Abstract
Background
Adherence to inhaled steroid regimens for asthma is poor in adults and children. Although it is assumed that nonadherence contributes to morbidity in older adolescents, investigation is limited.
Objective
To describe adherence to preventive asthma medications and explore relevant beliefs and attitudes in older urban adolescents including their ideas for improving adherence.
Methods
Quantitative and qualitative methods were employed to collect data from a convenience sample of adolescents with asthma previously prescribed fluticasone/salmeterol. Two semi-structured face-to-face interviews were conducted one month apart and analyzed for themes. Fluticasone/salmeterol use was electronically monitored between visits and calculated as the number of actuations divided by the number of inhalations prescribed.
Results
40 participants, 15–18 years, 19 female, 30 Black/African-American, 11 Medicaid-insured, 24 previously hospitalized for asthma, median FEV1 98% predicted, (range 67%–127%), had median adherence 43% (range 4%–89%). Adherence was not associated with FEV1 or ED visits. Themes emerged from interviews: teens 1) take fluticasone/salmeterol inconsistently; 2) believe fluticasone/salmeterol is “supposed to help me breathe”; 3) dislike its taste; 4) are “too busy” and “forget”; and 5) recommend “reminder” solutions to poor adherence. 20% believed that taking fluticasone/salmeterol was unnecessary and another 18% expressed ambivalence about its benefits.
Conclusion
Adherence was poor. Examining and acknowledging health beliefs of older teens in the context of their complicated lives may facilitate discussions about self-management.
Keywords: asthma, adolescent, adherence, inhaled corticosteroid
INTRODUCTION
Adherence to inhaled corticosteroid (ICS) regimens for asthma is poor in adults and children.1–8 Although older adolescents, age 15 to 20, are less studied than younger or older age groups, suboptimal adherence is thought to contribute substantially to their morbidity.9, 10 Asthma most severely affects urban teens, including blacks.11, 12 Among 15–19 year olds with asthma, blacks have 3 times the ED visits, 4.5 times the hospitalizations, and 5 times the death rate of whites.13 These disparities among older adolescents have increased at a time when total asthma morbidity has decreased.13–16
Older adolescence is a unique stage of cognitive and psychosocial development, and a time when self-regulatory behavior and organizational skills develop,10 all needed for adherence. Adolescent health beliefs related to adherence will be influenced by these development processes, as well as family and cultural factors.17, 18 Adolescent health beliefs, including attitudes toward medicine-taking for asthma. have been previously explored in broader and younger age groups, however, no studies have specifically examined adherence and health beliefs among urban older adolescents, a population at particular risk.9, 19–26
The current mixed method exploratory study was designed to assess beliefs about adherence and asthma management of asthma among older adolescents in open-ended interviews, and probe for teens’ ideas for improving or maintaining adherence. We recruited adolescents from clinics serving urban low-income neighborhoods to participate in these open-ended interviews and electronically monitor the teen’s adherence over 4 weeks. We organized teens’ interview responses as they align with the constructs of The Health Belief Model (HBM), a theory of health behavior that has been previous applied to adolescents.27, 28 HBM proposes that a person’s willingness to perform a health behavior, e.g., increase amount of ICS taken, is related to the perception of 1) susceptibility to the disease (e.g. asthma) the behavior (e.g. adherence) addresses, 2) the severity of the disease, 3) the benefits of taking the recommended action in order to avoid or ameliorate the negative health condition, 4) the barriers to be overcome in accomplishing the behavior, 5) cues to action (e.g. to improve adherence), and 6) likelihood of successfully accomplishing the health action (self-efficacy).29 Theories of health behavior can facilitate identification of determinants of behavior and motivation for change for both adults and adolescents and the present study provides new information about the relationship between health beliefs and adherence behavior among urban older adolescents.29
METHODS
Design and protocol summary
We conducted an observational cohort study using quantitative and qualitative methodology to collect data from a convenience sample of adolescents who had moderate to severe asthma.30–33 Teens were recruited for two interviews one month apart; adherence to ICS was electronically monitored between interviews. During the initial interview we collected socio-demographic and asthma history information. In the semi-structured audio-taped interviews we explored teen perceptions and beliefs about medicine-taking, adherence, and asthma.
Subjects were enrolled until saturation was achieved, i.e., no new information was presented,34 and at least 30 subjects had been enrolled. All subjects were enrolled and interviewed by one trained investigator (DRN). The Children’s Hospital of Philadelphia Institutional Review Board approved this study.
Participant identification and recruitment
From December 2006 through November 2007 we recruited teens, aged 15 to 21 years with moderate or severe persistent asthma according to National Asthma Education and Prevention Program Expert Panel Report guidelines,30, 35 who were prescribed fluticasone/salmeterol (F/S), a frequently prescribed controller medication for which we had an electronic monitor. Schedules and medical records of patients of the Allergy Clinic and the Adolescent Care Center of The Children’s Hospital of Philadelphia were scanned for teens with a diagnosis of asthma prescribed F/S. Potential participants were approached during an outpatient clinic visit or during an inpatient stay for asthma (two patients). They voluntarily signed consent or assent to study procedures. Interviews took place in an unoccupied private examining room or in a private hospital room. Participants received one free movie ticket ($6 value) after the first interview and 2 tickets after completing the second interview.
