Abstract
Study Objectives:
Insomnia is a chronic condition with significant burden on health care and productivity costs. Despite this recognized burden, very few studies have examined associations between insomnia severity and healthcare and productivity costs.
Design:
A retrospective study linking health claims data with a telephone survey of members of a health plan in the Midwestern region of the United States.
Participants:
The total healthcare costs study sample consisted of 2086 health plan members who completed the survey and who had complete health claims data. The productivity costs sample consisted of 1329 health plan members who worked for pay—a subset of the total healthcare costs sample.
Measurements:
Subjects' age, gender, demographic variables, comorbidities, and total health care costs were ascertained using health claims. Insomnia severity and lost productivity related variables were assessed using telephone interview.
Results:
Compared with the no insomnia group, mean total healthcare costs were 75% larger in the group with moderate and severe insomnia ($1323 vs. $757, P < 0.05). Compared with the no insomnia group, mean lost productivity costs were 72% larger in the moderate and severe insomnia group ($1739 vs. $1013, P < 0.001). Chronic medical comorbidities and psychiatric comorbidities were positively associated with health care cost. In contrast, psychiatric comorbidities were associated with lost productivity; while, medical comorbidities were not associated with lost productivity.
Conclusions:
Health care and lost productivity costs were consistently found to be greater in moderate and severe insomniacs compared with non-insomniacs. Factors associated with lost productivity and health care costs may be fundamentally different and may require different kinds of interventions. Future studies should focus on better understanding mechanisms linking insomnia to healthcare and productivity costs and to understanding whether developing targeted interventions will reduce these costs.
Citation:
Sarsour K; Kalsekar A; Swindle R; Foley K; Walsh JK. The association between insomnia severity and healthcare and productivity costs in a health plan sample. SLEEP 2011;34(4):443-450.
Keywords: Insomnia severity, insomnia costs, administrative health claims-linked survey, productivity costs, healthcare costs
INTRODUCTION
Epidemiologic studies consistently estimate that about one third to one half of the general population report occasional problems with sleep, and 6% to 10% report sleep problems and associated daytime consequences consistent with diagnostic criteria for chronic insomnia.1,2 The growing recognition of the widespread prevalence of insomnia and its symptoms has led to an increase in the published literature on insomnia-related healthcare costs and productivity burden. Several studies have shown that patients with insomnia tend to have higher utilization of health care resources and increased health care costs relative to patients without insomnia.3–13
Daytime consequences of insomnia impact indirect costs through absenteeism (defined as employees' absence from the workplace) or presenteeism (defined as being present at the workplace despite being sick or impaired, directly leading to compromised productivity).14–22 For example, a large study conducted in Canada found that having insomnia was associated with 27.6 days per year of insomnia-related lost productivity versus 2.6 days per year for good sleepers.15 In a related analysis, 40.6% of those with insomnia reported a reduction in their productivity versus 12.3% of those without insomnia.16
While existing evidence consistently demonstrates that insomnia is associated with significantly higher healthcare and lost productivity costs, studies in this area have had a number of limitations. First, studies that examined insomnia and total medical costs have relied on administrative health claims definitions for insomnia and as a result did not ascertain the presence of insomnia using validated tools. Second, most studies in this area have studied the presence or absence of insomnia in a binary fashion without considering the relevance of insomnia severity to health care and productivity costs. Third, while several studies provide evidence of the directional impact of insomnia on lost productivity, the association is often confounded by concomitant physical and mental illnesses.
This study linked survey data with administrative health claims data to better understand the association between insomnia severity and total healthcare and lost productivity costs due to presenteeism and absenteeism in insomnia patients compared to patients without insomnia.
METHODS
A single health plan in the Midwestern USA which contributes to MarketScan with coverage of approximately 150,000 lives was used to select potential study participants. In order to ensure adequate respondents with insomnia and a wide range of insomnia severity levels, 5000 subjects with an insomnia diagnosis health claim or prescription claim in 2004/5 and 6,000 randomly selected individuals who had no insomnia related health care claims and who were representative of the health plan population were invited to participate in a telephone survey on sleep problems and associated impact.
Inclusion diagnosis codes for insomnia were 307.41 and 307.42 (transient or persistent disorder of initiating or maintaining sleep); 307.45 (phase-shift disruption of 24-h sleep cycle); 307.49 (subjective insomnia complaint); 780.52 (other insomnia NOS); and 780.55 (disruptions of 24-h sleep wake cycle). Inclusion drug codes were for benzodiazepine hypnotics (estazolam, flurazepam, quazepam, temazepam, and triazolam), non-benzodiazepine hypnotics (eszopiclone, zaleplon, and zolpidem), and sedating antidepressants (amitriptyline [< 50 mg], doxepin [< 50 mg], nefazodone [< 100 mg], and trazadone, [< 150 mg]). The latter were indicators of insomnia only when used in low doses.
