Abstract
Background
The influence of health beliefs on human papillomavirus (HPV) vaccine acceptability have been extensively documented in past research. However, studies documenting the generalizability of prior findings to culturally diverse participants are lacking. The importance of generalizability studies is underscored by the immense disparities in cervical cancer rates across ethnicities. Moreover, theory in cultural psychology suggests that beliefs derived from personal expectations may not be the strongest predictors of intentions in individuals socialized in collectivist cultures. The purpose of this research was to investigate the strongest predictors of mothers' intentions to vaccinate their daughters across three cultural groups: Hispanic, non-Hispanic white, and African American.
Methods
One hundred fifty mothers were recruited from Public Health Department clinics in Milwaukee, Wisconsin. Mothers were asked to answer measures that assessed personal and normative predictors of intentions.
Results
Results indicated that predictors of vaccination intentions varied cross-culturally. Specifically, culture moderated the influence of norms on intentions.
Conclusions
Interventions designed for Hispanics may be more effective if norms, rather than attitudes, are targeted.
Introduction
Cervical cancer accounts for the death of approximately one-quarter million women in the world each year. It is estimated that in the United States alone, 4000 women die of the disease yearly.1 Most cervical cancers are caused by the human papillomavirus (HPV), the most common sexually transmitted disease (STD) in the United States.2,3 High-risk resistant HPV strains 16 and 18 are recognized as precursors of 70% of cervical cancers. Two low-risk HPV strains, 6 and 11, are associated with 90% of genital warts.3 In 2006, the U.S. Food and Drug Administration (FDA) approved a three-dose vaccine to protect against HPV types 16, 18, 11, and 6.3 The Centers for Disease Control and Prevention (CDC) recommends the vaccine for preadolescent girls between the ages of 11 and 12 before the onset of sexual intercourse. Moreover, the CDC recommends catchup vaccination for girls aged 13–26. Because the HPV vaccine protects against only 70% of all cervical cancers, the CDC highlights the importance of continued cervical cancer screening after vaccination. However, recent estimates indicate that only 18% of U.S. girls in the target age group have received the three-dose series.3–5
Health disparities have been identified in the incidence of cervical cancer.2 Incidence is greater in Hispanic and African American women compared to non-Hispanic white women.6 Research suggests that being an ethnic minority is associated with high-risk HPV prevalence.7 In order to alleviate racial and ethnic health disparities, it is necessary to understand the most effective way to promote vaccine uptake in individuals from diverse cultures.
Models of health behavior (i.e., Health Belief Model8) suggest that individuals' beliefs about the riskiness and severity of a health threat, as well as their expectations about the pros and cons of taking action, influence health-protective behavior. For example, the belief that receiving the HPV vaccine will effectively reduce the likelihood of contracting HPV has been associated with willingness to receive the vaccine. Also, the perceived likelihood of getting cervical cancer and perceived negative side effects of the vaccine are also significant predictors of vaccine uptake.5 In addition to personal beliefs and outcome expectations, other models of health behavior (i.e., Theory of Reasoned Action9) indicate that norms (the opinions of significant others and the importance assigned to those opinions) are important influences on people's self-protective behaviors. For public health interventions to effectively engage individuals of different cultural groups, it is important to understand the potential contribution of norms and personal expectations to behavior change. Members from cultures oriented to the group (collectivist cultures) perceive themselves as an extension of the in-group, whereas members from cultures that emphasize personal accomplishments and individual initiative (individualist cultures) perceive themselves as unique and separate from others.10 Consequently, decisions of individuals who emphasize the group will tend to be organized around the opinion of important others, and the decisions of individuals who emphasize individual uniqueness and agency will tend to be based on personal opinions and attitudes. For example, research has documented that norms compared to attitudes are more important predictors of health-protective behavioral intentions in Hispanics.11,12
Researchers have extensively studied parents' and adults' willingness to receive the vaccine and have their children vaccinated. However, little has been done to understand the generalizability of findings of HPV vaccine acceptance studies to participants of diverse cultures.5,13 This is an important topic because research suggests that culture may moderate previously found associations. A recent study compared predictors of HPV vaccine acceptance in non-Appalachian and Appalachian women. Results indicate that for non-Appalachian women, younger age, lack of a college degree, and residency in a rural county were positively related to vaccine acceptance. On the other hand, for Appalachian women, smoking and having children living at home predicted vaccine acceptance, whereas being married predicted nonacceptance.14 The results of this study indicate that a one-size approach to promote behavior change may not fit all. Culture matters when considering potential factors to target in public health interventions. The emergence of cultural differences in factors associated with vaccine acceptance suggests that tailoring interventions to culturally diverse populations could help address health disparities in cervical cancer.
