Abstract
Background
Social isolation is associated with progression of cardiovascular disease with the most socially isolated patients being at increased risk. Increased left ventricular mass is a predictor of cardiovascular morbidity and mortality. It is not yet clear whether social isolation is a determinant of increased left ventricular mass.
Methods
We performed a cross-sectional study of Northern Manhattan Study participants who were free of clinical cardiovascular disease, had obtained transthoracic echocardiograms (n=2021) and a baseline questionnaire on social habits. Social isolation was defined as the lack of friendship networks (knowing fewer than 3 people well enough to visit within their homes). Echocardiographic left ventricular mass was indexed to height2.7, analyzed as a continuous variable and compared between exposure groups.
Results
The prevalence of social isolation was 13.5%. The average left ventricular mass was significantly higher (50.2 gm/m2.7) in those who were, as compared to those who were not (47.6 gm/m2.7), socially isolated (p<0.05). Higher prevalence of social isolation was found among those less educated, uninsured or unemployed.There were no significant race-ethnic differences in the prevalence of social isolation. In multivariate analysis, there was a trend toward an association between social isolation and increased left ventricular mass in the total cohort (p=0.09). Among Hispanics, social isolation was significantly associated with greater left ventricular mass. Hispanics who were socially isolated averaged 3.9 gm/ht2.7 higher left ventricular mass compared to those not socially isolated (p=0.002). This relationship was not present among non-Hispanic blacks or whites.
Conclusion
In this urban tri-ethnic cohort, social isolation was prevalent and associated with indices of low socioeconomic status. Hispanics who were socially isolated had a greater risk for increased left ventricular mass.
Keywords: social isolation, left ventricular mass, Hispanics, psychosocial factors
Epidemiological data have shown that echocardiographic left ventricular hypertrophy as defined by increased left ventricular mass, is an independent predictor of morbidity and mortality from cardiovascular disease.1, 2 Blacks and Hispanics are known to have a higher average left ventricular mass than whites,3, 4. These associations are independent of arterial hypertension, diabetes mellitus, and other traditional cardiovascular risk factors. Underlying psychosocial factors, either emotional factors such as hostility and anger, or chronic stressors such as low social support, may contribute to the differential burden of increased left ventricular mass seen in various race-ethnic groups.5
Within the past few years, there has been renewed interest in social isolation and its relationship to cardiovascular health and well-being.6 The hypothesis that health can be affected by supportive interactions with individuals within one’s social network has now been strengthened by evidence on the relationship between measures of social support and morbidity as well as all-cause mortality.7–10 Studies of social environment and cardiovascular disease risk suggest that the most socially isolated patients are at increased risk of cardiovascular disease.11 Race likely has a broad impact on social networks in American society. Non-Hispanic blacks have smaller networks of confidants and markedly smaller friendship networks than non-Hispanic whites,12, 13 with much less known about Hispanics in this regard.
Although not completely understood, the mediating mechanisms are hypothesized to involve both health behaviors and neuroendocrine pathways. Examples of influences on health behaviors include a positive association between social support and exercise, and significant inverse associations with smoking.9, 10 Sympathetic stimulation has been shown to vary with exposure to stressful environments in the workplace and at home.14, 15 Studies indicate that low social support may be related to blood pressure reactivity.16 7 It is possible that more socially isolated individuals have blood pressure responses to stress that are larger and more prolonged, in the absence of the buffering effects of social support during a stressor 17, thereby experiencing more frequent sympathetic activation. Chronic or even intermittent adrenergic stimulation, even in the absence of overt hypertension, can cause increased left ventricular mass.18–20
The relationship between social isolation and increased left ventricular mass, however, has not been elucidated in multiethnic cohorts inclusive of Hispanics. We performed a cross-sectional study hypothesizing that social isolation will be associated with increased left ventricular mass and that this relationship would vary by race-ethnicity.
Methods
Study population
The Northern Manhattan Study (NOMAS) is a population-based prospective cohort study of stroke-free individuals designed to investigate cardiovascular and stroke risk factors and prognosis in a multi-ethnic urban population of the northern Manhattan (New York) area. The methods of subject recruitment and enrollment into NOMAS have been described previously.4, 21, 22 Briefly, community subjects from northern Manhattan were eligible if they (1) had never been diagnosed with a stroke, (2) were ≥ 40 years of age, and (3) resided in northern Manhattan for at least 3 months in a household with a telephone. Stroke-free subjects were identified by random digit dialing. Of those called, 90% participated in a telephone interview used for screening and recruiting participants, and 75% of those who were eligible and invited to participate came to Columbia University Medical Center (CUMC) for an in-person evaluation during which all demographic and social resource information was obtained. The study was approved by the Institutional Review Boards at CUMC and the University of Miami, and all participants gave written informed consent. Participants who were free of clinical cardiovascular disease (defined as having a history of bypass surgery, angioplasty, or myocardial infarction) and received technically adequate transthoracic echocardiograms (n=2021) completed a baseline questionnaire on social resource information.
