteins were electroblotted onto polyvinylidene difluoride membrane (Bio-Rad, Hercules, CA) and then blocked with a PBS-Tween 20 solution containing 5% dried milk (Bio-Rad) for 1 h at room temperature. The membranes were then incubated with rat SMVT-specific polyclonal antibodies. The specificity of the antibodies was confirmed by treating synthetic antigenic peptide against rat SMVT protein as described by us previously (4, 30, 49). The SMVT-immunoreactive bands were detected by using a chemiluminescence kit (Amersham Pharmacia Biotech) and autoradiography (Kodak film). The SMVT-specific bands were quantified by use of UN-SCAN-IT gel version 6.1 (Silk Scientific, Orem, UT) gel digitizing software.
Semiquantitative RT-PCR Assay of hnRNA
To investigate the effect of chronic alcohol feeding on transcriptional rate of SMVT gene in rat intestine, we determined and compared the level of hnRNA expression in the jejunum of alcohol-fed rats and their pair-fed controls. The first product of gene transcription is the primary transcript of pre-mRNA or hnRNA, which includes introns as well as exons (10). Rate of hnRNA transcription reflects rate of gene transcription (2, 10, 17). We determined the level of SMVT hnRNA expression in rat intestine SMVT using gene-specific primers (designed to amplify 619-bp product) as shown in Table 1. A negative control, which constituted a reaction without cDNA template, was run with every assay to establish specificity. The amplified products were then run on 1% agarose gel, and the specific bands were quantified by using UN-SCAN-IT gel automated digitizing system, version 6.1 (Silk Scientific) gel digitizing software.
Table 1.
Primers used for amplifying coding region of the respective genes by real-time and semiquantitative PCR
| Gene Name | Primers |
|---|---|
| Real-time PCR | |
| rSMVT | Forward: 5′-GAGGATGACTGTGGCGAGCAC-3′ |
| Reverse: 5′-CAGCTCACCAACAGTATGGC-3′ | |
| mSMVT | Forward: 5′-CGTAGGAACTTTGGTAGCCCTGG-3′ |
| Reverse: 5′-CTTAGGTGTGATGGGTCTCTCC-3′ | |
| β-Actin | Forward: 5′-GTCAGGTCATCACTATCGGC-3′ |
| Reverse: 5′-CATGGATGCCACAGGATTCC-3′ | |
| hnRNA primers | |
| rSMVT | Forward: 5′-CTAAGGAAGATGCCTGATG-3′ |
| Reverse: 5′-CTCTGGGAAAAAGAGTCAG-3′ | |
| rβ-Actin | Forward: 5′-CTGCTCTTTCCCAGATGAG-3′ |
| Reverse: 5′-CTCATAGATGGGCACAGTG-3′ |
Real-Time PCR Analysis
Total RNA (5 μg) was isolated from jejunum of alcohol-fed rats and their pair-fed controls were treated with DNAse I (Invitrogen, Carlsbad, CA) enzyme to prevent DNA contamination. The DNAse I-treated samples were subjected for cDNA synthesis by using iScript cDNA synthesis kit (Bio-Rad). To amplify the coding region of rat SMVT, and β-actin, we used the gene specific primers (Table 1) for real-time PCR study. Real-time PCR conditions were same as described previously (35, 50). The data were normalized to β-actin and then quantified by a relative relationship method supplied by the vendor (Bio-Rad) (22).
Chronic Alcohol Feeding of Transgenic Mice Carrying the Human SLC5A6 5′-Regulatory Region
In these investigations, we use transgenic mice that carry the full-length human SLC5A6 5′-regulatory region (which encompasses promoters P1 and P2) that have been generated and characterized by us previously (37). Sex- and weight-matched littermate transgenic mice (determined by PCR to have similar level of luciferase expression) were divided into a control group and an alcohol-fed group. The first group was given control-liquid diet (maltose-dextrin replaced ethanol isocalorically) whereas the latter group was fed for 4 wk an ethanol-liquid diet (Lieber-DeCarli; Bio-Serv) that provided 25% of total calories in the form of ethanol. Alcohol in the liquid diet was gradually increased (by 5% of total calories per day until it reached 25%).
Isolation of Epithelial Cells, Determination of Luciferase Activity, and Real-Time PCR from Mouse Jejunum
Intestinal epithelial cells were isolated from alcohol-fed transgenic mice and their pair-fed controls on the same day by using an established procedure (31). Briefly, mice were euthanized and their jejunum was removed, washed with ice-cold PBS, open longitudinally, and sliced into small pieces then washed with Hank's balanced salt solution (HBSS) containing 1% FBS followed by HBSS with 2% glucose and BSA. Enterocytes were isolated by incubation (2 × 15 min) at 37°C with shaking in HBSS supplemented with 0.5 mM dithiothreitol and 1.5 mM EDTA. Cell viability was determined by Trypan blue exclusion and found >85% for both control and alcohol-treated groups. The cells were collected by centrifugation (1,000 g for 5 min) and divided into two groups. The first group was suspended in Na+-containing KR buffer (in mM: 133 NaCl, 4.93 KCl, 1.23 MgSO4, 0.85 CaCl2, 5 glucose, 5 glutamine, 10 HEPES, 10 MES, pH 7.4). The second group of cells was suspended in Na-free KR buffer (Na was replaced isoosmotically by Li). Uptakes were carried out by incubating (for 5 min; initial rate; unpublished observations) 50 μl cell suspension with 50 μl of Na+-containing or Na-free KR buffer containing 250 nM [3H]biotin. A small piece of mouse jejunum was also removed for determination of luciferase activity as described by us previously (37) or stored in TRIzol for determination of mouse endogenous SMVT mRNA by using mouse SMVT-specific primers (Table 1) and real-time PCR conditions as described above.
