Abstract
Background/Aims
There have been few Asian studies regarding anxiety and depression associated with irritable bowel syndrome (IBS). The aim of this study was to evaluate the frequency and importance of anxiety and depression in Korean patients with IBS.
Methods
A total of 124 IBS patients and 91 healthy subjects were enrolled consecutively. All participants were asked to complete self-administered questionnaires: one addressing symptom severity, the Short Form 36, and the Hospital Anxiety and Depression Scale (HADS). The patients were also asked to complete the IBS-specifi c quality of life (IBS-QOL) questionnaire.
Results
Anxiety and depression were observed in 38.6% and 38.6% of IBS patients, respectively, and in 24.2% and 16.5% of healthy subjects, respectively (p<0.05 for both). The mean HADS scores for anxiety and depression in IBS patients were 6.8±4.5 and 7.1±4.4, respectively. Both anxiety and depression were associated with self-reported symptom severity (p<0.012 and p<0.001, respectively). As determined by multivariate analysis, symptom severity was the most important factor in the prediction of anxiety and depression. Self-reported symptom severity and depression were clearly and independently associated with the overall IBS-QOL score.
Conclusions
Anxiety and depression were frequently observed in Korean IBS patients and were related to the severity of their symptoms and the impairment of the patient's QOL. Our data suggest that assessing anxiety and depression is important when evaluating IBS patients.
Keywords: Irritable bowel syndrome, Anxiety, Depression, Quality of life
INTRODUCTION
Irritable bowel syndrome (IBS) is the most common gastrointestinal disorder seen at gastroenterology clinics. IBS is a complex disorder with an incompletely defined etiology and various pathogeneses, such as abnormal motility, visceral hypersensitivity, inflammation, abnormalities of autonomic activity, and central nervous system modulation. Besides these physiological factors, psychological factors also play a role in IBS. Psychological stress is known to exacerbate gastrointestinal symptoms. Psychological and psychiatric comorbidity is common among patients with IBS, and psychosocial factors affect health status and clinical outcome.1,2 Therefore, knowledge of the psychosocial aspects of IBS is fundamental and critical to our understanding of this disorder and its effective treatment.3,4
The most common psychological disorders are anxiety, depression, panic, posttraumatic stress, and somatization disorders.5 IBS patients experience levels of anxiety and depression intermediate between those of psychiatric patients and healthy controls.6 Some evidence suggests that psychotropic agents are effective in controlling the symptoms related to IBS.7,8 Psychiatric disorders such as anxiety and depression may also contribute to the negative impact of IBS on the patient's quality of life (QOL).9,10 Treatment of the psychological aspects of the disease can improve the QOL of patients with IBS, emphasizing the importance of the psychological aspects of the condition.7,11 However, there are few data available regarding the contribution of psychological factors to the patient's QOL.
The impact of the psychological factors associated with IBS has been widely studied in Western countries.12-14 Individuals may interprete one's health events in a manner that is partly dependent on their social and cultural backgrounds. However, there are only a few studies in Asia, and these studies have mainly focused on the prevalence, symptom patterns, or impact on the QOL of IBS patients.15-17
In this study, we evaluated the frequency of anxiety and depression in Korean IBS patients, and assessed the relationships between these psychological features and the impairment of their QOL.
MATERIALS AND METHODS
1. Study subjects
Subjects were recruited consecutively at the Seoul St. Mary's Hospital, Seoul, Korea between January 2006 and September 2006. IBS patients were enrolled through the gastroenterology clinic. The following criteria were used to select patients with IBS: 18-75 years of age, no abnormal results on a colonoscopic examination or barium enema, and symptoms consistent with the Rome II criteria.18 Patients with a history of gastrointestinal, renal, or gynecological pathology or surgery that could cause IBS-like symptoms were excluded. Participants who had taken medications specific for a psychiatric illness for six months or less before the study were also excluded. Levels of thyroid-stimulating hormone, fasting plasma glucose, and other biochemical indices were analyzed to rule out IBS-like symptoms caused by other diseases. Healthy subjects who visited for a routine checkup and had no prior history of disease or symptoms related to the gastrointestinal system were enrolled through the Health Promotion Center. Subjects were excluded if they answered positively to the interviewer's questions regarding the presence of any major current medical or psychological illness, previous abdominal surgery, pregnancy, lactation, and severe medical illness. Eligible participants gave their informed consent and provided details of their age, sex, marital status, and level of education upon entry to the study. The study protocol was approved by the institutional review board of the same hospital.
