Abstract
Niemann-Pick type C1 disease arises from a mutation inactivating NPC1 protein that normally moves unesterified cholesterol from the late endosomal/lysosomal complex of cells to the cytosolic compartment for processing. As a result, cholesterol accumulates in every tissue of the body causing liver, lung and central nervous system disease. Treatment of the murine model of this disease, the npc1−/− mouse, subcutaneously with β-cyclodextrin (4,000 mg/kg) one time each week normalized cellular cholesterol metabolism in the liver and most other organs. At the same time, the hepatic dysfunction seen in the untreated npc1−/− mouse was prevented. The severity of cerebellar neurodegeneration also was ameliorated, although not entirely prevented, and the median lifespan of the animals was doubled. In contrast to these other organs, however, lung showed progressive macrophage infiltration with development of lipoid pneumonitis. These studies demonstrated that weekly cyclodextrin administration overcomes the lysosomal transport defect associated with the NPC1 mutation, nearly normalizes hepatic and whole animal cholesterol pools, and prevents the development of liver disease. Furthermore, this treatment slows cerebellar neurodegeneration, but has little or no effect on the development of progressive pulmonary disease.
Niemann-Pick type C1 (NPC1) disease arises when a mutation inactivates the protein, NPC1, which normally operates in association with NPC2 to move unesterified cholesterol (C) across the limiting membrane of the late endosomal/lysosomal (E/L) complex of cells to the cytosolic compartment where it can be metabolized and/or excreted (1). In the absence of NPC1 function, C continuously accumulates in every tissue of the body at rates proportional to the uptake of apoB100- and apoE-containing lipoproteins by each organ through receptor-mediated and bulk-phase endocytosis (2, 3). In the murine model of this disease, the NPC1 mouse, this leads to expansion of the whole animal cholesterol pool by 70–80 mg/day per kg body weight. In both the mouse and child, this accumulation of C is associated with macrophage infiltration and activation, and with parenchymal cell death in many organs including the liver, lung and central nervous system (3–5). Clinically, these histological alterations are manifest as enlargement of the liver and spleen, active liver disease, lipoid pneumonitis, and progressive neurological dysfunction.
One approach to the treatment of this genetic disorder is to limit the delivery of sterol to the target tissues which, in turn, would reduce the amount of C that is sequestered in a particular organ, and ameliorate cell death and severity of disease. For example, blocking the intestinal absorption of sterol in the NPC1 mouse with a drug like ezetimibe reduces the flow of cholesterol to the liver through uptake of chylomicron remnants. As a consequence, the size of the liver and the amount of C sequestered is reduced, and there is improvement in liver function abnormalities and molecular measures of inflammation (6). Alternatively, treatment with an agent such as an LXR agonist increases cholesterol loss from the central nervous system, presumably reducing the amount of apoE/C complex available for uptake into glia and neurons (7, 8). This, in turn, is associated with a reduction in glial activation and measures of inflammation, and with amelioration of the neurodegeneration (7).
A second, more effective approach to this disorder comes from the observation that administration of the cholesterol-binding agent, 2-hydroxypropyl-β-cyclodextrin (CYCLO), to the mutant mouse in vivo allows the C sequestered in the late E/L compartment of cells throughout the body to immediately move to the cytosolic compartment and be metabolized through normal pathways for excretion from the animal (9). After a single subcutaneous dose of CYCLO, in nearly every organ there is a rapid increase in the concentration of cholesteryl esters (CE), suppression of SREBP2 target genes and C synthesis, and activation of several LXR target genes. These changes all attest to the fact that the sequestered pool of C has rapidly moved to the metabolically active pool of sterol in the cytosolic compartment of cells. Over the next several days, this pool of excess cholesterol that is temporarily stored in the cytosolic compartment as CE, moves to the liver and is excreted from the body, predominantly as fecal acidic sterols (10). When CYCLO is administered to the mutant animal, either as a single dose or as repeated doses, the liver disease and neurodegeneration is significantly improved, and life expectancy is extended (6, 9, 11). This striking effect of CYCLO in acutely reversing or bypassing the transport defect present in the limiting membrane of the late E/L complex, provides an explanation for how the sequestered pool of C can be metabolized and excreted from the animal.
This observation, in turn, raises the important possibility that repeated doses of this compound might totally normalize whole animal cholesterol pools, and prevent clinical disease in the NPC1 mouse. This is particularly likely given the recent observations that the young NPC1 mouse over the course of a week sequesters about 490–560 mg/kg of excess C while a single dose of CYCLO can flush from the body approximately 500 mg/kg (9). Thus, the present studies were undertaken, first, to determine if weekly CYCLO administration could entirely prevent expansion of the whole animal sterol pool, and, further, whether this therapeutic effect would be seen equally in every organ. Second, additional investigations were undertaken to determine if this reduction in tissue cholesterol content correlated with histological and clinical evidence of amelioration of disease and with prolongation of life.