Chronic Exposure of Human Intestinal Epithelial Caco-2 Cell to Alcohol
Caco-2 cells (ATCC, Manassas, VA; passages 5 to 15) were plated at a density of 2 × 105 cells/well onto 12-well plates in MEM (ATCC) supplemented with 10% FBS and antibiotics. Twenty-four hours later, fresh growth medium containing 200 mM of alcohol [a concentration that mimics the level of alcohol in the intestine in chronic alcohol drinkers (34)] was introduced, and the plates were kept in an ethanol-saturated incubator for 96 h as described recently (50) to minimize ethanol evaporation; in addition, the alcohol-containing growth medium was changed every 12 h (50). Uptake studies were performed at 37°C in KR buffer as described by us previously (23). Labeled and unlabeled biotin was added to the incubation medium at the onset of incubation, and uptake was examined during the initial linear period of uptake (5 min; data not shown). The reaction was terminated by the addition of 2 ml of ice-cold KR buffer followed by immediate aspiration. Cells were then rinsed twice with ice-cold KR buffer, digested with 1 ml of 1 N NaOH, neutralized with 10 N HCl, and then measured for radioactive content via scintillation counter. Digested samples (100 μl each) were taken for determining protein concentration (Bio-Rad Dc protein assay kit).
Transfection of Caco-2 Cells and Assay of Promoter Activity
Promoters P1 and P2 of the human SLC5A6 gene were generated and characterized by us previously (7). Caco-2 cells were cotransfected (in 12-well plates at <80% confluency) with 4 μg of either SLC5A6 promoter P1 (−5846 to −4400 bp; using the A in the initiator ATG as position +1) or P2 (−4417 to −3679 bp) constructs, together with 100 ng of plasmid carrying the Renilla luciferase-thymidine kinase (pRL-TK) (Promega, Madison, WI) to serve as an internal control. Transfection was performed with Lipofectamine 2000 (Invitrogen) according to the manufacturer's instructions. On the second posttransfection day, cells were treated with MEM containing 200 mM alcohol for 96 h. At the end of 96 h of exposure to alcohol, Renilla-normalized firefly luciferase activity was determined by using the Dual Luciferase Assay System (Promega) as described by us previously (7, 37, 50).
Statistical Analysis
Uptake data with rat intestinal preparations presented in this paper are means ± SE of multiple separate determinations from multiple rats and are expressed in femtomoles per milligram protein per unit time. Uptakes with the human intestinal epithelial Caco-2 cells were also means ± SE from at least three separate experiments. Student's t-test was used for statistical analysis. P < 0.05 was considered statistically significant. Carrier-mediated biotin uptake was determined by subtracting uptake by simple diffusion (determined from the slope of the line between uptake at high pharmacological concentration of 1 mM and point of origin) from total uptake. Protein, mRNA, and hnRNA determinations as well as promoter assays were run on at least three different occasions using different preparations.
RESULTS
Effect of Chronic Alcohol Feeding on Physiological and Molecular Parameters of the Biotin Uptake Process in Rat Intestine
Effect of chronic alcohol feeding on physiological parameters of biotin transport in rat small intestine.
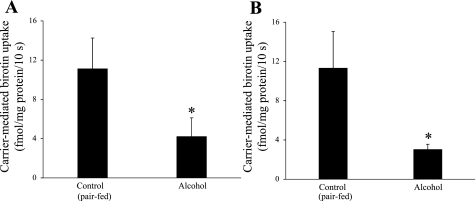
Effect of chronic alcohol feeding (for 2 and 4 wk) of rats on biotin transport across jejunal BBM was examined by using purified BBMV preparations. Data were compared with uptake by jejunal BBMV simultaneously isolated from pair-fed rats. The results showed significant (P < 0.05 for both) inhibition in initial rate of carrier-mediated biotin (250 nM) uptake by BBMV from rats chronically fed alcohol for 2 and 4 wk compared with uptake by their pair-fed controls (Fig. 1, A and B, respectively). We performed all other studies at 4 wk of chronic alcohol feeding.
Fig. 1.
Effect of chronic alcohol feeding on carrier-mediated biotin uptake by rat jejunal brush border membrane (BBM) vesicles (BBMV). Rats were chronically fed alcohol-liquid diet for 2 (A) and 4 wk (B); control rats were pair fed the same liquid diet but without alcohol. BBMV were isolated from the jejunum of both rat groups simultaneously and were used fresh on the day of isolation. [3H]biotin (250 nM) was added at the onset of the uptake experiment. Data are means ± SE of at least 4 separate uptake determinations from multiple sets of rats. *P < 0.05.
