Abstract
Cutaneous metastases from internal malignancies are uncommon. Furthermore, cutaneous metastases from cholangiocarcinoma are extremely rare. Here we report a case of two patients with distant cutaneous metastases of cholangiocarcinoma: 1) a 66-year-old man who presented with a solitary, erythematous nodule on the scalp and 2) a 44-year-old man who presented with multiple, erythematous nodules on the scalp, the chest wall, and the back. In both cases, the erythematous nodules were the first clinical signs of cholangiocarcinoma. Histopathological analyses of skin biopsy specimens of the two patients revealed adenocarcinomas with features similar to the original cholangiocarcinoma. Two cases of cholangiocarcinoma in which metastatic skin nodules appeared as the first sign of the disease are reported here, with a review of the relevant literature.
Keywords: Cutaneous metastasis, Cholangiocarcinoma
INTRODUCTION
Cutaneous metastases from internal malignancies are uncommon, and have been reported to occur in only 0.7-9% of patients.1,2 Moreover, cutaneous metastases from cholangiocarcinomas are extremely rare. Few published reports mention cutaneous metastases from cholangiocarcinomas, and those found in the literature were derived from direct tumor seeding by percutaneous procedures.
Our report describes two patients who presented with metastatic skin lesions as the first sign of cholangiocarcinoma, and provides a review of the related literature.
CASE REPORT
1. Case 1
A 66-year-old man was admitted to our hospital in January 2009 for evaluation of a painless, subcutaneous nodule on his frontal scalp. The scalp nodule had been present for 1 month; after excisional biopsy performed at a different institution, the nodule was histologically diagnosed as a metastatic adenocarcinoma. The patient was referred to our hospital for further investigation of the primary malignancy.
The patient was asymptomatic, and reported no complaint of weight loss or abdominal pain. His past medical history was non-contributory, with no evidence of exposure to hepatitis virus or potentially hepatotoxic drugs. On physical examination, a 0.7 cm, firm, fixed, painless, subcutaneous nodule was noted on the right frontal scalp (Fig. 1A). Apart from the detection of the subcutaneous nodule, the findings of the physical examination were normal, including the absence of any palpable abdominal mass.
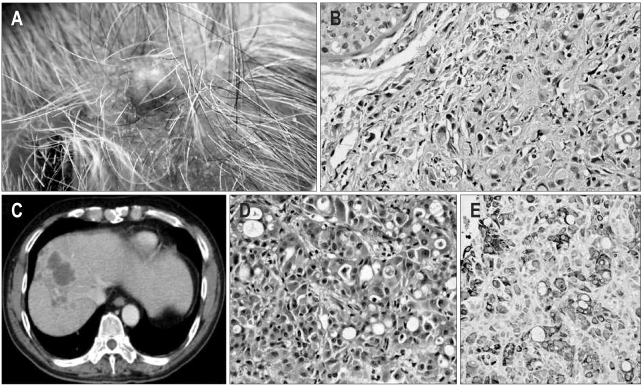
Fig. 1.
(A) The skin lesion on the right frontal scalp was a 0.7-cm, firm, fixed, round, painless erythematous nodule. (B) Histopathologic findings of the skin biopsy sample showed a metastatic adenocarcinoma with features of signet-ring-cell carcinoma (H&E stain, ×200). (C) Abdominal CT revealed a multilobulated low-attenuation mass in the right hepatic lobe with multiple satellite lesions. (D) Histopathologic findings of the liver biopsy showed poorly differentiated adenocarcinoma infiltration (H&E stain, ×200). (E) Immunohistochemical staining showed that the tumor cells in the liver mass were positive for cytokeratin 19 (CK 19) (×200).
Laboratory analysis showed the following results: white cell count 8,130/mm3, hemoglobin 13.6 mg/dL, total bilirubin 0.5 mg/dL, serum aspartate transaminase 48 IU/L, alanine aminotransferase 59 IU/L, alkaline phosphatase 163 IU/L, carbohydrate antigen 19-9 (CA 19-9) 117.0 ng/mL, carcinoembryonic antigen (CEA) 3.42 ng/mL, and alpha-fetoprotein 4.05 IU/mL.