Monitoring steroid-containing inhalers
The electronic monitor, the Diskus Adherence Monitor (DAL), records date and time of an F/S inhalation.36 DAL was attached to the patient’s ICS at the end of the first visit and adherence data was downloaded during the second. Participants were told that the monitors recorded the time and date of each inhaler actuation.
Patient data
Participants reported age, race and ethnicity choosing from US census classifications, grade level, asthma-related ED visits and hospitalizations; co-morbidities; and current medications. We used the teen’s address to estimate median household income from census block data.37 Spirometry was completed at both visits according to American Thoracic Society criteria.38, 39
Qualitative interviews
Interviews were held in a private location as described above; if caregivers had accompanied the teen, they were asked to remain outside the interview room. Each audio-taped interview was transcribed. A portion of the tapes were reviewed by investigators who did not conduct the interview in order to ensure the consistency and completeness of data collection.
During the first one-on-one interview, adolescents were asked about their general well-being and school life. We began with these topics to help the teens become comfortable in discussing daily activities. Then, we asked about knowledge of the function of F/S, and barriers to adherence. Teens were asked to weigh the risks and benefits (attitude) of taking chronic F/S, ways to prevent omission of doses, and beliefs about their ability (self-efficacy) to overcome barriers to adherence, since attitude influenced adherence in adults.1, 40 Finally, we asked how asthma and medicine-taking affected school and home life. All questions were asked in a nonjudgmental manner using open-ended questions with permissive stems.
On the second visit, participants were asked about adherence over the 4 weeks of monitoring, shown the DAL data, and asked for further comments about adherence and the impact of asthma. They again were asked how asthma and medicine-taking influenced their everyday lives.
Data analysis
Adherence
Adolescents were prescribed 1 puff of F/S over either a 12-hour or a 24-hour period. A monitoring period was defined as the time during which an adolescent was prescribed 1 puff of F/S. For those prescribed a 12-hour regimen, we used from 0:00 through 11:59 and from 12:00 through 23:59 as the two monitoring periods in a day; a 24-hour period was 00:00 through 23:59.
We truncated adherence at 100% for each monitoring period because it controls for dumping, i.e., multiple actuations over a very short period of time, and thus provides a better measure of adherence.1, 2, 41–43 ICS adherence was calculated as (the total truncated number of actuations recorded over all monitoring periods) / (the number of monitoring periods) × 100. Because adherence is not normally distributed, adherence was categorized in quartiles according to its frequency distribution (< 26.8%, between 26.8 and 42.9%, between 42.9 and 61%, > 61%). Ordered logistic regression was used to test the association of adherence with demographic and asthma-related predictors.
Qualitative analysis
The data collection process was iterative in that after the first few interviews we added prompts and refined and supplemented questions, based on responses of the first interviewees.34, 44 The data collection continued until saturation was achieved.34 Three investigators (DRN, TGF, AJA) independently analyzed each transcribed interview using the transcriptions and observational notes of the interviewer. In a data reduction process using content analysis, the investigators independently looked for common themes, 29, 44, 45 using grounded theory structure, that is, returning to the original tapes and transcripts.44, 46, 47 Themes were identified by consensus of the investigators, and were summarized and interpreted within the framework of the HBM.
Themes from the interviews were coded and compared with electronically monitored adherence to understand the relationship between the quantitative and qualitative data. For example, a variable was created to represent a teen’s report during the interview of degree of adherence (e.g., coded as 0 if the teen reported no or little inhalation of prescribed ICS, 1= if teen stated some ICS doses were taken, and 1 if the teen reported taking most or all prescribed ICS doses). A variable was created from teens’ report during the interviews of whether ICS was helpful: 0= no help, 1= some help. Two investigators coded these variables independently. Where there were inconsistencies, the transcripts were reviewed by the coders together until agreement was reached. Nonparametric correlations were performed to test if these responses were correlated with monitored adherence.
RESULTS
We approached 47 adolescents; 40 agreed to participate and 39 completed the protocol. The seven teens that declined stated they were too busy or lived too far away. Approximately half were female; most were black; and most were from low-income neighborhoods (Table I). Seven spent at least 2 nights /week away from home: 5 stayed at the home of family members, one reported nights away from home due to family conflict. FEV1 was above 90% predicted for all but 6 individuals. Almost half had had an ED visit, and 20% had been hospitalized in the past year for asthma. Four participants were noted to be coughing or wheezing during one or both of their visits.
Table I.