MATERIAL AND METHODS
Animals
Control (npc1+/+) and homozygous mutant (npc1−/−) mice were generated from heterozygous (npc1+/−) animals on a pure BALB/c background, and the pups were genotyped at 19 days of age (1, 2). All experimental protocols were approved by the Institutional Animal Care and Use Committee of The University of Texas Southwestern Medical School.
Diets and treatment
Animals were fed ad libitum a cereal-based, low-cholesterol (0.02% cholesterol, 4% total fat, w/w) diet (no. 7001; Harland Teklad, Madison, WI) upon weaning. Groups of mice were administered a subcutaneous injection of a 20% (w/v, in saline) solution of 2-hydroxypropyl-β-cyclodextrin (Sigma; product H107), (4000 mg/kg body weight), during the late dark phase (09:00 hours) at the scruff of the neck (12). Matching mice were also injected with saline alone to serve as controls.
Tissue cholesterol concentrations and synthesis rates
Tissue cholesterol concentrations and synthesis rates were determined as described (10), as were liver triacylglycerol contents (13). Esterified cholesterol levels in tissues were also measured as described (6). Tissue sterol contents are expressed as mg of cholesterol per whole organ (mg/organ). The cholesterol values found in every tissue, and in the remaining carcass, were summed to give whole animal cholesterol pools expressed as mg of cholesterol per kg body weight (mg/kg). The rates of sterol synthesis are expressed as the amount of [3H] water incorporated into sterols per hour per organ (nmol/hr/organ). The [3H] water incorporation rates in all organs were summed and used to calculate the whole animal synthesis rates. These values were then converted to the absolute mg of cholesterol synthesized each day per kg body weight (mg/day/kg).
Relative mRNA levels
Tissues from each animal were collected, snap-frozen in liquid nitrogen, and stored at -85° C. Quantitative real-time PCR was performed using an Applied Biosystems 7900HT sequence detection system and SYBR-green chemistry (14).
Liver function tests
Plasma was sent to a commercial laboratory for measurement of alanine aminotransferase (ALT), aspartate aminotransferase (AST) and alkaline phosphatase.
Tissue histology
Tissues sections were prepared, and histological examination and Purkinje cell number were assessed as described (9).
Data analysis
All data are presented as a mean ± 1 SEM. Differences between means in groups were tested for significance (P<0.05) using one-way ANOVA, followed by the Newman-Keuls multiple comparison test (Graph-Pad Software, Inc.; San Diego, CA). Significant differences between groups are designated with different symbols. Statistical differences among survival curves were determined utilizing the Wilcoxon-Gehard and Log-rank analyses.
RESULTS
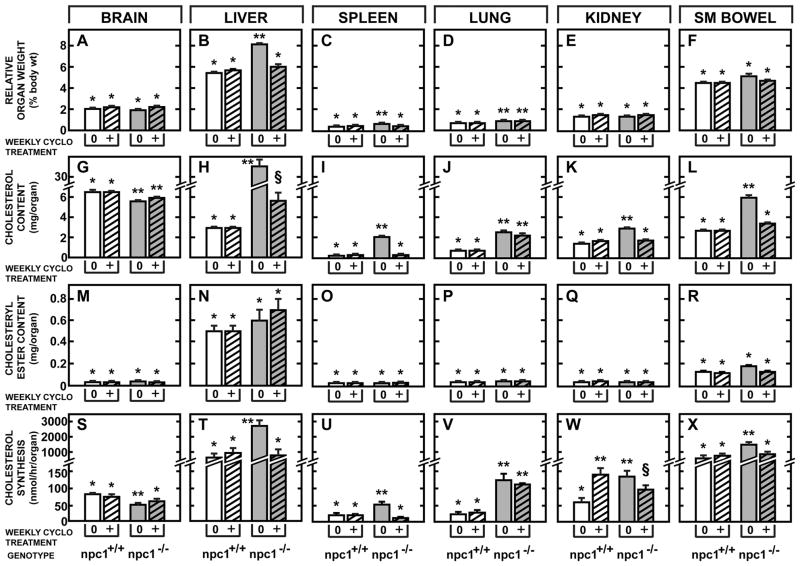
Groups of npc1+/+ and npc1−/− mice were given either saline or a dose of CYCLO (4000 mg/kg) subcutaneously at 7 days of age and every week thereafter until they were studied as young adults at 49 days of age. At this time, the npc1+/+ and npc1−/− mice treated with only saline weighed 21.8 ± 1.0 and 20.0 ± 0.8 g, respectively. As seen in Fig. 1 A–F, the npc1−/− mice receiving only saline had significant enlargement of the liver, spleen, and lung, but not of the other organs. Weekly treatment with CYCLO prevented this hepatosplenomegaly.
Figure 1.
