Abstract
Endoscopic papillary balloon dilation (EPBD) is an alternative method of endoscopic sphincterotomy (EST). Although concerns regarding post-procedure pancreatitis have been expressed, EPBD has come to be recognized as an effective and safe method for stone removal in specific cases. To analyze the proper indications, ideal methods, complications, and long-term follow-up results for EPBD, we reviewed articles about EPBD located through a search of the PubMed data base. We analyzed the ballooning methods, indications, results and complications of EPBD among the articles found and compared the results with those of EST. We considered the authors' own clinical experience and knowledge in developing recommendations for EPBD. EPBD showed similar efficacy and safety for the removal of choledocholithiasis to that of EST. Although large or multiple stones were difficult to remove by EPBD, it was safer and easier to apply in patients with coagulopathy or abnormal anatomy. To prevent severe pancreatitis, excessive ballooning and impractical cannulation should be avoided, and precut sphincterotomy or adjuvant prophylaxis should be considered. Due to its preservation of the sphincter of Oddi, EPBD is expected to have fewer long-term complications, such as stone recurrence, cholangitis and cholecystitis. In conclusion, EPBD appears to be safe and effective for the treatment of choledocholithiasis with proper selection of ballooning methods and patients.
Keywords: Choledocholithiasis, Endoscopic papillary balloon dilation, Endoscopic sphincterotomy, Endoscopic papillary large balloon dilation
INTRODUCTION
Before endoscopic retrograde cholangiopancreatography (ERCP) and sphincterotomy was introduced in the 1970s, there was no other choice than surgery for the treatment of choledocholithiasis except. After Classen et al.1 and Kawai et al.2, first introduced endoscopic sphincterotomy (EST), the endoscopic removal of stones has been widely accepted as a standard treatment for bile duct stones. Moreover, advances in intraductal lithotripsy techniques, such as mechanical basket lithotripsy and electrohydraulic lithotripsy, have made it easier to fragment large stones. Although the safety of EST has been proven in many studies, there are still several limitations on its applications due to complications: pancreatitis (5.4%), hemorrhage (2.0%), perforation (0.3%), cholangitis (1.0%), cholecystitis (0.5%), and procedure-related death (0.4%).3 Bleeding after EST should be carefully monitored in patients with coagulopathy because of its high mortality (24.3-22.2%).4-6 Recurrence of stones and chronic biliary inflammation were also associated with loss of ampulla of Vater function.7-9 There have been many efforts to decrease the occurrence of these complications as much as possible.
Endoscopic papillary balloon dilation (EPBD) is almost the only existing alternative to EST. Although it was not welcomed in Western groups because of complications, it has come into wide usage in Korea and Japan. Nowadays, an extended technique of EPBD, endoscopic papillary large balloon dilatation (EPLBD) with limited sphincterotomy, is successfully used for stone removal.
To maximize the effects and minimize the complications of endoscopic lithotripsy, it is important to recognize the proper indications and to apply the technique in a proper manner. In this paper, we reviewed articles about EPBD by searching PubMed for making suggestions on the appropriate use of EPBD. We analyzed the ballooning methods, indications, results and complications of EPBD among the articles, and compared the results with those of EST. We considered the authors' own clinical experience and knowledge in developing recommendations for EPBD.
EPBD
EPBD was presented for the first time by Staritz et al.10, in order to minimize damage to the sphincter of Oddi. Following selective deep cannulation, the balloon catheter was placed across the papillary orifice and gradually inflated with diluted contrast material at a pressure of 8-12 atm. The sphincter was adequately dilated if the waist in the balloon completely disappeared. The fully inflated balloon was maintained in its position for dozens of seconds, and then deflated. The procedure can be repeated for complete dilation. Various sizes of balloon catheter with 6-15 mm in diameter and 30-40 mm in length can be used according to the bile duct diameter and stone size. The velocity and duration of balloon inflation varied from seconds to minutes. After EPBD, the stones were extracted using a Dormia basket and/or a retrieval balloon catheter (Fig. 1).
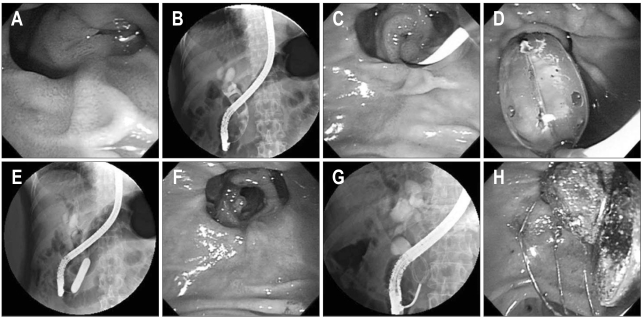
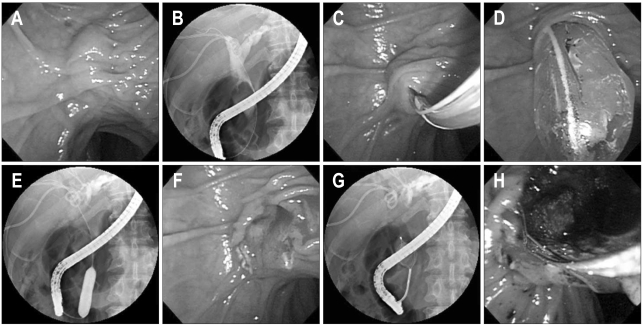
Fig. 1.
Endoscopic papillary balloon dilation (EPBD) for choledocholithiasis with perivater diverticulum. (A) Duodenoscopic finding shows an ampulla of Vater located in a diverticulum. (B) ERCP shows multiple stones in the common bile duct. (C) The guidewire is inserted into the bile duct. (D) The 10 mm balloon is gradually inflated with diluted contrast material; inflation is maintained for 30 seconds. (E) X-ray during balloon dilation shows complete disappearance of the sphincter waist. (F) Duodenoscopic finding after EPBD shows a well-visualized common bile duct with a large dilated opening of the sphincter of choledochus. (G) ERCP shows a stone grasped by a mechanical lithotripter. (H) Duodenoscopic finding shows stones removed from the common bile duct by a Dormia basket.
1. Advantages
1) EPBD has several advantages over EST
First, it is less traumatic to the ampullary sphincter, which was proven in both animal and human studies. The resected specimens of pigs, obtained immediately after EPBD, showed only acute inflammation and intramucosal hemorrhage without smooth muscle disruption on histological analysis.11 Even after several weeks, no architectural distortion or smooth muscle disruption was noted. In human studies, histological analysis of the papilla after EPBD showed only mild to moderate inflammation and fibrosis in most patients (80-90%), while no smooth muscle disruption nor architectural distortion was observed.12,13
Second, EPBD may preserve papillary function. After EPBD, a mild decrease in papillary function was noted on manometry without significant difference. On the other hand, all patients who had received EST completely lost papillary function.14 Papillary function began to return to normal only a month after EPBD, and the basal and peak pressures of the sphincter of Oddi (SO) had significantly recovered by that time as compared with the data immediately after EPBD.15 In contrast, SO contraction did not recover even after one year after EST.16 Because the cutting method was unnecessary, the SO function was not completely lost after EPBD.