2. Measurements
1) Symptom severity, duration, and subtypes
Patients with IBS were asked to rate the severity of their bowel problems ("In your own opinion, how would you describe your bowel problems?") on a three-point response scale: mild (can be ignored if I don't think about it), moderate (cannot be ignored, but does not affect my lifestyle), or severe (affects my lifestyle). They were also asked the duration of their IBS-related symptoms. Patients were classified as constipation-predominant IBS (C-IBS), diarrhea-predominant IBS (D-IBS), or mixed-type IBS (M-IBS) according to their primary bowel patterns.19 An abdominal pain or discomfort score was selected by the patients from a seven-point Likert scale, from 0 (no pain) to 6 (very severe).
2) Short Form 36 (SF-36) questionnaire
All participants completed the SF-36 questionnaire. QOL was evaluated using the Korean version of the generic SF-36 questionnaire (version 2). This 36-item questionnaire scores eight domains of patient functioning: physical functioning, physical role, bodily pain, general health, vitality, social functioning, emotional role, and mental health.20 Each subscale was scored from 0 to 100; a high score indicated a good health status.
3) Irritable bowel syndrome-quality of life (IBS-QOL) questionnaire
IBS patients completed the IBS-QOL questionnaire. The IBS-QOL questionnaire was developed by Patrick et al.,21 translated into Korean using a standard accepted process, and validated cross-culturally.22 It consists of 34 IBS-specific QOL items. The patients were asked to choose between descriptive statements using a recall period of the previous 30 days.21 A five-point Likert response scale was used to assess the degree to which each statement described the feelings of the respondent (not at all, slightly, moderately, quite a bit, and extremely or a great deal). There were eight subscales: dysphoria, interference with activities, body image, health concern, food avoidance, social reaction, sexual function, and relationships. Each subscale could be transformed onto a 0-100 scale, ranging from 0 (poor QOL) to 100 (maximum QOL). All items were summed to calculate the overall score, which was transformed onto a 0-100 scale. The overall IBS-QOL score was used as the dependent variable with which the factors that affected the patient's QOL were determined.
4) Anxiety and depression
Both IBS patients and healthy subjects were asked to complete the Hospital Anxiety and Depression Scale (HADS). HADS is a 14-item self-report measure that was specifically developed to assess anxiety and depression in people with medical illnesses.23 It is considered an effective screening measure for anxiety and depression and has been widely used.24,25 It has two subscales, which evaluate anxiety and depression. The scores for each subscale range from 0 to 21. A cutoff score of 8 was used for both anxiety and depression, because this score had been previously reported to yield good sensitivity and specificity (89.2% and 82.5%, respectively) in Korean patients with anxiety and depression and in the general population.26
3. Statistical analysis
Continuous data were presented as means±standard deviations, and categorical data were presented as quantities and proportions. For categorical data, group differences were tested using the χ2 test and the Mantel-Haenszel test. Analysis of variance (ANOVA) and the two-sample independent t-test or the Mann-Whitney test was used for the analysis of continuous variables. A univariate analysis was performed to evaluate the association between anxiety, depression, and IBS. Multiple linear regressions were performed to adjust the data for age, sex, IBS subtype, self-reported symptom severity, education, and marital status to identify factors that were significantly related to the anxiety and depression of the patients with IBS. The statistics were reported as estimates with 95% confidence intervals for ordinal variables, and as p-values for continuous variables, with the level of statistical significance specified as 0.05. All statistical analyses were performed with SAS for Windows software (version 8.02; SAS Institute Inc., Cary, NC, USA).
RESULTS
1. Characteristics of IBS patients and healthy subjects
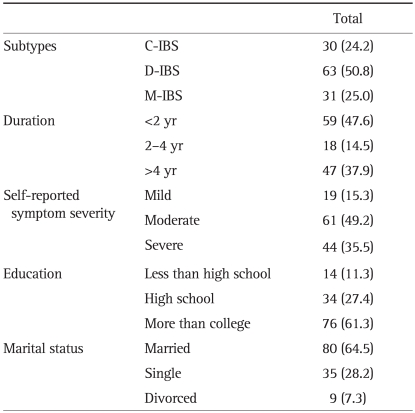
A total of 124 IBS patients and 91 healthy subjects were enrolled in this study. The mean age of the IBS patients was 43.3±14.3 years, and 49.2% were female. The mean age of the healthy subjects was 45.8±15.2 years, and 46.2% were female. There were no significant differences in sex or age between the patients and the healthy subjects. Information on IBS subtypes, symptom duration, self-reported symptom severity, level of education, and marital status was presented in Table 1.
