Abstract
OBJECTIVE:
To determine patterns of comorbidity, functioning, and service use for US children with attention-deficit/hyperactivity disorder (ADHD).
METHODS:
Bivariate and multivariable cross-sectional analyses were conducted on data from the 2007 National Survey of Children's Health on 61 779 children ages 6 to 17 years, including 5028 with ADHD.
RESULTS:
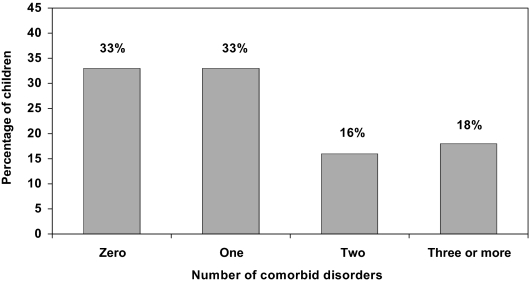
Parent-reported diagnosed prevalence of ADHD was 8.2%. Children with ADHD were more likely to have other mental health and neurodevelopmental conditions. Parents reported that 46% of children with ADHD had a learning disability versus 5% without ADHD, 27% vs 2% had a conduct disorder, 18% vs 2% anxiety, 14% vs 1% depression, and 12% vs 3% speech problems (all P < .05). Most children with ADHD had at least 1 comorbid disorder: 33% had 1, 16% had 2, and 18% had 3 or more. The risk for having 3 or more comorbidities was 3.8 times higher for poor versus affluent children (30% vs 8%). Children with ADHD had higher odds of activity restriction (odds ratio: 4.14 [95% confidence interval: 3.34–5.15]), school problems (odds ratio: 5.18 [95% confidence interval: 4.47–6.01]), grade repetition, and poor parent-child communication, whereas social competence scores were lower and parent aggravation higher. Functioning declined in a stepwise fashion with increasing numbers of comorbidities, and use of health and educational services and need for care coordination increased.
CONCLUSIONS:
Clinical management of ADHD must address multiple comorbid conditions and manage a range of adverse functional outcomes. Therapeutic approaches should be responsive to each child's neurodevelopmental profile, tailored to their unique social and family circumstances, and integrated with educational, mental health and social support services.
Keywords: ADHD, health outcomes, children
WHAT'S KNOWN ON THIS SUBJECT:
Attention-deficit/hyperactivity disorder (ADHD) is known to be associated with a range of mental health and neurodevelopmental comorbidities, but the pattern of these comorbidities and their relationship to child and family functioning and service use at the population level investigated has not been found in previous studies.
WHAT THIS STUDY ADDS:
Two-thirds of US children with ADHD have comorbid conditions. Social and educational functioning declines with more comorbidities and cross-sector service use and need for care coordination increase. Management of ADHD should be tailored to each child's neurodevelopmental profile.
Attention-deficit/hyperactivity disorder (ADHD) is 1 of the most common cognitive and behavioral disorders currently diagnosed in US children of school age,1 with an estimated annual societal cost of $34 billion to $52 billion.2 Children with ADHD have elevated problems in many areas, including academic functioning and strained social and family relationships.3,4 Studies also show that children with ADHD commonly exhibit additional mental health and neurodevelopmental comorbidities, including learning disabilities,5–7 epilepsy,8 tic and communication disorders,9–11 conduct disorder,4,12 anxiety,13,14 and depression.15 Presence of comorbidities has, in turn, been associated with poorer functioning in social and educational domains.14,16–19 However, most existing studies of children with ADHD have been conducted on clinic-based or small-scale community samples that are not representative of the general population of children in the US and do not use adequate samples to measure the effect of multiple comorbidities.20
It is essential to understand patterns of comorbidity, functioning, and service use among children with ADHD so services can be designed to meet the population's needs, and clinicians can be optimally responsive to patterns of illness they are likely to encounter in practice. Understanding the functional impact of ADHD also provides an indication of how well the existing system of care is performing. This study uses data from the 2007 National Survey of Children's Health (NSCH) to examine patterns of comorbidity, functioning, and service use for US children with ADHD. We chose comorbid conditions based on prior studies suggesting possible associations with ADHD and measures of function and service use that best encompassed health, education, and social domains. This is the first US population-based study to examine associations between ADHD and a comprehensive set of comorbidities, and to address the relationship between multiple comorbidities and functioning and service use. We hypothesized that comorbidities would be highly prevalent among children with ADHD, and that each additional comorbidity would be associated with worse functioning and greater service use across health, educational, and social domains.
METHODS
Sample
The 2007 NSCH was conducted by the National Center for Health Statistics as a module of the State and Local Area Integrated Telephone Survey. The NSCH used a stratified random-digit-dial sampling design to achieve a nationally representative sample of 91 642 parents of children aged 0 to17. One child was randomly selected from each household, and a detailed telephone interview was conducted with the parent or guardian who knew the most about the child's health and health care. Interviews of ∼30 minutes were conducted in English and Spanish. The overall weighted response rate (American Association for Public Opinion Research rate 4) was 51.2%, assuming that telephone numbers that rang with no answer or were busy on all call attempts were nonresidential.
The study sample includes 64 076 children ages 6 to 17 from the NSCH. The sample was further restricted to include only individuals with no missing data on the study covariates, except household income, which was multiply imputed by National Center for Health Statistics statisticians and applied to our analyses.21 This produces a sample size of N = 61 779 children. There is a small amount of variability in sample size for different functioning and service use measures because of missing data on the outcome. The sample size never dipped below 59 941. A total of 5028 children were available for the analyses that examine factors associated with outcomes for children with ADHD.