In light of the prevalent racial and ethnic health disparities, lack of understanding of the cross-cultural variation of factors that influence motivations to receive an HPV vaccine is an important caveat that needs to be addressed. The purpose of the study is to understand the cross-cultural variation of predictors of vaccination intentions among Hispanic, non-Hispanic white, and African American mothers of 9–17-year-old adolescent girls 4 years after licensure of the HPV vaccine.
Materials and Methods
The study was approved by the Medical College of Wisconsin Institutional Review Board. Our sample was one of convenience. We recruited 150 mothers who where the parent or legal guardian of a daughter who had not received the HPV vaccine. Mothers were 50 Hispanic, 50 non-Hispanic white, and 50 African American. In an attempt to control for important demographic variables, such as income, education, and insurance status, that may account for cross-cultural differences, we recruited only mothers who were receiving Women Infant and Children (WIC) federal program services at one of four city Health Department clinics in Milwaukee, Wisconsin. The eligibility requirements to receive WIC are determined by the U.S. Department of Health. To be eligible to receive WIC, women must be a) pregnant or the new mother of an infant up to age 5, b) resident of the state where she is applying to receive WIC services, and c) between 100 and 185% of the federal poverty guidelines.
Mothers were approached while waiting to be seen by a WIC program coordinator and asked if they would like to answer a brief questionnaire that would determine their eligibility to participate in the study. Mothers who volunteered answered a brief screening questionnaire to check that they met eligibility criteria. Mothers who self-reported being the parents or legal guardians of a daughter between the ages of 6 and 19 who had not been vaccinated against HPV were asked to participate in the study. All study materials were available in English and Spanish.
Participants answered a demographic questionnaire assessing age, number of children and their ages, education level, employment, and insurance status. Participants were also asked if they had previously thought about vaccinating their daughters against HPV and, if so, to name the place where they heard about the HPV vaccine. Prior experience with cervical neoplasia or cancer, HPV, or another sexually transmitted infection (STI) was assessed by asking mothers to indicate if they personally had been diagnosed with cervical cancer or neoplasia, HPV, or another STI and if they knew someone (friend or relative) who had been diagnosed. Response options were yes and no.
Intention to vaccinate daughters was the main outcome measure and was assessed with a measure that consisted of 5 items assessing intention to vaccinate, intention to convince daughter to get the vaccine if she objected, intention to convince a significant other if he or she objected, and intention to talk to a pediatrician or healthcare provider about it. Response options ranged from 1, definitely no, to 7, definitely yes. The Cronbach alpha for the Hispanic group was 0.91, for the non-Hispanic white group was 0.90, and for the African American group was 0.88.
The personal predictors of intention to vaccinate daughters were also assessed. Perceptions of risk were assessed with the following three items: How likely is your daughter to acquire HPV in her lifetime? What are the chances that your daughter will acquire HPV in her lifetime? and What is the probability that your daughter will acquire HPV in her lifetime? Response options for the first 2 items ranged from 1, very unlikely/almost zero, to 7, very likely/almost certain. Response options for the third item ranged from 0 to 100% in increments of 10. The first two items assessing risk perceptions were combined to form one scale. We included a slight variation in wording (e.g., likely vs. chances) in an attempt to capture slight variations in participants' nonquantitative estimates of risk. Interitem correlations were 0.87 for the Hispanic group, 0.93 for the non-Hispanic white group, and 0.84 for the African American group.