Effect of weekly CYCLO administration on organ weights and various parameters of cholesterol metabolism in the npc1−/− mouse. Both npc1+/+ and npc1−/− mice were treated subcutaneously, weekly with either saline or CYCLO (4,000 mg/kg), and then studied at 49 days of age. The relative organ weights were measured in six major tissues (A–F). The content of total cholesterol present in each of these tissues was quantitated (G–L), as was the component of this sterol pool that was esterified (M–R). Both of these latter values are given as the mg of sterol present in the whole organs. Cholesterol synthesis rates in these same tissues are also shown (S–X), and are expressed as the nmol of [3H]water incorporated into sterols per hour per organ. Each column represents the mean ± 1 SEM for six animals. Significant differences (P<0.05) among groups are designated by different symbols in each panel.
Cholesterol content and synthesis
Except for the brain, the C content was markedly elevated in all organs of the saline treated npc1−/− mice (Fig. 1G–L). While C does accumulate in glia and neurons in the brain of the npc1−/− mice, this accumulation is offset by loss of C through partial demyelination (15, 16). Importantly, nearly all of this sequestered sterol was unesterified cholesterol since the content of CE in every organ was very low (Fig. 1M–R). The rate of sterol synthesis was also significantly increased in every organ, except the brain, as previously described (Fig. 1S–X) (9, 15).
However, following weekly CYCLO administration to the npc1−/− mice, these abnormalities in tissue cholesterol metabolism were all largely prevented. The content of C in nearly all organs of these treated animals was markedly reduced. There was no increase in the content of CE in any organ, and the rates of sterol synthesis were maintained at or near the levels found in the animals with normal NPC1 function, even in the brain. The notable exception to these findings was the lung where there was still a significant increase in C content (Fig. 1J) and synthesis (Fig. 1V).
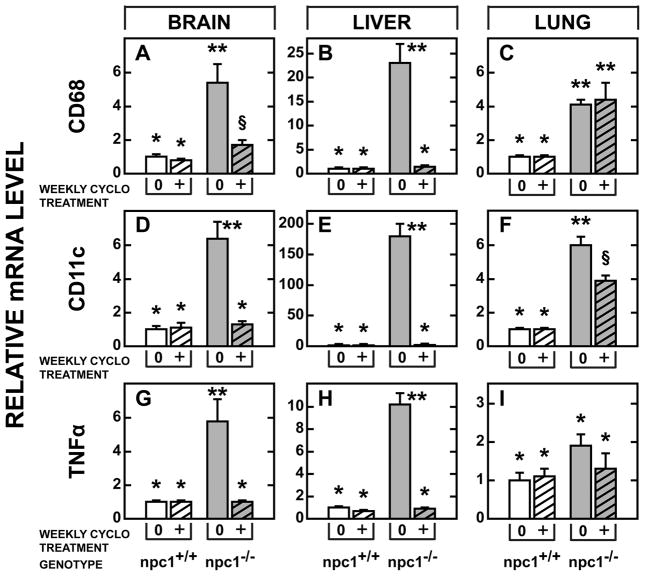
Relative mRNA levels for macrophage markers
Histologically, one of the hallmarks of NPC1 dysfunction and disease is a striking macrophage infiltration (3). This abnormality was reflected in the markedly elevated expression of mRNA for the macrophage and monocyte markers, CD68 and CD11c, and the cytokine, TNFα, found in the brain, liver and lung of the untreated npc1−/− mice (Fig. 2). With weekly CYCLO administration, however, these abnormalities were near completely prevented in the brain and liver. The lung, however, was resistant to this treatment (Fig. 2C,F).
Figure 2.
Effect of weekly CYCLO administration on the relative mRNA levels of various inflammatory proteins in brain, liver, and lung. Both npc1+/+ and npc1−/− mice were treated weekly with either saline or CYCLO, and then studied at 49 days of age. Each column represents the mean ±1 SEM for six mice. Significant differences (P<0.05) among groups are indicated by different symbols in each panel.
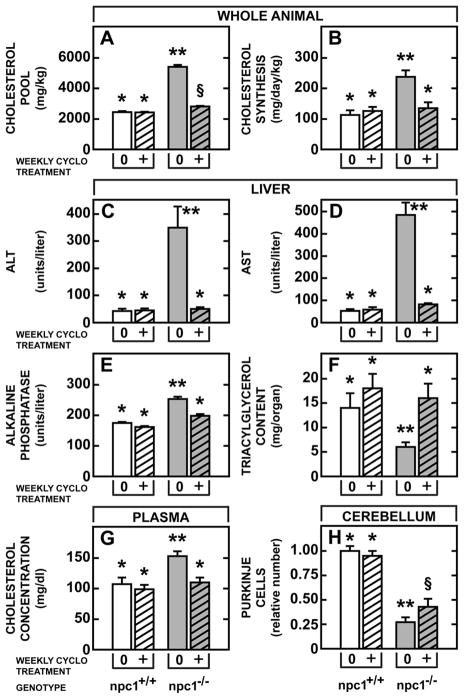
Whole animal pools and clinical effects
The whole mouse cholesterol pool in the npc1+/+ animals was about 2400 mg/kg, regardless of whether these mice were administered saline or CYCLO, while this pool reached 5,408 mg/kg in the untreated npc1−/− animals (Fig. 3A). Weekly CYCLO administration kept this pool at almost normal levels (2811 mg/kg). Similarly, the rate of whole animal cholesterol synthesis was nearly doubled (238 mg/day/kg) in the mutant mice, but this rate was maintained at near normal levels (137 mg/day/kg) with weekly CYCLO administration (Fig. 3B). The npc1−/− mice had markedly abnormal liver function tests (Fig. 3C, D, E), depressed levels of hepatic triacylglycerol (Fig. 3F), and elevated plasma cholesterol concentrations (Fig. 3G). All of these functional and lipid abnormalities were prevented by weekly CYCLO administration to the npc1−/− mice. Finally, in the 49 day old mutant animals, nearly 75% of the Purkinje cells in the cerebellum had disappeared, (Fig. 3H), but following CYCLO administration, nearly twice as many of these cells survived.
