Abstract
We report a rare case of vesico-acetabular fistula due to an improperly treated pelvic fracture with urinary stone formation in the joint cavity. This complication was related to an unrecognized mechanism of bladder wall entrapment in the acetabular floor defect during weight bearing. This situation led to several mistreatment decisions in our case and should be always considered by urologists dealing with patients after major pelvic trauma. In this case report, we analyze the publications related to this problem, discuss the main mechanisms of bladder wall damage after acetabular fracture, and propose tips for diagnosis and treatment.
Keywords: Malunited fractures, Multiple trauma, Urinary bladder diseases, Urinary bladder fistula, Urinary calculi
Bladder trauma is a common comorbidity of pelvic fractures. Porter et al report a frequency of bladder injury of as high as 15% in acetabular fractures resulting from the lateral load mechanism compared with just 2% for the axial load mechanism [1]. Here we report a rare urologic complication as the consequence of a missed bladder entrapment after an untreated pelvic fracture.
CASE REPORT
A 42-year-old man was admitted with a recurring vesicocutaneous fistula on the lateral surface of the left hip after two surgical repairs. Three years previously he had experienced a major pelvic trauma (closed left acetabular and left hip fracture) in a motor vehicle accident with immobilization being the only treatment applied. Three months after the accident, the patient denoted urine leakage from a small orifice on the left hip. He used two to three incontinence pads per day for the leakage. During the following 2 years the patient twice underwent surgical treatment (extraperitoneal fistula excision and bladder wall suturing) in a small rural hospital. The fistula recurred shortly after both operations.
Admission radiograms disclosed ankylosis of the left hip joint, avascular necrosis of the femoral head, and central hip dislocation through the perforated acetabulum (Fig. 1).
FIG. 1.
Computed tomography-tomogram showing bony fragment displacement and malunion after the left-side hip and pelvic fractures, which led to collapse of the femur head as the result of avascular necrosis and protrusion of the femur into the perforated acetabulum (central hip dislocation).
On the lateral surface of the left hip in the projection of the greater trochanter, there was a 2 mm fistula orifice with hyperemic rims and discharge confirmed biochemically to be urine. There were no clinical signs of systemic or local inflammation.
The median micturition volume was 210 ml with a maximum flow speed of 18 ml/s according to the uroflowmetry. Otherwise, the patient was healthy and all laboratory parameters were within the normal ranges.
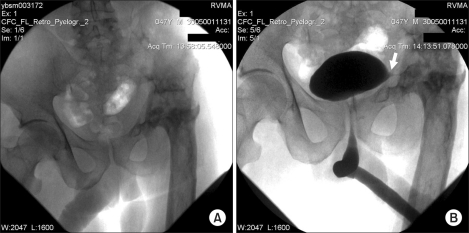
Neither sonography nor urethrocystoscopy yielded any abnormal findings. The cystography combined with the fistulography showed contrast extravasation through the left bladder wall but could not elucidate any relevant information about the fistula tract's course or its relation to the pelvic bones and the hip joint (Fig. 2). To obtain this information, we performed multispiral computed tomography (CT) combined with CT-fistulography.
FIG. 2.
Panoram X-Ray of pelvis (A) and miction cystourethrography (B). Arrow points to extravasation of the contrast medium.
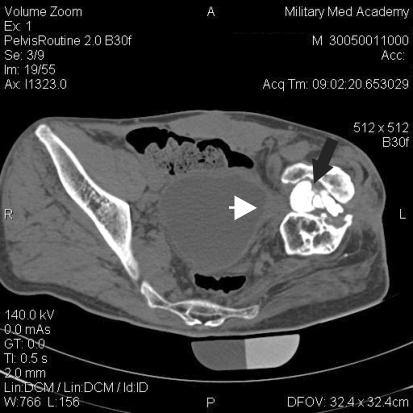
The nonenhanced CT images showed a drastic disfigurement of the left hip joint with some dense structures up to 5 cm in size lying in the joint cavity (Fig. 3).
FIG. 3.
Non-enhanced computed tomography of the pelvis. Black arrow shows the left hip joint with free-lying dense objects within. The arrowhead points to the site of bladder wall impingement.
A fistulography showed contrast extension to the bladder with excellent visualization of the fistula tract within the left hip joint (Fig. 4).
FIG. 4.
Computed tomography-fistulography. Arrow shows contrast medium within the left hip joint (fistula tract) extending to the bladder lumen.
The patient underwent a retroperitoneal fistula excision and a double-layer closure of the bladder wall. The patient was discharged on the 14th postoperative day, and cystography showed no contrast extravasation. No signs of urine leakage in the old fistula location were evident.