Information about risk factors was collected through standardized in-person interviews by trained research assistants, and physical examinations were performed by study physicians. Blood pressure (BP) was measured with mercury sphygmomanometers and cuffs of appropriate site. Hypertension was defined as a BP recording ≥140/90 mmHg (based on an average of two BP measurements during one sitting by a trained research assistant), the participant’s self-report of a history of hypertension, or antihypertensive medication use. Diabetes mellitus was defined by the participant’s self-report of such a history, use of insulin or hypoglycemic agent, or fasting glucose ≥ 126mg/dL. Height and weight were determined by the use of calibrated scales. Assessments were conducted in English or Spanish, depending on the primary language of the participant. Race-ethnicity was based on self-identification through a series of questions modeled after the 2000 US census, and conformed to the standard definitions outlined by Directive 15. Current smoking was defined by smoking within the past year. The measures of physical activity have been previously described.23 In brief, questionnaires administered were used to record the frequency and duration of different recreational activities during the 2-week period before the interview. For our analysis, we evaluated either the presence/absence of physical activity and the presence/absence of current smoking.
Social Isolation
Social isolation, our primary exposure of interest, was defined and assessed as previously described in NOMAS.24 Briefly, we assessed social isolation according to response to the question “How many people do you know well enough to visit with in their homes.” Ordinal response categories were 1=none, 2=one or two, 3=three or four, or 4=five or more. Social isolation was defined as lack of friendship networks dichotomized as knowing fewer than three people well enough to visit with in their homes. Thus, we focused on the presence and structure (number of friends) related to these friendship networks rather than the perceived effects or quality of such networks. NOMAS social isolation questions regarding the presence and size of friendship networks were adapted from the Berkman Social Network Index25 and have been associated with vascular risk factors and outcomes.22, 26
Other social/economic resources included marital status, years of education, and health insurance type. Education was further dichotomized into those who had completed high school versus those who had not. Mutually exclusive insurance categories were defined as no insurance, private insurance, Medicare only, and Medicaid/Medicare.
Echocardiographic left ventricular mass
Transthoracic 2-dimensional echocardiography was performed according to the recommendations of the American Society of Echocardiography (ASE).27 left ventricular mass was calculated according to the simplified ASE formula28:
Since the ASE left ventricular mass overestimates autopsy left ventricular mass by 20%, the modified ASE formula proposed by Devereux, et al.29 was applied: left ventricular mass = 0.8 (ASE left ventricular mass) + 0.6.
Left ventricular mass was then indexed to body size by dividing raw left ventricular mass by height to the allometric power of 2.7 and analyzed as a continuous variable.
Statistical analyses
Distributions of risk factors were compared for the entire cohort and across each race-ethnic group using Chi-square for categorical variables and ANOVA for continuous variables. Categorical variables are expressed as frequencies and percentages. The relationship between left ventricular mass and baseline characteristics and social isolation was assessed using linear regression models. Regression models are reported unadjusted and adjusted for classical risk factors for increased left ventricular mass including age, sex, body mass index (BMI), diabetes, physical activity, hypertension, and education level. One-way analysis of variance was used to test differences among group left ventricular mass means. To address any potential issue with outliers, we used a robust analysis approach employing median regression. To investigate the potential effect of race-ethnicity on the relationship between social isolation and left ventricular mass, interaction terms were included for Hispanics, blacks, and whites and for Hispanic vs. non-Hispanics.
Results
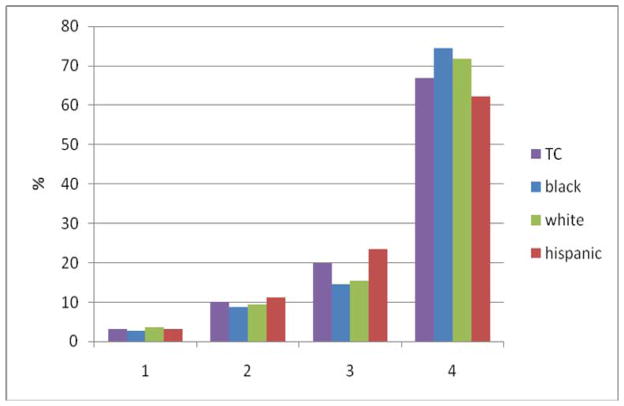
Table 1 describes the demographic characteristics and social resources of our cohort. Participants were primarily elderly, hypertensive, overweight, mostly uninsured, and with little education. There was a 13.5% prevalence of social isolation. Those socially isolated were significantly older, less educated, tended to be less insured or on Medicaid, and more likely to be unemployed or retired. There was a non-significant trend that those married tended to be less socially isolated. Details regarding the number of friends reported by participants is shown in Figure 1 for the total cohort and according to race-ethnic status. There were no significant race-ethnic differences in the prevalence of social isolation.