Participants were required to be between the ages of 18 and 80 years, and to have continuous health plan enrollment for ≥ 24 months. Following the completion of the surveys, a deidentified data file with the survey responses and claims-based variables was created. Evaluation of non-responders could not be performed due to IRB regulations.
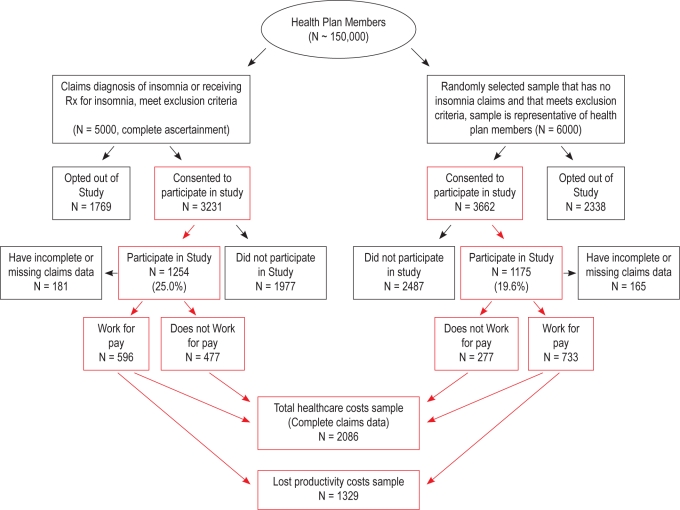
After allowing plan members to opt out of the study, a total of 2,432 health plan members (22.1%) participated in the telephone survey, including 1,257 of the insomnia-related claim group and 1,175 of the no-insomnia-related claim group. Of these, only 2,086 subjects had complete administrative health records and formed the sample for healthcare cost analyses. After excluding those who did not work for pay, 1,329 subjects remained and formed the study sample for the ascertainment of lost productivity costs. A study sample flow diagram is presented in Figure 1 and is described elsewhere.23 Study protocol including the patient identification process and informed consent was reviewed and approved by the health plan's IRB.
Figure 1.
Study sample flow diagram
Measures
Healthcare claims based measures
Subjects' age, gender, demographic variables, comorbidities, and total health care costs were ascertained directly from the healthcare claims records.
The Chronic Disease Score (CDS) was used as a measure of chronic medical comorbidities. The CDS was calculated based on the number of therapeutic drug classes an individual takes in each of 17 disease/condition categories. CDS has high year-to-year stability (a correlation of 0.74 over time), has been shown to be related to physician ratings of physical disease severity, and to predict hospitalization and mortality.24,25
The psychiatric index provides a claims-based measure for psychiatric disease burden in patients who are active in the out-patient as well as the inpatient health system. It consists of 12 psychiatric diagnostic groupings (PDGs) for alcohol, drug, and mental disorders consistent with the DSM-III-R classification, which coincides with major diagnostic groups in the inpatient-focused diagnosis-related groups (DRG) system. Within each PDG there are 4-9 groups of Psychiatric Patient Classes, which provide additional detail for mental disorders. Although each of the12 groupings has multiple diagnoses within, a patient receives just one point for each of the 12 groups in which he or she has a diagnosis. Thus, the maximum possible score is 12, and the minimum is 0. Prior research has shown that the additional detail for mental disorders within each PDG results in an 11% improvement in variance over the original DRGs.26
Overall health expenditures were assessed in the 12 months prior to the date of survey and were aggregated as a total. For services in which the plan was a secondary payer, the amounts paid by other insurers were added. All actual and proxy payments were inflation adjusted to 2005 dollars using the Consumer Price Index.
Survey Based Measures
Survey based measures included measures of self-reported insomnia treatment, insomnia severity, and productivity over the past 4 weeks.
Insomnia severity
The Insomnia Severity Index (ISI) has been validated against both polysomnographic and prospective sleep diary measures, and demonstrates convergence with clinical interview criteria.27 The ISI score was obtained by summing the scores across seven of the survey questions that assessed the severity of individual symptoms, the level of interference of symptoms in the patient's life, and patient satisfaction and concern with sleep patterns. The maximum possible score on the ISI is 28. Previous research provides the following 4 categories of insomnia severity: scores of 0 through 7 indicate no clinically signifi-cant insomnia, 8 through 14 indicate subthreshold insomnia, 15 through 21 indicate moderate clinical insomnia, and 22 through 28 indicate severe clinical insomnia.27
Productivity-related variables
The survey included questions on occupation, wages, absenteeism, and presenteeism. The World Health Organization Health and Work Performance Questionnaire (HPQ), a validated instrument, was used in the evaluation of absenteeism and presenteeism.28 The concept of absenteeism is measured based on the number of hours missed from work. The concept of presenteeism is measured in terms of lost productivity, calculated by gauging self-reported actual performance in relation to an individual's possible performance on the job. Participants rated themselves on a scale of 0-10, with 0 indicating worst job performance possible and 10 the top performance possible. This self-reported score was subtracted from the maximum possible score of 10, and the resulting number was used to calculate lost productivity: lost productivity = (maximum score of 10 - actual score) × 10. Lost productive hours were calculated as lost productivity × hours worked in past 4 weeks. Cost of lost productive hours from presenteeism was calculated as lost productive hours × hourly wage. Cost of lost productive hours from absenteeism was calculated as hours absent × hourly wage. For those individuals who did not report a salary (20.1% of the work for pay sample), hourly rates per the 2004 Current Population Survey (inflated to 2005) were applied to the job categories as collected by the questions from the HPQ. Total lost productivity cost variable used in this study combined both absenteeism and presenteeism.