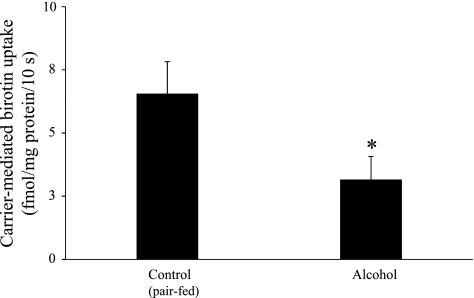
We also examined the effect of chronic alcohol feeding (4 wk) of rats on biotin transport across jejunal BLM (i.e., on the exit step from the enterocyte) using purified BLMV preparations. Data were compared with uptake by jejunal BLMV isolated simultaneously from pair-fed rats. The results showed a significant (P < 0.01) inhibition in the initial rate of carrier-mediated biotin (250 nM) uptake by BLMV from rats chronically fed alcohol for 4 wk compared with uptake by their pair-fed controls (Fig. 2).
Fig. 2.
Effect of chronic alcohol feeding on carrier-mediated biotin uptake by rat jejunal basolateral membrane vesicles (BLMV). Rats were chronically fed alcohol-liquid diet for 4 wk; control rats were pair fed the same liquid diet but without alcohol. BLMV were isolated from the jejunum of both rat groups simultaneously and were used fresh on the day of isolation. [3H]biotin (250 nM) added at the onset of uptake experiment. Data are means ± SE of at least 6 separate uptake determinations from multiple sets of rats. *P < 0.01.
Effect of chronic alcohol feeding on molecular parameters of biotin transport in rat small intestine.
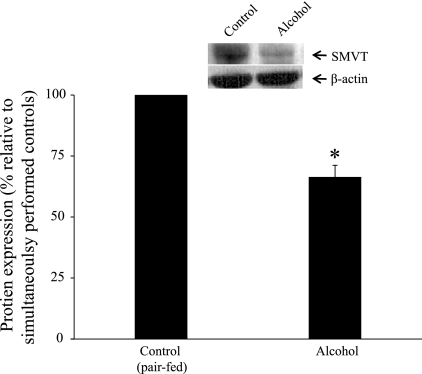
Effect of chronic alcohol feeding on level of expression of the SMVT protein (which is expressed exclusively at the apical membrane domain of enterocytes) (49) was examined by means of Western blot analysis utilizing jejunal BBM preparations isolated from alcohol-fed rats and their pair-fed controls and specific rat anti-SMVT polyclonal antibodies. The results showed a significantly (P < 0.05) lower level of expression of the SMVT protein in the jejunal BBM preparations of rats chronically fed alcohol compared with their pair-fed controls (Fig. 3).
Fig. 3.
Effect of chronic alcohol feeding of rats on sodium-dependent multivitamin transporter (SMVT) protein expression at intestinal BBM. Western blot analysis was carried out by using intestinal BBM proteins (60 μg) isolated from chronic alcohol-fed rats (4 wk) and their pair-fed controls (see materials and methods). BBM proteins were resolved on NuPAGE 4–12% mini gel and electroblotted onto polyvinylidene difluoride membrane as described in materials and methods. Blots were incubated with rabbit polyclonal anti-SMVT primary antibody and detected by using anti-rabbit conjugated with horseradish peroxidase as described in materials and methods. Data are means ± SE of 3 separate samples from multiple rats and were normalized relative to β-actin protein expression as described in materials and methods. *P < 0.05.
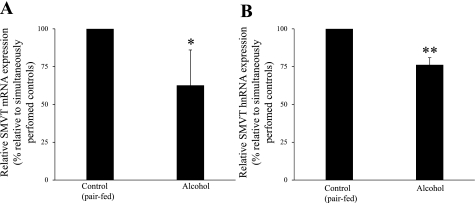
In other studies we examined (by means of real-time PCR) the effect of chronic alcohol feeding (4 wk) on the level of expression of the SMVT mRNA in rat jejunal mucosa and compared the data to level of expression in the jejunal mucosa of pair-fed control animals. The results showed a significant (P < 0.05) reduction in the level of expression of the SMVT mRNA in the jejunal mucosa of alcohol-fed rats compared with controls (Fig. 4A).
Fig. 4.
Effect of chronic alcohol feeding of rats on SMVT mRNA and heterogenous nuclear RNA (hnRNA) expression. A: real-time quantitative PCR was performed with use of rat SMVT gene-specific primers, normalized relative to rat β-actin, and calculated as described in materials and methods. Data are means ± SE of 6 separate samples from 6 rats. *P < 0.05. B: a semiquantitative RT-PCR was carried out by using SMVT hnRNA gene-specific primers and rat β-actin gene specific primers as described in materials and methods. Data are means ± SE of 6 separate samples from 6 rats. **P < 0.02.
We also determine the effect of chronic alcohol feeding (4 wk) on level of expression of SMVT hnRNA in rat jejunal mucosa (see materials and methods), since hnRNA level is an indicative of gene transcriptional activity (10). The results showed a significant (P < 0.02) reduction in the level of expression of the SMVT hnRNA in alcohol-fed rats compared with their pair-fed controls (Fig. 4B). These results suggest that the above-described inhibition in intestinal biotin uptake by chronic alcohol feeding is, at least in part, being exerted at the transcriptional level.
Effect of chronic alcohol feeding on biotin uptake in rat colon.