Characteristics of Enrolled Adolescents
| Demographics | n = 40 |
| Age (years)* | 16 (15–18) |
| Female | 19 (48%) |
| Race | |
| Black/African American | 30 (75%) |
| White | 11 (28%) |
| Asian | 2 (5%) |
| American Indian/Alaskan native | 6 (15%) |
| Hawaiian | 1 (3%) |
| More than one race | 13 (33%) |
| Ethnicity: Hispanic/Latino | 1 (3%) |
| # of medications prescribed* | 5.5 (2–9) |
| Medicaid insured | 11 (28%) |
| Current smoker | 2 (5%) |
| Median household income (dollars)* | 38.5k (9.8k–71.8k) |
| Asthma severity | |
| FEV1 (% predicted)** | 98 ± 12 |
| Age at diagnoses (years)** | 6 ± 4.5 |
| ED visits in past year | 17 (43%) |
| Hospitalizations in past year | 8 (20%) |
| Lifetime hospitalizations | 24 (60%) |
| Lifetime intensive care admissions | 4 (10%) |
Mean (range)
Mean ± SD
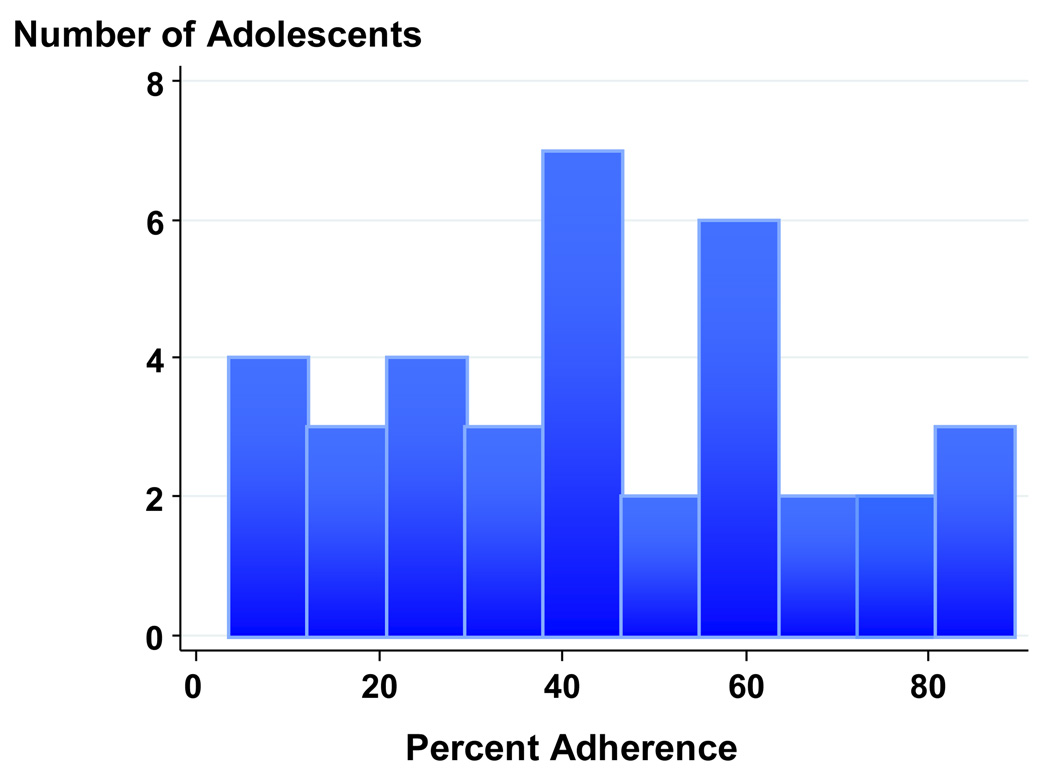
Electronically-Monitored Adherence
The monitors of three participants failed to download; data was available for 37 out of the 40 participants. Median adherence was 43% (interquartile range: 25%–62%) (Figure 1). Adherence was better for younger than older participants, (p=0.01). There was no difference in adherence by sex (p=0.75), race/ethnicity (p=0.39), estimated household income (p=0.27), FEV1 at enrollment (p=0.59), ED visits (p=0.92) or hospitalizations (p=0.71) in the past year.
Figure 1.
Frequency distribution of mean truncated adherence. Adherence is expressed as the mean of adherence of the monitoring periods, as a percent adherence truncated at 100%.
Adolescent Health Beliefs: HBM Themes from Qualitative Interviews
Prevalent interview themes were classified according to key elements of the HBM: 1) self-reported description of degree of adherence, 2) perceived severity of asthma—how it affects daily life, 3) perceived benefits/risks of taking ICS, 4) perceived barriers to medicine taking, 5) proposed cues to action e.g. to improve adherence, and 6) belief in ability to take medication (self-efficacy). (Table II)
Table II.
Patient Themes Framed According to Health Belief Model
| DATA REDUCTION | THEMES |
|---|---|
| Health Behavior: Adherence | Teens for the most part do not take ICS regularly |
Perceived susceptibility/severity
|
Asthma may affect daily life, but not always
|
Perceived Benefits/Risks of taking ICS
|
Teens do not perceive great benefit from ICS
|
Perceived Barriers
|
Taking ICS regularly is very difficult
|
Cues to Action: Strategies to promote ICS adherence
|
Proposed strategies surround external reminders |
Self-Efficacy
|
Changing pattern of taking ICS will not be easy
|
Self-reported adherence behavior
Thirty-eight of the 40 teens during the first interview and all in the second interview admitted they did not take F/S as often as prescribed.
… I don't really take it that religiously or anything, …[I don’t take it] a lot…maybe three times…maybe three times every two weeks, two or three weeks, something like that…
Perceived susceptibility to attacks/perceived severity: How asthma affects their daily activities
Although 29 (73%) teens reported asthma interfered with activities, 8 reported no symptoms.
…when I first had asthma, my mom said, "Well, you can't do this…you can't do that." And, I was sorta left out because I couldn't do stuff the other kids did… And, now…it's still hard, because, I run track. And, my coach says, "Well, you know you can't run because you got asthma." Or, he'll say, "You got to slow down," or something. I don't …
I pay attention to my asthma, but I like to do more than what I'm supposed to…
Perceived benefits/risks of taking ICSs
Six teens specifically stated that F/S was not helpful and an additional 6 reported that this medication was not necessary.