Third, EPBD was shown to be safer for patients with bleeding tendency. Coagulopathy under liver cirrhosis, portal hypertension or administration of anticoagulation is a known risk factor for EST-related bleeding.3,17 Because EPBD can avoid an incision, it may significantly reduce the bleeding risk and mortality in patients with liver cirrhosis and coagulopathy.18-20
Finally, it is favorable for those with abnormal anatomy, such as periampullary diverticulum and Billroth II gastrojejunostomy. EST is technically difficult in patients with periampullary diverticulum or Billroth II gastrojejunostomy because the cutting direction of the sphincterotome is not easy to control. Therefore a high level of precision in the direction and length of the incision is necessary to avoid severe complication. In contrast, EPBD requires simple technique to insert the balloon catheter into the common bile duct and inflate it. Therefore, EPBD is more suitable for the patients with periampullary diverticulum or Billroth II gastrojejunostomy.21 Komatsu et al.20 reported on their experience of EPBD in 226 patients, and EPBD was successful in 86 patients (38.0%) with periampullary diverticulum and in two patients who had previously undergone Billroth II gastrectomy.
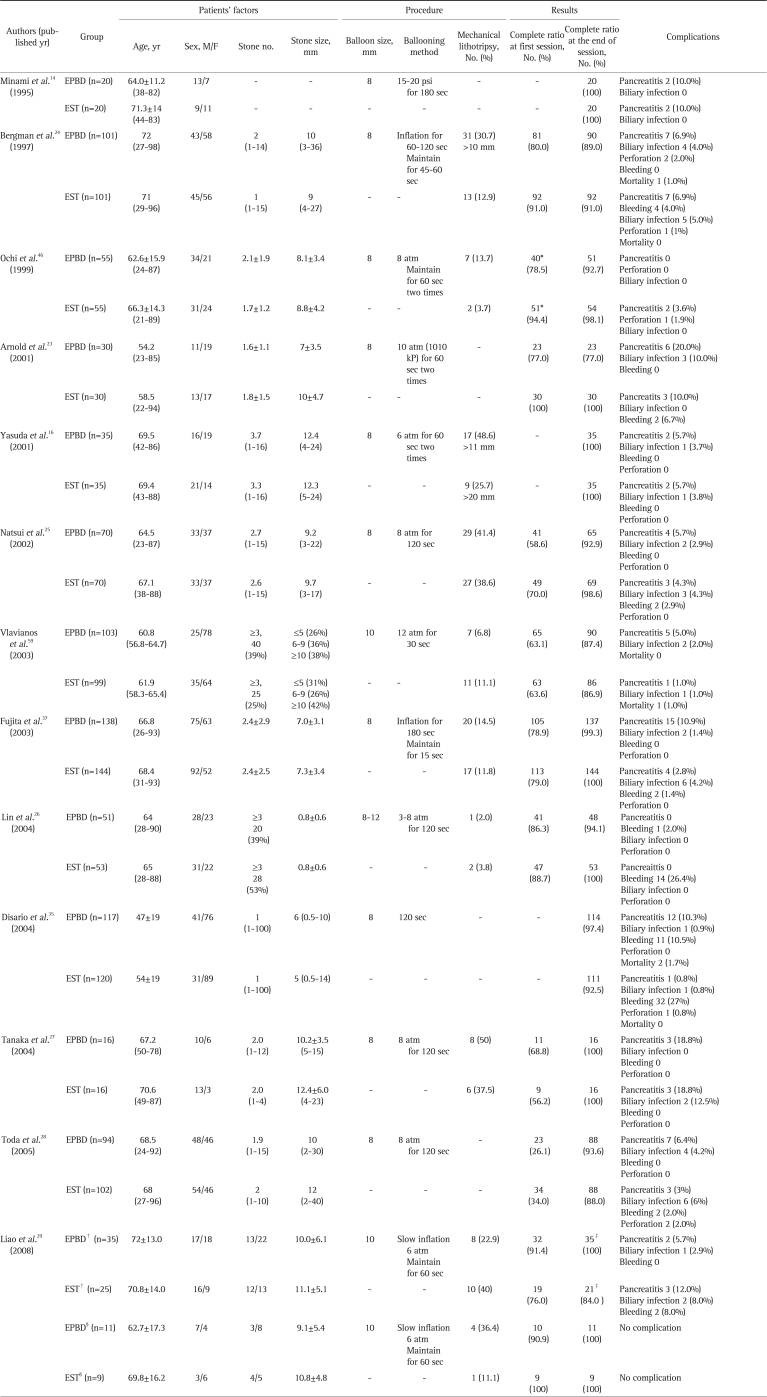
2. Comparison of success rates between EPBD and EST for removal of choledocholithiasis (Table 1)
Table 1.
Comparisons between EPBD and EST for Removal of Choledocholithiasis
Biliary infection included cholangitis and cholecystitis.
EPBD, endoscopic papillary balloon dilation; EST, endoscopic sphincterotomy.
*p=0.02; †In the patients with periampullary diverticulum; ‡p=0.026; §In the patients with prior sphincterotomy history.
There have been many trials comparing the efficacy and safety of EPBD with EST. According to the meta-analysis of eight randomized, controlled studies, the overall success rate for stone removal was similar in the two groups (94.3% vs 96.5%, p=0.2), but the completion rate for the first session was significantly higher in the EST group than in the EPBD group (79.8% vs 70.0%, p=0.001).22 Mechanical lithotripsy was also needed significantly more often in the EPBD group in that study (20.9% vs. 14.8%, p=0.01). In 23% of patients who had failed stone removal with EPBD at the first session, the additional EST as a rescue procedure contributed to raising the overall success rate of the EPBD group.23 Another study also showed that 9% of the EPBD group needed the additional EST.24
Large or multiple stones are more difficult to remove using EPBD because the biliary opening is not wide enough. The difference of initial success rate between the EPBD and EST group was widened in difficult cases, such as stones of larger than 10 mm in diameter or four or more stones (70.0% vs 83.0%); these cases needed more mechanical lithotripsy in the EPBD group (50.0% vs 23.0%, p<0.01).24 For patients with stones over 10 mm in diameter, EPBD required a significantly larger mean number of treatment sessions than EST (2.4 vs 1.6, p<0.05).25 Multiple or larger stones also required the additional EST in 13% of patients, while smaller and fewer stones did so in 3% of patients.24 On the other hand, studies limited to stones smaller than 2.0 cm in diameter showed that not only overall success rate but also initial success rate and requirement of mechanical lithotripsy to be similar in both groups.26 Tanaka et al.27 also reported that EPBD was more effective in cases with small-sized (≤15 mm) and small numbers (≤3) of stones (100% vs 55.6%, p<0.05). However, Toda et al.28 reported that the initial and overall success rates with EPBD were comparable to that of EST, regardless of stone size.