Perceived benefits of vaccinating daughters were assessed with the following item: “How effective is the vaccine in protecting against HPV? Response options ranged from 1, not at all, to 7, very much. Severity of acquiring HPV were assessed with the following three items: If your daughter acquired HPV, how severe would the consequences be? How traumatic would it be for your daughter? How embarrassed would your daughter be? Response options ranged from 1, not at all, to 7, very much. Interitem correlations were 0.91 for the Hispanic group, 0.90 for the non-Hispanic white group, and 0.88 for the African American group.
Barriers against vaccinating daughters were assessed with a variety of items asking about the potential side effects of the vaccine, worry that vaccination will lead to early initiation of sexual relations, more sexual activity, discouragement from engaging in other cancer-prevention activities such as cervical cancer screening, number of required vaccine shots, vaccine cost, and daughters' fear of vaccination. Response options ranged from 1, not at all, to 7, very much. Because of low interitem correlations, only the 2 items that assessed sexual-related barriers were combined to form one scale. Interitem correlations were 0.77 for the Hispanic group 0.86 for the non-Hispanic white group, and 0.87 for the African American group. The rest of the items assessing barriers were included in the analyses as individual predictors.
Normative predictors were assessed with the following item: How many of your friends' daughters have been vaccinated against HPV? Response options were none of them, some of them, almost all, and all of them. The extent to which the decision to vaccinate was shared was assessed with the following item: How much of the decision to vaccinate your daughter is up to you? Response options ranged from 1, not up to me, to 7, entirely up to me. This question was followed with an open-ended question that asked participants to state their relationship with the person with whom they shared the decision.
We first conducted a series of regression equations to understand if norms predicted additional variation, beyond that predicted by prior experience with HPV, neoplasia, and other STIs and barriers and health beliefs, in intention to vaccinate daughters across ethnic groups. Thus, we conducted separate multivariate blocked linear regressions for each ethnic group. In step one, we entered the variables that assessed prior experience with HPV, cervical neoplasia or cancer, and an STI using the forced entry procedure. Our rationale for entering prior experience with HPV, cervical neoplasia, or other STIs in the first step was to determine if barriers to vaccination and health beliefs predicted additional variation above and beyond prior experience. In the second step, we entered all the barriers to vaccination and health beliefs. In the third step of the equation, we entered norms. We entered norms in the last step of the equation to understand the percentage of variance that norms would account for after all the hypothesized variables had been included in the model. Our intent was to understand whether normative aspects may contribute differently to the behavioral intentions of members of certain cultural groups.
We conducted a final analysis to formally test whether culture (Hispanic, non-Hispanic white, and African American) moderates the expected relationship between intention to vaccinate daughters and norms, and we followed the procedure recommended by Cohen et al.15 and created two dummy codes for the variable ethnic group. The first code compared African Americans with Hispanics and non-Hispanic whites. Consequently, African Americans were coded 1, and the other two groups were coded 0. The second code compared Hispanics with African Americans and non-Hispanic whites Consequently, Hispanics were coded 1, and the other two groups were coded 0. We conducted a blocked hierarchical regression analysis to predict vaccination intentions by entering in the first step of the equation education and insurance status, as there were significant differences in these variables as a function of ethnicity; We then entered codes, norms, and the products of each of the codes and norms in the second step of the equation. The significance of higher-order terms independent of first-order terms would suggest the presence of interactions and would lend support to findings obtained when analyses are conducted separately for each ethnic group.
Results
Mothers' mean age was 33.72 (standard deviation [SD] 7.95). Mothers reported a mean of 3.38 (SD 1.42) children, with a mean age of daughters of 10.94 (SD 4.01) years. Table 1 displays demographic characteristics by ethnic group. As Table 1 shows, our attempt to control for demographic differences by recruiting mothers who were receiving WIC services was ineffective. We expected more homogeneous samples, and chi-square analyses comparing demographics across ethnic groups revealed statistically significant differences in insurance status (chi-square = 49.42, df = 6, p < 0.001) and education level (chi-square = 24.89, df = 8, p < 0.01). Hispanic mothers were less likely to be insured and more likely to have had only high school education than both white and African American mothers.
Table 1.