Table 1.
Characteristics of Patients with IBS
Data are presented as number (%).
IBS, irritable bowel syndrome; C-IBS, constipation-predominant IBS; D-IBS, diarrhea-predominant IBS; M-IBS, mixed-type IBS.
2. Anxiety and depression in the IBS patients and healthy subjects
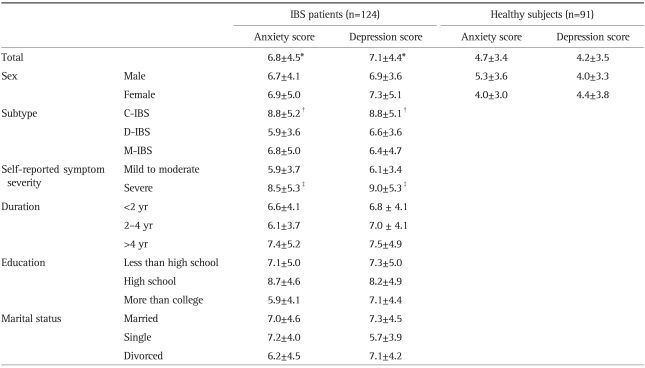
Anxiety was found more frequently in the IBS patients than in the healthy subjects (38.6% and 24.2%, respectively; p<0.05). The mean score for anxiety in the IBS patients was higher than that of healthy subjects (6.8 vs 4.7, p<0.001). Depression was also more frequently found in the IBS patients than in the healthy subjects (38.6% and 16.5%, respectively; p<0.05). The mean score for depression in the IBS patients was higher than that of healthy patients as well as anxiety (7.1 vs 4.2, p<0.001; Table 2).
Table 2.
HADS Scores for IBS Patients and Healthy Subjects
HADS, Hospital Anxiety and Depression Scale; IBS, irritable bowel syndrome; C-IBS, constipation-predominant IBS; D-IBS, diarrhea-predominant IBS; M-IBS, mixed-type IBS.
*p<0.05 (compared with healthy subjects); †p<0.05 (compared with patients with the other subtypes); ‡p<0.05 (compared with patients with mild to moderate symptoms).
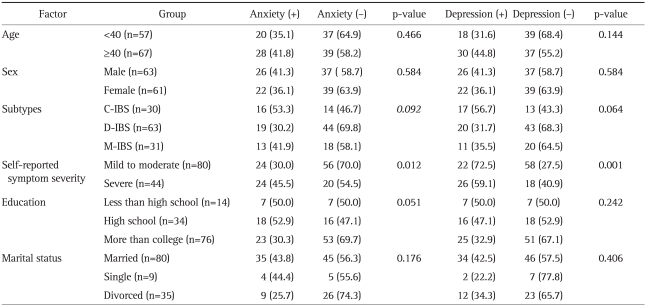
The frequencies of anxiety and depression in patients with severe symptoms were 54.5% and 59.1%, respectively, which were higher than those of the patients with mild to moderate symptoms (30% and 27.5%, respectively). The HADS scores of the IBS patients with mild symptoms did not differ from those of the healthy subjects (anxiety, p=0.691; depression, p=0.228). IBS patients with severe symptoms showed anxiety or depression more frequently than did patients with mild or moderate symptoms (p=0.012 and p=0.001, respectively; Table 3). Among the three subtypes of IBS, anxiety was present in 16 (53.3%) of the 30 patients with C-IBS, in 19 (30.2%) of the 63 patients with D-IBS, and in 13 (41.9%) of the 31 patients with M-IBS, which are not significantly different (p=0.092, Table 3). Depression was present in 17 (56.7%) patients with C-IBS, 20 (31.7%) with D-IBS, and 11 (35.5%) with M-IBS, which were also not significantly different (p=0.064). The anxiety and depression scores were significantly different for the different subtypes (p=0.014 and p=0.047, respectively). C-IBS patients had higher anxiety and depression scores than those of the other subtypes (Table 2).
Table 3.
Results of Univariate Analysis of the Differences between Patients with Anxiety or Depression and Those without Anxiety or Depression
Data are presented as number (%).
IBS, irritable bowel syndrome; C-IBS, constipation-predominant IBS; D-IBS, diarrhea-predominant, IBS; M-IBS, mixed-type IBS.