As mentioned earlier, normal microflora of the large intestine synthesize a considerable amount of biotin and epithelial cells of the large intestine possess an efficient Na+-dependent carrier-mediated mechanism for uptake of this biotin and express SMVT (41). Thus we investigate the effect of chronic alcohol feeding on initial rate of carrier-mediated biotin (25 nM) uptake by rat colon by using an established colonic sheet preparations (15); the results were compared with uptake by colonic sheets prepared simultaneously from pair-fed controls. The results showed a significant inhibition (P < 0.05) in carrier-mediated biotin uptake in colonic sheets from alcohol-fed rats compared with controls (Fig. 5). These results suggest that chronic alcohol feeding also negatively affects biotin uptake process in colon, thereby inhibiting absorption of bacterially synthesized biotin.
Fig. 5.
Effect of chronic alcohol feeding of rats on carrier-mediated biotin uptake by colonic sheets. Colonic sheets were prepared as described in materials and methods from chronic alcohol-fed rats (4 wk) and their pair-fed controls. The initial rate of carrier-mediated [3H]biotin (25 nM) uptake was determined. Data are means ± SE of 5 separate uptake determinations from multiple rats. *P < 0.05.
Effect of Chronic Alcohol Feeding on Physiological and Molecular Parameters of Biotin Uptake in the Small Intestine of Transgenic Mice Carrying the Human Full-Length SLC5A6 5′-Regulatory Region
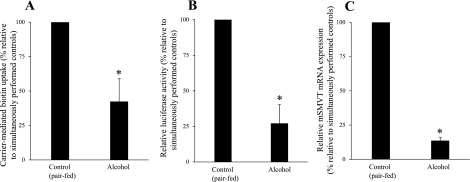
In these studies, we first confirmed the effect of chronic alcohol feeding (alcohol provided 25% of total calories for 4 wk) on biotin (250 nM) uptake by isolated jejunal epithelial cells of transgenic mice carrying the human full-length SLC5A6 5′-regulatory region (this genomic region encompasses promoters P1 and P2, i.e., −5846 to −3679). This transgenic mouse line has been previously generated and characterized in our laboratory and has been used in previous physiological investigations (36, 37). Results were compared with simultaneously performed studies on sex- and weight-matched pair-fed control transgenic littermates. The results showed a significant inhibition (P < 0.01) in the initial rate of the Na+-dependent carrier-mediated biotin uptake in the alcohol-fed transgenic mice compared with control transgenic littermates (Fig. 6A). We then examined the effect of chronic alcohol feeding (4 wk) of the transgenic mice on activity of the human full-length SLC5A6 5′-regulatory region in jejunal mucosa. Activity of the 5′-regulatory region was determined by measuring the level of activity of the firefly luciferase reporter gene as described by us previously (36, 37). Data were compared with luciferase activity in jejunal mucosa of pair-fed control (littermate) transgenic mice. The results showed that chronic alcohol feeding leads to a significant (P < 0.01) reduction in luciferase activity in the jejunal mucosa compared with its activity in the jejunal mucosa of the pair-fed control transgenic mice (Fig. 6B). A concomitant significant (P < 0.01) decrease in the level of expression of the mouse endogenous SMVT mRNA in the same jejunal mucosal samples of the alcohol-fed transgenic mice was observed compared with its level in the jejunal mucosa of control transgenic littermate mice (Fig. 6C). These results further confirm that the inhibition in intestinal biotin uptake by chronic alcohol feeding is, at least in part, exerted at the level of transcription of the SLC5A6 gene.
Fig. 6.
Effect of chronic alcohol feeding on carrier-mediated biotin uptake, activity of the human full-length SLC5A6 5′-regulatory region, and on level of expression of the endogenous mouse SMVT (mSMVT) mRNA, in transgenic mice carrying the human full-length SLC5A6 5′-regulatory region. Enterocytes were isolated as described in materials and methods from chronic alcohol-fed transgenic mice and their pair-fed transgenic littermate controls. A: Na+-dependent carrier-mediated [3H]biotin (250 nM) uptake by isolated enterocytes prepared from chronic alcohol-fed transgenic mice with their pair-fed control littermates. Data are means ± SE of 7 separate uptake determinations from multiple mice. *P < 0.01. B: firefly luciferase activity in the jejunum of transgenic mice carrying the human full-length SLC5A6 5′-regulatory region (which encompasses promoter P1 and P2) fused to firefly luciferase reporter gene after 4 wk of alcohol or control (pair) feeding. Data are means ± SE of 5 separate samples from 5 mice. *P < 0.01. C: real-time quantitative PCR was performed by using mouse SMVT gene-specific primers and normalized relative to mouse β-actin as described in materials and methods. Data are means ± SE of 5 separate samples from 5 mice. *P < 0.01.