…when I take my medicine, sometimes, I still get sick. When I don't take my medicine, I don't get sick. I really don't see where it comes in handy, but I guess if the doctor says I need it, I need it…
Eight (20%) did not experience any difference in symptoms whether they took their F/S regularly or not, 7 (18%) more were ambivalent about its benefit.
I don’t [need to take F/S]. Because when I don’t take it I feel the same as when I do take it. To me, it doesn’t make a difference.
Thirteen participants reported feeling well as a reason for forgetting to take medications. Eight believed they did not need to take their medications because they had no symptoms.
…I don’t use it at all… right after I come from the doctor’s I take it for 2–3 days and then I just forget…It is not that I don’t want to take it, it is that I forget to take it…if I had more symptoms, then I would take it …
Eighteen (45%) did not like the taste of F/S and reported that the taste discouraged them from using the ICS.
…I don’t like the taste or the way it feels in your mouth or anything… it always gets caught in my throat and I can taste it and feel it in there…for half an hour afterwards…
Three teens expressed fear of addiction to medication like this 17 y.o. male:
… Well, I actually do see a use for albuterol, but I don’t really like taking it a lot. Cause I feel …if I take medicine its going to slow me down… it does help…especially the nebulizer. But, I don’t really think I need it…and…if I was to continue using it…I feel I’d get …hooked on it.
Two others thought it affected their appearance, e.g. “gave me acne”, or “made me stocky.”
Perceived Barriers to ICS use
22 teens (55%) reported difficulty in organizing time and setting priorities as a reason for forgetting to take ICS.
… I have generally two essays due a week and one project. So, I come home and work for a couple hours and then go upstairs to do … my little homework. And, I'll just fall asleep for the night. So … I just forget.
A 15yo boy thought he was prescribed too many medications, a belief expressed by 33%.
…It is a pain…not just the [F/S], but I do take a lot of other medicine and it takes up time and stuff…
9 participants reported losing the F/S inhaler and then either going without medication, using another inhaler – their own, or one belonging to another family member.
…Oh, that’s ‘cause I lost my [F/S] in my luggage. I couldn’t find it…I checked in my luggage, but then it fell into another bag and I didn’t check that for a while…
…I move my stuff around so much that I sort of forgot and didn't keep track of it…
A 17yo girl like 6 others reported not taking medications because of staying at a friend’s or family member’s home and leaving her medications behind. At least seven teens regularly spent at least 1 night away from home.
… I'm never home. I'm usually at my friend's…I'm barely ever home. But, if I come home, it's for a little while to help out, and I take my medicine at home, if I have to. I carry it with me if I go out, to like sleep out. But, if I feel like taking it, or remember taking it, I'll take it…
Only one teen described conflicts at home. A 16yo boy described why he spent a lot of time away from home and a tumultuous relationship with his father. His story demonstrates both how parental relationships can be viewed as a hindrance by teenagers and suggest how, in the context of larger stressors and pulls, medication may take on minimal significance for the teen.
My dad make me feel bad about myself…like he would say little smart remarks, like stuff…like he say he can't wait ‘til I leave, get out of the house…I am going to get kicked out when I'm 18. He don't care what is going to happen to me… I don't be home a lot cause all [my parents] want to do is argue a lot…they really don't care about me …that is why I do the things I do…
Only three teens felt uncomfortable taking asthma inhalers in front of their friends. A 15yo female said:
… I wouldn't be scared, or shy to take [medicine] in front of [my friends], cause they all know about it…
In fact, many teens had friends with asthma:
… Generally, we take [our medications] together at gym… if one of us forgets the other one will remind…
Cues to Action: Strategies to promote adherence to medications
Teens were asked to suggest methods for increasing adherence to controller medications. 73% provided concrete, organizational solutions. For example, 17 recommended placing the inhaler near their toothbrush or on their nightstand. Others suggested using reminder notes, a calendar, alarms/cellular phone reminders, or prizes or rewards. Although 21 (53%) expressed annoyance when reminded by a parent (most often their mother), 8 also interpreted the reminder as a sign of attention and caring.
…[My mother reminding me] gets annoying, but it helps because I don't forget.
Twenty-five related taking ICS more often because a monitor was attached to it. Some recounted seeing the monitor on the ICS served as a reminder. Four others said they wanted to show they did take their medication when they were supposed to and didn’t want to be embarrassed. Seven adolescents stated their parents (and even siblings) were more vigilant in reminding them to take their ICS since they were enrolled in a monitoring study.
I would have to say maybe because I knew I was being monitored. And, then, plus I know my mom really, really stayed on top of me about it. That kinda did make a change. I know my mom does stay on top of me about taking my medicine all the time. But, she did really stay on me about taking my medicine.
Self-efficacy
Teens were not confident they could overcome forgetting to take the medicine.
…It is not that I don’t want to take it; it is that I forget to take it …I just forget.
Association of electronic adherence with themes
Self-reported adherence was highly correlated with electronic adherence (rho=0.55, p=0.002). Neither reported nor electronic adherence was associated with perception of interference of asthma with activities, or with beliefs that ISCs were beneficial or with reporting forgetting doses.