To produce population-based estimates, data records were assigned a sampling weight. NSCH weights were designed to minimize bias by incorporating adjustments for various forms of survey nonresponse, including poststratification so the sample matches population control totals on key demographic variables obtained from the American Community Survey. Additional details on the NSCH design are reported elsewhere.21 This study was exempted by the University of California, Los Angeles, institutional review board.
Measures
ADHD and Comorbid Disorders
Parents were asked if a doctor or health care provider ever told them that their child had ADHD, and if so, if their child currently had ADHD. Children were identified as having ADHD if parents responded “yes” to both questions. Ten potential comorbid disorders were identified in the same manner: learning disability; conduct disorder; anxiety; depression; speech problems; autism spectrum disorder; hearing problems; epilepsy or seizures; vision problems; and Tourette's syndrome.
Child and Family Functioning
Parents reported an activity restriction if the child was “limited or prevented in his/her ability to do things most children of the same age can do.” School functioning was assessed by parent report of a contact in the past year by the school about problems and if the child ever repeated a grade. Social competence was measured by parent ratings (0: never; 1: rarely; 2: sometimes; 3: usually; 4: always) of how often the child does the following: shows respect for teachers and neighbors; gets along well with other children; tries to understand others' feelings; and tries to resolve conflicts. Items were summed to create a composite, with higher scores indicating more competence. This scale has strong internal validity, good reliability, and predicts other indicators of positive behavior.22
The Aggravation in Parenting scale23 measures stress in parenting by asking how often the child was much harder to care for than others, does things that really bothers them, and made them feel angry (0: never; 1: rarely; 2: sometimes; 3: usually; 4: always). Items were summed to create a scale ranging from 0 to 12. This measure has been used across multiple previous studies and has good reliability and construct validity.23 Scales were analyzed as continuous and as indicators of low social competence (bottom 20%; score < 12) and high parent aggravation (top 20%; score > 4). Parent-child communication was assessed by parent report of how well they can “share ideas or talk about things that really matter.” Responses were dichotomized as “very well/somewhat well” versus “not very well/not well at all.”
Service Use
Measures of health and educational service use include parent report of any preventive health visit in the past year, any mental health visit in the past year, and whether the child received special education. Parents also reported if they needed “extra help arranging or coordinating care” across different service providers in the previous year.
Study Covariates
Study covariates include household income (<100% federal poverty level [FPL], 100–199% FPL, 200–299% FPL, 300–399% FPL, and ≥400% FPL), family structure, race/ethnicity, highest parent education, child age in years, child gender, and global child health status.
Analysis
All statistical analyses were performed using Stata 11.0 (Stata Corp, College Station, TX). Survey estimation procedures were applied, and the Taylor-series linearization method adjusted the SEs for the complex survey design. χ2 tests were calculated to compare prevalence of comorbid disorders for children with ADHD versus those without, and relative risks were adjusted for sociodemographics. For children with ADHD, we constructed a comorbidity index, which counts the total number of comorbid conditions (range: 0–3 or more).
Child and family functioning and service use were analyzed in relation to the presence of an ADHD diagnosis and the number of comorbid conditions. χ2 and analysis of variance tests were used to evaluate differences between children with and without ADHD, and also to examine associations between comorbidity and functioning and service use for children with ADHD. Logistic and linear regression models added controls for sociodemographics and global child health status.
RESULTS
ADHD Prevalence and Comorbidity
Parent-reported diagnosed prevalence of ADHD for all children ages 6 to 17 was 8.2% (95% confidence interval [CI]: 7.7–8.7), corresponding with more than 4010 000 cases nationwide. Children with ADHD were more likely to also have each of 10 other mental health and neurodevelopmental disorders (Table 1). For example, 46% of children with ADHD had a learning disability versus 5% without ADHD, 27% vs 2% had a conduct disorder, 18% vs 2% anxiety, 14% vs 1% depression, and 12% vs 3% speech problems. Nine of the associations remained significant after adjustment for sociodemographics. In total, 67% of children with ADHD had at least 1 other reported mental health/neurodevelopmental disorder (compared with 11% in the population without ADHD). Among children with an ADHD diagnosis, 33% had 1 comorbid disorder, 16% had 2, and 18% had 3 or more (Fig 1).
TABLE 1.
Prevalence of Comorbid Disorders for Children With ADHD Versus Those Without (N = 61 779)
| No ADHD | ADHD | Adjusted Relative Riskb | 95% CI | |
|---|---|---|---|---|
| Learning disability (%) | 5.3 | 46.1a | 7.79 | 6.86–8.86 |
| Conduct disorder (%) | 1.8 | 27.4a | 12.58 | 10.23–15.48 |
| Anxiety (%) | 2.1 | 17.8a | 7.45 | 6.08–9.12 |
| Depression (%) | 1.4 | 13.9a | 8.04 | 6.09–10.62 |
| Speech problem (%) | 2.5 | 11.8a | 4.42 | 3.41–5.73 |
| Autism spectrum disorder (%) | 0.6 | 6.0a | 8.72 | 5.97–12.72 |
| Hearing problem (%) | 1.2 | 4.2a | 2.77 | 1.87–4.11 |
| Epilepsy or seizures (%) | 0.6 | 2.6a | 3.93 | 2.19–7.06 |
| Vision problem (%) | 1.4 | 2.3a | 1.47 | 0.98–2.20 |
| Tourette's syndrome (%) | 0.09 | 1.3a | 10.70 | 4.72–24.23 |
| Any MH/ND disorder (%) | 11.5 | 66.9a | 5.12 | 4.72–5.55 |
P < .05 for χ2 test.
Relative risks were adjusted for child age, gender, race/ethnicity, parent education, household income, and family structure.
FIGURE 1.
Percentage of children with ADHD who have comorbid disorders (N = 5 028).