Table 1.
Baseline Characteristics*
| Percentage/Mean ± SD | Not Social Isolated n=1750 | Socially Isolated n=271 | P value |
|---|---|---|---|
| Age | 67.7 ± 9.5 | 69.6 ± 10.4 | 0.004 |
| Race-Ethnicity: | 22.4 | 18.8 | 0.36 |
| Black | |||
| Hispanic | 56.9 | 60.9 | |
| White | 20.7 | 20.3 | |
| Women | 60.5 | 61.3 | 0.80 |
| Diabetes Status | 21.5 | 25.5 | 0.14 |
| Hypertension Status | 67.8 | 70.9 | 0.32 |
| Current Smoker | 16.3 | 20.3 | 0.10 |
| Physical Activity | 58.8 | 50.2 | 0.008 |
| BMI (kg/m2) | 27.7 ± 5.3 | 27.6 ± 5.9 | 0.86 |
| Left Ventricular Mass (gm/ht2.7) | 47.7 ± 15.5 | 50.2 ± 18.7 | 0.03 |
| Married | 35.8 | 29.9 | 0.057 |
| Education ≥HS | 47.3 | 36.9 | 0.001 |
| Unemployed (or Retired) | 77.5 | 88.6 | <0.0001 |
| Unskilled Labor | 39.5 | 46.1 | 0.03 |
| Insurance Status: | 45.4 | 60.7 | <0.0001 |
| Medicaid/Medicare | |||
| Uninsured | 12.5 | 12.6 | |
| Private | 42.1 | 26.9 | |
BMI (n-2018) and current smoking status (n-1993) were the only baseline characteristics with missing values.
Figure 1. Proportion of Participants according to Number of Friends in Social Network by Race.
How many people do you know well enough to visit with in their homes?
1 = None
2 = one or two
3 = three or four
4 = five or more
In unadjusted analyses, mean left ventricular mass was higher among those socially isolated (50.2 ± 18.7 gm/m2. 7 among those with social isolation vs. 47.6 ± 15.5 gm/m2. 7 among those not isolated; unadjusted p=0.03). Table 2 shows social isolation was a univariate predictor of left ventricular mass on graded continuous analysis. Being married showed an inverse relation with left ventricular mass on univariate analysis. There was, however, no significant association between the number of friends and marital status (p=0.16).
Table 2.
Univariate Regression Analysis of Factors Associated with Left Ventricular Mass
| Regression Coefficient (β)† | SE | P value | |
|---|---|---|---|
| Social isolation | 2.56 | 1.04 | 0.01 |
| Age (per year) | 0.22 | 0.04 | <0.001 |
| Male Sex | −0.83 | 0.73 | 0.26 |
| BMI (per kg/m2) | 0.95 | 0.06 | <.0001 |
| Diabetes Status | 3.57 | 0.85 | <.0001 |
| Physical Activity | −0.10 | 0.10 | 0.31 |
| Hypertension Status | 7.40 | 0.75 | <.0001 |
| SBP (per mm Hg) | 0.19 | 0.02 | <.0001 |
| Hispanic§ | 3.67 | 0.91 | <.0001 |
| Black§ | 3.61 | 1.08 | 0.0009 |
| Current Smoking | 0.30 | 0.96 | 0.75 |
| Education ≥HS | −2.58 | 0.71 | 0.0003 |
| Marriage | −1.77 | 0.74 | 0.02 |
β reflects the change in left ventricular mass (gm/ht2.7) associated with a change in one unit of left ventricular mass determinants, e.g.- For each unit increase in age (1 year) there is an average 0.22 gm/ht2.7 increase in left ventricular mass.