Figure 3.
Effect of weekly CYCLO administration on whole animal cholesterol metabolism, liver function tests, plasma total cholesterol concentrations and cerebellar neurodegeneration. Both npc1+/+ and npc1−/− mice were treated weekly with either saline or CYCLO, and then studied at 49 days of age. Whole animal cholesterol pools are expressed as mg of cholesterol per kg body weight (A). Whole animal synthesis rates (B) are expressed as mg of cholesterol synthesized per day per kg body weight. The liver function tests ALT (C), AST (D), and alkaline phosphatase (E) were quantitated, as were the levels of hepatic triacylglycerol (F). The plasma total cholesterol concentrations were also measured (G). The numbers of Purkinje cells in the cerebellum were counted, and are expressed relative to the number found in the npc1+/+ mice treated with saline (H). Each column represents the mean ± 1 SEM for six animals in each group. Significant differences (P<0.05) among groups are indicated by different symbols in each panel.
Animal Survival
In order to explore the overall effect of these changes on longevity, groups of npc1−/− mice were administered either saline alone, CYCLO one time at 7 days of age, or CYCLO at 7 days of age followed by serial, weekly injections. As seen in Fig. 4, the single dose of CYCLO at 7 days of age significantly prolonged life by about 30 days, while continuous weekly administration of this compound extended lifespan by nearly 80 days. Of note, this later group of mice appeared very mobile and vigorous, even beyond 120 days of age, and the npc1−/−females could be readily mated with npc1+/+ males, the npc1−/− males with npc1+/+ females, giving rise to heterozygous offspring.
Figure 4.
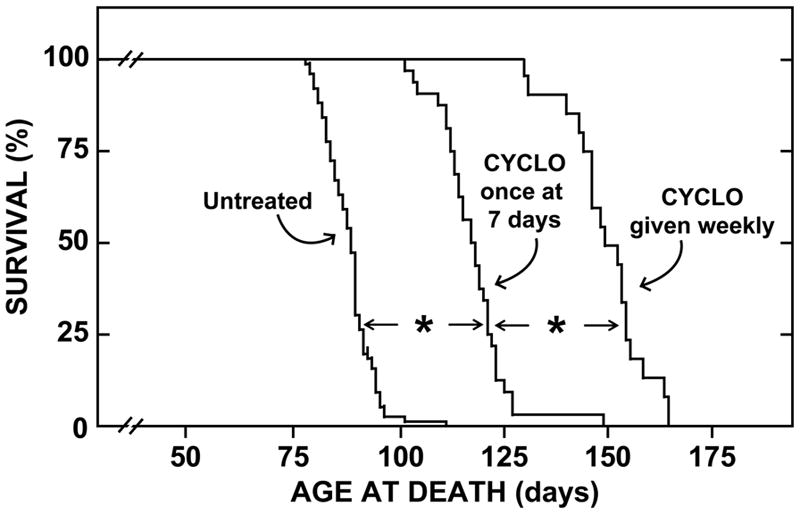
Age at death of npc1−/− mice treated with CYCLO. This figure shows three groups of npc1−/− animals that were either untreated, administered a single dose of CYCLO (4,000 mg/kg) once at 7 days of age, or treated weekly with this same dose of CYCLO. There were 76 untreated mice, 32 treated once, and 20 treated weekly. Both the single and weekly doses of CYCLO significantly (*) prolonged the life of these npc1−/−animals (P<0.001).
