Abstract
Background:
Khat chewing is popular among Yemenis. This study was performed to investigate the effects of khat chewing on periodontal tissue and oral hygiene status.
Methods:
A total of 730 subjects (336 chewers and 394 non-chewers with a mean age of 31.5 ± 0.8 and 29.4 ± 0.9 years, respectively) were involved. Clinical data on periodontal tissues, oral hygiene sta-tus, gingival bleeding, burning sensation in the soft tissues, halitosis, ulcers in the oral cavity, difficulty in opening the mouth and swallowing solid food were collected to evaluate periodontal condition. Lo-gistic regression analysis, student t test and chi-squared test were employed according to which hypo-theses were being tested.
Results:
The oral hygiene status of non-chewers was significantly better than that of chewers. The mean oral hygiene index of chewers was 2.12 ± 0.86 while that of non-chewers was 1.54 ± 1.12, the difference being statistically significant (P < 0.001). The incidence of gingival bleeding was signifi-cantly higher in khat-chewers. About 23% of chewers complained of difficulty in mouth-opening, as compared with only about 1% of non-chewers. Furthermore, 10% of chewers had difficulty in swal-lowing solid food. A burning sensation in the soft tissues was also found in a higher proportion of khat-chewers. Similarly, ulcers on the oral mucosa were present in about 7% of chewers, as com-pared to 0.5% of non-chewers. Gingival recession was present in about 51% and 26% of chewers and non-chewers, respectively.
Conclusion:
There does appear to be a relationship between the effect of chewing khat on peri-odontal tissue and oral hygiene status.
Keywords: Chewers, Gingival Hemorrhage, Khat, Oral hygiene, Yemen
Introduction
Khat (catha edulis) is a natural stimulant from the catha edulis plant, found in the flowering evergreen tree or large shrub of Celastracea family, which grows mainly in Yemen, Ethiopia, Somalia, Kenya, Saudi Arabia, and at high altitude areas in South Africa and Madagascar.1 The plant is known by different names in different countries: Qat in Yemen, Khat in Ethiopia, Mirra in Kenya and Qaad or Jaad in Somalia, but in most of the literature it is known as khat. In khat growing countries, the chewing of khat leaves for social and psychological reasons has been practiced for many centuries and its use has been gradually expanded to many countries worldwide.2 Modern users report that chewing khat gives increased energy levels, alertness and confidence, a sense of happiness, better thinking capacity and creativity, facilitation of communication ability, enhanced imaginative ability and the capacity to associate ideas. For some, chewing khat is a method of increasing energy and elevating mood in order to improve their work performance.3 The active ingredient of khat responsible for its psychostimulant effect is an alkaloid chemical known as cathinone, which is structurally and chemically similar to damphetamine, and cathine, a milder form of cathinone. Cathinone is a highly potent stimulant, which produces sympathomimetic and central nervous system stimulation analogous to the effect of amphetamine. Fresh leaves contain both ingredients; those left unrefrigerated beyond 48 hours would contain only cathine, which explains users′ preference for fresh leaves. Khat loses its potency after 48 hours. The results of various in vivo and in vitro experiments indicate that the substance could be considered as a “natural amphetamine”.4
In Yemen, khat is commonly used for social recreation. Occupational groups such as motor vehicle drivers and truck drivers chew khat during long distance driving to keep them awake; those in cutting of rock stone and building establishment, also use it under a variety of other conditions. A significant number of students chew khat to be alert especially during examination periods. There is also specific usage of khat by the special sections of the community: craftsmen and farmers use khat to reduce physical fatigue and traditional healers to heal ailments.5
Khat leaves, which are generally placed in the mouth in the lower distal mucobuccal fold, are usually chewed during sociocultural meetings where the chewing process may take up to 6 hours.6 Since the process of khat chewing has a drying effect on the oral mucosa, its users tend to consume a great quantity of fluids.7 Some of the khat users also supplement their chewing practice with smoking habits.8 Side effects that are believed to be related to the chewing of khat include systemic effects like elevation of blood pressure, tachycardia, hyperthermia, increased sweating, muscular weakness, loss of appetite, spermatorrhea some gastrointestinal disturbances9 and local (oral) effects like gingival bleeding,10 halitosis, difficulty in opening the mouth periodontitis,11 teeth discoloration xerostomia , and ulcers in the oral cavity.12
Materials and Methods
Subjects
A crosssectional study was performed on 730 patients attending the outpatient dental clinics of the government dental college, Sana′a University, Yemen. The subjects were divided into two groups, khatchewers (n = 336) and nonchewers (n = 394) for comparison purposes. The mean age (SE) of the khatchewers and nonchewers was 31.5 (0.8) and 29.4 (0.9) years, respectively. About 25% of khatchewers and 4% of nonchewers were smokers. The subjects were examined at the Government Dental College, Sana′a University, under artificial light using a mouth mirror, explorer and curved probe. Data related to gingival bleeding, halitosis, ability to swallow solid food, presence of a burning sensation in the soft tissues, etc., were collected by questionnaire, and the presence of ulcers in the oral cavity was checked clinically. These data were considered to be possible indicators of the presence and extent of lesions. In addition, each subject was asked to open his/her mouth in order to confirm whether there was any difficulty with mouth opening.