Sociodemographics of ADHD Prevalence and Comorbidity
Parent-reported diagnosed prevalence of ADHD was higher for children in lower income households and families headed by single mothers (Table 2). The income gradient in ADHD prevalence was less steep than the gradient for comorbidity. Children in poor families were ∼1.4 times more likely to have an ADHD diagnosis than were children with incomes at 400% FPL or greater (10% vs 7%). The risk for having 3 or more comorbid conditions among children with ADHD was 3.8 times higher for poor versus most affluent children (30% vs 8%). Separate analyses (not shown) indicated each comorbid condition except anxiety and epilepsy, and Tourette'swas more common for poor children. Hispanic children were less likely than were white children to have an ADHD diagnosis, but more likely to have comorbid conditions. Comorbidity did not vary by child age or gender.
TABLE 2.
Sociodemographic Correlates of ADHD Prevalence and Comorbidity
| ADHD (%) (N = 61 779) ± | >3 Comorbid Disorders (%) (N = 5028) | |
|---|---|---|
| Household income | ||
| <100% FPL | 10a | 30a |
| 100–199% FPL | 8 | 20 |
| 200–299% FPL | 8 | 21 |
| 300–399% FPL | 7 | 12 |
| 400% FPL or greater | 7 | 8 |
| Family structure | ||
| Two biological/adoptive parents | 6a | 16 |
| Single mother | 12 | 22 |
| Other | 11 | 21 |
| Race/ethnicity | ||
| White | 9a | 16a |
| Black | 9 | 19 |
| Hispanic | 5 | 28 |
| Multiracial/other | 7 | 20 |
| Highest parent education | ||
| High school diploma | 9a | 24a |
| More than high school | 7 | 15 |
| Child age, y | ||
| 6–9 | 6a | 19 |
| 10–13 | 9 | 21 |
| 14–17 | 9 | 15 |
| Child gender | ||
| Male | 11a | 19 |
| Female | 4 | 17 |
P < .05 for χ2 test.
Associations Between ADHD, Comorbid Conditions, and Functioning
Children with ADHD had more reported problems across every indicator of functioning (Table 3). For example, 69% of parents with children who had ADHD were contacted about school problems, compared with 27% of other parents. Twenty-nine percent of children with ADHD had repeated a grade, compared with 9% of children without ADHD. Average parent aggravation scores were 4.9 for those with ADHD versus 2.9 for those without (53% vs 19% classified in high range).
TABLE 3.
Bivariate and Multivariable Associations Between ADHD, No. of Comorbid Disorders, and Child and Family Functioning
| No ADHD (N = 56 751)a | ADHD (N = 5028)a | No. of Comorbid Disorders (N = 5028)a |
||||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 or More | |||
| Bivariate | ||||||
| Activity restriction (%) | 5 | 24b | 7 | 16 | 34 | 59b |
| School problems (%) | 27 | 69b | 57 | 68 | 81 | 81b |
| Repeat grade (%) | 9 | 29b | 17 | 32 | 32 | 46b |
| Social competence (mean) | 13.3 | 11.5b | 12.2 | 11.7 | 11.2 | 10.1b |
| Low social competence (%) | 18 | 43b | 33 | 43 | 45 | 61b |
| Parent aggravation (mean) | 2.9 | 4.9b | 4.1 | 4.6 | 5.1 | 6.5b |
| High parent aggravation (%) | 19 | 53b | 40 | 48 | 56 | 83b |
| Poor communication (%) | 3 | 8b | 2 | 6 | 6 | 21b |
| Multivariablec | ||||||
| Activity restriction OR (95% CI) | — | 4.14b (3.34–5.15) | — | 2.35b (1.31–4.21) | 5.72b (3.17–10.33) | 12.58b (7.20–21.96) |
| School problems OR (95% CI) | — | 5.18b (4.47–6.01) | — | 1.49b (1.08–2.06) | 2.58b (1.70–3.91) | 2.45b (1.56–3.86) |
| Repeat grade OR (95% CI) | — | 3.71b (3.02–4.55) | — | 2.14b (1.38–3.29) | 2.07b (1.35–3.18) | 3.01b (1.93–4.70) |
| Social competence β (SE) | — | −1.50b (0.10) | −0.40 (0.22) | −0.61b (0.26) | −1.67b (0.29) | |
| Low social competence OR (95% CI) | — | 2.86b (2.46–3.31) | — | 1.42 (0.99–2.04) | 1.35 (0.89–2.05) | 2.41b (1.55–3.77) |
| Parent aggravation β (SE) | — | 1.80b (0.08) | — | 0.38b (0.19) | 0.70b (0.24) | 1.96b (0.23) |
| High parent aggravation OR (95% CI) | — | 4.30b (3.72–4.98) | — | 1.37 (0.98–1.92) | 1.67b (1.13–2.47) | 6.25b (4.03–9.64) |
| Poor communication OR (95% CI) | — | 2.55b (1.84–3.52) | — | 2.39b (1.18–4.84) | 2.01b (1.02–3.99) | 8.53b (4.41–16.52) |
Sample size varies slightly across different child and family functioning measures because of missing data on the outcome.
P < .05. Bivariate results are based on χ2 tests for dichotomous outcomes and analysis of variance for continuous outcomes.
Models include controls for child age, gender, race/ethnicity, parent education, household income, family structure, and global child health status.
Child and family functioning was distributed by the number of comorbid disorders for children with ADHD. Children with ADHD and 3 or more comorbid disorders exhibited severe deficits in functioning. For example, 59% of these children had an activity restriction, 81% had problems in school, 46% repeated a grade, 61% had low social competence, and 83% had parent aggravation scores classified as high.