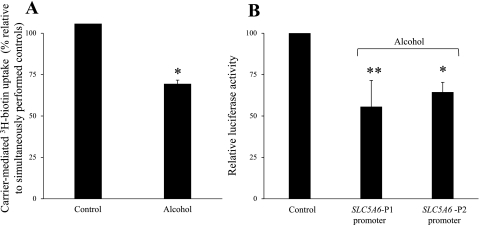
Effect of Chronic Alcohol Exposure on Physiological and Molecular Parameters of Biotin Uptake by Human Intestinal Epithelial Caco-2 Cells
To extend our studies to the human intestine, to further confirm that the effect of chronic alcohol use is (at least in part) being exerted at the transcriptional level, and to determine whether chronic alcohol is exerting its effect on the activity of the promoters P1 and/or P2 of the SLC5A6 gene, we performed these studies. First we examined the effect of chronic alcohol exposure (96 h) of human intestinal epithelial Caco-2 cells on biotin uptake. Chronic exposure of confluent monolayers was performed as described recently by You et al. (54) and adopted in our laboratory (50). A concentration of alcohol of 200 mM was chosen to mimic the level of alcohol in the intestinal lumen of chronic alcoholics (34). The results showed a significant (P < 0.01) inhibition in carrier-mediated biotin (25 nM) uptake by cells exposed chronically to alcohol compared with control cells (Fig. 7A). We then examined the effect of chronic alcohol exposure (200 mM, 96 h) on the activity of the individual human SLC5A6 promoters P1 and P2 (7) after transient expression in Caco-2 cells. The results showed chronic alcohol exposure to lead to a significant reduction in the activity of both promoter P1 (P < 0.05) and P2 (P < 0.01) (Fig. 7B). These results further indicate that the inhibitory effect of chronic alcohol exposure on intestinal biotin uptake is being exerted (at least in part) at the transcriptional level of the human SLC5A6 gene and shows that activity of both promoters P1 and P2 are affected.
Fig. 7.
Effect of chronic alcohol exposure of Caco-2 cells on carrier-mediated biotin uptake and on activity of the SLC5A6 full-length promoters P1 and P2. A: Caco-2 cells were exposed to 200 mM alcohol for 96 h. Initial rate of carrier-mediated [3H]biotin (25 nM) uptake was then determined and data were compared with simultaneously performed controls. Data are means ± SE of 3 separate uptake determinations performed by using different batches of cells on 3 different occasions. *P < 0.01. B: human full-length SLC5A6 promoters P1 and P2 in PGL3-basic were transfected individually into Caco-2 cells, which were then exposed (200 mM alcohol for 96 h) to ethanol. Luciferase activity was then determined as described in materials and methods. Data are represented as means ± SE of 3 independent experiments performed on different batches of cells on 3 different occasions. **P < 0.05.
DISCUSSION
As mentioned earlier, chronic alcohol consumption is associated with a significant reduction in plasma biotin levels (5, 11), and animal studies have shown that chronic alcohol feeding significantly inhibit intestinal biotin absorption (46). Since little is known about the cellular and molecular parameters of the intestinal biotin absorption process that are affected by chronic alcohol use, we investigated these issues in the present study. We used an in vivo model of alcohol delivery involving rats and transgenic mice that carry the human full-length SLC5A6 5′-regulatory region, and an in vitro model of chronic alcohol exposure of human intestinal epithelial Caco-2 cells [an established in vitro model to study human intestinal biotin transport (23)].
Our studies with the rat model showed chronic alcohol feeding to cause a significant inhibition in both the entry step of biotin into the polarized enterocytes, i.e., transport across the BBM, and the exit step, i.e., transport across the BLM. This inhibition was evident as early as 2 wk following the initiation of alcohol-feeding regimen. These findings confirm the previously reported finding that chronic alcohol feeding inhibits intestinal biotin absorption (46) and further demonstrate that the inhibition affects biotin movement across both membrane domains of the absorptive epithelial cells. Chronic alcohol feeding of rats was also found to lead to a significant decrease in the level of expression of the SMVT protein and mRNA (SMVT is the predominant biotin uptake system in the gut) (3). The decrease in the level of expression of SMVT mRNA in chronic alcohol-fed rats compared with their pair-fed controls suggests that the inhibition may be, at least in part, being exerted at the transcriptional level of the SLC5A6 gene. This possibility was supported by the observation that chronic alcohol feeding leads to a significant inhibition in the level of expression of the SMVT hnRNA in intestinal mucosa. Whether other mechanisms are also involved in causing the inhibition in intestinal biotin absorption (e.g., change in SMVT RNA stability, changes in the level of expression of an accessory protein that is needed for normal function of the SMVT system) is not clear and requires further investigations.
The effect of chronic alcohol feeding was not limited to absorption of biotin in the small intestine (the site of absorption of dietary biotin) but also included inhibition in carrier-mediated biotin uptake in the large intestine (colon), which is the site of absorption further bacterially synthesized biotin. Thus chronic alcohol feeding appears to affect the overall intestinal physiology of biotin, and therefore, availability of biotin from both the dietary and the bacterial sources could be compromised. It is relevant to mention here that the concentration of ethanol in the colon is relatively low and is mainly derived from the blood since the majority of ingested alcohol is absorbed in the small intestine (34). However, since some of the ethanol that enters the colon is oxidized by colonic bacteria to the more toxic acetaldehyde (34), and that colonic mucosa has a low level of alcohol dehydrogenase activity (47), it is possible that the observed inhibition in biotin uptake in the colon of rats fed alcohol chronically is also the result of an effect of this metabolite on the biotin absorption process.