When EST was difficult to apply due to periampullary diverticulum or prior EST, EPBD was easier and safer than EST.29
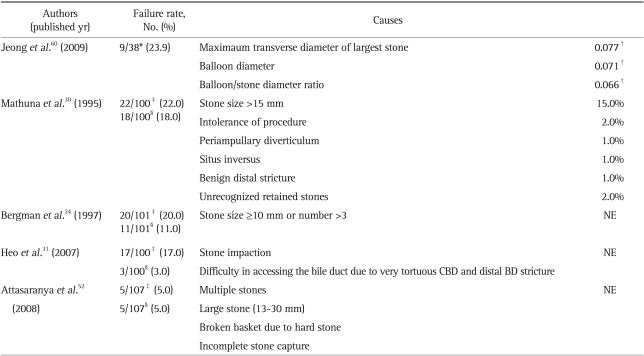
3. Causes for failure to remove choledocholithiasis (Table 2)
Table 2.
The Causes of Failure of EPBD/EPLBD for Removal of Choledocholithiasis
EPBD, endoscopic papillary balloon dilation; EPLBD, endoscopic papillary large balloon dilation; NE, not evaluated; CBD, common bile duct; BD, bile duct.
*Application of mechanical lithotripsy or failure to extract stone; †p-value; ‡Failure at first session; §Overall failure.
The maximum diameter of the stones affects complete stone removal, especially when larger than 15 mm in length. Patients' intolerance to the procedure, unrecognized retained stones and anatomic problem such as periampullary diverticulum, situs inversus and benign distal stricture make it difficult to clear stones completely.30 Tortuous common bile duct and distal bile duct stricture also interfere with accessing the bile duct.31 In situations where deep cannulation to the bile duct may have failed, precut sphincterotomy was one of the most effective methods. Dilating the balloon immediately after the precut sphincterotomy became the method of choice before EPBD when deep cannulation failed.
4. Complications
1) Post-EPBD pancreatitis
Pancreatitis is one of the most fearful post-ERCP complication, and occurred in 5-19.8% after EPBD.13,20,30,32,33 Because of the significant occurrence of complications, Kozarek34 insisted that EPBD should not replace EST. A randomized controlled study was finished prematurely due to excessive morbidity in the EPBD group (20.0% vs 10.0%).23 Another randomized, controlled multicenter trial was also terminated early at the first interim analysis, because two patients died from severe pancreatitis as a complication of EPBD.35 Actually, meta-analysis demonstrated that post-ERCP pancreatitis occurred more commonly in the EPBD group than in the EST group (7.4% vs 4.3%, p=0.05).22 The authors thought that the balloon dilation of the sphincter of Oddi may have been causing spasm, compression and edema of the distal pancreatic duct, resulting in restricted flow of pancreatic juice and causing pancreatitis, biliary obstruction and cholangitis. To minimize the damage on papilla, two different methods of balloon inflation were tried; rapid inflation and maintenance for 120 seconds and slow inflation and maintenance for 15 seconds. However, the incidences of pancreatitis did not differ significantly between the two methods (73.3% vs 60.6%, p=0.3220).32 A larger balloon (10 to 15 mm) may cause more compression and edema of the distal pancreatic duct, thus precipitating pancreatitis. Smaller balloons of less than 8mm may be safer and more effective in the management of bile duct stones, and decrease the incidence of pancreatitis.30,36 Balloon dilation in a stepwise fashion, avoiding rapid application and excessive pressure, may also contribute to decreasing the occurrence of the post-EPBD pancreatitis.37
According to another study, previous pancreatitis history is one of the most significant factor of EPBD related pancreatitis (odds ratio [OR], 10.69; 95% confidence interval [CI], 1.57-72.97).36 In contrast, another study revealed that history of acute pancreatitis was not identified as a risk factor, but that contrast medium injection to the pancreas was a significant risk factor by multivariate analysis (OR, 3.788; 95% CI, 1.036-13.853).32
As Chinese study showed younger age to be a significant risk factor for post-ERCP pancreatitis (OR, 1.59; 95% CI, 1.06-2.39).38 The progressive decline in pancreatic exocrine function that comes with aging may protect older patients from pancreatic injury.39 However, there was no significant difference in the incidence of post-EPBD pancreatitis between older and younger patients.32,36 However, age of younger than 60 years demonstrated relevance to asymptomatic hyperamylasemia.36
Total procedure time, sex, periampullary diverticulum, mechanical lithotripsy, non-dilated bile duct and difficult cannulation were found not to be significant by univariate and multivariate analysis.32,36 However, cannulation trauma might result in spasm of the sphincter of Oddi and/or hemorrhagic edematous change,33 and was a potential risk factor for asymptomatic hyperamylasemia after EPBD (OR, 5.12; 95% CI, 2.79-16.81).36 In cases of difficult cannulation, minimal EST before standard endoscopic balloon dilation may be recommended. Since EST may direct the force exerted by the dilating balloon to be directed more toward the common bile duct than the pancreatic duct, it may decrease the risk of pancreatitis.40
Several methods were suggested for preventing EPBD-related pancreatitis. Gabexate mesylate may reduce the incidence of especially moderate or severe pancreatitis.41 Insertion of a pancreatic stent,42 epinephrine irrigation after EPBD,43 isosorbide dinitrate infusion,44 and injection of botulinum toxin to lower the pancreatic sphincter pressure45 may augment pancreatic drainage. However these adjuvant interventions also present potential for complications, and their time or cost-effectiveness remains questionable.
2) Bleeding
As stated above, EPBD has little theoretical risk of bleeding, and clinically significant bleeding which was defined as continuous bleeding after procedure or conditions requiring transfusion and additional intervention for hemostasis, is rarely reported after EPBD. Meta-analysis showed no episode of bleeding in the EPBD group, whereas it was noted in 2.0% of the EST group.22 In case of self-limited or endoscopically controlled bleeding, the incidence was significantly higher in EST group (27%) than in EPBD group (10.5%).35
3) Perforation
Although meta-analysis showed no significant difference in the perforation rate between the EPBD and EST groups,22 only one study reported two retroperitoneal perforations after EBPD,24 whereas four studies reported five perforations after EST.24,28,35,46 EPBD does not appear to increase the rate of perforation compared with EST.