Associations between ADHD and functioning remained significant in adjusted regression models. Children with ADHD had higher odds of activity restriction (odds ratio [OR]: 4.14 [95% CI: 3.34–5.15]), school problems (OR: 5.18 [95% CI: 4.47–6.01]), grade repetition, and poor communication, whereas social competence scores were lower and parent aggravation higher. For children with ADHD, the odds/β of poorer functioning increased in a step-wise fashion with increasing numbers of comorbidities (see Table 3). For example, compared with children with ADHD and no comorbid conditions, children with 3 or more comorbid disorders had the highest odds of activity restriction (OR: 12.58 [95% CI: 7.20–21.96]), whereas children with 2 (OR: 5.72 [95% CI: 3.17–10.33]) and 1 comorbid disorder (OR: 2.35 [95% CI: 1.31–4.21]) had intermediate odds.
Income Gradients in Functioning
Among those with ADHD, functioning was consistently lower for children in lower-income households (see Table 4). For example, children with ADHD who lived in poverty had a 44% prevalence of grade repetition, compared with 19% for those who had family incomes of 400% FPL or greater. Among poor children with ADHD, 52% had low social competence scores versus 34% for the most affluent. These associations remained significant with controls for sociodemographics (not shown).
TABLE 4.
Income Gradients in Child and Family Functioning Among Those With ADHD (N = 5028)a
| Functional Health Outcomes | Household Income Level |
||||
|---|---|---|---|---|---|
| Below 100% FPL | 100–199% FPL | 200–299% FPL | 300–399% FPL | 400% FPL or Greater | |
| Activity restriction (%) | 31 | 28 | 24 | 17 | 17b |
| School problems (%) | 77 | 72 | 66 | 71 | 61b |
| Repeat grade (%) | 44 | 32 | 32 | 17 | 19b |
| Social competence (mean) | 10.9 | 11.3 | 11.5 | 11.4 | 12.1b |
| Low social competence (%) | 52 | 46 | 46 | 41 | 34b |
| Parent aggravation (mean) | 5.3 | 5.0 | 4.8 | 4.8 | 4.5b |
| High parent aggravation (%) | 58 | 59 | 53 | 52 | 45b |
| Poor communication (%) | 10 | 9 | 7 | 10 | 3b |
Sample size varies slightly across different child and family functioning measures because of missing data on the outcome.
P < .05 based on χ2 tests for dichotomous outcomes and analysis of variance for continuous outcomes.
Associations Between ADHD, Comorbid Conditions, and Service Use
Children with ADHD consistently used more health, mental health, and education services than did other children (Table 5). Separate analyses (not shown) indicated that children with ADHD had higher health and mental health service use than did children with any other mental health or neurodevelopmental disorder. Among children with ADHD, mental health and education service use increased with each additional comorbid condition. For example, odds of special education use increased by 5.27 (95% CI: 3.55–7.82) with 1 comorbidity, 8.80 (95% CI: 5.58–13.87) with 2, and 16.04 (95% CI: 9.84–26.14) with 3. Most children with ADHD plus 3 or more comorbidities used each service, and nearly half of parents (42%) reported a need for more assistance with care coordination among the providers.
TABLE 5.
Health and Educational Service Use by ADHD Status and No. of Comorbid Disorders
| No ADHD (N = 56 751)a | ADHD (N = 5028)a | No. of Comorbid Disorders (N = 5028)a |
||||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 or More | |||
| Bivariate | ||||||
| Preventive health visit | 84 | 92a | 90 | 93 | 94 | 93 |
| Mental health visit | 6 | 48b | 35 | 42 | 60 | 72b |
| Special education services | 7 | 49b | 19 | 55 | 68 | 79b |
| Needed care coordination | 8 | 20b | 9 | 18 | 24 | 42b |
| Multivariablec | ||||||
| Preventive health visit OR (95% CI) | — | 2.19b (1.69–2.83) | — | 1.38 (0.81–2.36) | 1.58 (0.82–3.04) | 1.24 (0.62–2.50) |
| Mental health visit OR (95% CI) | — | 11.42b (9.63–13.55) | — | 1.33 (0.94–1.88) | 2.73b (1.82–4.09) | 4.55b (2.93–7.04) |
| Special education services OR (95% CI) | — | 9.88b (8.34–11.69) | — | 5.27b (3.55–7.82) | 8.80b (5.58–13.87) | 16.04b (9.84–26.14) |
| Needed care coordination OR (95% CI) | — | 3.01b (2.38–3.80) | — | 1.87 (0.98–3.58) | 2.52b (1.27–4.99) | 4.51b (2.21–9.21) |
Sample size varies slightly across different service use measures because of missing data on the outcome.
P < .05. Bivariate results are based on χ2 tests.
Models include controls for child age, gender, race/ethnicity, parent education, household income, family structure, and global child health status.
DISCUSSION
In 2007, ADHD was diagnosed for 8.2% of school-aged children in the US, corresponding to slightly more than 4 million cases nationwide. ADHD was significantly associated with all 10 mental health and neurodevelopmental conditions studied. The majority (67%) of children with ADHD had at least 1 other comorbidity. Almost one-fifth of children with ADHD had complex clinical pictures, with 3 or more comorbidities. The odds of poorer functioning, use of health and education services, and need for care coordination increased in a step-wise fashion with increasing numbers of comorbidities. These results have important implications for the organization and delivery of health care services for children with ADHD.
The parent-reported diagnosed prevalence of ADHD from the 2007 NSCH is comparable with that obtained in other studies, and matches more direct assessment from the National Health and Nutrition Examination Survey, 2001 to 2004 (8.7%).24,25 Rates of comorbidities reported in the literature have varied widely, owing to differing definitions of comorbid conditions, ages of the study cohorts, and origin of samples.13,26,27 Our estimate of a 67% comorbidity rate is consistent with 2 clinical samples in the US and Canada in which approximately two-thirds of children reported comorbid conditions.13,17 These findings support an emerging view that “pure” ADHD, in the absence of comorbidities, occurs in a minority of cases,26,28 even in population samples.29 Rates of specific comorbidities including learning disabilities,30–33 anxiety,31,34 depression,34,35 and conduct disorder,31–34 were broadly within the ranges currently reported from regional and clinical samples.