Statistical Analysis
The dependent variables of this study are lost productivity costs and total healthcare costs. Descriptive frequencies were calculated for study variables. Because the distributions of the productivity and healthcare cost data were skewed due to the inclusion of individuals with zero costs, generalized linear models (GLM) were chosen for performing the analyses based on accepted econometric methods.29 Standard multicollinearity and outlier analysis were also conducted. Because very few subjects fell in the severe insomnia category (see Table 1), we combined the severe and moderate insomnia groups together. Exponentiated coefficients on the insomnia variables show the percentage effect of insomnia on healthcare costs while controlling for all other covariates. Predicted costs were calculated by applying the model coefficients to each individual's values on each of the variables included in the model. Mean predicted costs were generated for by level of insomnia severity. The full multivariate model included age, gender, insomnia treatment type, CDS, and psychiatric index scores.
Table 1.
Descriptive characteristics of study sample
| Work for pay (N = 1329) | Doesn't work for pay (N = 754) | Total sample (N = 2086) | |
|---|---|---|---|
| Variable | n (%) or mean (SD) | ||
| Female | 912 (68.6%) | 539 (71.5%) | 1452 (69.6%) |
| Age (years) | 46.3 (11.4) | 61.4 (14.0) | 51.7 (14.3) |
| Age ≥ 65 | 72 (5.4%) | 366 (48.5%) | 485 (23.3%) |
| ISI category | |||
| No insomnia | 543 (40.9%) | 311 (33.2%) | 869 (41.7%) |
| Subthreshold insomnia | 477 (35.9%) | 231 (24.6%) | 709 (34.0%) |
| Moderate insomnia | 257 (19.3%) | 170 (18.1%) | 428 (20.5%) |
| Severe insomnia | 52 (3.9%) | 42 (4.5%) | 80 (3.84%) |
| Claims based insomnia diagnosis* | 80 (6.0%) | 29 (2.8%) | 108 (5.2%) |
| Insomnia related prescription claim* | 352 (26.5%) | 265 (35.1%) | 618 (29.6%) |
| Self-reported treatments** | |||
| OTC treatment | 83 (6.3%) | 60 (8.0%) | 143 (6.9%) |
| Prescription treatments | 346 (26.0%) | 274 (36.3%) | 620 (29.7%) |
| No treatment | 821 (61.9%) | 389 (51.6%) | 1213 (58.1%) |
| > 0 absenteeism | 157 (11.8%) | N/A | N/A |
| > 0 presenteeism | 1070 (80.5%) | N/A | N/A |
| Occupation | |||
| Executive (administrator or senior manager) | 53 (3.5%) | N/A | N/A |
| Professional (engineer, accountant, analyst) | 517 (34.6%) | N/A | N/A |
| Technical support (programmer, lab assistant, legal assistant) | 228 (15.3%) | N/A | N/A |
| Clerical/administrative support | 433 (29.0%) | N/A | N/A |
| Precision production/craft worker | 86 (5.8%) | N/A | N/A |
| Operator or laborer | 122 (8.2%) | N/A | N/A |
| Work hours | 42.8 (24.9) | N/A | N/A |
| Income | $41495 (51758) | N/A | N/A |
| Self-rated work performance (0-10) | 8.4 (1.3) | N/A | N/A |
| Weeknights sleep hours | 6.4 (2.1) | 6.5 (2.6) | 6.5 (2.0) |
| Self-rated Sleep Quality (0-10) | 6.0 (2.3) | 6.0 (2.6) | 6.0 (2.4) |
| Psychiatric index score | 0.16 (0.49) | 0.22 (0.50) | 0.18 (0.54) |
| Chronic disease index score | 1.73 (2.48) | 2.9 (2.53) | 2.15 (2.82) |
In year preceding the survey.
In 4 weeks preceding the survey.