4) Abdominal pain during inflation of the balloon
During inflation of the balloon, 23.5-50% of patients felt abdominal pain or discomfort. However this adverse effect was temporary and got better by a reduction in balloon pressure and duration.20,26,30
5) Cholangitis and cholecystitis
Acute cholangitis within 15 days after procedure occurred only in the EST group (12.5%).27 Acute cholecystitis developed more often in the EST group than in the EPBD group (9.9% vs 1.3%, p<0.05). This may be explained by loss of sphincter function after EST, which enables bacteria colonization from the intestine into the biliary system.24
6) Gallstone ileus
Gallstone ileus is an extremely rare complication of ERCP and EST.47 Advanced age, a history of prior small bowel resection and stricture are a possible causes of intestinal obstruction by the passed stone via widened orifice of the sphincter.48 Unlike EST, EPBD can preserve the sphincter of Oddi and thus decrease the risk of gallstone ileus. However, there is the possibility of small bowel obstruction by the stones extracted during the ERCP. Thus, it is recommended that large stones be removed after pulverization by mechanical lithotripsy.
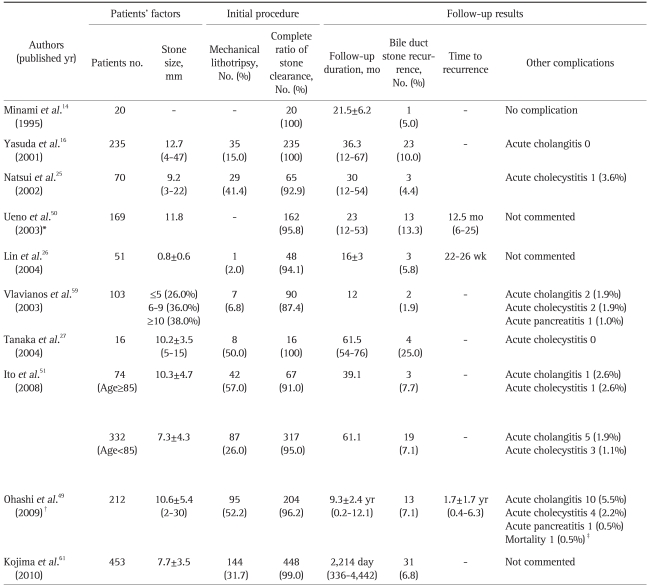
5. Long-term follow-up results (Table 3)
Table 3.
Long Term Follow-Up Results of EPBD
The size of the balloon used in the endoscopic papillary balloon dilation (EPBD) procedures was approximately 8 mm, except in studies performed by Lin et al. (8 to 12 mm) and Vlavianos et al. (10 mm).
All of the patients were followed up, except in the studies of Natsui et al. (68, 97.1%), Ueno et al. (98, 58%), and Ohashi et al. (182, 89.2%).
Prognostic factors were determined by multivariate analysis.
*Bile duct diameter>20 mm (relative risk 6.83) and diverticulum (relative risk 6.88); †Previous cholecystectomy (odds ratio 4.8), bile duct diameter>15 mm (odds ratio 4.4) and confirmation using IDUS (odds ratio 11.2); ‡Mortality was related to gallstone pancreatitis.
Little is known about long-term complications of EPBD. A Japanese study with a mean overall follow-up duration of 9.3 years (7.0-12.1 years) demonstrated that 22 patients (12.1%) of 182 experienced 33 biliary complications during the follow-up period; stone recurrences in 13 patients (7.1%), stone migration from the gallbladder in 5 patients (2.7%), acute cholangitis in 10 patients (5.5%), acute cholecystitis in 4 patients (2.2%), and fatal gallstone pancreatitis in one patient (0.5%).49 Approximately 85% of recurring bile duct stones occurred within 3 years after EPBD. All recurring stones were bilirubinate, and the majority of patients (92.3%) with stone recurrence did not have pneumobilia. Previous cholecystectomy (OR, 4.813; 95% CI, 1.237-18.726), dilated bile duct of more than 15 mm in width (OR, 4.433; 95% CI, 1.084-18.117) and no confirmation of clean duct using IDUS (OR, 11.197; 95% CI, 2.170-57.771) were significant risk factors for stone recurrence according to multivariate analysis. Although periampullary diverticulum was noted as a risk factor in another study with mid-term follow-up period (mean 23 moths),50 it was not significant in this long-term follow-up study. Age, sex, large stone, multiple stones, multiple endoscopic sessions and mechanical lithotripsy were not associated with stone recurrence in this study, either. Between the patients younger and older than 85 years of age, there was no significantly difference in overall complications, such as cumulative stone recurrence rate (7.1% vs 7.7%, p=0.6225), acute cholangitis (1.9% vs 2.6%, p=0.7711) and acute cholecystitis (1.1% vs 2.6%, p=0.4594) during the follow-up period (mean, 61.1 months vs 39 months).51 Remnant GB stone was one of the factors related with biliary stone recurrence. During a mean follow-up of 2,214 days, recurrence was observed more frequently in the group with GB stones.
There were several comparative studies of mid-term and long-term complications between the EPBD and EST groups. During a mean follow-up of 16 months, common bile duct stones recurred at a similar rate in both groups (5.8% at 22-26 weeks vs 7.5% at 12-48 weeks).26 Another study compared early, mid-term and late complications of the procedure. Within 1 year of follow-up, bile duct stones recurred more frequently in the EPBD group (25.0%) than in the EST group (6.3%). On the contrary, if the follow-up period was longer than one year, stone recurrences were more common in EST group (26.7%) than the EPBD group (6.3%). A larger post-EST papillary opening facilitated spontaneous passage of small biliary duct stones. However, other factors may contribute to stone recurrence in long-term follow-up after EST, for example repeated reflux of intestinal juice to the bile duct from the duodenum. Preservation of sphincter function might prevent the stone recurrence beyond the early post procedure period.27 After one year, SO function was not restored in the EST group, while it was significantly recovered in the EPBD group.16 The preservation of SO function prevents the later biliary complications. When follow-ups were done for about 3 years in the EPBD and EST groups, pneumobilia appeared at a significantly higher rate in the EST group (40.0%) than in the EPBD group (8.9%) (p<0.01). Similarly, cholecystitis was observed significantly more often in the EST group (18.8%) than in the EPBD group (4.7%) (p<0.05). Significant difference was found between the two groups with the regard to the cumulative incidence of biliary complications (p<0.05).