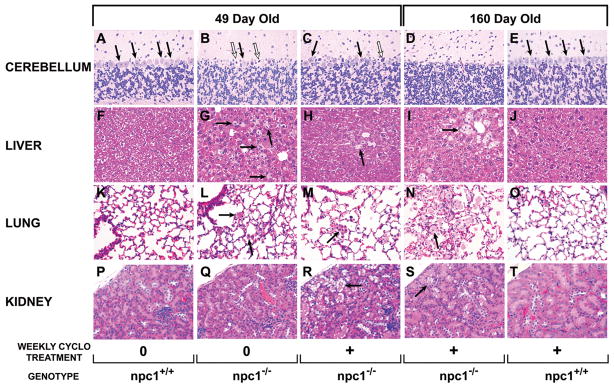
Histology of the major target organs
The histology of several important organs in the various experimental groups is shown in Fig. 5. The first three columns show organs taken from 49 day old npc1+/+ mice given only saline and from npc1−/− animals administered either saline or CYCLO every week. The last two columns of figures come from 160 day old npc1−/− and npc1+/+ mice treated weekly with CYCLO. At 49 days of age, only about 25% of Purkinje cells remained in the untreated npc1−/− mice, and many of these appeared to be pyknotic and dying (Fig. 5B). CYCLO treatment slowed this rate of Purkinje cell loss, still cell numbers were significantly reduced (Fig. 5C). Importantly, in animals that survived to 160 days of age, no Purkinje cells could be identified (Fig. 5D). In untreated 49 day old npc1−/− mice there were numerous, lipid-laden macrophages scattered throughout the liver (Fig. 5G) while this infiltrate was almost completely absent in the animals treated with CYCLO (Fig. 5H). Even after 160 days of treatment, the architecture of the liver was essentially normal in the npc1−/− mice, except for occasional clusters of macrophages in a pericentral distribution (Fig. 5I). The histological appearance of the liver was entirely normal in npc1+/+ animals treated with weekly CYCLO (Fig. 5J).
Figure 5.
Representative histological sections of four tissues in npc1−/− mice treated with CYCLO. Both npc1+/+ and npc1−/− mice were administered saline, while other groups of animals were given CYCLO (4,000 mg/kg) weekly. Histological preparations were then made of the cerebellum, liver, lung, and kidney at either 49 or 160 days of age. The solid arrows point to Purkinje cells in the cerebellum (A–E), to lipid-laden macrophages in the liver and lung (F–O), or to vacuolization in the kidney epithelium (P–T). The open arrows in panels B and C point to pyknotic Purkinje cells. The bar equals 50 μm (P), and all panels are at the same magnification (400X).
The lung behaved differently, however. In the 49 day old, untreated npc1−/− mice there were small clusters of macrophages scattered throughout the alveoli of the lung (Fig. 5L), and similar clusters were still found after treatment with CYCLO (Fig. 5M). This progressive infiltration continued, even with weekly CYCLO treatment, until at 160 days of age there were collections of lipid-laden macrophages filling many of the alveolar spaces (Fig. 5N). Of note, the lungs appeared to be entirely normal in the npc1+/+ mice treated with weekly CYCLO (Fig. 5O). Finally, kidney architecture was essentially normal in the untreated npc1−/− mice (Fig. 5Q), but vacuolization was noted in some tubular epithelium following administration of CYCLO (Fig. 5R), as has been previously reported (17). Of note, this vacuolization apparently did not progress, even after 160 days of weekly CYCLO treatment (Fig. 5S ,T).
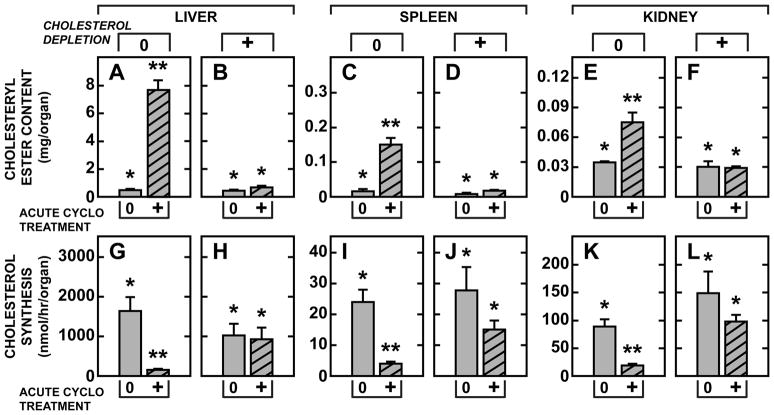
Flow of C from the late E/L complex to the cytosol
Finally, there is a remarkable difference in CE formation and suppression of cholesterol synthesis in these studies using repetitive CYCLO administration, compared to previously published investigations utilizing a single dose of this cholesterol-binding agent. These differences go directly to the mechanism of action of CYCLO within the cells of the body. While 49 day old npc1−/− mice not previously treated with CYCLO had markedly expanded pools of sequestered C in nearly every organ (Fig. 3A), these pools were largely maintained at normal levels following weekly administration of this compound. As a result of these differences, acute reversal of the transport defect in the untreated npc1−/− mice led to flux of massive amounts of C into the cytosolic compartment, while there was virtually no increase in this flux in animals previously treated with weekly CYCLO administration. These differences are illustrated by the data shown in Fig. 6. In 48 day old, npc1−/− mice that had received no prior CYCLO treatment, the pools of tissue C were markedly elevated in liver (9-fold), spleen (7-fold), and kidney (2-fold), and rates of synthesis were increased. Twenty-four hours after administration of a single dose of CYCLO, CE levels had markedly increased in the liver (15-fold), spleen (9-fold) and kidney (2-fold) (Fig. 6A, C, E) while synthesis was markedly suppressed (Fig. 6G, I, K). Thus, these indirect measures of C flow into the cytosolic compartment demonstrated a metabolic effect proportional to the size of the pool of C sequestered in each organ. In contrast, if this sequestration was prevented by prior, weekly administration of CYCLO, and the tissue C pools were relatively normal in the liver (1.9-fold), spleen (1.1-fold) and kidney (1.3-fold), twenty-four hours after CYCLO administration there was little or no increase in the level of CE in these organs (Fig. 6B, D, F), nor was there significant suppression of synthesis (Fig. 6H, J, L). Thus, repetitive CYCLO administration had markedly reduced the pool of C in the late E/L compartment of cells, and so markedly blunted the metabolic response of these cells to acute CYCLO administration. CYCLO had no effect on tissues of the npc1+/+ or npc1−/− mice treated weekly with this compound since there were no pools of sequestered, excess C in the tissues of these animals.