DISCUSSION
Our study is noteworthy for examining the health beliefs that influence adherence of a unique developmental age group, older adolescents, one that has received limited attention. Additionally, within this group we have focused on teens from a population at high risk for morbidity from low-income urban neighborhoods. Finally, our study is unique in documenting adherence electronically in this age group and combining this quantitative information with qualitative information concerning health beliefs, framed around the HBM. These adolescents with moderate to severe persistent asthma reported they did not take F/S regularly, consistent with data downloaded from electronic monitors. Better adherence was associated with younger age but not any other collected socio-demographic or disease-related characteristic.
Framing the interviews according to the HBM yielded valuable insights (Table II). Teens were more willing to take medications when they did not feel well, but having only intermittent symptoms reduced the perception of benefit of taking medicine chronically. Taking preventive medication, a concept that involves avoiding risk, was not meaningful to this age group, compared with adults. Nevertheless, like adults,1, 48 teens expressed fear of side-effects. Unlike adults, they were not concerned about the cost of medication.
Teens’ complicated lives, including school commitments, were the most frequently expressed barrier to taking F/S regularly. For some, spending nights at other family members was a significant barrier to taking medications regularly. The bad taste of F/S was frequently cited.
The teens suggested cues to action that were largely external reminders that did not address teens’ perceptions of benefits and barriers to taking F/S regularly. With limited perceived benefit and significant barriers, taking F/S was not a high priority and teens “simply forgot,” that is, they lacked self-efficacy. Teens’ impression of generally “feeling well” was supported by spirometry. This finding differs from some49–52 but not all studies53 of mostly younger children that show a lack of correlation of symptoms and FEV1. Yet, despite mostly normal spirometry, 20% of the teens had hospitalizations and 43% had ED visits in the past year. During our study there was no difference in adherence among those who had had an ED visit or hospitalization compared with those who had not, however, our spirometric and adherence assessments likely do not reflect the state of asthma at the time of an ED visit. Thus, more effective management might involve medication schedules that account for intermittent and possibly rapidly evolving changes in control such as may occur with the onset of a viral respiratory infection.
Noteworthy was the finding that many teens spent nights regularly away from their primary home. Family conflict may be a reason, but in our sample that was generally not the case; it was expedient for providing care for these youth. Nevertheless, clinicians may want to inquire about nights away from home because spending time in two or more locations makes to chronic medication regimens difficult to organize.
Our data also suggest the possibility that for at least some of these teens, asthma status truly was improving and less ICS than was prescribed was needed. This may be particularly true for the 21 teens who had neither a hospitalization nor ED visit in the past year. This also would be consistent with the observation that asthma, can remit over teenage years.13, 54 In these cases appropriate clinical management should include careful evaluation to determine if regimen intensity can be stepped down.
In diabetic adolescents, parental monitoring has improved medication adherence and diabetic control.55 Although many of our participants expressed annoyance at parents’ prompting, and such prompts did not appear to change medicine-taking, the teens seemed to regard such reminders as a sign a parent was concerned about them and watching over them.
Our study has limitations. Since teens knew they were being monitored, the observed adherence could differ from adherence without observation (Hawthorne effect). It might be expected that observed adherence would be better than unobserved adherence,56 but our observed adherence was suboptimal. On the other hand, some teens who knew they were being observed may have responded paradoxically, increasing nonadherence to gain the interviewer’s attention. Almost all participants were recruited during a regularly scheduled follow-up appointment; therefore, it could be assumed we recruited a population more adherent than those who missed or never made appointments. Nevertheless, even in this group, adherence was poor. A small number of monitors malfunctioned, but we were able to capture data on almost all of the participants. Most importantly, as a small mostly qualitative study, we do not know how representative our findings are of other teens. Future research must test the generated hypotheses in this exploratory study within a broader population of urban older teens.
Our group of interviewed teens raised some of the same but also differing concerns about medicine-taking that have been expressed by adults in other studies.1, 48 Discovering these concerns seems to have been facilitated by allowing teens to feel comfortable about disclosing poor adherence and their beliefs about adherence. An important lesson is that providers may benefit from including some one-on-one time with teens to facilitate communication. In this study teens were concerned about addiction, were not sure of the benefits of medication, and did not believe they needed medication when they felt well.48 In other words, these teens, like adults with poor adherence, did not believe that taking medicine has a substantial benefit.1, 48 Examining and acknowledging health beliefs of older teens in the context of their complicated lives may facilitate discussions about self-management.57
Acknowledgments
Declaration of all sources of funding:
David R. Naimi, DO: AAAAI Sepracor Research Excellence Award
Andrea J. Apter, MD, MSc: HL070392, HL088469
Abbreviations
- DAL
Diskus Adherence Logger
- ED
emergency department
- F/S
fluticasone/salmeterol
- HBM
Health Belief Model
- ICS
inhaled corticosteroids
Footnotes
Clinical Implications:
Adherence to regular inhaled steroid regimens is often poor in older adolescents. Assessing health beliefs and adherence along with asthma control may improve medicine recommendations, foster good communication, and help teens achieve effective self-management.
Contributor Information
David R. Naimi, Division of Allergy and Immunology, The Children’s Hospital of Philadelphia, Philadelphia, PA.
Tovia G. Freedman, Clinical and Research Consultant, Philadelphia, PA.
Kenneth R. Ginsburg, Division of Adolescent Medicine, The Children's Hospital of Philadelphia, Philadelphia, PA.