EPLBD
Because EPBD showed limited success rate in cases of large bile duct stones, EPLBD was attempted in 2003 by Ersoz et al.40 Prior to balloon dilation of the sphincter, a small sphincterotomy incision was made from the orifice of the papilla proximally to the transverse fold. A large-diameter balloon catheter (12-20 mm) was introduced into the bile duct and gradually inflated with diluted contrast medium until the waist of balloon was disappeared, and maintained in position for a dozens of seconds (Fig. 2).
Fig. 2.
Endoscopic papillary large balloon dilation (EPLBD) with limited sphincterotomy. (A) Duodenoscopic finding shows an ampulla of Vater. (B) ERCP shows a large stone in the common bile duct and percutaneous transhepatic biliary drainages placed in the right hepatic lobe. (C) A pull-type sphincterotome is inserted into the bile duct along the guidewire. The biliary sphincter is incised by electrocautery with the bowed cutting wire. (D, E) The 15 mm sized large balloon is gradually inflated with diluted contrast material; inflation is maintained for 30 seconds. (F) Duodenoscopic finding after EPLBD shows a well-visualized common bile duct with a large, dilated opening of the sphincter of choledochus. (G) ERCP shows a large stone grasped by a mechanical lithotripter. (H) Duodenoscopic finding shows stones removed from the common bile duct by a Dormia basket.
EPLBD enlarged the biliary orifice enough to facilitate removal of multiple and larger stones, resulting in a decreased use of mechanical lithotripsy and increased rate of stone removal. According to reports on the efficacy of EPLBD with EST, the complete rates of bile duct stone at first and final session were 72-100% and 95-100%, respectively (Table 4).31,40,52-58
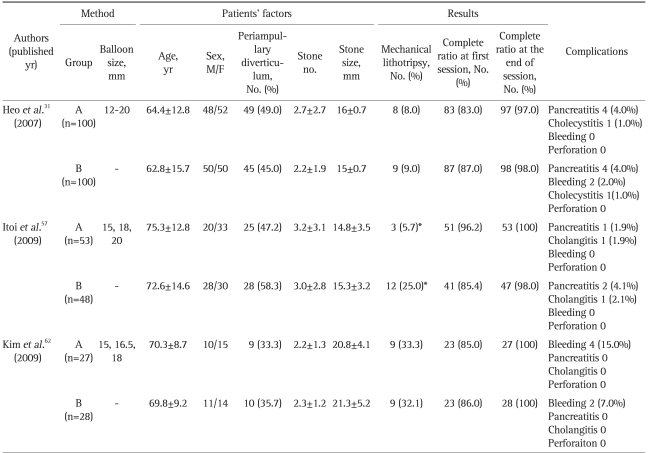
Table 4.
Comparisons between EPLBD with EST (Group A) and EST Alone (Group B) for Removal of Choledocholithiasis
EPLBD, endoscopic papillary large balloon dilatation; EST, endoscopic sphincterotomy.
*p<0.01.
Even though the stone is large, the less mechanical lithotripsy was needed with large diameter balloon plus sphincterotomy. The largest stone in the studies was up to 30 mm in diameter.52,56 When EPLBD with a 13 mm sized balloon was used to remove the 10-30 mm sized stones, the overall success rate was 95% as usual, but mechanical lithotripsy was required in 27.0% of the cases.52 On the other hand, when larger balloons of up to 15 mm in size were used for the removal of 6-30 mm sized stones, the overall success rate was 95% and the mechanical lithotripsy was required in only 4.5% of the cases.56
The efficacy of stone removal in EPLBD plus EST as compared with that of EST alone was similar. The initial success rate of EPLBD plus EST was higher than that of EST (96.2% vs 85.4%), which showed marginal statistical significance (p=0.057). Stone fragmenting by mechanical lithotripsy disturbed complete clearance and prolonged the procedure time. Because combining of EPLBD and EST reduces the need for mechanical lithotripsy (5.7% vs 25.0%, p<0.01), it effectively reduces the total procedure time (31.6±8.8 seconds vs 40.2±16.3 seconds, p<0.05) and radiation exposure (13.1±6.6 seconds vs 21.9±14.7 seconds. p<0.05).57 The complete duct clearances in cases of stones larger than 15 mm were not significantly different between EPLBD plus EST and EST alone (94.4% vs 96.7%, p=0.569) (Table 5).31 Mechanical lithotripsy or repetitive procedure were in fact less necessary in EPLBD plus EST. EPLBD may decrease the risks of EST and clear away larger stones in cases with difficult anatomies.
Table 5.
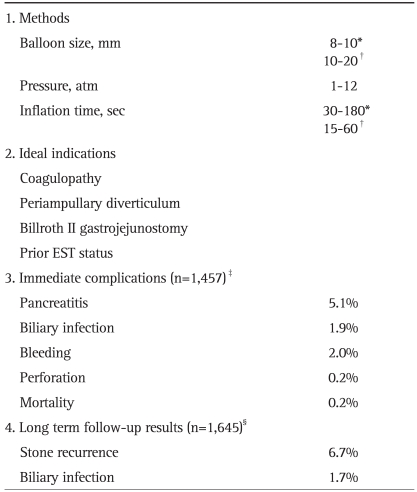
Summary of EPBD and EPLBD
Biliary infection included cholangitis and cholecystitis.
EPBD, endoscopic papillary balloon dilation; EPLBD, endoscopic papillary large balloon dilatation; EST, endoscopic sphincterotomy.
*EPBD; †EPLBD; ‡These results were calculated from total 23 articles (13 for EPBD and 10 for EPLBD);15,16,23-29,31,35,37,40,46,52-59,62 §These results were calculated from total 8 articles.16,26,27,49-51,59,61
Theoretically, it is feared that large size balloon dilation could cause perforation or fatal pancreatitis, however there is only one report of cystic duct perforation52 and none of fatal pancreatitis. On the other hands, in patients with coagulopathy who have a great risk of bleeding after EST, compression by ballooning seems to be effective for hemostasis. There are some concerns that the sphincter of Oddi could be destroyed by large sized-balloon. For lack of long-term results, we have little information of stone recurrence or cholangitis after EPLBD.
EPLBD plus EST be applied to anatomically difficult cases without critical complications but should also be confirmed by long-term follow-up studies.