The fistula and urinary leakage recurred within 2 months. A decrease in mean bladder volume to 130 ml was found according to the bladder diary and during the bladder filling through the urethral catheter.
A second operation was performed 3 months later. Wide dissection of the left bladder wall was performed with a complete excision of scar tissue. Revision of the hip joint was performed. Up to 10 urinary stones 0.3 to 4 cm in size were extracted from the joint cavity (which were previously seen on CT). Also, ileocystoplasty was performed to augment the bladder, and the left rectus abdominis muscle flap was interposed between the bladder and the acetabulum.
Again we had a complete fistula closure in 14 days without discharge.
However, in 2 months, the fistula relapsed again. The bladder capacity during filling was 150 ml with a postvoid residual volume of 20 to 30 ml.
After analyzing the previous failures, we decided to make a urinary diversion as a salvage procedure for this patient. The Bricker procedure was chosen by the patient after explanation of all possible variants (the patient refused to catheterize himself because of living in rural conditions very far from any medical help). Cystectomy was not performed because the access to the bladder was virtually impossible as the result of the previous procedures.
After the operation, discharge from the fistula continued with significant decrease of the amount and change in appearance to a whitish cloudy liquid.
We suspected joint osteomyelitis to be the most probable cause for these manifestations. The patient was referred to the orthopaedic center for further treatment. During the next 2 months, the patient two joint revisions with the removal of the nonviable bone tissue and open reduction internal fixation (ORIF) to stabilize the pelvic bones. These were the final steps in the treatment of this patient.
DISCUSSION
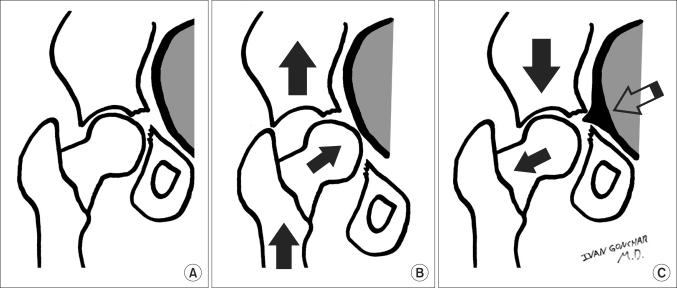
According to current guidelines, acetabular fractures with articular displacement of more than 2 mm, as observed in our patient, should be treated by the ORIF procedure [2,3]. Left without fixation, the bony fragments in this weight-bearing area could lead to bladder wall entrapment by the mechanism demonstrated in Fig. 5. During weight bearing under the circumstances of an unstable fracture, the iliac gets displaced cranially. Together with the central dislocation of the hip, this leads to bladder wall jamming between the bony fragments.
FIG. 5.
Mechanism of bladder wall entrapment in central hip dislocation resulting from lateral load acetabular fracture: (A) Acetabular fracture (B) Dislocation, weight bearing in the fracture without fixation. (C) Reduction, release of the weight-bearing stress in the fracture left without fixation.
A failure to reduce the bladder impingement leads to local ischemic and mechanical damage causing a connection between the bladder lumen and the joint cavity to ensue. Regularly rising pressure within the bladder can press the bladder wall against the sharp bony fragments (if present), which could also contribute to the relapse of the fistula, even with soft tissue interposition, as long as the fracture is left without ORIF and special care is taken to remove all sharp bony prominences in the bladder vicinity.
Delayed presentation of the bladder entrapment secondary to the nonoperative treatment of the lateral compression pelvic fracture has been reported in the literature, with authors particularly recommending the use of CT with bladder contrast or magnetic resonance tomography if an injury is treated nonoperatively because of the high probability of occult bladder entrapment and the unreliability of cystography for visualization [4-8].
In our experience, CT-fistulography was a more relevant investigation than cystography. Also, previously, an acetabular wall defect in an intimate relation to the truncated bladder extension was cited as a pathognomonic finding of acetabular bladder entrapment on the CT images [7], which we also observed in our patient. These two signs (fistula tract visualization during CT-fistulography and bladder wall extension towards the acetabular perforation) are the tips for the correct diagnosis of bladder wall entrapment.
Concerning the orthopedic treatment options for this patient, restoration of the hip joint is feasible only after bladder integrity has been restored and pelvic ring stability is established. In cases of untreated acetabular fractures with a central hip dislocation, acetabular augmentation with meshes, bone grafting, and extended cups are often required if total hip arthroplasty (THA) is considered. One more point that should be taken into consideration is that our patient had the hip joint ankylosis for several years. THA of the ankylosed joint with the restoration of range of motion is possible as has been reported in the literature [9]. However, the clinical outcomes of this procedure are compromised by the long-term muscle disuse, resulting in atrophy and soft tissue contracture.