3. Factors related to anxiety and depression
On univariate analysis, symptom severity was significantly different between the patients with and without anxiety (p<0.05), and between the patients with and without depression (p=0.001, Table 3).
Among the patients with severe symptoms, the abdominal pain or discomfort score was significantly higher in patients with depression than that in patients without depression (p<0.01). In this subgroup of patients, the presence of anxiety was not significantly related to the abdominal pain or discomfort score (p=0.058).
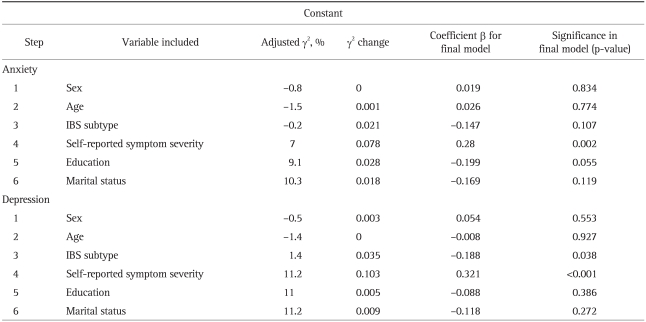
Table 4 shows the results of a multivariate analysis of the factors affecting anxiety or depression. The most significant factor affecting the patient's anxiety or depression was IBS-related symptoms. IBS subtype was also an independent factor influencing the patient's depression status. However, sex, age, education level, and marital status did not affect the patient's anxiety or depression.
Table 4.
Results of Multiple Stepwise Regression Analysis of the Relationship between Self-Reported Symptom Severity, Sex, Age, and IBS Subtypes and Anxiety and Depression
IBS, irritable bowel syndrome.
4. Association of IBS-QOL with anxiety and depression in IBS patients
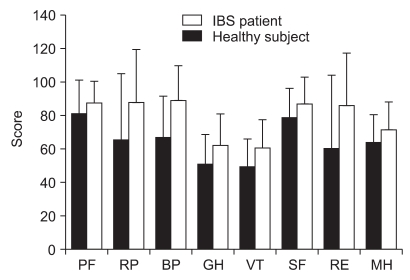
There were statistically significant differences in all SF-36 domains between the IBS patients and the healthy subjects (p<0.01 for all, Fig. 1). The scores of the IBS patients for all eight domains were lower than those of the healthy controls.
Fig. 1.
Short Form 36 (SF-36) scale scores were significantly lower in the patients with IBS (n=124) than in the healthy subjects (n=91).
Data are presented as mean±SD.
IBS, irritable bowel syndrome; PF, physical function; RP, role limitations-physical; BP, bodily pain; GH, general health; VT, vitality; SF, social functioning; RE, role limitations-emotional; MH, mental health.
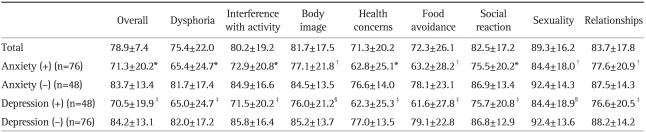
As shown in Table 5, the mean overall score for IBS-QOL was 78.9. Patients with anxiety had lower scores on all subscales of the IBS-QOL (p<0.05). Among the eight subscales of the IBS-QOL, difference of mean scores for dysphoria (16.3), food avoidance (14.9), and health concerns (13.8) were relatively higher than those for the other subscales. This pattern of impairment in different domains was also observed in patients with and without depression. The greatest differences between the two groups defined by the presence/absence of depression were observed for food avoidance (17.4), dysphoria (17.0), and health concerns (14.6).
Table 5.
Relationships between Results of the IBS-QOL and Anxiety or Depression
Data are presented as mean±SD.
IBS, irritable bowel syndrome; QOL, quality of life.
*p<0.001 and †p<0.05 (compared with patients without anxiety); ‡p<0.001 and §p<0.05 (compared with patients without depression).
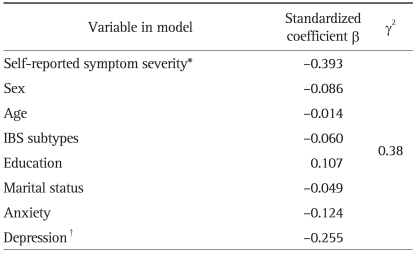
Multiple regression analysis was performed to evaluate the influence of anxiety and depression on the QOL of the patients. As shown in Table 6, self-reported symptom severity was clearly and independently associated with the overall IBS-QOL score (β=-0.393, p<0.001). Depression also independently affected the overall IBS-QOL score (β=-0.255, p=0.027), but anxiety did not significantly affect it.