We observed steep social gradients for comorbidities. Poor children with ADHD had close to 4 times the risk of 3 or more comorbid conditions compared with the most affluent. Few studies examine ADHD comorbidity for poor children, although 1 study of Finnish adolescents found more comorbid externalizing disorders.16 Findings are consistent with a broader literature demonstrating that multiple health vulnerabilities, including physical health problems and psychosocial conditions like ADHD, tend to cluster together for children from families with lower socioeconomic status.36–40 Because children from low-income families typically have less access to health services, “over-diagnosis” of comorbidities in poorer children with ADHD is unlikely. One plausible explanation is that ADHD and other examined conditions could have certain common etiologic factors (eg, genetic susceptibility,41,42 maternal stress,43,44 and prenatal smoke exposure44,45) that are more prevalent in families with lower income.
Consistent with previous literature, children with ADHD had more problems across a wide range of school, social, and family functioning indicators.4,46,47 This study is novel in showing steep gradients, with each additional comorbid disorder associated with worse functioning across all domains, even controlling for sociodemographics. Children with ADHD and 3 or more comorbidities, corresponding to more than 700 000 children nationally, had particularly severe functional deficits. The very high prevalence of school problems (81%) and grade repetition (46%) indicates that existing management strategies are falling short of meeting the needs of these children. Grade repetition may substitute for more customized, proactive individual interventions. High parent-child communication problems and parent aggravation indicate that families need additional supports to maintain good quality relationships with their children and might benefit from individual and family counseling.48–50
The relationship between family income and functioning in children with ADHD has not been well studied; however, more hyperactivity and peer problems have been reported in children from lower income households.4 We found steep income gradients in social and educational functioning for children with ADHD. Reasons underlying these gradients were beyond the scope of this study, but the relative contributions of access to health and educational interventions, and presence of comorbidities need additional research.
Our findings have several implications for practice. First, comprehensive screening for other problems that occur with ADHD is necessary, and treatment profiles should be tailored by comorbidity status and levels of functional impairment in home and school settings.51–54 Current AAP guidelines call for assessment and management of comorbidity with ADHD.55,56 Most physicians report screening for common comorbidities such as depression,57 but only 20% agree that they are adequately trained to treat children with ADHD and comorbidity.58 A need for more supports to establish a chronic disease management approach also is suggested by studies, including written intervention plans tailored to each child's neurodevelopmental profile and protocols for follow-up monitoring/assessment of functioning.58,59 Children from families with a lower socioeconomic status had more comorbidity and impaired functioning, which indicates more intensive assessment and treatment from the start to help manage their illness are needed. Finally, health and educational service use increased for children with ADHD and multiple comorbidities, and nearly half of parents reported a need for more care coordination with complex comorbidity. These findings reinforce a need for greater integration of primary care with mental health, education, and social services.60–62
Study limitations include parent report and the cross-sectional nature of the data, which precludes inferences about cause. The parent-reported diagnosed prevalence of ADHD was consistent with estimates using other methods; however, we could not gauge the possible rate of false-positives or false-negatives in the sample. Parent reports have been widely used in the literature,63–66 and our comorbidity patterns were similar with clinical and regional studies. This gives us confidence our results are valid representations of comorbidity and related consequences for children diagnosed with ADHD in the US. Our study did not address medication use or specific behavioral interventions, and we could not determine whether ADHD developed before or after onset of the comorbid conditions. Our study is novel in demonstrating steep increases in impairment and service use with multiple comorbidities, and future research should expand this by examining costs. Study strengths include the large, nationally representative sample and data on a wide range of comorbidities, affording a unique opportunity to explore relationships between comorbidities, functioning, and service use at the population level.
CONCLUSIONS
Professionals and parents need to be aware of the high prevalence of mental health/neurodevelopmental comorbidities among school-aged children with ADHD in the United States. Patterns of worsening function with increasing numbers of comorbidities reflect the challenge of meeting the needs of children with complex clinical pictures within the current system of care. Comparative effectiveness studies of primary care treatment strategies for ADHD in children have been identified as an Institute of Medicine priority.67 Our findings indicate that such studies are urgently needed. Testing innovative models of care integration across health, mental health, educational, and social domains would be a fruitful area of research to determine the best management approach, especially for those children at greatest risk of poorer function.60–62,68–71
ACKNOWLEDGMENTS
This work was supported in part by funding to Dr Halfon from the Maternal and Child Health Bureau of the Health Resources and Services Administration Interdisciplinary Maternal and Child Health Training Program (2 T76M600014:11) and to Dr Larson from the National Institutes of Health Loan Repayment Program.
We also thank Ms Louba Aaronson and Ms Amy Graber, who assisted with data analysis and manuscript preparation.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
Funded by the National Institutes of Health (NIH).