CONCLUSIONS
EPBD and EPLBD seem to be safe and effective for the treatment of bile duct stones although mechanical lithotripsy is more frequently needed than in EST. Due to the preservation of SO function, EPBD seems to present less at risk of long term complications, such as stone recurrence, cholangitis and cholecystitis than EST. Although concerns were presented about post-procedure pancreatitis, recent reports have demonstrated that EPBD can be successfully and safely used for removal of small size and small unmber of stones. In patients with a higher risk of bleeding or an abnormal anatomy (periampullary diverticulum, Billrothe II gastrojejunostomy and prior EST status), EPBD is safer than EST. The most important ways to avoid severe complications are proper balloon size according to bile duct width and a wake-up not to excessively increase balloon pressure. When there are high risk factors of post ERCP panceatitis (young patients, previuos history of pancreatitis, and so on), balloon size should be as small as possible and adjuvant prophylaxis (pancreatic duct stent, gabexate mesylate, and so on) could be considered. In case of difficult cannulation, impractical cannulation should be avoided and minimal EST before balloon dilation is recommended. EPLBD could be useful adjuvant in patients with very large bile duct stones. We summarize the indications, methods, and complications of EPBD and EPLBD in Table 5. In the near future, making a guide-line for endoscopic management of bile duct stones according to the individual patient's characteristics (e.g., age, coagulopathy, previous history of EST, pancreatitis and gastric operation) and bile duct stone characteristics (e.g., size, number) will be helpful to gastroenterologist.
References
- 1.Classen M, Demling L. Endoscopic sphincterotomy of the papilla of vater and extraction of stones from the choledochal duct (author's transl) Dtsch Med Wochenschr. 1974;99:496–497. doi: 10.1055/s-0028-1107790. [DOI] [PubMed] [Google Scholar]
- 2.Kawai K, Akasaka Y, Murakami K, Tada M, Koli Y. Endoscopic sphincterotomy of the ampulla of Vater. Gastrointest Endosc. 1974;20:148–151. doi: 10.1016/s0016-5107(74)73914-1. [DOI] [PubMed] [Google Scholar]
- 3.Freeman ML, Nelson DB, Sherman S, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909–918. doi: 10.1056/NEJM199609263351301. [DOI] [PubMed] [Google Scholar]
- 4.Moreira VF, Arribas R, Sanroman AL, et al. Choledocholithiasis in cirrhotic patients: is endoscopic sphincterotomy the safest choice? Am J Gastroenterol. 1991;86:1006–1010. [PubMed] [Google Scholar]
- 5.Sugiyama M, Atomi Y, Kuroda A, Muto T. Treatment of choledocholithiasis in patients with liver cirrhosis. Surgical treatment or endoscopic sphincterotomy? Ann Surg. 1993;218:68–73. doi: 10.1097/00000658-199307000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chijiiwa K, Kozaki N, Naito T, Kameoka N, Tanaka M. Treatment of choice for choledocholithiasis in patients with acute obstructive suppurative cholangitis and liver cirrhosis. Am J Surg. 1995;170:356–360. doi: 10.1016/s0002-9610(99)80303-1. [DOI] [PubMed] [Google Scholar]
- 7.Geenen JE, Toouli J, Hogan WJ, et al. Endoscopic sphincterotomy: follow-up evaluation of effects on the sphincter of Oddi. Gastroenterology. 1984;87:754–758. [PubMed] [Google Scholar]
- 8.Bergman JJ, van Berkel AM, Groen AK, et al. Biliary manometry, bacterial characteristics, bile composition, and histologic changes fifteen to seventeen years after endoscopic sphincterotomy. Gastrointest Endosc. 1997;45:400–405. doi: 10.1016/s0016-5107(97)70151-2. [DOI] [PubMed] [Google Scholar]
- 9.Bergman JJ, van der Mey S, Rauws EA, et al. Long-term follow-up after endoscopic sphincterotomy for bile duct stones in patients younger than 60 years of age. Gastrointest Endosc. 1996;44:643–649. doi: 10.1016/s0016-5107(96)70045-7. [DOI] [PubMed] [Google Scholar]
- 10.Staritz M, Ewe K, Meyer zum Büschenfelde KH. Endoscopic papillary dilation (EPD) for the treatment of common bile duct stones and papillary stenosis. Endoscopy. 1983;15(Suppl 1):197–198. doi: 10.1055/s-2007-1021507. [DOI] [PubMed] [Google Scholar]
- 11.Mac Mathuna P, Siegenberg D, Gibbons D, et al. The acute and long-term effect of balloon sphincteroplasty on papillary structure in pigs. Gastrointest Endosc. 1996;44:650–655. doi: 10.1016/s0016-5107(96)70046-9. [DOI] [PubMed] [Google Scholar]
- 12.Kawabe T, Komatsu Y, Isayama H, et al. Histological analysis of the papilla after endoscopic papillary balloon dilation. Hepatogastroenterology. 2003;50:919–923. [PubMed] [Google Scholar]
- 13.Ueno N, Kurihara K. Impact of endoscopic sphincter dilation on papillary structure: a case report. Gastrointest Endosc. 1999;50:713–715. doi: 10.1016/s0016-5107(99)80032-7. [DOI] [PubMed] [Google Scholar]
- 14.Minami A, Nakatsu T, Uchida N, et al. Papillary dilation vs sphincterotomy in endoscopic removal of bile duct stones. A randomized trial with manometric function. Dig Dis Sci. 1995;40:2550–2554. doi: 10.1007/BF02220440. [DOI] [PubMed] [Google Scholar]
- 15.Sato H, Kodama T, Takaaki J, et al. Endoscopic papillary balloon dilatation may preserve sphincter of Oddi function after common bile duct stone management: evaluation from the viewpoint of endoscopic manometry. Gut. 1997;41:541–544. doi: 10.1136/gut.41.4.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yasuda I, Tomita E, Enya M, Kato T, Moriwaki H. Can endoscopic papillary balloon dilation really preserve sphincter of Oddi function? Gut. 2001;49:686–691. doi: 10.1136/gut.49.5.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383–393. doi: 10.1016/s0016-5107(91)70740-2. [DOI] [PubMed] [Google Scholar]