Figure 6.
Flow of cholesterol from the late E/L compartment into the cytosolic compartment in npc1−/− mice that were either untreated or were depleted of sequestered sterol pools. Two groups of npc1−/− mice were used in these studies. One group received no prior treatment until 48 days of age at which time they were given a single dose of either saline (0) or CYCLO (4,000 mg/kg) (+), and then studied 24 hours later (A, C, E, G, I, K). The second group received weekly CYCLO administration beginning at 7 days of age to deplete tissue cholesterol pools. At 48 days of age these animals were then given either saline (0) or CYCLO (+), and studied 24 hours later (B, D, F, H, J, L). The level of cholesteryl ester found in the liver, spleen, and kidney was quantitated (A–F) as was the rate of cholesterol synthesis in these organs (G–L). Each column represents the mean ± 1 SEM for 4–8 animals in each group. Significant differences (P<0.05) among groups are indicated by different symbols in each panel.
DISCUSSION
These studies demonstrate that weekly CYCLO administration nearly prevents the abnormal cholesterol sequestration and tissue metabolic dysfunction typical of NPC1 disease (Fig. 1, 3). As a result, plasma cholesterol concentrations, hepatic triacylglycerol levels, liver function tests, and measures of tissue macrophage infiltration and inflammation are all maintained at normal levels. In addition, the magnitude of neurodegeneration is slowed, animal fertility is restored, and lifespan of the npc1−/− animals is essentially doubled. These findings support the concept that it is the disordered C metabolism in organs of the NPC1 mouse, and child, that leads, directly or indirectly, to organ dysfunction and disease.
At the dose utilized in these studies, plasma concentrations of CYCLO reach 2–5 mg/ml within 1 to 3 hours after administration. The compound is then rapidly excreted in the urine, and virtually no C is carried out of the animals with the excreted CYCLO (10). Rather, in cells throughout the body, within hours of administration there is net flow of the sequestered pool of C out of the late E/L compartment into the cytosol where it is temporarily stored as CE (9, 10). Over the following few days, this pool of CE in the peripheral organs is slowly hydrolyzed, and the released C is moved across the plasma membrane onto HDL and transferred to the liver. This process of centripetal sterol flow is unaffected by the mutation in NPC1 (18). The pool of C generated from the hydrolysis of CE in the liver, along with that taken up from HDL, is then metabolized to bile acid and excreted from the body as fecal acidic sterols (10). In this manner, the weekly administration of CYCLO permits excretion of an amount of C essentially equal to that ordinarily sequestered in the individual organs of the npc1−/− mouse and, so, maintains the whole animal cholesterol pool at near normal levels (Fig. 3A).
However, it is clear from these studies that not all organs respond equally well to the subcutaneous administration of CYCLO. In the liver, for example, a single dose of CYCLO given to young or mature npc1−/− mice leads to the acute flow of C into the cytosolic compartment for metabolism and/or excretion (10). As a result of this responsiveness to a single dose, the weekly administration of CYCLO maintains essentially normal hepatic C pools and synthesis rates (Fig. 1), prevents infiltration of lipid-laden macrophages (Fig. 5), maintains molecular markers of inflammation at normal levels (Fig. 2), and prevents abnormalities in liver function tests and liver disease (Fig. 3). Thus, in the liver, and many other organs, weekly CYCLO administration nearly completely overcomes the transport defect seen in the npc1−/−animals.