An abdominal computed tomographic scan detected a multilobulated mass in the right hepatic lobe with multiple satellite lesions (Fig. 1C). There were multiple lymph node metastases in the hepatic hilum, portacaval space, and retroperitoneum. Ultrasound-guided gun-biopsy of the liver showed microscopic findings on the hepatic mass, suggesting a poorly differentiated adenocarcinoma (Fig. 1D). Immunohistochemical staining of the tumor cells in the liver mass were positive for cytokeratin 19 (CK 19) (Fig. 1E). An excisional biopsy of the scalp nodule displayed a metastatic adenocarcinoma, with features of signet ring cell carcinoma (Fig. 1B).
Based on these findings, a diagnosis of cholangiocarcinoma with cutaneous metastasis was made. The patient was treated with systemic chemotherapy; however, the cholangiocarcinoma progressed, resulting in the death of the patient 5 months later.
2. Case 2
A 44-year-old man was referred to our dermatology department in June 2008 with a 1-month history of multiple, erythematous nodules on the head, face, and back. His past medical history was non-contributory, but he reported a family history of colon cancer, which had affected his father and brother. The patient complained of abdominal discomfort and a 3 kg weight loss over the previous 2 months.
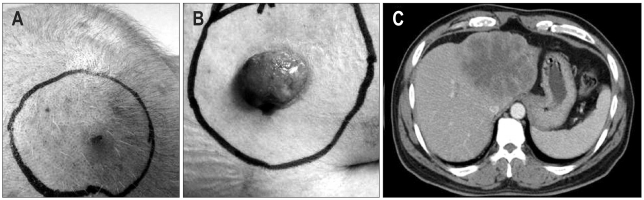
A physical examination revealed a 1 cm erythematous, tender, subcutaneous nodule on the left temporal scalp (Fig. 2A). A 0.8 cm, erythematous, subcutaneous nodule was detected on the left upper back, and a 3×4 cm ulcerofungating skin mass was found above the left axillary area (Fig. 2B). Additionally, the liver was palpable below the costal margin.
Fig. 2.
(A) The skin mass on the left temporal scalp exhibited erythematous, nodular features. (B) The skin lesion on the back was a 3×4-cm ulcerofungating mass above the axillary area. (C) PET/CT scan revealed a 10-cm mass on the left lobe of the liver.
Laboratory analysis showed the following results: white cell count 7,460/mm3, hemoglobin 14.0 mg/dL, total bilirubin 1.0 mg/dL, serum aspartate transaminase 60 IU/L, alanine aminotransferase 56 IU/L, alkaline phosphatase 418 IU/L, CA 19-9 27.1 ng/mL, CEA 3.79 ng/mL, and alpha-fetoprotein 1.76 IU/mL.
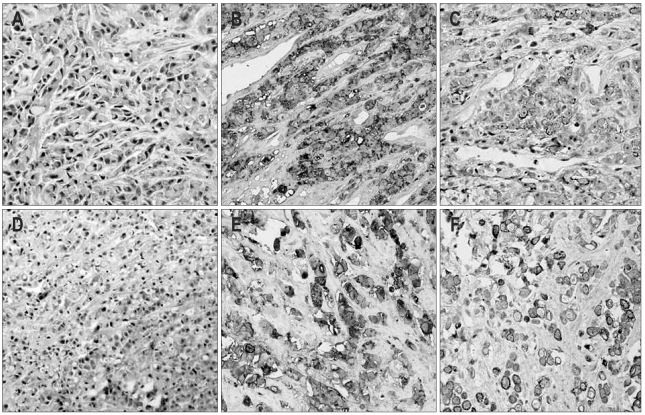
Microscopic evaluation and immunohistochemical staining of the left temporal scalp skin nodule showed a poorly differentiated adenocarcinoma (Fig. 3A), which stained positive for CEA (Fig. 3B) and CK 19 (Fig. 3C). To evaluate the primary malignancy, the patient underwent a PET/CT scan, which showed a 10 cm mass with high uptake on the left lobe of the liver (Fig. 2C), multiple bone metastases to the left 6th rib, at the T11 spine, the L4 spine, and both pelvic bones, and multiple scattered skin nodules, which were suspected of being skin metastases. Microscopic and immunohistochemical analysis of the liver biopsy specimens showed a poorly differentiated adenocarcinoma (Fig. 3D), which stained positive for CEA (Fig. 3E) and CK 19 (Fig. 3F) and was suggestive of cholagiocarcinoma.
Fig. 3.