- ADHD
- attention-deficit/hyperactivity disorder
- NSCH
- National Survey of Children's Health
- FPL
- federal poverty level
- CI
- confidence interval
- OR
- odds ratio
REFERENCES
- 1. Banerjee TD, Middleton F, Faraone SV. Environmental risk factors for attention-deficit hyperactivity disorder. Acta Paediatr. 2007;96(9):1269–1274 [DOI] [PubMed] [Google Scholar]
- 2. Pelham WE, Foster EM, Robb JA. The economic impact of attention-deficit/hyperactivity disorder in children and adolescents. J Pediatr Psychol. 2007;32(6):711–727 [DOI] [PubMed] [Google Scholar]
- 3. Currie J, Stabile M. Child mental health and human capital accumulation: the case of ADHD. J Health Econ. 2006;25(6):1094–1118 [DOI] [PubMed] [Google Scholar]
- 4. Strine TW, Lesesne CA, Okoro CA, et al. Emotional and behavioral difficulties and impairments in everyday functioning among children with a history of attention-deficit/hyperactivity disorder. Prev Chronic Dis. 2006;3(2):A52. [PMC free article] [PubMed] [Google Scholar]
- 5. Pastor PN, Reuben CA. Diagnosed attention deficit hyperactivity disorder and learning disability: United States, 2004–2006. Vital Health Stat 10. 2008;(237):1–14 [PubMed] [Google Scholar]
- 6. August GJ, Garfinkel BD. Comorbidity of ADHD and reading disability among clinic-referred children. J Abnorm Child Psychol. 1990;18(1):29–45 [DOI] [PubMed] [Google Scholar]
- 7. Mayes SD, Calhoun SL. Learning, attention, writing, and processing speed in typical children and children with ADHD, autism, anxiety, depression, and oppositional-defiant disorder. Child Neuropsychol. 2007;13(6):469–493 [DOI] [PubMed] [Google Scholar]
- 8. Tai YM, Chiu HW. Comorbidity study of ADHD: applying association rule mining (ARM) to National Health Insurance Database of Taiwan. Int J Med Inform. 2009;78(12):e75–e83 [DOI] [PubMed] [Google Scholar]
- 9. Freeman RD. Tic disorders and ADHD: answers from a world-wide clinical data set on Tourette syndrome. Eur Child Adolesc Psychiatry. 2007;16(1 suppl):15–23 [DOI] [PubMed] [Google Scholar]
- 10. Geurts HM, Embrechts M. Language profiles in ASD, SLI, and ADHD. J Autism Dev Disord. 2008;38(10):1931–1943 [DOI] [PubMed] [Google Scholar]
- 11. McGrath LM, Hutaff-Lee C, Scott A, Boada R, Shriberg LD, Pennington BF. Children with comorbid speech sound disorder and specific language impairment are at increased risk for attention-deficit/hyperactivity disorder. J Abnorm Child Psychol. 2008;36(2):151–163 [DOI] [PubMed] [Google Scholar]
- 12. Scahill L, Schwab-Stone M, Merikangas KR, Leckman JF, Zhang H, Kasl S. Psychosocial and clinical correlates of ADHD in a community sample of school-age children. J Am Acad Child Adolesc Psychiatry. 1999;38(8):976–984 [DOI] [PubMed] [Google Scholar]
- 13. Elia J, Ambrosini P, Berrettini W. ADHD characteristics: I. Concurrent comorbidity patterns in children & adolescents. Child Adolesc Psychiatry Ment Health. 2008;2(1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bowen R, Chavira DA, Bailey K, Stein MT, Stein MB. Nature of anxiety comorbid with attention deficit hyperactivity disorder in children from a pediatric primary care setting. Psychiatry Res. 2008;157(1–3):201–209 [DOI] [PubMed] [Google Scholar]
- 15. Ostrander R, Crystal DS, August G. Attention deficit-hyperactivity disorder, depression, and self- and other-assessments of social competence: a developmental study. J Abnorm Child Psychol. 2006;34(6):773–787 [DOI] [PubMed] [Google Scholar]
- 16. Hurtig T, Ebeling H, Taanila A, et al. ADHD and comorbid disorders in relation to family environment and symptom severity. Eur Child Adolesc Psychiatry. 2007;16(6):362–369 [DOI] [PubMed] [Google Scholar]
- 17. Klassen AF, Miller A, Fine S. Health-related quality of life in children and adolescents who have a diagnosis of attention-deficit/hyperactivity disorder. Pediatrics. 2004;114(5). Available at: www.pediatrics.org/cgi/content/full/114/5/e541 [DOI] [PubMed] [Google Scholar]
- 18. Nijmeijer JS, Minderaa RB, Buitelaar JK, Mulligan A, Hartman CA, Hoekstra PJ. Attention-deficit/hyperactivity disorder and social dysfunctioning. Clin Psychol Rev. 2008;28(4):692–708 [DOI] [PubMed] [Google Scholar]
- 19. Spencer TJ. Issues in the management of patients with complex attention-deficit hyperactivity disorder symptoms. CNS Drugs. 2009;23(suppl 1):9–20 [DOI] [PubMed] [Google Scholar]
- 20. Stein RE. Measurement of ADHD outcomes: implications for the future. Ambul Pediatr. 2007;7(suppl 1):140–143 [DOI] [PubMed] [Google Scholar]
- 21. Blumberg SJ, Foster EB, Frasier AM, et al. Design and operation of the National Survey of Children's Health, 2007. National Center for Health Statistics. Vital Health Stat 1. 2009; in Press [PubMed] [Google Scholar]
- 22. Blumberg S, Carle C, O'Connor K, Moore K, Lippman L. Social competence: development of an indicator for children and adolescents. Child Ind Res. 2008;1:176–197 [Google Scholar]
- 23. Macomber J, Moore K. Benchmarking Measures of Child and Family Well-being in the 1997 NSAF: Report No. 6. Washington, DC: The Urban Institute; 1999 [Google Scholar]