Discharge continuation after the urinary diversion in our case suggested osteomyelitis.
The treatment of joint osteomyelitis is usually two-staged. First, after the resection of all nonviable bone tissue and closure, a continuous irrigation system is established. When the perfusate is clean and cultures are negative, the cement/antibiotic molds in the form of hip prosthesis (spacer) should be placed into the bone canal and the joint cavity to maintain the joint space for several months with rehabilitation to prevent immobilization morbidity.
If there is no infection recurrence, THA can be performed after several months of observation.
In our case, the treatment strategy was suboptimal because the fistula excision and the bladder wall repair and prolonged bladder drainage had to be combined with the joint revision and ORIF. It was initially unclear that the patient, who was ambulating freely without assistance 3 years after the trauma, had an unstable pelvic fracture. Nevertheless, leaving the pelvis without fixation enables the bladder entrapment mechanism to work even after a successful reconstructive operation and creates conditions for fistula recurrence. Failure to eliminate the entrapment mechanism could lead to multiple operations up to salvage procedures with heterotopic urinary diversion.
This case of a vesico-acetabular fistula is an illustrative example of how a hidden cause for a pathology can lead to mistreatment. The bladder entrapment mechanism, encountered during the acute period of pelvic fractures, persisted in this patient for 3 years after the trauma, even when he regained the ability to walk without assistance, because of the malunion of the fractured bones, which led to the initial mistake in the clinical assessment. This issue should be considered by urologists when managing patients with urological problems related to pelvic trauma, especially in countries with high rates of trauma and difficulties for patients in reaching specialized medical help, as in our case.
ACKNOWLEDGEMENTS
The authors acknowledge Prof. Sergey Petrov, Head of Urology Clinic of Military Medical Academy, for being a scientific advisor for this article.
Footnotes
The authors have nothing to disclose.
References
- 1.Porter SE, Russell GV, Dews RC, Qin Z, Woodall J, Jr, Graves ML. Complications of acetabular fracture surgery in morbidly obese patients. J Orthop Trauma. 2008;22:589–594. doi: 10.1097/BOT.0b013e318188d6c3. [DOI] [PubMed] [Google Scholar]
- 2.Mayo KA. Open reduction and internal fixation of fractures of the acetabulum. Results in 163 fractures. Clin Orthop Relat Res. 1994;305:31–37. [PubMed] [Google Scholar]
- 3.de Ridder VA, de Lange S, Kingma L, Hogervorst M. Results of 75 consecutive patients with an acetabular fracture. Clin Orthop Relat Res. 1994;305:53–57. [PubMed] [Google Scholar]
- 4.Ochs BG, Marintschev I, Hoyer H, Rolauffs B, Culemann U, Pohlemann T, et al. Changes in the treatment of acetabular fractures over 15 years: analysis of 1266 cases treated by the German Pelvic Multicentre Study Group (DAO/DGU) Injury. 2010;41:839–851. doi: 10.1016/j.injury.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 5.Min W, Gaines RJ, Sagi HC. Delayed presentation of bladder entrapment secondary to nonoperative treatment of a lateral compression pelvic fracture. J Orthop Trauma. 2010;24:e44–e48. doi: 10.1097/BOT.0b013e3181a9ee1d. [DOI] [PubMed] [Google Scholar]
- 6.Banihani MN, Al-Azab RS, Waqfi NR, Kharashgah MN, Al Manasra AR. Vesicocutaneous fistula presenting as a thigh abscess. Singapore Med J. 2009;50:e336–e337. [PubMed] [Google Scholar]
- 7.Nehme A, Maalouf G, Oakes D, Ghantous I, Trousdale RT. Persistent bladder entrapment following acetabular fracture with subsequent vesical injury during total hip arthroplasty. A case report. J Bone Joint Surg Am. 2005;87:870–873. doi: 10.2106/JBJS.D.02029. [DOI] [PubMed] [Google Scholar]
- 8.McKee MD, Waddell JP. Entrapment of the bladder in an acetabular fracture. A case report. J Bone Joint Surg Am. 1997;79:113–117. doi: 10.2106/00004623-199701000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Rutz E, Schäfer D, Valderrabano V. Total hip arthroplasty after hip joint ankylosis. J Orthop Sci. 2009;14:727–731. doi: 10.1007/s00776-009-1390-3. [DOI] [PubMed] [Google Scholar]