RESULTS
Healthcare Cost Sample Descriptive Characteristics
The health care cost sample (n = 2,086) had a mean age (SD) of 51.7 (14.3) years and nearly 70% of respondents were female. ISI scores indicated that 41.7%, 34.0%, 20.5%, and 3.8% were categorized as no insomnia, subthreshold insomnia, moderate insomnia, and severe insomnia, respectively. Because of the small number in the severe category, moderate and severe were combined for remaining analyses. Of the sample, 5.2% had an insomnia diagnosis claim and 29.6% had an insomnia-related prescription claim. Interestingly 47.2% of the moderate/severe insomnia group had no insomnia related health care claims (diagnosis or prescription) even though 90.8% reported having their sleep problems for ≥ 1 year. Mean (SD) CDS and psych index scores were 2.15 (2.82) and 0.18 (0.54), respectively. Within the study sample, there were no significant differences between those who worked for pay and those who did not in terms of gender, reported mean sleep hours, or sleep quality. Only mean age (SD) was significantly different between those who worked for pay and those who did not (46.3 [11.3] versus 61.4 [14.0]]. Of those who had an insomnia claim, a greater percentage also had a psychiatric diagnosis (5.6%, 20.1% and 27.9% in the ISI no insomnia, subthreshold insomnia and moderate/severe groups, respectively). Of those who had no insomnia claim and no insomnia per the ISI, 16.1% had a psychiatric diagnosis, while 10.4% and 11.7% of those who had no insomnia-related claim fell in the ISI categories of subthreshold and moderate/severe, respectively.
Healthcare Cost Findings
Adjusted (predicted) and unadjusted total health care costs by insomnia category are presented in Table 2. Mean (SD) observed (unadjusted) medical costs for the no insomnia group were $643 ($1587), while the mean costs for subthreshold and moderate/severe insomnia groups were $912 ($2035) and $1254 ($3676) respectively.
Table 2.
Annual observed and predicted costs by insomnia group
| Observed (unadjusted) costs Mean (SD) |
Predicted (adjusted) Costs Mean (SD) |
|||
|---|---|---|---|---|
| Total healthcare costs | Lost productivity costs | Total healthcare costs | Lost productivity costs | |
| No insomnia | $643 (1587) | $1035 (5230) | $757 (510) | $1,013 (501) |
| Subthreshold insomnia | $912 (2035) | $1323 (6623) | $907 (729) | $1,352 (691) |
| Moderate/severe insomnia | $1254 (3676) | $1554 (5481) | $1323 (924) | $1,739 (950) |
Adjusted costs models adjusts for age, gender, medical and psychiatric comorbidities and insomnia treatments
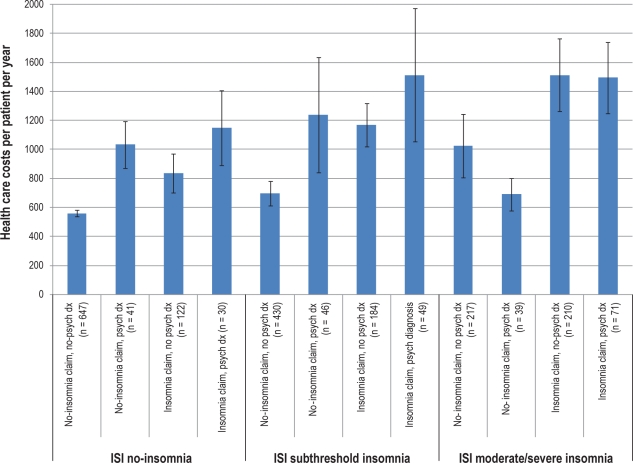
In the full multivariate model and after adjusting for subject's age, chronic medical and psychiatric comorbidities, and insomnia treatment type, the group with subthreshold insomnia had mean total health care costs 20% larger than the non-insomnia group; however, this increase was not statistically significant (P = 0.41). The moderate and severe insomnia group had mean total health care costs 75% larger than the non-insomnia group ($1323 vs. $757, P < 0.05). Those who had no insomnia-related health claim consistently had lower health care costs than those with an insomnia related claim ($586 vs. $898, $750 vs. $1241, and $974 vs. $1509 in the ISI no insomnia, subthreshold, and moderate/severe groups respectively). A similar trend was observed when we stratified by insomnia related claim and psychiatric diagnosis status. Those with no insomnia related claim and no psychiatric diagnosis had the lowest costs while those who had both insomnia related claim and a psychiatric diagnosis had the highest health care costs (Figure 2).
Figure 2.
Annual health care costs stratified by ISI insomnia status, insomnia claims, and psychiatric diagnosis
Multivariate model coefficients are presented in Table 3. As expected, increasing age, higher CDS, and a higher psychiatric index scores were all significantly associated with increased healthcare costs. Gender was not significantly associated with medical costs. Individuals reporting both prescription and over-the-counter (OTC) treatment had the highest costs, and those with prescription only, OTC only, or no treatment had lower costs.
Table 3.