Table 6.
Results of Multiple Regression Analysis of Self-Reported Symptom Severity, Sex, Age, IBS Subtype, Anxiety, and Depression with the IBS-QOL Overall Scores
IBS, irritable bowel syndrome; QOL, quality of life.
*p<0.001; †p=0.027.
DISCUSSION
In this study, we investigated whether anxiety and depression occur more frequently in Korean patients with IBS than in healthy subjects. The HADS score of the IBS patients was significantly higher than that of the healthy subjects. Anxiety and depression were important in IBS patients with severe symptoms. The HADS score of the IBS patients with mild symptom did not differ from that of healthy subjects. The most important factor influencing anxiety and depression in IBS patients was symptom severity. IBS subtype was also a significant factor in depression. Depression in patients with IBS was significantly associated with impairment of their QOL.
Patients with IBS generally have significantly higher psychiatric comorbidity rates than similar groups of general medical patients or patients with organic disorders.27 The most frequent psychiatric disorder in clinical IBS patients is depression, followed by anxiety and somatization disorders.6,27,28 Our study was undertaken in the social and cultural environment of an Asian country, and anxiety and depression were in about 40% of patients with IBS, which is consistent with the results of Western studies. Several studies have assessed the association between IBS and psychological factors in Eastern countries.15-17 However, these studies enrolled small numbers of IBS patients, and did not assess psychological factors directly. Our study reveals the importance of symptom severity on psychological status, especially anxiety and depression, and also shows a strong association between psychological factors and QOL in patients with IBS.
Patients with IBS are particularly susceptible to stressful experiences, which produce gastrointestinal symptoms.1 Psychiatric disorders are associated with changes in the processing of visceral sensations in patients with IBS, which could elicit the symptoms of IBS.29 Patients with IBS who have a concomitant psychiatric diagnosis may also manifest changes in gut-related autonomic nervous system function, affecting gut motility and sensation.1 In recent years, an appreciation of the modulation of visceral stimuli by the central nervous system has developed, particularly with the growing number of functional neuroimaging studies available.30 In these studies, changes in the perception of and endogenous pain modulation by visceral stimuli in IBS patients have been delineated. As shown in Table 2, patients with severe symptoms had higher scores for anxiety or depression, which is consistent with the findings of a previous study. Among the patients with severe symptoms, anxiety and depression were related to the abdominal pain or discomfort score, although the association with anxiety was not significant. These findings imply that central perceptual differences in visceral stimuli may arise from psychological differences.
A biopsychosocial model has been suggested to explain the complexity of the pathophysiology of IBS.3 This includes reciprocal influences and feedback mechanisms between gastrointestinal changes and psychological factors, and emphasizes the strong relationship between gastrointestinal symptoms and psychological factors. From our data, the most important factor in the anxiety and depression experienced by IBS patients was symptom severity. Symptom severity was also affected by psychological factors, which was apparent in the higher abdominal pain or discomfort scores of patients with severe symptoms, who also had anxiety or depression, compared with those of patients who did not.
It is well recognized that patients with IBS and other functional gastrointestinal disorders experience considerable impairment of their health-related QOL.31-34 Many studies have reported that the impairment of the QOL of IBS patients is associated with the degree of IBS-related symptoms.13,21,35,36 However, several recent studies have shown that only some of this impairment is explained by the symptoms of functional gastrointestinal disorders and that psychological factors have a major and unique negative impact on health-related QOL.35,37-40 Our data support the importance of psychological factors in the QOL of Korean IBS patients. We have shown that depression is an independent factor determining the QOL of IBS patients. This is consistent with the findings of previous studies, which showed that psychiatric disorders can directly impair health-related QOL.35,37
Although the C-IBS patients had more frequent anxiety and depression than the other subtypes in our study, the IBS subtypes did not affect the impairment of the patients' IBS-QOL, which is consistent with reports in the literature.41 This might be attributable to the fact that symptom severity was the most important factor affecting QOL.
Antidepressants have proven effective for abdominal pain and are recommended for moderate to severe IBS symptoms because psychotropic medications like antidepressants are considered to have central and peripheral neuromodulatory effects.42 They are typically used in IBS management at low doses for their neuromodulatory effects. The high prevalence of psychiatric illness in IBS, as shown in our study, makes the management of these psychiatric symptoms with psychotropic drugs appropriate. Furthermore, because our data revealed the importance of depression as a determent of the IBS-specific QOL, treating comorbid depression with antidepressants can reduce the impairment of QOL associated with IBS, and enable IBS patients to better adjust to their health problem.