compared with non-Hispanic Whites
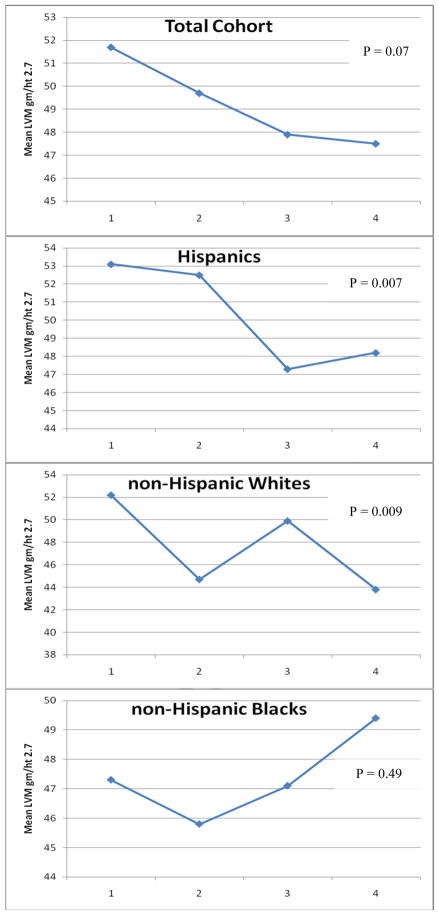
Figure 2 shows that, for the total cohort, those most socially isolated had on average 4.1 gm/m2.7 higher left ventricular mass than those with the least degree of isolation. In fully adjusted models (Table 3), social isolation showed a non-significant trend for predicting increased left ventricular mass in the total cohort. A social isolation*race interaction was seen (p=0.004) when strata compared Hispanics versus non-Hispanics. Table 3 shows that among Hispanics, left ventricular mass averaged 3.9 gm/m2.7 higher among the more socially isolated Hispanics versus those not socially isolated (p=0.002). This relationship was not present among non-Hispanic whites, and there was a non-significant trend towards an inverse relationship among non-Hispanic blacks. Among the total cohort, Hispanics, non-Hispanic blacks and non-Hispanic whites, 17%, 15%, 21% and 15% of the variance in left ventricular mass respectively, was explained by our multivariate model. When mean left ventricular mass was analyzed as a function of the number of friends in a person’s social network (Figure 2), a graded significant inverse relationship was seen among Hispanics; among non-Hispanic whites, the relationship was most significant among the two extremes (those most socially isolated versus those with the least degree of social isolation); among non-Hispanic blacks a non-significant direct relationship was seen. The β coefficient for social isolation in univariate median regression was 1.91 (SE=1.12, p=0.09) and remained non-significant in multivariate median regression (p=0.22).
Figure 2. Mean left ventricular mass according to Number of Friends in Social Network by Race.
How many people do you know well enough to visit with in their homes?
1 = None
2 = one or two
3 = three or four
4 = five or more
Table 3.
Multivariate Regression Analysis of Factors Associated with Left Ventricular Mass
| Regression Coefficient (β)† | SE | P value | |
|---|---|---|---|
| Social isolation | 1.65 | 0.96 | 0.09 |
| Age (per year) | 0.32 | 0.04 | <0.0001 |
| Male Sex | 1.36 | 0.68 | 0.05 |
| BMI (per kg/m2) | 0.99 | 0.06 | <0.0001 |
| Diabetes Status | 1.05 | 0.80 | 0.19 |
| Hypertension Status | 4.2 | 0.73 | <0.0001 |
| Education ≥HS | −1.43 | 0.67 | 0.03 |
| Physical Activity | −0.67 | 0.67 | 0.32 |
| Stratified by Race-ethnicity¶ | |||
| Hispanics n=1162 | 3.9 | 1.23 | 0.002 |
| Blacks n=443 | −4.3 | 2.3 | 0.06 |
| Whites n=418 | 0.17 | 2.07 | 0.94 |
β reflects the change in left ventricular mass (gm/ht2.7) associated with a change in one unit of left ventricular mass determinants, e.g.- For each unit increase in age (1 year) there is an average 0.32 gm/ht2.7 increase in left ventricular mass.
Adjusted for age, sex, BMI, physical activity, hypertensive status, educational level, and diabetes
Discussion
A linear relationship between social support and health status has been well documented. 11, 30–32 Social isolation has been shown to prospectively predict mortality and serious morbidity both in general population samples33, 34 and in individuals with established morbidity35, especially coronary heart disease36. However, our understanding of how and why social isolation is risky for health or, conversely, how and why social ties and relationships are protective of health, still remains quite limited. Our data support a possible role for social isolation as a factor influencing left ventricular mass. It is possible that subclinical cardiovascular disease such as increased left ventricular mass may be a mediating mechanism or modifying factor in the pathway by which a lack of social networks contribute to cardiovascular morbidity and mortality but ours was not a prospective study. Our multivariate model controlled for standard cardiac risk factors, and such factors do not fully account for or explain the deleterious effects of social isolation on left ventricular mass among Hispanics.
Social isolation may be related to left ventricular mass through a number of underlying mechanisms including psycho-physiologic stress related to isolation, depression, and poorer regulation of risk factors due to decreased medication compliance and decreased participation in healthful activities. Poor social friendship networks may turn off the means of obtaining health-related information 37 and enhance health risk behaviors. 9, 38, 39 Poor social support may lead to increased left ventricular mass via mental stress that is not buffered by the supportive presence of others. Mental stress activates neuro-endocrine components including the hypothalamic-pituitary-adrenal-axis and autonomic nervous system 11 Mental stress may induce hypertension40, and increase cardiovascular reactivity41 and endothelial dysfunction 42, all of which lead to increased left ventricular mass. The deleterious effects of social isolation are likely multifactorial. Further study is warranted to test these hypotheses.