The response in the brain is less robust, however. Subcutaneous administration of a single dose of CYCLO to either 7 day old or mature npc1−/− animals also results in the flow of C into the cytosolic CE pool and suppression of sterol synthesis (10). However, the magnitude of this response is quantitatively less than that seen in liver. Thus, with the weekly administration of CYCLO utilized in these studies, there is only partial restoration of C metabolism in the brain, although measures of glial cell activation are maintained at near normal levels (Fig. 2). Associated with these changes, the rate of Purkinje cell death is slowed (Fig. 3, 5), and the animals survive for a much longer time without gross neurological abnormalities (Fig. 4). This partial response of the brain to systemic CYCLO administration is the result of lower permeability of the capillaries of the brain to this compound.
The lung is even more resistant to CYCLO administration than brain. As in the other tissues, the severity of pulmonary disease is proportional to the amount of C sequestered in the tissue. For example, when uptake of lipoprotein-C is enhanced and the amount of C sequestered in the lung is increased, there is significantly greater infiltration by lipid-laden macrophages and pneumonitis (3). However, the acute administration of a single dose of CYCLO to npc1−/− mice has no effect on these pools of C or on sterol synthesis at either 7 or 49 days of age (10). Not surprisingly, therefore, the weekly administration of CYCLO did not normalize sterol metabolism in the lung and did not prevent the development of progressive “lipoid” pneumonitis. Relative organ weight, cholesterol content, and sterol synthesis (Fig. 1D, J, V) in the lung all remain uncorrected. There is progressive infiltration of the lung with lipid-laden macrophages (Fig. 5) and persistent, high relative mRNA levels for CD68 and CD11c (Fig. 2) despite treatment. As a result, by 160 days of age these mutant mice develop a “lipoid” pneumonitis (Fig. 5N) that appears nearly identical to that seen in infants with NPC disease who die of progressive pulmonary failure (19).
In summary, these studies demonstrate that weekly CYCLO administration to the npc1−/−mouse brings about the excretion of nearly all of the C that is sequestered in the various tissues during the preceding week, and maintains the whole animal sterol pool at essentially normal levels. This therapeutic effect prevents the liver dysfunction seen in these animals and ameliorates the rate of neurodegeneration, but does not alter the progressive development of lung disease. Future studies must explore alternative means for delivering CYCLO directly into the CNS and lung. Importantly, however, these studies also indicate that CYCLO administration is essentially free of side effects. The compound is rapidly cleared from the plasma into the urine without, apparently, causing any untoward effects. Even after 160 days of administration there is no evidence of tissue damage so that liver and lung histology remain normal in the npc1+/+ animal. The only histological abnormality seen is mild vacuolization in some renal epithelial cells 49 days after beginning therapy, but even this lesion apparently does not progress.
Acknowledgments
This work was supported by US Public Health Service Research Grant R01-HL009610 [J.M.D, S.D.T.] and by grants from the Moss Heart Fund [J.M.D.] and the Ara Parseghian Medical Research Foundation [J.J.R.]. C.M.R.and B.L. also received post-doctoral support from the Ara Parseghian Medical Research Foundation.
The authors express their appreciation to Carolyn Crumpton, Mario Saucedo, Jennifer Burg, and S. Sean Campbell for their excellent technical assistance, and to Annemarie Kelsey for expert preparation of the manuscript.
Abbreviations
- C
unesterified cholesterol
- CE
cholesteryl esters
- CYCLO
2-hydroxypropyl-β-cyclodextrin
- E/L
endosomal/lysosomal
- NPC1
Niemann-Pick type C1
Footnotes
Publisher's Disclaimer: Pediatric Research Articles Ahead of Print contains articles in unedited manuscript form that have been peer-reviewed and accepted for publication. As a service to our readers, we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting and review of the resulting proof before it is published in its final definitive form. Please note that during the production process errors may be discovered, which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Loftus SK, Morris JA, Carstea ED, Gu JZ, Cummings C, Brown A, Ellison J, Ohno K, Rosenfeld MA, Tagle DA, Pentchev PG, Pavan WJ. Murine model of Niemann-Pick C disease: mutation in a cholesterol homeostasis gene. Science. 1997;277:232–235. doi: 10.1126/science.277.5323.232. [DOI] [PubMed] [Google Scholar]