- 24. Froehlich TE, Lanphear BP, Epstein JN, Barbaresi WJ, Katusic SK, Kahn RS. Prevalence, recognition, and treatment of attention-deficit/hyperactivity disorder in a national sample of US children. Arch Pediatr Adolesc Med. 2007;161(9):857–864 [DOI] [PubMed] [Google Scholar]
- 25. Bloom B, Cohen RA, Freeman G. Summary health statistics for US children: National Health Interview Survey, 2007. National Center for Health Statistics. Vital Health Stat 10. 2009;239:1–80 [PubMed] [Google Scholar]
- 26. Ostrander R, Herman K, Sikorski J, Mascendaro P, Lambert S. Patterns of psychopathology in children with ADHD: a latent profile analysis. J Clin Child Adolesc Psychol. 2008;37(4):833–847 [DOI] [PubMed] [Google Scholar]
- 27. Furman L. What is attention-deficit hyperactivity disorder (ADHD)? J Child Neurol. 2005;20(12):994–1002 [DOI] [PubMed] [Google Scholar]
- 28. Gillberg C, Gillberg IC, Rasmussen P, et al. Coexisting disorders in ADHD: implications for diagnosis and intervention. Eur Child Adolesc Psychiatry. 2004;13(suppl 1):180–192 [DOI] [PubMed] [Google Scholar]
- 29. Kadesjö B, Gillberg C. The comorbidity of ADHD in the general population of Swedish school-age children. J Child Psychol Psychiatry. 2001;42(4):487–492 [PubMed] [Google Scholar]
- 30. Jensen PS, Martin D, Cantwell DP. Comorbidity in ADHD: implications for research, practice, and DSM-V. J Am Acad Child Adolesc Psychiatry. 1997;36(8):1065–1079 [DOI] [PubMed] [Google Scholar]
- 31. Spencer T, Biederman J, Wilens T. Attention-deficit/hyperactivity disorder and comorbidity. Pediatr Clin North Am. 1999;46(5):915–927, vii [DOI] [PubMed] [Google Scholar]
- 32. Spencer TJ. ADHD and comorbidity in childhood. J Clin Psychiatry. 2006;67(suppl 8):27–31 [PubMed] [Google Scholar]
- 33. Spencer TJ, Biederman J, Mick E. Attention-deficit/hyperactivity disorder: diagnosis, lifespan, comorbidities, and neurobiology. Ambul Pediatr. 2007;7(suppl 1):73–81 [DOI] [PubMed] [Google Scholar]
- 34. Angold A, Costello EJ, Erkanli A. Comorbidity. J Child Psychol Psychiatry. 1999;40(1):57–87 [PubMed] [Google Scholar]
- 35. Daviss WB. A review of comorbid depression in pediatric ADHD: etiology, phenomenology, and treatment. J Child Adolesc Psychopharmacol. 2008;18(6):565–571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Starfield B. Childhood morbidity: comparisons, clusers, and trends. Pediatrics. 1991;88(3):519–526 [PubMed] [Google Scholar]
- 37. Newacheck PW, Stoddard JJ. Prevalence and impact of multiple childhood chronic illnesses. Pediatrics. 1994;124(1):40–48 [DOI] [PubMed] [Google Scholar]
- 38. Starfield B, Riley AW, Witt WP, Robertson J. Social class gradients in health during adolescence. J Epidemiol Community Health. 2002;56(5):354–361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Starfield B, Robertson J, Riley A. Social class gradients and health in childhood. Ambul Pediatr. 2002;2(4):238–246 [DOI] [PubMed] [Google Scholar]
- 40. Van den Akker M, Buntinx F, Metsemakers JFM, Knottnerus JA. Multimorbidity in general practice: prevalence, incidence, and determinants of co-occuring chronic and recurrent diseases. J Clin Epidemiology. 1998;51(5):367–375 [DOI] [PubMed] [Google Scholar]
- 41. Cole J, Ball HA, Martin NC, Scourfield J, McGuffin P. Genetic overlap between measures of hyperactivity/inattention and mood in children and adolescents. J Am Acad Child Adolesc Psychiatry. 2009;48(11):1094–1101 [DOI] [PubMed] [Google Scholar]
- 42. Coghill D, Banaschewski T. The genetics of attention-deficit/hyperactivity disorder. Expert Rev Neurother. 2009;9(10):1547–1565 [DOI] [PubMed] [Google Scholar]
- 43. Grizenko N, Shayan YR, Polotskia A, Ter-Stepanian M, Joober R. Relation of maternal stress during pregnancy to symptom severity and response to treatment in children with ADHD. J Psychiatry Neurosci. 2008;33(1):10–16 [PMC free article] [PubMed] [Google Scholar]
- 44. Rodriguez R, Bohlin G. Are maternal smoking and stress during pregnancy related to ADHD symptoms in children? J Child Psychol Psychiatry. 2005;46(3):246–254 [DOI] [PubMed] [Google Scholar]
- 45. Froehlich TE, Lanphear BP, Auinger P, et al. Association of tobacco and lead exposure with attention-deficit/hyperactivity disorder. Pediatrics. 2009;124(6). Available at: www.pediatrics.org/cgi/content/full/124/6/e1054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Barbaresi WJ, Katusic SK, Colligan RC, Weaver AL, Jacobsen SJ. Long-term school outcomes for children with attention-deficit/hyperactivity disorder: a population-based perspective. J Dev Behav Pediatr. 2007;28(4):265–273 [DOI] [PubMed] [Google Scholar]
- 47. Loe IM, Feldman HM. Academic and educational outcomes of children with ADHD. Ambul Pediatr. 2007;7(suppl 1):82–90 [DOI] [PubMed] [Google Scholar]
- 48. Daly BP, Creed T, Xanthopoulos M, Brown RT. Psychosocial treatments for children with attention deficit/hyperactivity disorder. Neuropsychol Rev. 2007;17(1):73–89 [DOI] [PubMed] [Google Scholar]
- 49. Smith BH, Waschbusch DA, Willoughby MT, Evans S. The efficacy, safety, and practicality of treatments for adolescents with attention-deficit/hyperactivity disorder (ADHD). Clin Child Fam Psychol Rev. 2000;3(4):243–267 [DOI] [PubMed] [Google Scholar]