Demographic Variables Stratified by Ethnic Group
| |
Ethnic group |
|
||
|---|---|---|---|---|
| Hispanic | Non-Hispanic white | African American | p | |
| Employment status | NS | |||
| Employed | 67% | 75% | 64% | |
| Unemployed | 25% | 24% | 30% | |
| Retired | 6% | — | 6% | |
| Insurance status | <0.001 | |||
| Don't have | 43% | 8% | 4% | |
| Medicaid or state | 23% | 18% | 58% | |
| Private | 6% | 11% | 7% | |
| Education | <0.01 | |||
| Grade 0–12 | 82% | 57% | 40% | |
| Technical school | 6% | 4% | 8% | |
| 1–3 years college | 6% | 22% | 42% | |
| Bachelors degree | 6% | 14% | 8% | |
| Postgraduate | — | 1% | 1% | |
Some proportions do not add to 100% due to missing data.
NS, not significant.
Table 2 displays participants' prior experience with HPV, cervical neoplasia or cancer, and STIs by ethnic group. Chi-square analyses comparing prior experiences across ethnic groups revealed statistically significant differences in knowing a relative or friend who had been diagnosed with cervical cancer or neoplasia (chi-square = 6.90, df = 2, p < 0.05) and in knowing a relative or friend who had been diagnosed with an STI (chi-square = 20.06, df = 2, p < 0.001). Non-Hispanic white and African American mothers were more likely than Hispanic mothers to know a relative or friend who had been diagnosed with cervical cancer or neoplasia and an STI.
Table 2.
Percentages of Participants with Prior HPV-Related Experience by Ethnic Group
| |
Ethnic group |
|||
|---|---|---|---|---|
| Hispanic | Non-Hispanic white | African American | p | |
| Diagnosis of HPV for self | 10% | 17% | 8% | NS |
| Know other who had HPV diagnosis | 55% | 34% | 18% | NS |
| Diagnosis of cancer for self | 2% | 11% | 2% | <0.05 |
| Know other who had cancer diagnosis | 16% | 38% | 37% | <0.001 |
| Diagnosis of STI for self | 14% | 19% | 33% | NS |
| Know other who had STI diagnosis | 24% | 66% | 61% | NS |
HPV, human papillomavirus; STI, sexually transmitted infection.
Fifty-five percent of Hispanic mothers (n = 27), 50% of African American mothers (n = 25), and 70% of non-Hispanic white mothers (n = 33) said they had previously thought about vaccinating their daughters. Across the groups, the majority reported that the primary source of information about the HPV vaccine was televised advertisements from a pharmaceutical company (62% of Hispanics, 76% of non-Hispanic white women, and 87% of African Americans). Fifty-five percent of Hispanic, 57% of African American, and 45% of non-Hispanic white mothers reported sharing vaccination decisions with either their daughter, the father of their daughter, or both.
Table 3 presents the results of the first set of analyses for each ethnic group. For Hispanic mothers, norms was the only variable that predicted vaccination intentions. For non-Hispanic white mothers, knowing a relative or friend who has been diagnosed with cancer or neoplasia was a significant predictor of intentions (β = 0.33, p < 0.01), as were the following barriers and health beliefs: perception that vaccination would lead to increased sexual risk taking (β = −0.45, p = 0.06), potential side effects of the vaccine (β = −0.37, p < 0.01), and perception of vaccine effectiveness (β = 0.52, p < 0.001). Norms, however, did not predict additional variation in vaccination intentions in non-Hispanic white mothers. For African American mothers, a prior diagnosis of an STI was a significant predictor of intentions (β = 0.38, p < 0.05), as were the following barriers and health beliefs: perception that the vaccine could lead to a decrease in other cervical cancer prevention efforts (β = 0.74, p = 0.07), and perception of daughter's risk of contracting HPV (β = 0.36, p = 0.05). Contrary to our hypothesis and similarly to non-Hispanic white mothers, norms did not predict additional variation in the vaccination intentions of African American mothers.
Table 3.