As mentioned above, our studies with rats chronically fed alcohol has suggested that the inhibitory effect on intestinal biotin absorption process is, at least in part, being exerted at the Slc5A6 transcriptional level. To confirm this finding, we took advantage of the availability in our laboratory of a transgenic mouse line that carries the human full-length SLC5A6 5′-regulatory region that we have previously generate and characterized (36, 37). Our results showed that chronic alcohol feeding of these transgenic mice leads to a significant inhibition in both intestinal carrier-mediated-biotin uptake and in level of expression of the mouse endogenous SMVT mRNA in intestinal mucosa. Most importantly, activity of the human full-length SLC5A6 5′ regulatory region in the intestine of these transgenic mice was found to be significantly reduced compared with its activity in the intestine of their pair-fed control littermates. These findings clearly support the earlier suggestion that chronic alcohol inhibition of intestinal biotin transport is, at least in part, being exerted at the level of transcription of the SLC5A6 gene.
To extend our findings on the effect of chronic alcohol use on biotin transport in animal intestine to the human intestine and to further confirm that the effect of chronic alcohol feeding is, at least in part, being exerted at the transcriptional level as well as to determine whether chronic alcohol use is affecting the activity of promoters P1 and/or P2 of the SLC5A6 gene, we also performed studies in which we examined the effect of chronic exposure of human intestinal epithelial Caco-2 cells to alcohol on biotin uptake parameters. As seen with rat and mouse intestine, chronic alcohol exposure led to a significant inhibition in carrier-mediated biotin uptake by Caco-2 cells. This inhibition was associated with a significant reduction in the activity of both promoter P1 and P2 of the SLC5A6 gene. These findings clearly show that biotin uptake by human intestinal epithelial cells is similarly affected by chronic alcohol exposure and that the inhibitory effect is exerted, at least in part, at the transcriptional level and involves both of the SLC5A6 promoters.
As mentioned earlier, biotin deficiency is associated with neurological and dermatological disorders (52). Whether the reduced biotin levels (mediated in part by causing the inhibition in intestinal absorption) could play a role in neurological and dermatological disorders associated with chronic alcoholism (1, 14, 18) is not known and requires further investigation. Further studies are also warranted to address whether biotin deficiency is even more prevalent in alcoholics than originally reported (11) since a less sensitive assay was used to determine biotin level compared with the current more sensitive HPLC/gas chromatography-mass spectrometry procedures (27). When such sensitive assays were used in case of pregnancy (27, 28), a much higher prevalence of biotin deficiency was found than originally reported.
In summary, our studies show that chronic alcohol feeding/exposure inhibits cellular and molecular parameters of intestinal biotin uptake process and that the effect is (at least in part) being exerted at the transcriptional level. In addition, chronic alcohol consumption appears to negatively impact biotin absorption both in the small and large intestine.
GRANTS
This research was supported by grants from the Department of Veterans Affairs and the National Institutes of Health (DK58057 and AA18071).
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
REFERENCES
- 1. Aronson PJ, Malick F. Towards rational treatment of severe psoriasis in alcoholics: report of two cases. J Drugs Dermatol 9: 405–408, 2010 [PubMed] [Google Scholar]
- 2. Aydemir F, Jenkitkasemwong S, Gulec S, Knutson MD. Iron loading increases ferroportin heterogeneous nuclear RNA and mRNA levels in murine J774 macrophages. J Nutr 139: 434–438, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Balamurugan K, Ortiz A, Said HM. Biotin uptake by human intestinal and liver epithelial cells: role of the SMVT system. Am J Physiol Gastrointest Liver Physiol 285: G73–G77, 2003 [DOI] [PubMed] [Google Scholar]
- 4. Balamurugan K, Vaziri ND, Said HM. Biotin uptake by human proximal tubular epithelial cells: cellular and molecular aspects. Am J Physiol Renal Physiol 288: F823–F831, 2005 [DOI] [PubMed] [Google Scholar]
- 5. Bonjour JP. Vitamins and alcoholism. V. riboflavin, VI. niacin, VII. pantothenic acid, and VIII. biotin. Int J Vitam Nutr Res 50: 425–440, 1980 [PubMed] [Google Scholar]
- 6. Combs GF. The Vitamins: Fundamental Aspects in Nutrition and Health. San Diego, CA: Academic, 1992, p. 329–343 [Google Scholar]