(A) Histopathologic findings of the skin biopsy sample showing signet-ring-cell carcinoma infiltration (H&E stain, ×200). (B) The tumor cells in skin mass were positive for carcinoembryonic antigen (CEA) (×200). (C) The tumor cells in the skin mass were weakly positive for CK 19 (×200). (D) Histopathologic findings of the liver biopsy showed poorly differentiated adenocarcinoma infiltration (H&E stain, ×100). (E) The tumor cells in liver mass were positive for CEA (×200). (F) The tumor cells in liver mass were weakly positive for CK 19 (×200).
Based on these findings, a diagnosis of cholangiocarcinoma with multiple cutaneous and bone metastases was made. The patient underwent systemic chemotherapy and radiotherapy of the metastatic bone lesions. However, brain and leptomeningeal metastases developed as the cholangiocarcinoma progressed; the patient died 7 months later.
DISCUSSION
Cutaneous metastases from an internal malignancy are uncommon, and have been reported to occur in only 0.7-9% of patients.1,2 The most common tumors to metastasize to the skin are breast (36.2%), lung (16.3%), colorectal (11.3%), oral mucosal (7.8%), gastric (7.1%), hepatocellular (2.8%), and esophageal (2.1%).3
Cholangiocarcinoma is a neoplasm of the bile duct, which frequently invades or metastasizes to adjacent organs or other visceral organs, such as the lungs, bones, adrenal glands, and brain.4,5 Cutaneous metastases of cholangiocarcinoma are extremely rare and have been reported to occur in only 0.4-5.3%6,7 of cases. Most of the literature reporting cutaneous metastases of cholangiocarcinoma describes cases in which cancer cells were disseminated through catheter tracts used for percutaneous biliary drainage, or cases where cutaneous metastases were discovered after the diagnosis of cholangiocarcinoma was made.8
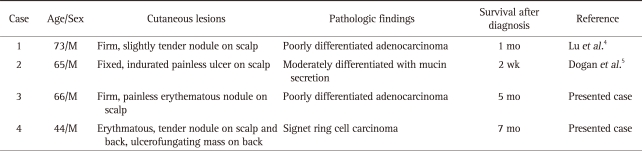
The incidence of metastatic skin lesions as the first sign of disease has been described in only 0.8% patients with systemic malignancies.2 Moreover, cutaneous metastases from cholangiocarcinomas have only been reported in two patients in whom a cutaneous lesion was the first sign of the carcinoma (Table 1).4,5 In both of these patients, the cutaneous lesion was found on the scalp. In one, there was a poorly circumscribed, firm, subcutaneous nodule on the occipital area, and the lesion was approximately 2 cm in diameter with slight tenderness and erythema.4 The other patient had a well-circumscribed, indurated, painless ulcer on his scalp, which was fixed to the underlying tissue.5 Both patients had erythematous, subcutaneous nodules on the scalp, and one of them also presented with an ulcerofungating mass on the back.
Table 1.
Reported Cases of Cutaneous Metastases from Cholangiocarcinoma in Which the First Clinical Signs Were Skin Lesions
The most common presentation of a metastatic skin lesion is a firm, painless nodule (multiple nodules are found in 46.4% of patients and a single nodule in 37.7% of patients; these can be macules, plaques, erythematous plaques, and ulcers).3 Previous reports indicate that the most common presentation of cutaneous metastases of cholangiocarcinoma is the nodular type; other skin lesions described include erythematous plaques, abscesses, and ulcers.4-11 Most nodular lesions are firm, painless, and non-ulcerative and covered by a normal appearing epithelium; this results in some lesions being misdiagnosed as benign. Clinicians should therefore consider the possibility of cutaneous metastases when examining patients with skin nodules, especially those with a history of malignancy.
The most common sites of cutaneous metastases are the chest (30.3%), abdomen (20.0%), and scalp (12.6%).3 Lookingbill et al.11 found that scalp metastases originated from a wide variety of cancers, including lung, renal, and hematopoietic malignancies. In the case of cholangiocarcinomas, the two previously reported patients, and those in our case studies, had a metastatic skin lesion on the scalp. Despite the obvious limitation of the small number of reported cases, we can be state that cutaneous metastasis of cholangiocarcinoma is most common on the scalp.