- 50. Wolraich ML, Wibbelsman CJ, Brown TE, et al. Attention-deficit/hyperactivity disorder among adolescents: a review of the diagnosis, treatment, and clinical implications. Pediatrics. 2005;115(6):1734–1746 [DOI] [PubMed] [Google Scholar]
- 51. Waxmonsky J. Assessment and treatment of attention deficit hyperactivity disorder in children with comorbid psychiatric illness. Curr Opin Pediatr. 2003;15(5):476–482 [DOI] [PubMed] [Google Scholar]
- 52. Reiff MI, Stein MT. Attention-deficit/hyperactivity disorder evaluation and diagnosis: a practical approach in office practice. Pediatr Clin North Am. 2003;50(5):1019–1048 [DOI] [PubMed] [Google Scholar]
- 53. Stein MT, Perrin JM. Diagnosis and treatment of ADHD in school-age children in primary care settings: a synopsis of the AAP practice guidelines. Pediatr Rev. 2003;24(3):92–98 [DOI] [PubMed] [Google Scholar]
- 54. Foster EM, Jensen PS, Schlander M, et al. Treatment for ADHD: is more complex treatment cost-effective for more complex cases? Health Serv Res. 2007;42(1 pt 1):165–182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. American Academy of Pediatrics Committee on Quality Improvement and Subcommittee on Attention-Deficit/Hyperactivity Disorder Clinical practice guideline: diagnosis and evaluation of the child with attention-deficit/hyperactivity disorder. Pediatrics. 2000;105(5):1158–1170 [DOI] [PubMed] [Google Scholar]
- 56. American Academy of Pediatrics Committee on Quality Improvement and Subcommittee on Attention-Deficit/Hyperactivity Disorder Clinical practice guideline: treatment of the school-aged child with attention deficit/hyperactivity disorder. Pediatrics. 2001;108(4):1033–1044 [DOI] [PubMed] [Google Scholar]
- 57. Chan E, Hopkins MR, Perrin JM, Herrerias C, Homer CJ. Diagnostic practices for attention deficit hyperactivity disorder: a national survey of primary care physicians. Ambul Pediatr. 2005;5(4):201–208 [DOI] [PubMed] [Google Scholar]
- 58. Wolraich M, Bard DE, Stein MT, Rushton JL, O'Connor KG. Pediatricians' attitudes and practices on ADHD before and after the development of ADHD pediatric practice guidelines. J Atten Disord. 2010;13(6):563–572 [DOI] [PubMed] [Google Scholar]
- 59. Epstein JN, Langberg PK, Mainwaring BA, Luzader CP, Stark LJ. Community-wide intervention to improve the attention-deficit/hyperactivity disorder assessment and treatment practices of community physicians. Pediatrics. 2008;122(1):19–27 [DOI] [PubMed] [Google Scholar]
- 60. Arons BS, Katz-Leavy J, Wittig AC, Wayne Holden E. Too young for ADHD: the potential role of systems of care. J Dev Behav Pediatr. 2002;23(suppl 1):S57–63 [DOI] [PubMed] [Google Scholar]
- 61. American Academy of Child and Adolescent Psychiatry Committee on Health Care Access and Economics Task Force on Mental Health Improving mental health services in primary care: reducing administrative and financial barriers to access and collaboration. Pediatrics. 2009;123(4):1248–1251 [DOI] [PubMed] [Google Scholar]
- 62. Committee on Psychosocial Aspects of Child and Family Health and Task Force on Mental Health The future of pediatrics: mental health competencies for pediatric primary care. Pediatrics. 2009;124(1):410–421 [DOI] [PubMed] [Google Scholar]
- 63. Altarac M, Saroha E. Lifetime prevalence of learning disability among US children. Pediatrics. 2007;119(suppl 1):S77–S83 [DOI] [PubMed] [Google Scholar]
- 64. Blanchard LT, Gurka MJ, Blackman JA. Emotional, developmental, and behavioral health of American children and their families: a report from the 2003 National Survey of Children's Health. Pediatrics. 2006;117(6). Available at: www.pediatrics.org/cgi/content/full/117/6/e1202 [DOI] [PubMed] [Google Scholar]
- 65. Gurney JG, McPheeters ML, Davis MM. Parental report of health conditions and health care use among children with and without autism: National Survey of Children's Health. Arch Pediatr Adolesc Med. 2006;160(8):825–830 [DOI] [PubMed] [Google Scholar]
- 66. Kogan MD, Blumberg SJ, Schieve LA, et al. Prevalence of parent-reported diagnosis of autism spectrum disorder among children in the US, 2007. Pediatrics. 2009;124(5):1395–1403 [DOI] [PubMed] [Google Scholar]
- 67. Institute of Medicine Committee on Comparative Effectiveness Research Prioritization Initial National Priorities for Comparative Effectiveness Research. Washington, DC: National Academies Press; 2009 [Google Scholar]
- 68. Foy JM, Earls MF. A process for developing community consensus regarding the diagnosis and management of attention-deficit/hyperactivity disorder. Pediatrics. 2005;115(1). Available at: www.pediatrics.org/cgi/content/full/115/1/e97 [DOI] [PubMed] [Google Scholar]
- 69. Kelleher KJ, Campos JV, Gardner WP. Management of pediatric mental disorders in primary care: where are we now and where are we going? Curr Opin Pediatr. 2006;18(6):649–653 [DOI] [PubMed] [Google Scholar]
- 70. Wolraich ML, Bickman L, Lambert EW, Simmons T, Doffing MA. Intervening to improve communication between parents, teachers, and primary care providers of children with ADHD or at high risk for ADHD. J Atten Disord. 2005;9(1):354–368 [DOI] [PubMed] [Google Scholar]
- 71. Leslie LK, Wolraich M. ADHD service use patterns in youth. J Pediatr Psychol. 2007;32(6):695–710 [DOI] [PubMed] [Google Scholar]