Our definition of social isolation represents the presence of a primary, informal network that incorporates friends or friend-neighbors. This type of primary support network would most likely be associated with tasks involving leisure activities, hobbies, companionship, community events, shopping, and perhaps religious services. Hence, lack of friendship networks may provide a mechanism for lack of access to a wide range of resources supportive of health, such as medical referral networks, access to others dealing with similar problems, or opportunities to acquire needed resources via jobs, shopping, or financial institutions.
The spouse/partner constitutes another type of primary support network that has been associated with decreased mortality, particularly among men.43 Indeed the proximity of friend networks may also take on a more prominent role in those who have lost a spouse. In our cohort, age was also associated with poorer social support as those socially isolated were older and had increased left ventricular mass. Social isolation tended to correlate with measures of low socioeconomic status. Although educational level, our most robust socioeconomic status measure, remained significant for the total cohort in our multivariate models, it was not significant among any of the race-ethnic groups (all p>0.20) when social isolation was also in the model. Socioeconomic status has been shown to be a determinant of left ventricular mass.4 It is possible that social isolation is a partial mediator of the relationship between socioeconomic status and left ventricular mass but this remains to be further studied.
Although the prevalence of social isolation was not significantly different among the race-ethnic groups, social isolation was associated with increased left ventricular mass among Hispanics but not in the other race-ethnic groups. Our analyses suggest that race-ethnicity may be a proxy for differences in the strength of social resources. Indeed, the strong social support systems among Hispanics who are poor but maintain traditional kin groupings24 may account for the lower mean left ventricular mass in the not socially isolated group. Hispanics may be more likely to stress family values over educational attainment: maintaining traditional kinship values that include living in extended family units and taking care of the sick and elderly. This is expressed in the core Hispanic belief of familism. Familism is having strong bonds with nuclear and extended family members thus extending a high level of perceived family support. Most studies on familism suggest that it has salutary effects and may explain the better-than-expected health outcomes observed in Hispanics.44 For example, family members are often a source of financial and emotional support which can facilitate access to health services,45 and better prevention practices including medical adherence.46, 47 Non-Hispanic blacks typically have not retained traditional kin norms. Despite levels of poverty similar to Hispanics, the elimination of traditional norms among non-Hispanic blacks has likely resulted in population level stresses, isolation of family values, and mistrust of both medical and other community resources. It may be that familism enhances the social friendship network among Hispanics in a manner that is not found in other race-ethnic groups studied.
That there was a non-significant trend towards an inverse relationship of social isolation with left ventricular mass among non-Hispanic blacks was surprising in light of the evidence that social support is beneficial in reducing stress among non-Hispanic blacks.48 However, prior studies used a different assessment tool to determine social isolation which may account for the different results. Alternatively, it our results may suggest that a more extensive social network is burdensome among non-Hispanic blacks for unclear reasons. The standard error of the regression coefficient for non-Hispanic blacks was the largest among the race-ethnic groups, likely the result of the limited number of non-Hispanic blacks in our cohort. The β coefficient for social isolation was non-significant in univariate or multivariate median regression which argues against outliers influencing the relation seen between social isolation and LVM among non-Hispanic blacks.
As for the relationship among non-Hispanic whites, although having no friends is clearly worse than having the highest number of friends, there is no significant trend seen. It seems as if among non-Hispanic whites, LVM has a non-linear relationship with social isolation. However, there is no way we could either prove or disprove this because the number of friends were categorized as ordinal variables. It is possible that what matters is not so much increasing isolation but a shift in the form and type of social connection. This will require further study.
Study Strengths and Limitations
A major strength of these analyses includes the use of a community based multiethnic cohort. Limitations of the study with regard to social support include the inability to capture individual participation in religious activities, senior centers, and other community-based organizations. Further, the data collected are limited in their ability to characterize the mechanisms by which social isolation impacts on left ventricular mass. Our study was cross-sectional in nature and thus causality cannot be inferred nor temporality be established. Unmeasured variables and residual confounding may account for some of the observed differences. Our interaction term was only significant when looking at Hispanics vs. non-Hispanics and not significant (p>0.20) when looking at Hispanics, whites, and blacks separately. Because of the limited number of participants in non-Hispanic race-ethnic groups and a power issue within each strata, our study was underpowered to detect statistically significant small to moderate interactions. Using values for mean left ventricular mass in those with and without social isolation and a two-sided type-I error of 0.05, the current sample had only 55% power to detect the 2.5 gm/m2.7 difference in left ventricular mass and would have much less power for within-strata analysis. Nevertheless, socially isolated Hispanics were at a significantly higher risk of increased left ventricular mass than the other groups. Lastly, our findings may not be generalizable to all Hispanics; 88% of our Hispanic sample consists of Caribbean-Hispanics from the Dominican Republic, Cuba, and Puerto Rico. Confirmation by other investigators using other Hispanic populations is required.