- 18.Park DH, Kim MH, Lee SK, et al. Endoscopic sphincterotomy vs. endoscopic papillary balloon dilation for choledocholithiasis in patients with liver cirrhosis and coagulopathy. Gastrointest Endosc. 2004;60:180–185. doi: 10.1016/s0016-5107(04)01554-8. [DOI] [PubMed] [Google Scholar]
- 19.Kawabe T, Komatsu Y, Tada M, et al. Endoscopic papillary balloon dilation in cirrhotic patients: removal of common bile duct stones without sphincterotomy. Endoscopy. 1996;28:694–698. doi: 10.1055/s-2007-1005579. [DOI] [PubMed] [Google Scholar]
- 20.Komatsu Y, Kawabe T, Toda N, et al. Endoscopic papillary balloon dilation for the management of common bile duct stones: experience of 226 cases. Endoscopy. 1998;30:12–17. doi: 10.1055/s-2007-993721. [DOI] [PubMed] [Google Scholar]
- 21.Prat F, Fritsch J, Choury AD, Meduri B, Pelletier G, Buffet C. Endoscopic sphincteroclasy: a useful therapeutic tool for biliary endoscopy in Billroth II gastrectomy patients. Endoscopy. 1997;29:79–81. doi: 10.1055/s-2007-1004079. [DOI] [PubMed] [Google Scholar]
- 22.Baron TH, Harewood GC. Endoscopic balloon dilation of the biliary sphincter compared to endoscopic biliary sphincterotomy for removal of common bile duct stones during ERCP: a meta-analysis of randomized, controlled trials. Am J Gastroenterol. 2004;99:1455–1460. doi: 10.1111/j.1572-0241.2004.30151.x. [DOI] [PubMed] [Google Scholar]
- 23.Arnold JC, Benz C, Martin WR, Adamek HE, Riemann JF. Endoscopic papillary balloon dilation vs. sphincterotomy for removal of common bile duct stones: a prospective randomized pilot study. Endoscopy. 2001;33:563–567. doi: 10.1055/s-2001-15307. [DOI] [PubMed] [Google Scholar]
- 24.Bergman JJ, Rauws EA, Fockens P, et al. Randomised trial of endoscopic balloon dilation versus endoscopic sphincterotomy for removal of bileduct stones. Lancet. 1997;349:1124–1129. doi: 10.1016/S0140-6736(96)11026-6. [DOI] [PubMed] [Google Scholar]
- 25.Natsui M, Narisawa R, Motoyama H, et al. What is an appropriate indication for endoscopic papillary balloon dilation? Eur J Gastroenterol Hepatol. 2002;14:635–640. doi: 10.1097/00042737-200206000-00008. [DOI] [PubMed] [Google Scholar]
- 26.Lin CK, Lai KH, Chan HH, et al. Endoscopic balloon dilatation is a safe method in the management of common bile duct stones. Dig Liver Dis. 2004;36:68–72. doi: 10.1016/j.dld.2003.09.014. [DOI] [PubMed] [Google Scholar]
- 27.Tanaka S, Sawayama T, Yoshioka T, et al. Endoscopic papillary balloon dilation and endoscopic sphincterotomy for bile duct stones: long-term outcomes in a prospective randomized controlled trial. Gastrointest Endosc. 2004;59:614–618. doi: 10.1016/s0016-5107(04)00157-9. [DOI] [PubMed] [Google Scholar]
- 28.Toda N, Saito K, Wada R, et al. Endoscopic sphincterotomy and papillary balloon dilation for bile duct stones. Hepatogastroenterology. 2005;52:700–704. [PubMed] [Google Scholar]
- 29.Liao WC, Huang SP, Wu MS, Lin JT, Wang HP. Comparison of endoscopic papillary balloon dilatation and sphincterotomy for lithotripsy in difficult sphincterotomy. J Clin Gastroenterol. 2008;42:295–299. doi: 10.1097/MCG.0b013e31802c3458. [DOI] [PubMed] [Google Scholar]
- 30.Mathuna PM, White P, Clarke E, Merriman R, Lennon JR, Crowe J. Endoscopic balloon sphincteroplasty (papillary dilation) for bile duct stones: efficacy, safety, and follow-up in 100 patients. Gastrointest Endosc. 1995;42:468–474. doi: 10.1016/s0016-5107(95)70052-8. [DOI] [PubMed] [Google Scholar]
- 31.Heo JH, Kang DH, Jung HJ, et al. Endoscopic sphincterotomy plus large-balloon dilation versus endoscopic sphincterotomy for removal of bile-duct stones. Gastrointest Endosc. 2007;66:720–726. doi: 10.1016/j.gie.2007.02.033. [DOI] [PubMed] [Google Scholar]
- 32.Tsujino T, Isayama H, Komatsu Y, et al. Risk factors for pancreatitis in patients with common bile duct stones managed by endoscopic papillary balloon dilation. Am J Gastroenterol. 2005;100:38–42. doi: 10.1111/j.1572-0241.2005.40638.x. [DOI] [PubMed] [Google Scholar]
- 33.Ueno N, Ozawa Y. Pancreatitis induced by endoscopic balloon sphincter dilation and changes in serum amylase levels after the procedure. Gastrointest Endosc. 1999;49(4 Pt 1):472–476. doi: 10.1016/s0016-5107(99)70045-3. [DOI] [PubMed] [Google Scholar]
- 34.Kozarek RA. Balloon dilation of the sphincter of Oddi. Endoscopy. 1988;20(Suppl 1):207–210. doi: 10.1055/s-2007-1018177. [DOI] [PubMed] [Google Scholar]
- 35.Disario JA, Freeman ML, Bjorkman DJ, et al. Endoscopic balloon dilation compared with sphincterotomy for extraction of bile duct stones. Gastroenterology. 2004;127:1291–1299. doi: 10.1053/j.gastro.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 36.Sugiyama M, Izumisato Y, Abe N, Masaki T, Mori T, Atomi Y. Predictive factors for acute pancreatitis and hyperamylasemia after endoscopic papillary balloon dilation. Gastrointest Endosc. 2003;57:531–535. doi: 10.1067/mge.2003.143. [DOI] [PubMed] [Google Scholar]
- 37.Fujita N, Maguchi H, Komatsu Y, et al. Endoscopic sphincterotomy and endoscopic papillary balloon dilatation for bile duct stones: a prospective randomized controlled multicenter trial. Gastrointest Endosc. 2003;57:151–155. doi: 10.1067/mge.2003.56. [DOI] [PubMed] [Google Scholar]
- 38.Wang P, Li ZS, Liu F, et al. Risk factors for ERCP-related complications: a prospective multicenter study. Am J Gastroenterol. 2009;104:31–40. doi: 10.1038/ajg.2008.5. [DOI] [PubMed] [Google Scholar]
- 39.Laugier R, Bernard JP, Berthezene P, Dupuy P. Changes in pancreatic exocrine secretion with age: pancreatic exocrine secretion does decrease in the elderly. Digestion. 1991;50:202–211. doi: 10.1159/000200762. [DOI] [PubMed] [Google Scholar]
- 40.Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003;57:156–159. doi: 10.1067/mge.2003.52. [DOI] [PubMed] [Google Scholar]