Multivariate model
| Lost Productivity Costs GLM coefficient (SE) | Total Healthcare Costs GLM coefficient (SE) | |
|---|---|---|
| Demographics | ||
| Age | -0.032 (0.0035)** | 0.021 (0.004)** |
| Male | 0.237 (0.075)* | 0.111 (0.118) |
| Pre index date CDS | -0.016 (0.0144) | 0.124 (0.020)** |
| Pre index date Psychiatric Index | 0.293 (0.0777)** | 0.242 (0.099)* |
| Treatment type | ||
| Prescription treatment | 0.439 (0.151)* | -0.550 (0.239)* |
| OTC Treatment | 0.347 (0.160)* | -0.793 (0.262)** |
| No Treatment | 0.615 (0.145)* | -0.671 (0.228)** |
| Prescription and OTC (REF) | – | – |
| ISI Category | ||
| Moderate/Severe Insomnia (15-28) | 0.565 (0.095)** | 0.363 (0.142)* |
| Subthreshold Insomnia (8-14) | 0.306 (0.077)** | 0.103 (0.126) |
| No Insomnia (0-7) (REF) | – | – |
P < 0.001;
P < 0.05;
CDS, Chronic Disease Score Index.
Lost Productivity Sample Descriptive Characteristics
Descriptive characteristics of the lost productivity sample are presented in Table 1. Of this sample, 68.6% were female, while 40.9%, 35.9 %, and 23.2% fell into the ISI no insomnia, subthreshold insomnia, and moderate/ severe insomnia respectively. Far more respondents reported the presence of any presenteeism (80.5%) than absenteeism (11.8%). As expected, insomnia diagnosis claims were rare. Six percent had an insomnia diagnosis claim while 26.5% had insomnia related prescription claim. Mirroring the health care costs sample, 53.2% of the ISI moderate/severe insomnia group of the presenteeism sample had no insomnia related health care claim even though 92% of them report having their sleep problem for ≥ 1 year.
Lost Productivity Costs Findings
The subthreshold and moderate/severe insomnia groups reported increased lost productivity hours per week relative to the no insomnia groups. The no insomnia group reported a mean (SD) reduction of 6.2 (8.7) h/week (14.8% reduction) of productivity hours relative to the full maximum productivity potential of an individual, while the subthreshold and the moderate/severe groups reported a reduction of 8.5 (9.0) h/week (19.1%, P < 0.05) and 9.4 (8.2) h/week (23.5%, P < 0.05) respectively. Similarly, unadjusted mean (SD) lost productivity costs were $1035 for the no insomnia group (SD $5230) while the mean costs for the subthreshold and moderate/severe insomnia groups were $1323 (SD $6623) and $1554 (SD $5481), respectively (Table 2).
In the fully adjusted multivariate model (Table 2), mean lost productivity costs were 33% greater for the subthreshold insomnia group compared with the non-insomnia group ($1352 vs. $1013, P < 0.001). Mean lost productivity costs were 72% greater in the moderate/severe insomnia group compared with the no insomnia group ($1739 vs. $1013, P < 0.001). Those who had no insomnia-related health claim had greater lost productivity costs than those with an insomnia-related claim in the no insomnia ($1089 vs. $777) and subthreshold groups ($1478 vs. $984). In the moderate/sever insomnia group, those with an insomnia-related claim had greater lost productivity costs than those with no insomnia related claim ($2017 vs. $1134). No interpretable trend emerged when we stratified by insomnia related claim and psychiatric diagnosis status due to small cell size in each of the strata.
In contrast to medical costs, increasing age was associated with lower lost productivity costs. However, only 72 subjects (5.4%) in the work-for-pay sample were > 65 years old. Lost productivity costs were higher in men. While pre-period CDS scores were not significantly associated with lost productivity costs, the pre-period psychiatric index was significantly associated with higher lost productivity costs. Relative to patients using both prescription and OTC medications for the treatment of insomnia, patients using either prescription or OTC medications alone and those with no treatment had higher lost productivity costs. Interestingly, it is the patients with no insomnia treatment who appear to have the greatest lost productivity costs (Table 3).
DISCUSSION
This study used administrative health claims and direct interview data to estimate annual healthcare and lost productivity costs associated with insomnia severity. The study found healthcare and lost productivity costs to be consistently greater in moderate and severe insomnia groups even after adjusting for chronic medical and psychiatric comorbidities.
This association was not simply the product of the presence or absence of insomnia but rather was associated with insomnia severity in a gradient “dose response” fashion. Findings from this study were consistent with independent associations between insomnia and health care costs even in the absence of psychiatric diagnosis. This differs from the findings by Kessler et al., which found sleep problems to be associated with decreased work productivity only in the presence of depression.30 However, this difference may be due to the fact that the Kessler study used a chronic conditions checklist to ascertain the presence or absence of sleep problem and not a validated instrument to measure the presence and severity of insomnia. It is unfortunate that we did not have adequate sample size to examine lost productivity costs stratified by ISI insomnia status, insomnia claims and psychiatric diagnosis. Future studies will enable a more nuanced understanding of the independent and interactive contributions of insomnia and psychiatric comorbidities to productivity costs.
One of the strengths of this study is the use of a validated tool for assessing the probable presence of insomnia and not simply relying on administrative claims definitions. This study found that 50% of those with moderate/severe insomnia had no evidence of interacting with the health care system for insomnia-related treatment even though 91% of them report having their sleep problems for ≥ 1 year. These data replicate previous findings that insomnia is underreported and underdiagnosed, even in a health plan population that has coverage for medical care and prescription medications.