- 2.Xie C, Turley SD, Pentchev PG, Dietschy JM. Cholesterol balance and metabolism in mice with loss of function of Niemann-Pick C protein. Am J Physiol. 1999;276:E336–E344. doi: 10.1152/ajpendo.1999.276.2.E336. [DOI] [PubMed] [Google Scholar]
- 3.Liu B, Xie C, Richardson JA, Turley SD, Dietschy JM. Receptor-mediated and bulk-phase endocytosis cause macrophage and cholesterol accumulation in Niemann-Pick C disease. J Lipid Res. 2007;48:1710–1723. doi: 10.1194/jlr.M700125-JLR200. [DOI] [PubMed] [Google Scholar]
- 4.Li H, Repa JJ, Valasek MA, Beltroy EP, Turley SD, German DC, Dietschy JM. Molecular, anatomical, and biochemical events associated with neurodegeneration in mice with Niemann-Pick type C disease. J Neuropathol Exp Neurol. 2005;64:323–333. doi: 10.1093/jnen/64.4.323. [DOI] [PubMed] [Google Scholar]
- 5.Gondré-Lewis MC, McGlynn R, Walkley SU. Cholesterol accumulation in NPC1-deficient neurons is ganglioside dependent. Curr Biol. 2003;13:1324–1329. doi: 10.1016/s0960-9822(03)00531-1. [DOI] [PubMed] [Google Scholar]
- 6.Beltroy EP, Liu B, Dietschy JM, Turley SD. Lysosomal unesterified cholesterol content correlates with liver cell death in murine Niemann-Pick type C disease. J Lipid Res. 2007;48:869–881. doi: 10.1194/jlr.M600488-JLR200. [DOI] [PubMed] [Google Scholar]
- 7.Repa JJ, Li H, Frank-Cannon TC, Valasek MA, Turley SD, Tansey MG, Dietschy JM. Liver X receptor activation enhances cholesterol loss from the brain, decreases neuroinflammation, and increases survival of the NPC1 mouse. J Neurosci. 2007;27:14470–14480. doi: 10.1523/JNEUROSCI.4823-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Posse De Chaves EI, Vance DE, Campenot RB, Kiss RS, Vance JE. Uptake of lipoproteins for axonal growth of sympathetic neurons. J Biol Chem. 2000;275:19883–19890. doi: 10.1074/jbc.275.26.19883. [DOI] [PubMed] [Google Scholar]
- 9.Liu B, Turley SD, Burns DK, Miller AM, Repa JJ, Dietschy JM. Reversal of defective lysosomal transport in NPC disease ameliorates liver dysfunction and neurodegeneration in the npc1−/− mouse. Proc Natl Acad Sci USA. 2009;106:2377–2382. doi: 10.1073/pnas.0810895106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu B, Ramirez CM, Miller AM, Repa JJ, Turley SD, Dietschy JM. Cyclodextrin overcomes the transport defect in nearly every organ of the newborn or mature NPC1 mouse leading to excretion of the sequestered cholesterol as bile acid. J Lipid Res. 2010;51:933–944. doi: 10.1194/jlr.M000257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davidson CD, Ali NF, Micsenyi MC, Stephney G, Renault S, Dobrenis K, Ory DS, Vanier MT, Walkley SU. Chronic cyclodextrin treatment of murine Niemann-Pick C disease ameliorates neuronal cholesterol and glycosphingolipid storage and disease progression. PLoS ONE. 2009;4:e6951. doi: 10.1371/journal.pone.0006951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu B, Li H, Repa JJ, Turley SD, Dietschy JM. Genetic variations and treatments that affect the lifespan of the NPC1 mouse. J Lipid Res. 2008;49:663–669. doi: 10.1194/jlr.M700525-JLR200. [DOI] [PubMed] [Google Scholar]
- 13.Repa JJ, Turley SD, Quan G, Dietschy JM. Delineation of molecular changes in intrahepatic cholesterol metabolism resulting from diminished cholesterol absorption. J Lipid Res. 2005;46:779–789. doi: 10.1194/jlr.M400475-JLR200. [DOI] [PubMed] [Google Scholar]
- 14.Valasek MA, Repa JJ. The power of real-time PCR. Adv Physiol Educ. 2005;29:151–159. doi: 10.1152/advan.00019.2005. [DOI] [PubMed] [Google Scholar]
- 15.Xie C, Burns DK, Turley SD, Dietschy JM. Cholesterol is sequestered in the brains of mice with Niemann-Pick type C disease but turnover is increased. J Neuropathol Exp Neurol. 2000;59:1106–1117. doi: 10.1093/jnen/59.12.1106. [DOI] [PubMed] [Google Scholar]
- 16.Zervas M, Dobrenis K, Walkley SU. Neurons in Niemann-Pick disease type C accumulate gangliosides as well as unesterified cholesterol and undergo dendritic and axonal alterations. J Neuropathol Exp Neurol. 2001;60:49–64. doi: 10.1093/jnen/60.1.49. [DOI] [PubMed] [Google Scholar]
- 17.Gould S, Scott RC. 2-Hydroxypropyl-beta-cyclodextrin (HP-beta-CD): a toxicology review. Food Chem Toxicol. 2005;43:1451–1459. doi: 10.1016/j.fct.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 18.Xie C, Turley SD, Dietschy JM. Centripetal cholesterol flow from the extrahepatic organs through the liver is normal in mice with mutated Niemann-Pick type C protein (NPC1) J Lipid Res. 2000;41:1278–1289. [PubMed] [Google Scholar]
- 19.Schofer O, Mischo B, Puschel W, Harzer K, Vanier MT. Early-lethal pulmonary form of Niemann-Pick type C disease belonging to a second, rare genetic complementation group. Eur J Pediatr. 1998;157:45–49. doi: 10.1007/s004310050764. [DOI] [PubMed] [Google Scholar]