Hierarchical Regression Equations for Intentions Stratified by Ethnic Group
| Steps in equation | R | R2 | R2Δ | p |
|---|---|---|---|---|
| Hispanic | ||||
| 1. Prior experience with HPVa | 0.26 | 0.06 | 0.06 | 0.90 |
| 2. Barriers and health beliefs | 0.56 | 0.31 | 0.24 | 0.65 |
| 3. Norms | 0.70 | 0.50 | 0.17 | 0.02* |
| Non-Hispanic white | ||||
| 1. Prior experience with HPV | 0.40 | 0.15 | 0.15 | 0.40 |
| 2. Barriers and health beliefs | 0.86 | 0.73 | 0.60 | 0.00* |
| 3. Norms | 0.86 | 0.73 | 0.00 | 0.49 |
| African American | ||||
| 1. Prior experience with HPV | 0.60 | 0.37 | 0.37 | 0.01* |
| 2. Barriers and health beliefs | 0.80 | 0.64 | 0.27 | 0.09 |
| 3. Norms | 0.80 | 0.64 | 0.00 | 0.67 |
The variable, Prior experience with HPV, refers to participants' prior experience with HPV, neoplasia, or other STIs as a result of a diagnosis for self or close other.
p < 0.05.
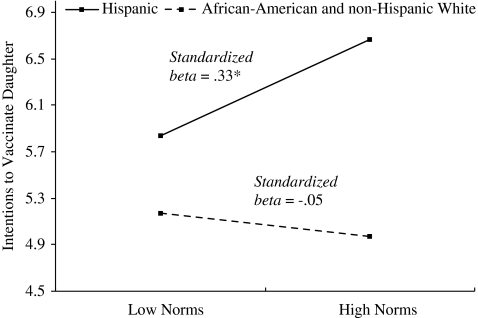
Finally, the results of our formal moderation analysis revealed that insurance and education status did not emerge as significant predictors (R2 = 0.00, p = 0.55), and only the interaction term composed of the code comparing Hispanics with the other two ethnic groups and norms (R2 = 0.11, β = 0.33, p = 0.02) emerged as significant (Fig. 1). As Figure 1 shows, at 1 SD above the mean for norms, intentions to vaccinate daughters increased significantly for the Hispanic group only (r = 0.51, p < 0.05).
FIG. 1.
Intentions to vaccinate as a function of ethnic group and social norms. Social norms predicted intentions in the Hispanic group only. Vaccination intentions ranged from 1, not at all, to 7, very much. *p < 0.05.
Discussion
Prior research has documented extensively the importance of personal health beliefs and outcome expectations as predictors of intentions and uptake of HPV vaccination. However, research on the generalizability of such findings to ethnic minority populations is lacking. In light of the ethnic health disparities in cervical cancer rates and research suggesting that norms may be an important predictor of intentions in members of collectivist cultures, the purpose of this study was to investigate whether norms predicted vaccination intentions above and beyond health beliefs and prior experience with HPV, cervical cancer or neoplasia, or another STI. Our study suggests that additional factors than those derived from personal expectations may need to be targeted in interventions aimed at promoting vaccination among Hispanics.
Overall, the findings of this study are consistent with prior studies in that experience with cervical cancer or neoplasia and personal health beliefs, such as beliefs about vaccine side effects and effectiveness, predict vaccination intentions in non-Hispanic white mothers. Chao et al.16 observed a modest association between prior experience with STIs and HPV vaccine uptake in a large representative sample. However, it seemed that ethnicity acted as a moderator, as an inverse association was observed for African Americans and an enhanced effect was seen for Asian Americans. These findings point to the importance of stratifying analyses by ethnicity or culture to uncover potential cultural variation in important predictors of vaccination.
In our study, the perception that the vaccine would lead to increased sexual risk taking predicted vaccination intentions only in non-Hispanic white mothers. Past research has produced conflicting findings about the influence on vaccination intentions of the belief that vaccination would lead to sexual disinhibition. Because many controversies surrounding HPV vaccination stem from this very issue, Brewer and Fazekas13 attempted to provide an answer through a meta-analysis. Because of the small number of studies available at the time, however, a conclusive answer could not be found. To date, more research has been conducted, and the time may be ripe to attempt to answer this question again.