Having no insomnia-related treatment was associated with increased lost productivity costs and decreased total health care costs. This may be related to the differing natures of lost productivity and health care costs. Untreated insomnia is likely associated with increased daytime impairment, which may translate into more immediate lost productivity. Untreated insomnia may also be a marker for attitudes towards treatment-seeking and general interaction with the healthcare system. Although evidence suggests that untreated insomnia may contribute to increased severity of comorbid disorders,31–33 it is possible that those who are not taking any treatments for their insomnia are initially delaying their other general health care utilization and may have increased costs at subsequent time points when their medical conditions are more severe and require greater medical intervention.
More specifically, we found that health care costs were consistently lower among subjects who had no insomnia-related claim regardless of their ISI insomnia status. In contrast, we found that lost productivity costs were higher in those with an insomnia-related claim if they were in the ISI no insomnia or subthreshold insomnia groups. The moderate/severe insomnia group on the other hand had greater lost productivity costs if they had an insomnia related claim. This speaks again to the differing natures of the underlying causes of lost productivity and healthcare costs. Those who have no insomnia claims are likely not health care treatment seekers and as such they have lower health care costs. Those who had an insomnia related claim and who fell into the ISI categories of no and subthreshold insomnia may have had lower productivity costs due to the alleviation of insomnia symptoms with their insomnia treatment. This observation did not hold for those who had an insomnia related claim and moderate/severe insomnia, possibly due to their greater level of insomnia severity and/or other chronic conditions. The full longitudinal trajectory of productivity and health care utilization for this population is not ascertainable from the present data. Longitudinal designs could help shed light on this question by tracking insomnia severity and health care and productivity costs over multiple time points.
It is interesting to observe that the magnitude and absolute difference of health care costs for the insomnia and no insomnia groups in this study was considerably lower than the magnitude and absolute difference of health care costs from other similar studies that used administrative heath claims. For example in the study by Ozminkowski et al. the insomnia group (age 18-64) had predicted 6-month health care costs of $4755 vs. $3831 for the no insomnia group (absolute difference = $924).10 This is to be contrasted with annual predicted costs of $1323 and $757 for our moderate/severe insomnia group and no insomnia group respectively (absolute difference = $566). This disparate finding may be due to differences in the underlying two study populations. In contrast to the Ozminkowski study, our study used a sample of health plan covered lives and not necessarily those who are active in the health care system. Healthcare costs of non-users are generally skewed towards zero and as a result may be responsible for the lower estimates for health care costs in both the insomnia and comparison group in our study. The fact that a significant percentage of the insomnia groups in this sample had no evidence of interacting with the health care system suggests that this at least partially explains the difference between our study and Ozminkowski's study.
In addition to the aforementioned main findings, this study also had a number of important results regarding factors associated with productivity and health care costs. We found that productivity costs were associated with psychiatric comorbidi-ties, but not chronic medical comorbidities. This is in contrast to total medical costs which were associated with both chronic medical and psychiatric comorbidities. Subjects who are still in the workforce are younger (in the present study the mean age was 46.3 among those working versus 61.4 for those not working) and have fewer comorbid medical conditions. As a result chronic medical conditions may not be as relevant to their productivity. Interestingly, the associations of lost productivity and total health care costs with age were in opposite directions. Increasing age was associated with greater total health care costs while increasing age was associated with decreased lost productivity costs. This finding has implications for the kinds of interventions that employers might consider developing for their employees. For younger age groups, psychiatric comorbidities appear to be more related to worker productivity than are chronic medical conditions.
Insomnia in this sample, unlike psychiatric comorbidities in this study, was associated with both total health care and lost productivity costs. This also has implications for employer-based interventions. Even without fully understanding the causal chain from insomnia to productivity and health care costs, the presence and severity of insomnia could be a marker for identifying target populations that would benefit from interventions aimed at boosting productivity and decreasing utilization of the health care system.
Further studies are needed to demonstrate and quantify the health care and productivity cost-savings of targeted treatment for insomnia and to better understand the kinds of interventions that produce durable clinical outcomes with the least expense.
Findings from this study should be interpreted in light of a number of limitations. The use of private insurance health claims for assessing associations with health care costs has its well-described limitations, including generalizability and lack of coverage continuity.34 Particular to this investigation, we were unable to compare those who opted out of the study to the actual study participants due to IRB regulations. Thus, the generalizability of our findings may not be rigorously ascertained. Moreover, the study insomnia sample included patients with circadian rhythm disorders (307.45 and 780.55) who may be a distinct patient subgroup that disproportionately contributes to lost productivity costs. However, upon examination of the original study base we found that of 150,000 health plan members only 100 subjects (0.067%) had either of the above two codes. Given the small number of patients with this diagnoses codes (100/150,000), it is unlikely that their inclusion or exclusion in the study would impact the present findings.