- 41.Cavallini G, Tittobello A, Frulloni L, Masci E, Mariana A, Di Francesco V. Gabexate for the prevention of pancreatic damage related to endoscopic retrograde cholangiopancreatography. Gabexate in digestive endoscopy--Italian Group. N Engl J Med. 1996;335:919–923. doi: 10.1056/NEJM199609263351302. [DOI] [PubMed] [Google Scholar]
- 42.Aizawa T, Ueno N. Stent placement in the pancreatic duct prevents pancreatitis after endoscopic sphincter dilation for removal of bile duct stones. Gastrointest Endosc. 2001;54:209–213. doi: 10.1067/mge.2001.115730. [DOI] [PubMed] [Google Scholar]
- 43.Ohashi A, Tamada K, Tomiyama T, et al. Epinephrine irrigation for the prevention of pancreatic damage after endoscopic balloon sphincteroplasty. J Gastroenterol Hepatol. 2001;16:568–571. doi: 10.1046/j.1440-1746.2001.02483.x. [DOI] [PubMed] [Google Scholar]
- 44.Nakagawa H, Ohara K. Safeguards against acute pancreatitis associated with endoscopic papillary balloon dilatation. J Hepatobiliary Pancreat Surg. 2006;13:75–79. doi: 10.1007/s00534-005-1061-5. [DOI] [PubMed] [Google Scholar]
- 45.Wehrmann T, Schmitt TH, Arndt A, Lembcke B, Caspary WF, Seifert H. Endoscopic injection of botulinum toxin in patients with recurrent acute pancreatitis due to pancreatic sphincter of Oddi dysfunction. Aliment Pharmacol Ther. 2000;14:1469–1477. doi: 10.1046/j.1365-2036.2000.00814.x. [DOI] [PubMed] [Google Scholar]
- 46.Ochi Y, Mukawa K, Kiyosawa K, Akamatsu T. Comparing the treatment outcomes of endoscopic papillary dilation and endoscopic sphincterotomy for removal of bile duct stones. J Gastroenterol Hepatol. 1999;14:90–96. doi: 10.1046/j.1440-1746.1999.01798.x. [DOI] [PubMed] [Google Scholar]
- 47.Pittman MA, Heath D, McNair A. Gallstone ileus following endoscopic retrograde cholangiopancreatography and endoscopic sphincterotomy. Dig Dis Sci. 2007;52:513–515. doi: 10.1007/s10620-006-9588-0. [DOI] [PubMed] [Google Scholar]
- 48.Sivagnanam P, Cheong E, Rhodes M. Delayed gallstone ileus presentation after ERCP and sphincterotomy. Gastrointest Endosc. 2009;69:156–158. doi: 10.1016/j.gie.2008.06.012. [DOI] [PubMed] [Google Scholar]
- 49.Ohashi A, Tamada K, Wada S, et al. Risk factors for recurrent bile duct stones after endoscopic papillary balloon dilation: long-term follow-up study. Dig Endosc. 2009;21:73–77. doi: 10.1111/j.1443-1661.2009.00835.x. [DOI] [PubMed] [Google Scholar]
- 50.Ueno N, Ozawa Y, Aizawa T. Prognostic factors for recurrence of bile duct stones after endoscopic treatment by sphincter dilation. Gastrointest Endosc. 2003;58:336–340. doi: 10.1067/s0016-5107(03)00004-x. [DOI] [PubMed] [Google Scholar]
- 51.Ito Y, Tsujino T, Togawa O, et al. Endoscopic papillary balloon dilation for the management of bile duct stones in patients 85 years of age and older. Gastrointest Endosc. 2008;68:477–482. doi: 10.1016/j.gie.2007.10.066. [DOI] [PubMed] [Google Scholar]
- 52.Attasaranya S, Cheon YK, Vittal H, et al. Large-diameter biliary orifice balloon dilation to aid in endoscopic bile duct stone removal: a multicenter series. Gastrointest Endosc. 2008;67:1046–1052. doi: 10.1016/j.gie.2007.08.047. [DOI] [PubMed] [Google Scholar]
- 53.Bang S, Kim MH, Park JY, Park SW, Song SY, Chung JB. Endoscopic papillary balloon dilation with large balloon after limited sphincterotomy for retrieval of choledocholithiasis. Yonsei Med J. 2006;47:805–810. doi: 10.3349/ymj.2006.47.6.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Minami A, Hirose S, Nomoto T, Hayakawa S. Small sphincterotomy combined with papillary dilation with large balloon permits retrieval of large stones without mechanical lithotripsy. World J Gastroenterol. 2007;13:2179–2182. doi: 10.3748/wjg.v13.i15.2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Maydeo A, Bhandari S. Balloon sphincteroplasty for removing difficult bile duct stones. Endoscopy. 2007;39:958–961. doi: 10.1055/s-2007-966784. [DOI] [PubMed] [Google Scholar]
- 56.Draganov PV, Evans W, Fazel A, Forsmark CE. Large size balloon dilation of the ampulla after biliary sphincterotomy can facilitate endoscopic extraction of difficult bile duct stones. J Clin Gastroenterol. 2009;43:782–786. doi: 10.1097/MCG.0b013e31818f50a2. [DOI] [PubMed] [Google Scholar]
- 57.Itoi T, Itokawa F, Sofuni A, et al. Endoscopic sphincterotomy combined with large balloon dilation can reduce the procedure time and fluoroscopy time for removal of large bile duct stones. Am J Gastroenterol. 2009;104:560–565. doi: 10.1038/ajg.2008.67. [DOI] [PubMed] [Google Scholar]
- 58.Espinel J, Pinedo E, Olcoz JL. Large hydrostatic balloon for choledocholithiasis. Rev Esp Enferm Dig. 2007;99:33–38. doi: 10.4321/s1130-01082007000100007. [DOI] [PubMed] [Google Scholar]
- 59.Vlavianos P, Chopra K, Mandalia S, Anderson M, Thompson J, Westaby D. Endoscopic balloon dilatation versus endoscopic sphincterotomy for the removal of bile duct stones: a prospective randomised trial. Gut. 2003;52:1165–1169. doi: 10.1136/gut.52.8.1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jeong S, Ki SH, Lee DH, et al. Endoscopic large-balloon sphincteroplasty without preceding sphincterotomy for the removal of large bile duct stones: a preliminary study. Gastrointest Endosc. 2009;70:915–922. doi: 10.1016/j.gie.2009.04.042. [DOI] [PubMed] [Google Scholar]
- 61.Kojima Y, Nakagawa H, Miyata A, et al. Long-term prognosis of bile duct stones: endoscopic papillary balloon dilatation versus endoscopic sphincterotomy. Dig Endosc. 2010;22:21–24. doi: 10.1111/j.1443-1661.2009.00913.x. [DOI] [PubMed] [Google Scholar]
- 62.Kim HG, Cheon YK, Cho YD, et al. Small sphincterotomy combined with endoscopic papillary large balloon dilation versus sphincterotomy. World J Gastroenterol. 2009;15:4298–4304. doi: 10.3748/wjg.15.4298. [DOI] [PMC free article] [PubMed] [Google Scholar]