Conclusion
Our findings suggests that it may be important to try to ensure that all individuals, especially elderly individuals, have social ties with at least one or a few other individuals. This may mean the need to develop both individual and population level strategies to identify individuals who are likely to be socially isolated. One such strategy is systematic screening by health care providers into the social components of the patient’s lifestyle with recommendations to become more involved in community type activities. From a public health perspective, increased funding for community organizations to promote programs in which people get together and share common interests may be needed to reduce social isolation and ultimately help reduce or prevent increased left ventricular mass and possibly subsequent cardiovascular disease.
Acknowledgments
Funding Sources: RLS, MSV (R01 NS29993) and MDT (K24 NS02241) are supported by the National Institute of Neurological Disorders and Stroke. CJR is supported by the Robert Wood Johnson Foundation Harold Amos Medical Faculty Development Award, and a National Heart, Lung, and Blood Institute Mentored Research Career Development Award (K23 HL079343-01A2).
Footnotes
The authors had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All of the authors meet criteria for authorship, including acceptance of responsibility for the scientific content of the manuscript.
Disclosures: The authors report no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP. Prognostic Implications of Echocardiographically Determined Left Ventricular Mass in the Framingham Heart Study. N Engl J Med. 1990;322:1561–6. doi: 10.1056/NEJM199005313222203. [DOI] [PubMed] [Google Scholar]
- 2.Liao Y, Cooper RS, McGee DL, Mensah GA, Ghali JK. The Relative Effects of Left Ventricular Hypertrophy, Coronary Artery Disease, and Ventricular Dysfunction on Survival among Black Adults. JAMA. 1995;273:1592–7. [PubMed] [Google Scholar]
- 3.Koren MJ, Mensah GA, Blake J, Laragh JH, Devereux RB. Comparison of Left Ventricular Mass and Geometry in Black and White Patients with Essential Hypertension. Am J Hypertens. 1993;6:815–23. doi: 10.1093/ajh/6.10.815. [DOI] [PubMed] [Google Scholar]
- 4.Rodriguez CJ, Sciacca RR, Diez-Roux AV, et al. Relation between Socioeconomic Status, Race-Ethnicity, and Left Ventricular Mass: The Northern Manhattan Study. Hypertension. 2004;43:775–9. doi: 10.1161/01.HYP.0000118055.90533.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shumaker SA, Czajkowski SM. Social Support and Cardiovascular Disease. 1994. [Google Scholar]
- 6.Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The Epidemiology, Pathophysiology, and Management of Psychosocial Risk Factors in Cardiac Practice: The Emerging Field of Behavioral Cardiology. J Am Coll Cardiol. 2005;45:637–51. doi: 10.1016/j.jacc.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 7.Knox SS, Adelman A, Ellison RC, et al. Hostility, Social Support, and Carotid Artery Atherosclerosis in the National Heart, Lung, and Blood Institute Family Heart Study. Am J Cardiol. 2000;86:1086–9. doi: 10.1016/s0002-9149(00)01164-4. [DOI] [PubMed] [Google Scholar]
- 8.Knox SS. Perception of Social Support and Blood Pressure in Young Men. Percept Mot Skills. 1993;77:132–4. doi: 10.2466/pms.1993.77.1.132. [DOI] [PubMed] [Google Scholar]
- 9.Treiber FA, Baranowski T, Braden DS, Strong WB, Levy M, Knox W. Social Support for Exercise: Relationship to Physical Activity in Young Adults. Prev Med. 1991;20:737–50. doi: 10.1016/0091-7435(91)90068-f. [DOI] [PubMed] [Google Scholar]
- 10.Romano PS, Bloom J, Syme SL. Smoking, Social Support, and Hassles in an Urban African-American Community. Am J Public Health. 1991;81:1415–22. doi: 10.2105/ajph.81.11.1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Knox SS, Uvnas-Moberg K. Social Isolation and Cardiovascular Disease: An Atherosclerotic Pathway? Psychoneuroendocrinology. 1998;23:877–90. doi: 10.1016/s0306-4530(98)00061-4. [DOI] [PubMed] [Google Scholar]
- 12.Tigges LM, Browne I, Green GP. Social Isolation of the Urban Poor: Race, Class, and Neighborhood Effects on Social Resources. The Sociological Quarterly. 2008;39:53–7. [Google Scholar]