Despite these limitations, evidence from this study suggests that factors associated with productivity costs and health care costs may be fundamentally different and may require different kinds of interventions. Furthermore, increasing insomnia severity was consistently found to be associated with greater lost productivity and increased health care costs. Future research should focus on better understanding mechanisms linking insomnia, health and productivity costs, and on determining whether treatment interventions reduce these costs.
DISCLOSURE STATEMENT
This study was sponsored by Eli Lilly. Dr. Sarsour, Dr. Swindle, and Anupama Kalsekar are employees and stockholders of Eli Lilly and Company. Dr. Walsh has consulted for Pfizer, Sanofi-Aventis, Cephalon, Schering-Plough/Organon, Neurocrine, Takeda America, Actelion, Sepracor, Jazz, Respironics, Transcept, Neurogen, GlaxoSmithKline, Somaxon, Eli Lilly, Evotec, Merck, Kingsdown, Vanda, Ventus, and Somnus and research support has been provided to Dr. Walsh's institution by Pfizer, Merck & Co., Somaxon, Evotec, Actelion, Vanda, Neurogen, Sanofi-Aventis, Ventus, Respironics, and Jazz Pharmaceuticals. Dr. Foley is an employee of Thomson Reuters. Thomson Reuters was contracted by Eli Lilly and Company to conduct the study. While Thomson Reuters received funding to conduct the study, Dr. Foley's participation in writing the manuscript was unfunded.
ACKNOWLEDGMENTS
The authors would like to acknowledge Drs. David Van Brunt and David J. Debrota for helpful comments on an earlier draft of this manuscript.
Footnotes
A commentary on this article appears in this issue on page 417.
REFERENCES
- 1.Morin CM, LeBlanc M, Daley M, Gregoire JP, Merette C. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. 2006;7:123–30. doi: 10.1016/j.sleep.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 2.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 3.Chilcott LA, Shapiro CM. The socioeconomic impact of insomnia. An overview. Pharmacoeconomics. 1996;10(Suppl 1):1–14. doi: 10.2165/00019053-199600101-00003. [DOI] [PubMed] [Google Scholar]
- 4.Fullerton DS. The economic impact of insomnia in managed care: a clearer picture emerges. Am J Manag Care. 2006;12:S246–52. [PubMed] [Google Scholar]
- 5.Hatoum HT, Kong SX, Kania CM, Wong JM, Mendelson WB. Insomnia, health-related quality of life and healthcare resource consumption. A study of managed-care organisation enrollees. Pharmacoeconomics. 1998;14:629–37. doi: 10.2165/00019053-199814060-00004. [DOI] [PubMed] [Google Scholar]
- 6.Kuppermann M, Lubeck DP, Mazonson PD, et al. Sleep problems and their correlates in a working population. J Gen Intern Med. 1995;10:25–32. doi: 10.1007/BF02599573. [DOI] [PubMed] [Google Scholar]
- 7.Leger D, Guilleminault C, Bader G, Levy E, Paillard M. Medical and socio-professional impact of insomnia. Sleep. 2002;25:625–9. [PubMed] [Google Scholar]
- 8.Linton SJ, Bryngelsson I-L. Insomnia and its relationship to work and health in a working-age population. J Occup Rehabil. 2000;10:169–83. [Google Scholar]
- 9.Metlaine A, Leger D, Choudat D. Socioeconomic impact of insomnia in working populations. Ind Health. 2005;43:11–9. doi: 10.2486/indhealth.43.11. [DOI] [PubMed] [Google Scholar]
- 10.Ozminkowski RJ, Wang S, Walsh JK. The direct and indirect costs of untreated insomnia in adults in the United States. Sleep. 2007;30:263–73. doi: 10.1093/sleep/30.3.263. [DOI] [PubMed] [Google Scholar]
- 11.Thase ME. Correlates and consequences of chronic insomnia. Gen Hosp Psychiatry. 2005;27:100–12. doi: 10.1016/j.genhosppsych.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 12.Walsh JK. Clinical and socioeconomic correlates of insomnia. J Clin Psychiatry. 2004;65(Suppl 8):13–9. [PubMed] [Google Scholar]
- 13.Walsh JK, Engelhardt CL. The direct economic costs of insomnia in the United States for 1995. Sleep. 1992;22(Suppl 2):S386–93. [PubMed] [Google Scholar]
- 14.Bolge SC, Doan JF, Kannan H, Baran RW. Association of insomnia with quality of life, work productivity, and activity impairment. Qual Life Res. 2009;18:415–22. doi: 10.1007/s11136-009-9462-6. [DOI] [PubMed] [Google Scholar]
- 15.Daley M, Morin CM, LeBlanc M, Gregoire JP, Savard J. The economic burden of insomnia: direct and indirect costs for individuals with insomnia syndrome, insomnia symptoms, and good sleepers. Sleep. 2009;32:55–64. [PMC free article] [PubMed] [Google Scholar]