The question arises: Do the IBS symptoms aggravate the patients' anxiety and depression or do their anxiety and depression exacerbate their IBS symptoms? The relationships between QOL and anxiety or depression are also the same. Because this was a cross-sectional study and not a longitudinal one, it is difficult to distinguish the cause from the effect. It is clear that IBS symptoms and anxiety or depression have reciprocal and feedback effects on each other.
Our study has several limitations, including the small sample size and the inclusion of tertiary-care patients, who may be more distressed than other patients. These factors may hinder generalizations and unfairly inflate the psychiatric aspects of IBS. However, our sample was large enough to explain the importance of psychological factors in the gastroenterology clinic.
In conclusion, anxiety and depression are common in Korean patients with IBS. IBS is strongly associated with anxiety and depression, which are in turn strongly associated with symptom severity. Impairment of the patients' QOL depends significantly on both the severity of their symptoms and their depression. Because QOL assessments encompass emotional and social dimensions as well as physical dimensions, it is important to discern the contribution of anxiety and depression to the QOL in different cultural milieu. The identification of the specific psychological stressors associated with the exacerbation of IBS symptoms may help us plan treatments including both psychological and psychopharmacological interventions.
ACKNOWLEDGEMENTS
This work was partly supported by 2009 Seoul St. Mary's Clinical Medicine Research Program.
References
- 1.Drossman DA, Camilleri M, Mayer EA, Whitehead WE. AGA technical review on irritable bowel syndrome. Gastroenterology. 2002;123:2108–2131. doi: 10.1053/gast.2002.37095. [DOI] [PubMed] [Google Scholar]
- 2.Whitehead WE, Crowell MD. Psychologic considerations in the irritable bowel syndrome. Gastroenterol Clin North Am. 1991;20:249–267. [PubMed] [Google Scholar]
- 3.Drossman DA. Presidential address: gastrointestinal illness and the biopsychosocial model. Psychosom Med. 1998;60:258–267. doi: 10.1097/00006842-199805000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Levy RL, Olden KW, Naliboff BD, et al. Psychosocial aspects of the functional gastrointestinal disorders. Gastroenterology. 2006;130:1447–1458. doi: 10.1053/j.gastro.2005.11.057. [DOI] [PubMed] [Google Scholar]
- 5.Walker EA, Katon WJ, Jemelka RP, Roy-Bryne PP. Comorbidity of gastrointestinal complaints, depression, and anxiety in the Epidemiologic Catchment Area (ECA) Study. Am J Med. 1992;92(1A):26S–30S. doi: 10.1016/0002-9343(92)90133-v. [DOI] [PubMed] [Google Scholar]
- 6.Drossman DA. Do psychosocial factors define symptom severity and patient status in irritable bowel syndrome? Am J Med. 1999;107(5A):41S–50S. doi: 10.1016/s0002-9343(99)00081-9. [DOI] [PubMed] [Google Scholar]
- 7.Creed F, Fernandes L, Guthrie E, et al. The cost-effectiveness of psychotherapy and paroxetine for severe irritable bowel syndrome. Gastroenterology. 2003;124:303–317. doi: 10.1053/gast.2003.50055. [DOI] [PubMed] [Google Scholar]
- 8.Drossman DA, Toner BB, Whitehead WE, et al. Cognitive-behavioral therapy versus education and desipramine versus placebo for moderate to severe functional bowel disorders. Gastroenterology. 2003;125:19–31. doi: 10.1016/s0016-5085(03)00669-3. [DOI] [PubMed] [Google Scholar]
- 9.Vandvik PO, Lydersen S, Farup PG. Prevalence, comorbidity and impact of irritable bowel syndrome in Norway. Scand J Gastroenterol. 2006;41:650–656. doi: 10.1080/00365520500442542. [DOI] [PubMed] [Google Scholar]
- 10.Hillilä MT, Siivola MT, Färkkilä MA. Comorbidity and use of health-care services among irritable bowel syndrome sufferers. Scand J Gastroenterol. 2007;42:799–806. doi: 10.1080/00365520601113927. [DOI] [PubMed] [Google Scholar]