- 13.McPherson M, Smith-Lovin L, MEB Social Isolation in America. American Sociological Review. 2006;71:353–75. [Google Scholar]
- 14.Everson SA, Lynch JW, Kaplan GA, Lakka TA, Sivenius J, Salonen JT. Stress-Induced Blood Pressure Reactivity and Incident Stroke in Middle-Aged Men. Stroke. 2001;32:1263–70. doi: 10.1161/01.str.32.6.1263. [DOI] [PubMed] [Google Scholar]
- 15.Lynch JW, Everson SA, Kaplan GA, Salonen R, Salonen JT. Does Low Socioeconomic Status Potentiate the Effects of Heightened Cardiovascular Responses to Stress on the Progression of Carotid Atherosclerosis? Am J Public Health. 1998;88:389–94. doi: 10.2105/ajph.88.3.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clark R. Self-Reported Racism and Social Support Predict Blood Pressure Reactivity in Blacks. Ann Behav Med. 2003;25:127–36. doi: 10.1207/S15324796ABM2502_09. [DOI] [PubMed] [Google Scholar]
- 17.Glynn LM, Christenfeld N, Gerin W. Gender, Social Support, and Cardiovascular Responses to Stress. Psychosom Med. 1999;61:234–42. doi: 10.1097/00006842-199903000-00016. [DOI] [PubMed] [Google Scholar]
- 18.Gump BB, Matthews KA, Raikkonen K. Modeling Relationships among Socioeconomic Status, Hostility, Cardiovascular Reactivity, and Left Ventricular Mass in African American and White Children. Health Psychol. 1999;18:140–50. doi: 10.1037//0278-6133.18.2.140. [DOI] [PubMed] [Google Scholar]
- 19.Rapaport E. Pathophysiological Basis of Ventricular Hypertrophy. Eur Heart J. 1982;3 (Suppl A):29–33. doi: 10.1093/eurheartj/3.suppl_a.29. [DOI] [PubMed] [Google Scholar]
- 20.Post WS, Larson MG, Levy D. Impact of Left Ventricular Structure on the Incidence of Hypertension. The Framingham Heart Study. Circulation. 1994;90:179–85. doi: 10.1161/01.cir.90.1.179. [DOI] [PubMed] [Google Scholar]
- 21.Boden-Albala B, Sacco RL. Annals of Epidemiology. 2004. Socio-Cultural Determinants of Stroke in a Multiethnic Community: Findings from the Northern Manhattan Stroke Study. [Google Scholar]
- 22.Willey JZ, Williams O, Boden-Albala B. Stroke Literacy in Central Harlem: A High-Risk Stroke Population. Neurology. 2009;73:1950–6. doi: 10.1212/WNL.0b013e3181c51a7d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Willey JZ, Moon YP, Paik MC, Boden-Albala B, Sacco RL, Elkind MS. Physical Activity and Risk of Ischemic Stroke in the Northern Manhattan Study. Neurology. 2009;73:1774–9. doi: 10.1212/WNL.0b013e3181c34b58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boden-Albala B, Litwak E, Elkind MS, Rundek T, Sacco RL. Social Isolation and Outcomes Post Stroke. Neurology. 2005;64:1888–92. doi: 10.1212/01.WNL.0000163510.79351.AF. [DOI] [PubMed] [Google Scholar]
- 25.Berkman LF, Syme SL. Social Networks, Host Resistance, and Mortality: A Nine-Year Follow-up Study of Alameda County Residents. Am J Epidemiol. 1979;109:186–204. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- 26.Boden-Albala B, Sacco RL. Socioeconomic Status and Stroke Mortality: Refining the Relationship. Stroke. 2002;33:274–5. [PubMed] [Google Scholar]
- 27.Lang RM, Bierig M, Devereux RB, et al. Recommendations for Chamber Quantification: A Report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, Developed in Conjunction with the European Association of Echocardiography, a Branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–63. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 28.Park SH, Shub C, Nobrega TP, Bailey KR, Seward JB. Two-Dimensional Echocardiographic Calculation of Left Ventricular Mass as Recommended by the American Society of Echocardiography: Correlation with Autopsy and M-Mode Echocardiography. J Am Soc Echocardiogr. 1996;9:119–28. doi: 10.1016/s0894-7317(96)90019-x. [DOI] [PubMed] [Google Scholar]
- 29.Park SH, Shub C, Nobrega TP, Bailey KR, Seward JB. Two-Dimensional Echocardiographic Calculation of Left Ventricular Mass as Recommended by the American Society of Echocardiography: Correlation with Autopsy and M-Mode Echocardiography. J Am SocEchocardiogr. 1996;9:119–28. doi: 10.1016/s0894-7317(96)90019-x. [DOI] [PubMed] [Google Scholar]
- 30.Orth-Gomer K, Rosengren A, Wilhelmsen L. Lack of Social Support and Incidence of Coronary Heart Disease in Middle-Aged Swedish Men. Psychosom Med. 1993;55:37–43. doi: 10.1097/00006842-199301000-00007. [DOI] [PubMed] [Google Scholar]