Daniel Bogen, Department of Bioengineering, University of Pennsylvania, Philadelphia, PA.
Cynthia S. Rand, Pulmonary and Critical Care Medicine, The Johns Hopkins School of Medicine, Baltimore, MD.
Andrea J. Apter, Section of Allergy & Immunology, Division of Pulmonary, Allergy, & Critical Care Medicine, University of Pennsylvania, Philadelphia, PA.
REFERENCES
- 1.Apter AJ, Boston R, George M, Norfleet A, Tenhave T, Coyne JC, et al. Modifiable barriers to adherence to inhaled steroids among adults with asthma: it's not just black and white. J Allergy Clin Immunol. 2003;111:1219–1226. doi: 10.1067/mai.2003.1479. [DOI] [PubMed] [Google Scholar]
- 2.Apter AJ, Reisine ST, Affleck G, Barrows E, ZuWallack RL. Adherence with twice-daily dosing of inhaled steroids. Socioeconomic and health-belief differences. Am J Respir Crit Care Med. 1998;157:1810–1817. doi: 10.1164/ajrccm.157.6.9712007. [DOI] [PubMed] [Google Scholar]
- 3.Rand CS. Patient and regimen-related factors that influence compliance with asthma therapy. Eur Respir Rev. 1998;8:270–274. [Google Scholar]
- 4.Rand CS. Measuring adherence with therapy for chronic diseases: implications for the treatment of heterozygous familial hypercholesterolemia. Am J Cardiol. 1993;72:68D–74D. doi: 10.1016/0002-9149(93)90014-4. [DOI] [PubMed] [Google Scholar]
- 5.Apter AJ, Joffe M, Weber A, George M, Norfleet AL, Cucchiara AJ, et al. Potentially modifiable predictors of adherence with inhaled steroids. Journal of Allergy and Clinical Immunology. 2002;109S:184. [Google Scholar]
- 6.Adams S, Pill R, Jones A. Medication, chronic illness and identity: the perspective of people with asthma. Soc Sci Med. 1997;45:189–201. doi: 10.1016/s0277-9536(96)00333-4. [DOI] [PubMed] [Google Scholar]
- 7.Haynes RB, Taylor DW, Sackett DL. Compliance in Health Care. Baltimore: Johns Hopkins University Press; 1979. [Google Scholar]
- 8.Milgrom H, Bender B, Ackerson L, Bowry P, Smith B, Rand C. Noncompliance and treatment failure in children with asthma. J Allergy Clin Immunol. 1996;98:1051–1057. doi: 10.1016/s0091-6749(96)80190-4. [DOI] [PubMed] [Google Scholar]
- 9.Birkhead G, Attaway NJ, Strunk RC, Townsend MC, Teutsch S. Investigation of a cluster of deaths of adolescents from asthma: evidence implicating inadequate treatment and poor patient adherence with medications. J Allergy Clin Immunol. 1989;84:484–491. doi: 10.1016/0091-6749(89)90361-8. [DOI] [PubMed] [Google Scholar]
- 10.Bruzzese JM, Bonner S, Vincent EJ, Sheares BJ, Mellins RB, Levison MJ, et al. Asthma education: the adolescent experience. Patient Educ Couns. 2004;55:396–406. doi: 10.1016/j.pec.2003.04.009. [DOI] [PubMed] [Google Scholar]
- 11.Akinbami LJ. The State of Childhood Asthma, United States, 1980–2005. Washington: U.S.: Dept of Health and Human Services, National Center for Health Statistics; 2006. [Google Scholar]
- 12.Akinbami LJ, Rhodes JC, Lara M. Racial and ethnic differences in asthma diagnosis among children who wheeze. Pediatrics. 2005;115:1254–1260. doi: 10.1542/peds.2004-0897. [DOI] [PubMed] [Google Scholar]
- 13.Moorman JE, Rudd RA, Johnson CA, King M, Minor P, Bailey C, et al. National surveillance for asthma--United States, 1980–2004. MMWR Surveill Summ. 2007;56:1–54. [PubMed] [Google Scholar]
- 14.Rand CS, Apter AJ. Mind the widening gap: have improvements in asthma care increased asthma disparities? J Allergy Clin Immunol. 2008;122:319–321. doi: 10.1016/j.jaci.2008.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gupta RS, Carrion-Carire V, Weiss KB. The widening black/white gap in asthma hospitalizations and mortality. J Allergy Clin Immunol. 2006;117:351–358. doi: 10.1016/j.jaci.2005.11.047. [DOI] [PubMed] [Google Scholar]
- 16.Ginde AA, Espinola JA, Camargo CA. Improved Trends but Persistent Racial Disparities in Emergency Department Visits for Acute Asthma, 1993–2005. J Allergy Clin Immunol. 2008;122:313–318. doi: 10.1016/j.jaci.2008.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fiese BH, Everhart RS. Medical adherence and childhood chronic illness: family daily management skills and emotional climate as emerging contributors. Curr Opin Pediatr. 2006;18:551–557. doi: 10.1097/01.mop.0000245357.68207.9b. [DOI] [PubMed] [Google Scholar]
- 18.Le TT, Bilderback A, Bender B, Wamboldt FS, Turner CF, Rand CS, et al. Do asthma medication beliefs mediate the relationship between minority status and adherence to therapy? J Asthma. 2008;45:33–37. doi: 10.1080/02770900701815552. [DOI] [PubMed] [Google Scholar]