- 7. Dey S, Subramanian VS, Chatterjee NS, Rubin SA, Said HM. Characterization of the 5′ regulatory region of the human sodium-dependent multivitamin transporter, hSMVT. Biochim Biophys Acta 1574: 187–192, 2002 [DOI] [PubMed] [Google Scholar]
- 8. Dudeja PK, Tyagi S, Gill R, Said HM. Evidence for a carrier-mediated mechanism for thiamine transport to human jejunal basolateral membrane vesicles. Dig Dis Sci 48: 109–115, 2003 [DOI] [PubMed] [Google Scholar]
- 9. Dudeja PK, Tyagi S, Kavilaveettil RJ, Gill R, Said HM. Mechanism of thiamine uptake by human jejunal brush-border membrane vesicles. Am J Physiol Cell Physiol 281: C786–C792, 2001 [DOI] [PubMed] [Google Scholar]
- 10. Elferink CJ, Reiners JJ., Jr Quantitative RT-PCR on CYP1A1 heterogeneous nuclear RNA: a surrogate for the in vitro transcription run-on assay. Biotechniques 20: 470–477, 1996 [DOI] [PubMed] [Google Scholar]
- 11. Fennelly J, Frank O, Baker H, Leevy CM. Peripheral neuropathy of the alcoholic: I, aetiological role of aneurin and other B-complex vitamins. Br Med J 2: 1290–1292, 1964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Forbes GM, Forbes A. Micronutrient status in patients receiving home parenteral nutrition. Nutrition 13: 941–944, 1997 [DOI] [PubMed] [Google Scholar]
- 13. Gastaldi G, Casirola D, Ferrari G, Rindi G. Effect of chronic ethanol administration on thiamine transport in microvillous vesicles of rat small intestine. Alcohol Alcohol 24: 83–89, 1989 [DOI] [PubMed] [Google Scholar]
- 14. Gehrig KA, Dinulos JG. Acrodermatitis due to nutritional deficiency. Curr Opin Pediatr 22: 107–112, 2010 [DOI] [PubMed] [Google Scholar]
- 15. Greene HL, Moore MC, Said HM, Ghishan FK, Orth DN. Intestinal glucose transport in suckling rats fed artificial milk with and without added epidermal growth factor. Pediatr Res 21: 404–408, 1987 [DOI] [PubMed] [Google Scholar]
- 16. Hunter CK, Treanor LL, Gray JP, Halter SA, Hoyumpa A, Jr, Wilson FA. Effects of ethanol in vitro on rat intestinal brush-border membranes. Biochim Biophys Acta 732: 256–265, 1983 [DOI] [PubMed] [Google Scholar]
- 17. Kohler CU, Roos PH. Focus on the intermediate state: immature mRNA of cytochromes P450—methods and insights. Anal Bioanal Chem 392: 1109–1122, 2008 [DOI] [PubMed] [Google Scholar]
- 18. Kostovic K, Lipozencic J. Skin diseases in alcoholics. Acta Dermato-Venerol 12: 181–190, 2004 [PubMed] [Google Scholar]
- 19. Krause KH, Berlit P, Bonjour JP. Impaired biotin status in anticonvulsant therapy. Ann Neurol 12: 485–486, 1982 [DOI] [PubMed] [Google Scholar]
- 20. Krause KH, Bonjour JP, Berlit P, Kochen W. Biotin status of epileptics. Ann NY Acad Sci 447: 297–313, 1985 [DOI] [PubMed] [Google Scholar]
- 21. Lieber CS, DeCarli LM. The feeding of ethanol in liquid diets. Alcohol Clin Exp Res 10: 550–553, 1986 [DOI] [PubMed] [Google Scholar]
- 22. Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 25: 402–408, 2001 [DOI] [PubMed] [Google Scholar]
- 23. Ma TY, Dyer DL, Said HM. Human intestinal cell line Caco-2: a useful model for studying cellular and molecular regulation of biotin uptake. Biochim Biophys Acta 1189: 81–88, 1994 [DOI] [PubMed] [Google Scholar]
- 24. McMahon RJ. Biotin in metabolism and molecular biology. Annu Rev Nutr 22: 221–239, 2002 [DOI] [PubMed] [Google Scholar]
- 25. Mock D. Biotin: physiology, dietary sources and nutrients. In: Encyclopedia of Human Nutrition ( 2nd ed.), edited by Caballero B, Allen L, Prentice A. London: Academic, 2004, p. 201–209 [Google Scholar]
- 26. Mock DM, deLorimer AA, Liebman WM, Sweetman L, Baker H. Biotin deficiency: an unusual complication of parenteral alimentation. N Engl J Med 304: 820–823, 1981 [DOI] [PubMed] [Google Scholar]
- 27. Mock DM, Jackson H, Lankford GL, Mock NI, Weintraub ST. Quantification of urinary 3-hydroxyisovaleric acid using deuterated 3-hydroxyisovaleric acid as internal standard. Biomed Environ Mass Spectrom 18: 652–656, 1989 [DOI] [PubMed] [Google Scholar]
- 28. Mock DM, Quirk JG, Mock NI. Marginal biotin deficiency during normal pregnancy. Am J Clin Nutr 75: 295–299, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Nabokina SM, Reidling JC, Said HM. Differentiation-dependent up-regulation of intestinal thiamin uptake: cellular and molecular mechanisms. J Biol Chem 280: 32676–32682, 2005 [DOI] [PubMed] [Google Scholar]
- 30. Nabokina SM, Subramanian VS, Said HM. Comparative analysis of ontogenic changes in renal and intestinal biotin transport in the rat. Am J Physiol Renal Physiol 284: F737–F742, 2003 [DOI] [PubMed] [Google Scholar]
- 31. Nassir F, Wilson B, Han X, Gross RW, Abumrad NA. CD36 is important for fatty acid and cholesterol uptake by the proximal but not distal intestine. J Biol Chem 282: 19493–19501, 2007 [DOI] [PubMed] [Google Scholar]
- 32. Prasad PD, Wang H, Huang W, Fei YJ, Leibach FH, Devoe LD, Ganapathy V. Molecular and functional characterization of the intestinal Na+-dependent multivitamin transporter. Arch Biochem Biophys 366: 95–106, 1999 [DOI] [PubMed] [Google Scholar]