In our study, the belief that the vaccine would lead to a decrease in other behaviors that protect against cervical cancer, such as screening, emerged as a deterrent of vaccination intentions among African American mothers. The relationship between mothers' attitudes toward other cervical cancer prevention efforts and vaccination intentions deserves further attention. To our knowledge, one study16 found an association between mothers' own Papanicolaou uptake and attitude toward vaccination. Mothers who are screened frequently have a more positive attitude toward vaccination, although we do not know the mediating mechanisms. Our study suggests that future research should seek to identify the interrelationships among mothers' attitude toward cervical cancer screening, beliefs about the influence of vaccination on screening, and intentions to vaccinate. These factors could be fruitful targets of future interventions to promote vaccine uptake. This is a key issue because of the importance of continued cervical cancer screening after vaccination.
Our findings also shed light on the influence of social norms, an important contributor to health decision making that has been understudied in HPV vaccination research. As hypothesized, social norms emerged as the strongest predictor of intentions in Hispanics. This finding supports our hypothesis that aspects other than those derived from personal health beliefs may be strong contributors to intentions in cultures that emphasize the in-group. Contrary to our expectations, however, we did not find an association between norms and intentions in African Americans, a culture that also emphasizes the in-group.17 In African Americans, personal experience with an STI was the strongest contributor to vaccination intentions. Although we did not find an association between norms and intentions in African American mothers, the association between intentions and prior experience with an STI underscores the importance of studying the influence of highly salient contextual factors particular to certain ethnic groups on health-related decisions. STIs are a salient aspect for African Americans because they disproportionately affect the African American community. The HPV vaccine protects against the most common STI, and public health interventions targeting African Americans that highlight this fact may be more persuasive than those that only highlight the protection that the vaccine offers against cervical cancer. This speculation is supported further by the association found between perceptions that daughters are at risk of contracting HPV and vaccination intentions in African American mothers.
Our study has several limitations. First, we used a small convenience sample at one point in time. This limitation restricts the generalizability of our results. Consequently, our recommendations should be taken with caution until supported by further research. Second, we focused on intentions to vaccinate rather than on actual vaccine initiation and completion. Third, gender may moderate the associations of theoretical tenets and intentions, and we only surveyed mothers. Fourth, our measures of prior diagnosis of cervical neoplasia or cancer and STIs were self-report and, thus, may have been subject to social desirability effects. Finally, although we attempted to control for demographic factors, such as income, by recruiting mothers who were receiving WIC services, demographic differences were present in education level and insurance status. Moreover, we did not measure actual income and key cultural constructs, such as collectivism. Future studies should recruit a random stratified sample from each ethnic group, use a longitudinal design to study vaccine initiation and completion, include other key decision makers, and assess such important demographic factors as income, and key cultural constructs to investigate plausible moderation and mediation effects.
Our findings may have important implications for the design of culturally tailored interventions to promote HPV vaccination. Our study suggests that interventions designed for Hispanics may be more effective if they target norms, rather than attitudes. Whereas interventions designed for African Americans may yield better results if designed to target perceptions of HPV risk. Social network interventions that have been shown to successfully modify norms and risk perceptions in HIV/AIDS research18,19 may be particularly suitable to promote uptake of the HPV vaccine in Hispanic and African American populations.
Acknowledgments
Preparation of this article was supported, in part, by center grant P30-MH52776 from the National Institute of Mental Health and by NRSA postdoctoral training grant T32-MH19985. We thank Nancy Castro, Ann White, Jennifer Vaclav, and Heidi Zimmer for their assistance in data collection and Steven D. Pinkerton and Carol L. Galletly for their invaluable feedback on early discussion of this work. We convey our gratitude to Laura Glasman for helpful editorial comments.
Disclosure Statement
The authors have no conflicts of interest to report.