- 19.McQuaid EL, Kopel SJ, Klein RB, Fritz GK. Medication adherence in pediatric asthma: reasoning, responsibility, and behavior. J Pediatr Psychol. 2003;28:323–333. doi: 10.1093/jpepsy/jsg022. [DOI] [PubMed] [Google Scholar]
- 20.Kyngas HA. Compliance of adolescents with asthma. Nurs Health Sci. 1999;1:195–202. doi: 10.1046/j.1442-2018.1999.00025.x. [DOI] [PubMed] [Google Scholar]
- 21.Logan D, Zelikovsky N, Labay L, Spergel J. The Illness Management Survey: identifying adolescents' perceptions of barriers to adherence. J Pediatr Psychol. 2003;28:383–392. doi: 10.1093/jpepsy/jsg028. [DOI] [PubMed] [Google Scholar]
- 22.Penza-Clyve SM, Mansell C, McQuaid EL. Why don't children take their asthma medications? A qualitative analysis of children's perspectives on adherence. J Asthma. 2004;41:189–197. doi: 10.1081/jas-120026076. [DOI] [PubMed] [Google Scholar]
- 23.van Es SM, Kaptein AA, Bezemer PD, Nagelkerke AF, Colland VT, Bouter LM. Predicting adherence to prophylactic medication in adolescents with asthma: an application of the ASE-model. Patient Educ Couns. 2002;47:165–171. doi: 10.1016/s0738-3991(01)00195-1. [DOI] [PubMed] [Google Scholar]
- 24.van Es SM, le Coq EM, Brouwer AI, Mesters I, Nagelkerke AF, Colland VT. Adherence-related behavior in adolescents with asthma: results from focus group interviews. J Asthma. 1998;35:637–646. doi: 10.3109/02770909809048966. [DOI] [PubMed] [Google Scholar]
- 25.Jonasson G, Carlsen KH, Sodal A, Jonasson C, Mowinckel P. Patient compliance in a clinical trial with inhaled budesonide in children with mild asthma. Eur Respir J. 1999;14:150–154. doi: 10.1034/j.1399-3003.1999.14a25.x. [DOI] [PubMed] [Google Scholar]
- 26.Fiese BH, Wamboldt FS. Tales of pediatric asthma management: family-based strategies related to medical adherence and health care utilization. J Pediatr. 2003;143:457–462. doi: 10.1067/S0022-3476(03)00448-7. [DOI] [PubMed] [Google Scholar]
- 27.Gillibrand R, Stevenson J. The extended health belief model applied to the experience of diabetes in young people. Br J Health Psychol. 2006;11:155–169. doi: 10.1348/135910705X39485. [DOI] [PubMed] [Google Scholar]
- 28.Eisen M, Zellman GL, McAlister AL. A Health Belief Model-Social Learning Theory approach to adolescents' fertility control: findings from a controlled field trial. Health Educ Q. 1992;19:249–262. doi: 10.1177/109019819201900208. [DOI] [PubMed] [Google Scholar]
- 29.Glanz K, Rimer BK, Viswanath K. Health behavior and health education: theory, research, and practice. 4th edition. San Francisco, CA: Jossey-Bass; 2008. [Google Scholar]
- 30.Expert Panel Report II: Guidelines for the Diagnosis and Management of Asthma. Bethesda, MD: Public Health Service, National Institutes of Health, National Heart, Lung, and Blood Institute; 1997. Publication 97–4051. [Google Scholar]
- 31.Expert Panel Report: Guidelines for the Diagnosis and Management of Asthma. Update on Selected Topics. J Allergy Clin Immunol. 2002;110:S141–S218. [PubMed] [Google Scholar]
- 32.Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. J Allergy Clin Immunol. 2007;120:S94–S138. doi: 10.1016/j.jaci.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 33.Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma, Full Report 2007. U.S. Department of Health and Human Services, National Institutes of Health, National Heart, Lung and Blood Institute; 2007. [Google Scholar]
- 34.Giacomini MK, Cook DJ. Users' guides to the medical literature: XXIII. Qualitative research in health care A. Are the results of the study valid? Evidence-Based Medicine Working Group. Jama. 2000;284:357–362. doi: 10.1001/jama.284.3.357. [DOI] [PubMed] [Google Scholar]
- 35.National Asthma Education and Prevention Program Expert Panel Report: Guidelines for the Diagnosis and Management of Asthma - Update on Selected Topics. J Allergy Clin Immunol. 2002;110:S141–S219. [PubMed] [Google Scholar]
- 36.Bogen D, Apter AJ. Adherence logger for a dry powder inhaler: a new device for medical adherence research. J Allergy Clin Immunol. 2004;114:863–868. doi: 10.1016/j.jaci.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 37.Bureau USC, editor. Anon. American FactFinder. Washington, DC: U.S. Census Bureau; 2000. [Google Scholar]
- 38.Standardization of Spirometry, 1994 Update. American Thoracic Society. Am J Respir Crit Care Med. 1995;152:1107–1136. doi: 10.1164/ajrccm.152.3.7663792. [DOI] [PubMed] [Google Scholar]
- 39.Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26:948–968. doi: 10.1183/09031936.05.00035205. [DOI] [PubMed] [Google Scholar]