Lu et al. demonstrated that the valveless vertebral venous plexus communicates above with the intracranial venous sinuses, and segmentally with the veins of the thorax, abdomen, and pelvis.4,12 Metastatic skin lesions, therefore, occur on the scalp more frequently than in other areas.
Traditionally, cutaneous metastases indicate the presence of advanced disease and are associated with poor prognosis. Hu et al.3 reported that the majority of patients (73.8%) with skin metastases had concomitant visceral metastases at the time of, or following cutaneous presentation. The two previously reported patients who presented with cutaneous metastases of cholangiocarcinoma, as well as the two patients described here, all died within 7 months of the diagnosis.
In summary, cutaneous metastases from cholangiocarcinoma are rare, but do occur. When metastatic skin lesions are discovered, clinicians should be aware of the possibility that these lesions can be associated with cutaneous metastases of cholangiocarcinoma.
We report here two unusual cases of distant cutaneous metastases from cholangiocarcinoma prior to the diagnosis of a primary tumor.
References
- 1.Schwartz RA. Cutaneous metastatic disease. J Am Acad Dermatol. 1995;33:161–182. doi: 10.1016/0190-9622(95)90231-7. [DOI] [PubMed] [Google Scholar]
- 2.Lookingbill DP, Spangler N, Sexton FM. Skin involvement as the presenting sign of internal carcinoma. A retrospective study of 7316 cancer patients. J Am Acad Dermatol. 1990;22:19–26. doi: 10.1016/0190-9622(90)70002-y. [DOI] [PubMed] [Google Scholar]
- 3.Hu SC, Chen GS, Lu YW, Wu CS, Lan CC. Cutaneous metastases from different internal malignancies: a clinical and prognostic appraisal. J Eur Acad Dermatol Venereol. 2008;22:735–740. doi: 10.1111/j.1468-3083.2008.02590.x. [DOI] [PubMed] [Google Scholar]
- 4.Lu CI, Wong WR, Hong HS. Distant cutaneous metastases of cholangiocarcinoma: report of two cases of a previously unreported condition. J Am Acad Dermatol. 2004;51:S108–S111. doi: 10.1016/j.jaad.2004.01.042. [DOI] [PubMed] [Google Scholar]
- 5.Dogan G, Karincaoglu Y, Karincaoglu M, Aydin NE. Scalp ulcer as first sign of cholangiocarcinoma. Am J Clin Dermatol. 2006;7:387–389. doi: 10.2165/00128071-200607060-00008. [DOI] [PubMed] [Google Scholar]
- 6.Shorvon PJ, Leung JW, Corcoran M, Mason RR, Cotton PB. Cutaneous seeding of malignant tumours after insertion of percutaneous prosthesis for obstructive jaundice. Br J Surg. 1984;71:694–695. doi: 10.1002/bjs.1800710916. [DOI] [PubMed] [Google Scholar]
- 7.Tersigni R, Rossi P, Bochicchio O, et al. Tumor extension along percutaneous transhepatic biliary drainage tracts. Eur J Radiol. 1986;6:280–282. [PubMed] [Google Scholar]
- 8.Lee BK, Seo YH, Lee NH, Joo SY, Ko HM. Cholangiocarcinoma with distant cutaneous metastases. Korean J Gastroenterol. 2009;54:342–345. doi: 10.4166/kjg.2009.54.5.342. [DOI] [PubMed] [Google Scholar]
- 9.Bloom RA, Gordon RL, Manny Y, Engelberg M. Seeding of cholangiocarcinoma along T-tube tracts. Gastrointest Radiol. 1984;9:167–169. doi: 10.1007/BF01887827. [DOI] [PubMed] [Google Scholar]
- 10.Ueda K, Okada N, Yoshikawa K. A case of cutaneous metastasis of bile duct carcinoma. J Am Acad Dermatol. 1991;25:848–849. doi: 10.1016/s0190-9622(08)80981-4. [DOI] [PubMed] [Google Scholar]
- 11.Lookingbill DP, Spangler N, Helm KF. Cutaneous metastases in patients with metastatic carcinoma: a retrospective study of 4020 patients. J Am Acad Dermatol. 1993;29:228–236. doi: 10.1016/0190-9622(93)70173-q. [DOI] [PubMed] [Google Scholar]
- 12.Baston OV. The role of the vertebral veins in metastatic processes. Ann Intern Med. 1942;16:38–45. [Google Scholar]