- 11.Boyce PM, Talley NJ, Balaam B, Koloski NA, Truman G. A randomized controlled trial of cognitive behavior therapy, relaxation training, and routine clinical care for the irritable bowel syndrome. Am J Gastroenterol. 2003;98:2209–2218. doi: 10.1111/j.1572-0241.2003.07716.x. [DOI] [PubMed] [Google Scholar]
- 12.Lackner JM, Jaccard J, Krasner SS, Katz LA, Gudleski GD, Blanchard EB. How does cognitive behavior therapy for irritable bowel syndrome work? A mediational analysis of a randomized clinical trial. Gastroenterology. 2007;133:433–444. doi: 10.1053/j.gastro.2007.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hahn BA, Kirchdoerfer LJ, Fullerton S, Mayer E. Patient-perceived severity of irritable bowel syndrome in relation to symptoms, health resource utilization and quality of life. Aliment Pharmacol Ther. 1997;11:553–559. doi: 10.1046/j.1365-2036.1997.00160.x. [DOI] [PubMed] [Google Scholar]
- 14.Simrén M, Abrahamsson H, Svedlund J, Björnsson ES. Quality of life in patients with irritable bowel syndrome seen in referral centers versus primary care: the impact of gender and predominant bowel pattern. Scand J Gastroenterol. 2001;36:545–552. doi: 10.1080/003655201750153476. [DOI] [PubMed] [Google Scholar]
- 15.Si JM, Wang LJ, Chen SJ, Sun LM, Dai N. Irritable bowel syndrome consulters in Zhejiang province: the symptoms pattern, predominant bowel habit subgroups and quality of life. World J Gastroenterol. 2004;10:1059–1064. doi: 10.3748/wjg.v10.i7.1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gwee KA, Wee S, Wong ML, Png DJ. The prevalence, symptom characteristics, and impact of irritable bowel syndrome in an asian urban community. Am J Gastroenterol. 2004;99:924–931. doi: 10.1111/j.1572-0241.2004.04161.x. [DOI] [PubMed] [Google Scholar]
- 17.Xiong LS, Chen MH, Chen HX, et al. A population-based epidemiologic study of irritable bowel syndrome in South China: stratified randomized study by cluster sampling. Aliment Pharmacol Ther. 2004;19:1217–1224. doi: 10.1111/j.1365-2036.2004.01939.x. [DOI] [PubMed] [Google Scholar]
- 18.Thompson WG, Longstreth GF, Drossman DA, Heaton KW, Irvine EJ, Müller-Lissner SA. Functional bowel disorders and functional abdominal pain. Gut. 1999;45(Suppl 2):II43–II47. doi: 10.1136/gut.45.2008.ii43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thompson WG, Longstreth GF, Drossman DA, et al. Functional bowel disorders and functional abdominal pain. In: Drossman DA, Corazziari E, Talley NJ, et al., editors. Rome II: the functional gastrointestinal disorders: diagnosis, pathophysiology and treatment--a multinational consensus. 2nd ed. McLean: Degnon Associates; 2000. pp. 351–432. [Google Scholar]
- 20.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 21.Patrick DL, Drossman DA, Frederick IO, DiCesare J, Puder KL. Quality of life in persons with irritable bowel syndrome: development and validation of a new measure. Dig Dis Sci. 1998;43:400–411. doi: 10.1023/a:1018831127942. [DOI] [PubMed] [Google Scholar]
- 22.Park JM, Choi MG, Oh JH, et al. Cross-cultural validation of Irritable Bowel Syndrome Quality of Life in Korea. Dig Dis Sci. 2006;51:1478–1484. doi: 10.1007/s10620-006-9084-6. [DOI] [PubMed] [Google Scholar]
- 23.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 24.Herrmann C. International experiences with the Hospital Anxiety and Depression Scale: a review of validation data and clinical results. J Psychosom Res. 1997;42:17–41. doi: 10.1016/s0022-3999(96)00216-4. [DOI] [PubMed] [Google Scholar]
- 25.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 26.Oh SM, Min KJ, Park DB. A study on the standardization of the Hospital Anxiety and Depression Scale for Koreans: a comparison of normal, depressed and anxious groups. J Korean Neuropsychiatr Assoc. 1999;38:289–296. [Google Scholar]