- 40.George M, Freedman TG, Norfleet AL, Feldman HI, Apter AJ. Qualitative research-enhanced understanding of patients' beliefs: results of focus groups with low-income, urban, African American adults with asthma. J Allergy Clin Immunol. 2003;111:967–973. doi: 10.1067/mai.2003.1459. [DOI] [PubMed] [Google Scholar]
- 41.Rand CS, Wise RA, Nides M, Simmons MS, Bleecker ER, Kusek JW, et al. Metered-dose inhaler adherence in a clinical trial. Am Rev Respir Dis. 1992;146:1559–1564. doi: 10.1164/ajrccm/146.6.1559. [DOI] [PubMed] [Google Scholar]
- 42.Bogen D, Apter AJ. An adherence logger for a dry-powder inhaler: a new device for medical adherence research. J Allergy Clin Immunol. 2004;114:863–868. doi: 10.1016/j.jaci.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 43.Bender B, Wamboldt FS, O'Connor SL, Rand C, Szefler S, Milgrom H, et al. Measurement of children's asthma medication adherence by self report, mother report, canister weight, and Doser CT. Ann Allergy Asthma Immunol. 2000;85:416–421. doi: 10.1016/s1081-1206(10)62557-4. [DOI] [PubMed] [Google Scholar]
- 44.George M, Apter AJ. Gaining insight into patients' beliefs using qualitative research methodologies. Curr Opin Allergy Clin Immunol. 2004;4:185–189. doi: 10.1097/00130832-200406000-00008. [DOI] [PubMed] [Google Scholar]
- 45.Krueger RA, Casey MA. Focus Groups: A practical guide for applied research. 3 ed. Thousand Oaks, CA: Sage Publisher; 2000. [Google Scholar]
- 46.Power R. The application of qualitative research methods to the study of sexually transmitted infections. Sex Transm Infect. 2002;78:87–89. doi: 10.1136/sti.78.2.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Byrne M. Grounded theory as a qualitative research methodology. Aorn J. 2001;73:1155–1156. doi: 10.1016/s0001-2092(06)61841-3. [DOI] [PubMed] [Google Scholar]
- 48.George M, Freedman TG, Norfleet AL, Feldman HI, Apter AJ. Qualitative research enhanced understanding of patients' beliefs: results of focus groups with low-income urban African American adults with asthma. J Alllergy Clin Immunol. 2003;111:967–973. doi: 10.1067/mai.2003.1459. [DOI] [PubMed] [Google Scholar]
- 49.Rubinfeld AR, Pain MC. Perception of asthma. Lancet. 1976;1:882–884. doi: 10.1016/s0140-6736(76)92097-3. [DOI] [PubMed] [Google Scholar]
- 50.Bacharier LB, Strunk RC, Mauger D, White D, Lemanske RF, Jr, Sorkness CA. Classifying asthma severity in children: mismatch between symptoms, medication use, and lung function. Am J Respir Crit Care Med. 2004;170:426–432. doi: 10.1164/rccm.200308-1178OC. [DOI] [PubMed] [Google Scholar]
- 51.Jenkins HA, Cherniack R, Szefler SJ, Covar R, Gelfand EW, Spahn JD. A comparison of the clinical characteristics of children and adults with severe asthma. Chest. 2003;124:1318–1324. doi: 10.1378/chest.124.4.1318. [DOI] [PubMed] [Google Scholar]
- 52.Horak E, Grassl G, Skladal D, Ulmer H. Lung function and symptom perception in children with asthma and their parents. Pediatr Pulmonol. 2003;35:23–28. doi: 10.1002/ppul.10218. [DOI] [PubMed] [Google Scholar]
- 53.Fuhlbrigge AL, Weiss ST, Kuntz KM, Paltiel AD. Forced expiratory volume in 1 second percentage improves the classification of severity among children with asthma. Pediatrics. 2006;118:e347–e355. doi: 10.1542/peds.2005-2962. [DOI] [PubMed] [Google Scholar]
- 54.Sears MR, Greene JM, Willan AR, Wiecek EM, Taylor DR, Flannery EM, et al. A longitudinal, population-based, cohort study of childhood asthma followed to adulthood. N Engl J Med. 2003;349:1414–1422. doi: 10.1056/NEJMoa022363. [DOI] [PubMed] [Google Scholar]
- 55.Ellis DA, Podolski CL, Frey M, Naar-King S, Wang B, Moltz K. The role of parental monitoring in adolescent health outcomes: impact on regimen adherence in youth with type 1 diabetes. J Pediatr Psychol. 2007;32:907–917. doi: 10.1093/jpepsy/jsm009. [DOI] [PubMed] [Google Scholar]
- 56.Onyirimba F, Apter AJ, Reisine ST, McCucsker C, Connors ML, ZuWallack RL. Direct Clinician-to-Patient Feedback of Inhaled Steroid Use: Its Effect on Adherence and Asthma Outcome. Annals of Allergy and Asthma Immunology. 2003;90:411–415. doi: 10.1016/S1081-1206(10)61825-X. [DOI] [PubMed] [Google Scholar]
- 57.van Es SM, Nagelkerke AF, Colland VT, Scholten RJ, Bouter LM. An intervention programme using the ASE-model aimed at enhancing adherence in adolescents with asthma. Patient Educ Couns. 2001;44:193–203. doi: 10.1016/s0738-3991(00)00195-6. [DOI] [PubMed] [Google Scholar]