- 33. Prasad PD, Wang H, Kekuda R, Fujita T, Fei YJ, Devoe LD, Leibach FH, Ganapathy V. Cloning and functional expression of a cDNA encoding a mammalian sodium-dependent vitamin transporter mediating the uptake of pantothenate, biotin, and lipoate. J Biol Chem 273: 7501–7506, 1998 [DOI] [PubMed] [Google Scholar]
- 34. Rajendram R, Preedy VR. Effect of alcohol consumption on the gut. Dig Dis 23: 214–221, 2005 [DOI] [PubMed] [Google Scholar]
- 35. Reidling JC, Nabokina SM, Balamurugan K, Said HM. Developmental maturation of intestinal and renal thiamin uptake: studies in wild-type and transgenic mice carrying human THTR-1 and 2 promoters. J Cell Physiol 206: 371–377, 2006 [DOI] [PubMed] [Google Scholar]
- 36. Reidling JC, Nabokina SM, Said HM. Molecular mechanisms involved in the adaptive regulation of human intestinal biotin uptake: a study of the hSMVT system. Am J Physiol Gastrointest Liver Physiol 292: G275–G281, 2007 [DOI] [PubMed] [Google Scholar]
- 37. Reidling JC, Said HM. Regulation of the human biotin transporter hSMVT promoter by KLF-4 and AP-2: confirmation of promoter activity in vivo. Am J Physiol Cell Physiol 292: C1305–C1312, 2007 [DOI] [PubMed] [Google Scholar]
- 38. Rodriguez-Melendez R, Zempleni J. Regulation of gene expression by biotin (review). J Nutr Biochem 14: 680–690, 2003 [DOI] [PubMed] [Google Scholar]
- 39. Said HM, Ortiz A, McCloud E, Dyer D, Moyer MP, Rubin S. Biotin uptake by human colonic epithelial NCM460 cells: a carrier-mediated process shared with pantothenic acid. Am J Physiol Cell Physiol 275: C1365–C1371, 1998 [DOI] [PubMed] [Google Scholar]
- 40. Said HM, Redha R. Biotin transport in rat intestinal brush-border membrane vesicles. Biochim Biophys Acta 945: 195–201, 1988 [DOI] [PubMed] [Google Scholar]
- 41. Said HM, Redha R. A carrier-mediated system for transport of biotin in rat intestine in vitro. Am J Physiol Gastrointest Liver Physiol 252: G52–G55, 1987 [DOI] [PubMed] [Google Scholar]
- 42. Said HM, Redha R. A carrier-mediated transport for folate in basolateral membrane vesicles of rat small intestine. Biochem J 247: 141–146, 1987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Said HM, Redha R, Nylander W. Biotin transport in basolateral membrane vesicles of human intestine. Gastroenterology 94: 1157–1163, 1988 [DOI] [PubMed] [Google Scholar]
- 44. Said HM, Redha R, Nylander W. Biotin transport in the human intestine: inhibition by anticonvulsant drugs. Am J Clin Nutr 49: 127–131, 1989 [DOI] [PubMed] [Google Scholar]
- 45. Said HM, Redha R, Nylander W. A carrier-mediated, Na+ gradient-dependent transport for biotin in human intestinal brush-border membrane vesicles. Am J Physiol Gastrointest Liver Physiol 253: G631–G636, 1987 [DOI] [PubMed] [Google Scholar]
- 46. Said HM, Sharifian A, Bagherzadeh A, Mock D. Chronic ethanol feeding and acute ethanol exposure in vitro: effect on intestinal transport of biotin. Am J Clin Nutr 52: 1083–1086, 1990 [DOI] [PubMed] [Google Scholar]
- 47. Salaspuro M. Bacteriocolonic pathway for ethanol oxidation: characteristics and implications. Ann Med 28: 195–200, 1996 [DOI] [PubMed] [Google Scholar]
- 48. Scalera V, Storelli C, Storelli-Joss C, Haase W, Murer H. A simple and fast method for the isolation of basolateral plasma membranes from rat small-intestinal epithelial cells. Biochem J 186: 177–181, 1980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Subramanian VS, Marchant JS, Boulware MJ, Ma TY, Said HM. Membrane targeting and intracellular trafficking of the human sodium-dependent multivitamin transporter in polarized epithelial cells. Am J Physiol Cell Physiol 296: C663–C671, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Subramanya SB, Subramanian VS, Said HM. Chronic alcohol consumption and intestinal thiamin absorption: effects on physiological and molecular parameters of the uptake process. Am J Physiol Gastrointest Liver Physiol 299: G23–G31, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Sweetman L, Nyhan WL. Inheritable biotin-treatable disorders and associated phenomena. Annu Rev Nutr 6: 317–343, 1986 [DOI] [PubMed] [Google Scholar]
- 52. Wolf B. Disorders of biotin metabolism. In: The Metabolic and Molecular Bases of Inherited Disease, edited by Scriver CR, Beaudet AL, Aly WS, Valle D, Childs B, Kinzler KW, Vogelstein B. New York: McGraw-Hill Medical, 2001, p. 3935–3962 [Google Scholar]
- 53. Wong OM, Edmonds CJ, Chadwick VS. The large intestine: its role in mammalian nutrition and homeostasis. New York: Wiley, 1981, p. 157–166 [Google Scholar]
- 54. You M, Liang X, Ajmo JM, Ness GC. Involvement of mammalian sirtuin 1 in the action of ethanol in the liver. Am J Physiol Gastrointest Liver Physiol 294: G892–G898, 2008 [DOI] [PubMed] [Google Scholar]