- 27.Whitehead WE, Palsson O, Jones KR. Systematic review of the comorbidity of irritable bowel syndrome with other disorders: what are the causes and implications? Gastroenterology. 2002;122:1140–1156. doi: 10.1053/gast.2002.32392. [DOI] [PubMed] [Google Scholar]
- 28.Farthing MJ. Irritable bowel, irritable body, or irritable brain? BMJ. 1995;310:171–175. doi: 10.1136/bmj.310.6973.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Guthrie E, Barlow J, Fernandes L, et al. Changes in tolerance to rectal distension correlate with changes in psychological state in patients with severe irritable bowel syndrome. Psychosom Med. 2004;66:578–582. doi: 10.1097/01.psy.0000128899.22514.c0. [DOI] [PubMed] [Google Scholar]
- 30.Chang L. Brain responses to visceral and somatic stimuli in irritable bowel syndrome: a central nervous system disorder? Gastroenterol Clin North Am. 2005;34:271–279. doi: 10.1016/j.gtc.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 31.El-Serag HB, Olden K, Bjorkman D. Health-related quality of life among persons with irritable bowel syndrome: a systematic review. Aliment Pharmacol Ther. 2002;16:1171–1185. doi: 10.1046/j.1365-2036.2002.01290.x. [DOI] [PubMed] [Google Scholar]
- 32.Akehurst RL, Brazier JE, Mathers N, et al. Health-related quality of life and cost impact of irritable bowel syndrome in a UK primary care setting. Pharmacoeconomics. 2002;20:455–462. doi: 10.2165/00019053-200220070-00003. [DOI] [PubMed] [Google Scholar]
- 33.Haug TT, Mykletun A, Dahl AA. Are anxiety and depression related to gastrointestinal symptoms in the general population? Scand J Gastroenterol. 2002;37:294–298. doi: 10.1080/003655202317284192. [DOI] [PubMed] [Google Scholar]
- 34.Drossman DA, McKee DC, Sandler RS, et al. Psychosocial factors in the irritable bowel syndrome. A multivariate study of patients and nonpatients with irritable bowel syndrome. Gastroenterology. 1988;95:701–708. doi: 10.1016/s0016-5085(88)80017-9. [DOI] [PubMed] [Google Scholar]
- 35.Creed F, Ratcliffe J, Fernandez L, et al. Health-related quality of life and health care costs in severe, refractory irritable bowel syndrome. Ann Intern Med. 2001;134(9 Pt 2):860–868. doi: 10.7326/0003-4819-134-9_part_2-200105011-00010. [DOI] [PubMed] [Google Scholar]
- 36.Lee OY, Fitzgerald LZ, Naliboff B, et al. Impact of advertisement and clinic populations in symptoms and perception of irritable bowel syndrome. Aliment Pharmacol Ther. 1999;13:1631–1638. doi: 10.1046/j.1365-2036.1999.00657.x. [DOI] [PubMed] [Google Scholar]
- 37.Naliboff BD, Balice G, Mayer EA. Psychosocial moderators of quality of life in irritable bowel syndrome. Eur J Surg Suppl. 1998;(583):57–59. doi: 10.1080/11024159850191256. [DOI] [PubMed] [Google Scholar]
- 38.Spiegel BM, Gralnek IM, Bolus R, et al. Clinical determinants of health-related quality of life in patients with irritable bowel syndrome. Arch Intern Med. 2004;164:1773–1780. doi: 10.1001/archinte.164.16.1773. [DOI] [PubMed] [Google Scholar]
- 39.Halder SL, Locke GR, 3rd, Talley NJ, et al. Impact of functional gastrointestinal disorders on health-related quality of life: a population-based case-control study. Aliment Pharmacol Ther. 2004;19:233–242. doi: 10.1111/j.0269-2813.2004.01807.x. [DOI] [PubMed] [Google Scholar]
- 40.Whitehead WE, Burnett CK, Cook EW, 3rd, Taub E. Impact of irritable bowel syndrome on quality of life. Dig Dis Sci. 1996;41:2248–2253. doi: 10.1007/BF02071408. [DOI] [PubMed] [Google Scholar]
- 41.Schmulson M, Lee OY, Chang L, Naliboff B, Mayer EA. Symptom differences in moderate to severe IBS patients based on predominant bowel habit. Am J Gastroenterol. 1999;94:2929–2935. doi: 10.1111/j.1572-0241.1999.01440.x. [DOI] [PubMed] [Google Scholar]
- 42.American Gastroenterology Association. American Gastroenterological Association medical position statement: irritable bowel syndrome. Gastroenterology. 2002;123:2105–2107. doi: 10.1053/gast.2002.37095b. [DOI] [PubMed] [Google Scholar]