References
- 1.Huang CM. Human papillomavirus and vaccination. Mayo Clin Proc. 2008;8:701–707. doi: 10.4065/83.6.701. [DOI] [PubMed] [Google Scholar]
- 2.National Cancer Institute. HPV vaccines for cervical cancer 2009. Bethesda, MD: National Cancer Institute; 2009. [Google Scholar]
- 3.Centers for Disease Control and Prevention. Immunization information systems (IIS) Frequently asked questions 2009. Atlanta, GA: CDC; 2009. [Google Scholar]
- 4.Gamble HL. Klosky JL. Parra GR. Randolph ME. Factors influencing familial decision-making regarding human papillomavirus vaccination. J Pediatr Psychol. 2010;35:704–715. doi: 10.1093/jpepsy/jsp108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reiter PL. Brewer NT. Gottlieb SL. McRee A-L. Smith JS. Parents' health beliefs and HPV vaccination of their adolescent daughters. Soc Sci Med. 2009;69:475–480. doi: 10.1016/j.socscimed.2009.05.024. [DOI] [PubMed] [Google Scholar]
- 6.American Cancer Society. Cancer facts & figures 2007. Atlanta, GA: American Cancer Society; 2007. [Google Scholar]
- 7.Kahn JA. Lan D. Kahn RS. Sociodemographic factors associated with high-risk human papillomavirus infection. Obstet Gynecol. 2007;110:87–95. doi: 10.1097/01.AOG.0000266984.23445.9c. [DOI] [PubMed] [Google Scholar]
- 8.Becker MH. The Health Belief Model and personal health behavior. Health Educ Monogr. 1974;2:324–473. [Google Scholar]
- 9.Ajzen I. Fishbein M. Understanding attitudes and predicting behavior. Englewood Cliffs, NJ: Prentice Hall; 1980. [Google Scholar]
- 10.Markus HR. Kitayama S. Culture and the self: Implications for cognition, emotion, and motivation. Psychol Rev. 1991;91:224–253. [Google Scholar]
- 11.Lechuga J. Wiebe JS. Can language prime culture in Hispanics? The differential impact of self-construals in predicting intentions to use a condom. Int J Psychol. 2009;44:468–476. doi: 10.1080/00207590902835710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ybarra O. Trafimow D. How priming the private self or collective self affects the relative weights of attitudes and subjective norms. Pers Soc Psychol Bull. 1998;4:362–370. [Google Scholar]
- 13.Brewer NT. Fazekas KI. Predictors of HPV vaccine acceptability: A theory-informed, systematic review. Prev Med. 2007;45:107–114. doi: 10.1016/j.ypmed.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 14.Christian WJ. Christian A. Hopenhayn C. Acceptance of the HPV vaccine for adolescent girls: Analysis of state-added questions from the BRFSS. J Adolesc Health. 2009;44:437–445. doi: 10.1016/j.jadohealth.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 15.Cohen J. Cohen P. West SG. Aiken LS. Applied regression/correlation analysis for the behavioral sciences. 3rd. Mahwah, NJ: Lawrence Erlbaum; 2003. [Google Scholar]
- 16.Chao C. Slezak JM. Coleman KJ. Jacobsen SJ. Papanicolaou screening behavior in mothers and human papillomavirus vaccine uptake in adolescent girls. Am J Public Health. 2009;99:1137–1142. doi: 10.2105/AJPH.2008.147876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Komarraju M. Cokley KO. Horizontal and vertical dimensions of individualism-collectivism: A comparison of African Americans and European Americans. Cult Divers Ethnic Minor Psychol. 2008;14:336–343. doi: 10.1037/1099-9809.14.4.336. [DOI] [PubMed] [Google Scholar]
- 18.Amirkhanian YA. Kelly JA. Kabakchieva E, et al. A randomized social network HIV prevention trial with young men who have sex with men in Russia and Bulgaria. AIDS. 2005;19:1897–1905. doi: 10.1097/01.aids.0000189867.74806.fb. [DOI] [PubMed] [Google Scholar]
- 19.Amirkhanian YA. Kelly JA. McAuliffe TL. Identifying, recruiting, and assessing social networks at high risk for HIV/AIDS: Methodology, practice, and a case study in St. Petersburg, Russia. AIDS Care. 2005;17:58–75. doi: 10.1080/09540120412331305133. [DOI] [PubMed] [Google Scholar]