- 16.Daley M, Morin CM, Leblanc M, Gregoire JP, Savard J, Baillargeon L. Insomnia and its relationship to health-care utilization, work absenteeism, productivity and accidents. Sleep Med. 2009;10:427–38. doi: 10.1016/j.sleep.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 17.Godet-Cayre V, Pelletier-Fleury N, Le Vaillant M, Dinet J, Massuel MA, Leger D. Insomnia and absenteeism at work. Who pays the cost? Sleep. 2006;29:179–84. doi: 10.1093/sleep/29.2.179. [DOI] [PubMed] [Google Scholar]
- 18.Kleinman NL, Brook RA, Doan JF, Melkonian AK, Baran RW. Health benefit costs and absenteeism due to insomnia from the employer's perspective: a retrospective, case-control, database study. J Clin Psychiatry. 2009;70:1098–104. doi: 10.4088/JCP.08m04264. [DOI] [PubMed] [Google Scholar]
- 19.Leger D, Massuel MA, Metlaine A. Professional correlates of insomnia. Sleep. 2006;29:171–8. [PubMed] [Google Scholar]
- 20.Loeppke R, Taitel M, Haufle V, Parry T, Kessler RC, Jinnett K. Health and productivity as a business strategy: a multiemployer study. J Occup Environ Med. 2009;51:411–28. doi: 10.1097/JOM.0b013e3181a39180. [DOI] [PubMed] [Google Scholar]
- 21.Loeppke R, Taitel M, Richling D, et al. Health and productivity as a business strategy. J Occup Environ Med. 2007;49:712–21. doi: 10.1097/JOM.0b013e318133a4be. [DOI] [PubMed] [Google Scholar]
- 22.Schultz AB, Chen CY, Edington DW. The cost and impact of health conditions on presenteeism to employers: a review of the literature. Pharmacoeconomics. 2009;27:365–78. doi: 10.2165/00019053-200927050-00002. [DOI] [PubMed] [Google Scholar]
- 23.Sarsour K, Morin CM, Foley K, Kalsekar A, Walsh JK. Association of insomnia severity and comorbid medical and psychiatric disorders in a health plan-based sample: Insomnia severity and comorbidities. Sleep Med. 2010;11:69–74. doi: 10.1016/j.sleep.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 24.Von Korff M, Wagner EH, Saunders K. A chronic disease score from automated pharmacy data. J Clin Epidemiol. 1992;45:197–203. doi: 10.1016/0895-4356(92)90016-g. [DOI] [PubMed] [Google Scholar]
- 25.Clark DO, Von Korff M, Saunders K, Baluch WM, Simon GE. A chronic disease score with empirically derived weights. Med Care. 1995;33:783–95. doi: 10.1097/00005650-199508000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Ashcraft ML, Fries BE, Nerenz DR, et al. A psychiatric patient classification system. An alternative to diagnosis-related groups. Med Care. 1989;27:543–57. doi: 10.1097/00005650-198905000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 28.Kessler RC, Ames M, Hymel PA, et al. Using the World Health Organization Health and Work Performance Questionnaire (HPQ) to evaluate the indirect workplace costs of illness. J Occup Environ Med. 2004;46:S23–37. doi: 10.1097/01.jom.0000126683.75201.c5. [DOI] [PubMed] [Google Scholar]
- 29.Moran JL, Solomon PJ, Peisach AR, Martin J. New models for old questions: generalized linear models for cost prediction. J Eval Clin Pract. 2007;13:381–9. doi: 10.1111/j.1365-2753.2006.00711.x. [DOI] [PubMed] [Google Scholar]
- 30.Kessler R, White LA, Birnbaum H, et al. Comparative and interactive effects of depression relative to other health problems on work performance in the workforce of a large employer. J Occup Environ Med. 2008;50:809–16. doi: 10.1097/JOM.0b013e318169ccba. [DOI] [PubMed] [Google Scholar]
- 31.Sunderajan P, Gaynes BN, Wisniewski SR, et al. Insomnia in patients with depression: a STAR*D report. CNS Spectr. 2010;15:394–404. doi: 10.1017/s1092852900029266. [DOI] [PubMed] [Google Scholar]
- 32.Pollack M, Kinrys G, Krystal A, et al. Eszopiclone coadministered with escitalopram in patients with insomnia and comorbid generalized anxiety disorder. Arch Gen Psychiatry. 2008;65:551–62. doi: 10.1001/archpsyc.65.5.551. [DOI] [PubMed] [Google Scholar]
- 33.Fava M, McCall WV, Krystal A, et al. Eszopiclone co-administered with fluoxetine in patients with insomnia coexisting with major depressive disorder. Biol Psychiatry. 2006;59:1052–60. doi: 10.1016/j.biopsych.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 34.Riley GF. Administrative and claims records as sources of health care cost data. Med Care. 2009;47:S51–5. doi: 10.1097/MLR.0b013e31819c95aa. [DOI] [PubMed] [Google Scholar]