- 31.Michael YL, Colditz GA, Coakley E, Kawachi I. Health Behaviors, Social Networks, and Healthy Aging: Cross-Sectional Evidence from the Nurses’ Health Study. Qual Life Res. 1999;8:711–22. doi: 10.1023/a:1008949428041. [DOI] [PubMed] [Google Scholar]
- 32.Vogt TM, Mullooly JP, Ernst D, Pope CR, Hollis JF. Social Networks as Predictors of Ischemic Heart Disease, Cancer, Stroke and Hypertension: Incidence, Survival and Mortality. J Clin Epidemiol. 1992;45:659–66. doi: 10.1016/0895-4356(92)90138-d. [DOI] [PubMed] [Google Scholar]
- 33.House JS, Landis KR, Umberson D. Social Relationships and Health. Science. 1988;241:540–5. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 34.Rosengren A, Wilhelmsen L, Orth-Gomer K. Coronary Disease in Relation to Social Support and Social Class in Swedish Men. A 15 Year Follow-up in the Study of Men Born in 1933. Eur Heart J. 2004;25:56–63. doi: 10.1016/j.ehj.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 35.House JS, Robbins C, Metzner HL. The Association of Social Relationships and Activities with Mortality: Prospective Evidence from the Tecumseh Community Health Study. Am J Epidemiol. 1982;116:123–40. doi: 10.1093/oxfordjournals.aje.a113387. [DOI] [PubMed] [Google Scholar]
- 36.Brummett BH, Barefoot JC, Siegler IC, et al. Characteristics of Socially Isolated Patients with Coronary Artery Disease Who Are at Elevated Risk for Mortality. Psychosom Med. 2001;63:267–72. doi: 10.1097/00006842-200103000-00010. [DOI] [PubMed] [Google Scholar]
- 37.Kawachi I, Colditz GA, Ascherio A, et al. A Prospective Study of Social Networks in Relation to Total Mortality and Cardiovascular Disease in Men in the USA. J Epidemiol Community Health. 1996;50:245–51. doi: 10.1136/jech.50.3.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Broman CL. Social Relationships and Health-Related Behavior. J Behav Med. 1993;16:335–50. doi: 10.1007/BF00844776. [DOI] [PubMed] [Google Scholar]
- 39.Hanson BS, Isacsson SO, Janzon L, Lindell SE. Social Support and Quitting Smoking for Good. Is There an Association? Results from the Population Study, “Men Born in 1914,” Malmo, Sweden. Addict Behav. 1990;15:221–33. doi: 10.1016/0306-4603(90)90065-6. [DOI] [PubMed] [Google Scholar]
- 40.Wirtz PH, von Kanel R, Mohiyeddini C, et al. Low Social Support and Poor Emotional Regulation Are Associated with Increased Stress Hormone Reactivity to Mental Stress in Systemic Hypertension. J Clin Endocrinol Metab. 2006;91:3857–65. doi: 10.1210/jc.2005-2586. [DOI] [PubMed] [Google Scholar]
- 41.Kamarck TW, Manuck SB, Jennings JR. Social Support Reduces Cardiovascular Reactivity to Psychological Challenge: A Laboratory Model. Psychosom Med. 1990;52:42–58. doi: 10.1097/00006842-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 42.Ghiadoni L, Donald AE, Cropley M, et al. Mental Stress Induces Transient Endothelial Dysfunction in Humans. Circulation. 2000;102:2473–8. doi: 10.1161/01.cir.102.20.2473. [DOI] [PubMed] [Google Scholar]
- 43.Waite LJ. Does Marriage Matter? Demography. 1995;32:483–507. [PubMed] [Google Scholar]
- 44.Uchino BN, Cacioppo JT, Kiecolt-Glaser JK. The Relationship between Social Support and Physiological Processes: A Review with Emphasis on Underlying Mechanisms and Implications for Health. Psychol Bull. 1996;119:488–531. doi: 10.1037/0033-2909.119.3.488. [DOI] [PubMed] [Google Scholar]
- 45.Sherraden MS, Barrera RE. Prenatal Care Experiences and Birth Weight among Mexican Immigrant Women. J Med Syst. 1996;20:329–50. doi: 10.1007/BF02257044. [DOI] [PubMed] [Google Scholar]
- 46.Suarez L. Pap Smear and Mammogram Screening in Mexican-American Women: The Effects of Acculturation. Am J Public Health. 1994;84:742–6. doi: 10.2105/ajph.84.5.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Abraido-Lanza AF, Guier C, Revenson TA. Coping and Social Support Resources among Latinas with Arthritis. Arthritis Care Res. 1996;9:501–8. doi: 10.1002/art.1790090612. [DOI] [PubMed] [Google Scholar]
- 48.Rodriguez CJ, Burg MM, Meng J, et al. Effect of Social Support on Nocturnal Blood Pressure Dipping. Psychosom Med. 2008;70:7–12. doi: 10.1097/PSY.0b013e31815aab4e. [DOI] [PubMed] [Google Scholar]