Only individuals who provided a history of chewing khat for more than 3 years, not less than 4 days per week and not less than 4 hours per day were considered. In addition, only individuals who used to chew khat on one side of their mouth were selected. So, it was considered that the nonchewing side which was diagnosed as the healthy side or the controlled side is the only parameter used to make sure that there is no other cause of periodontal disease presented at the time of investigation.
Oral Hygiene Status
The oral hygiene status of the involved subjects was determined by using the Simplified Oral Hygiene Index (OHI-S). The OHI-S, introduced by Greene and Vermilion13 in 1964 and quoted by Peter (2004), comprises the Simplified Debris Index (DI-S) and Simplified Calculus Index (CI-S). Each of these indices is based on numerical determinations representing the amount of debris or calculus on six preselected tooth surfaces.
Debris Index (DI-S)
DI-S was used for evaluating the extent of debris present on the six preselected tooth surfaces, i.e., buccal surface of the selected upper first molars, lingual surface of the selected lower first molars, and labial surface of the upper right and lower left central incisors. The surface area covered by debris was estimated by running the side of Shepherd crook explorer along each tooth surface.
Debris Index – Simplified - Scoring System
Score 0: Absence of debris, Score 1: Soft debris covering less than the cervical one-third of the tooth surface, Score 2: Soft debris covering more than the cervical one-third of the exposed tooth surface but less than the cervical two-thirds, Score 3: Soft debris covering more than the cervical two thirds of the exposed tooth surface.
Calculus Index – Simplified (CI-S)
An explorer was used for scoring the calculus. The same teeth as those for evaluation of the debris index were examined. The surface area covered by calculus was detected supragingivally, and subgingival calculus was explored on a randomly selected tooth quadrant.
Calculus Index – Simplified – Scoring System
Score 0: Absence of calculus, Score 1: Calculus covering less than the cervical one-third of the exposed tooth surface, Score 2: Supragingival calculus covering more than the cervical one-third, but less than the cervical two-thirds of the exposed tooth surface, or presence of individual flecks of subgingival calculus around the cervical portion of the tooth, Score 3: Supragingival calculus covering more than the cervical two-thirds of the exposed tooth surface, or a continuous heavy band of subgingival calculus around the cervical portion of the tooth.
The Simplified Oral Hygiene Index score for each individual was obtained by combining the Simplified Debris Index and the Calculus Index. Totaling the debris score per tooth surface and dividing by the number of the surfaces examined yielded the Simplified Debris Index score for an individual. The same method was used to obtain the CI-S. Thus, OHI-S = DI-S + CI-S. The Simplified Oral Hygiene Index (OHI-S) values range from 0 to 6. The clinical levels of oral hygiene that can be associated with group OHI-S scores are as follows; Good: 0.0 to 1.2, Fair: 1.3 to 3.0, and Poor: 3.1 to 6.0.
Gingival Recession
Assessment of gingival recession was done to specifically determine its extent, i.e., displacement of the gingival margin at least 1 mm apical to the cemento-enamel junction in all subjects.
Statistical analysis
Logistic regression analysis, student t test and chisquared test were employed according to which hypotheses were being tested (P < 0.05).
Results
Table 1, illustrating the different oral hygiene measures practiced routinely by the khatchewers and non-chewers. The data show that quite a large number of khat chewers (88%) and non-chewers (91%) used paste regularly for maintenance of oral hygiene. However, 9% of chewers did not use toothpaste, as compared to 5% of non-chewers. There was no significant difference between khat-chewers and non-chewers with respect to oral hygiene measures used. About 49% of non-chewers had good oral hygiene status, as compared to only about 15% of khat chewers (Table 2). The oral hygiene status of non-chewers was significantly better than that of chewers. Poor oral hygiene status was also realized in a higher proportion of khat-chewers (18%) than in non-chewers (11%). The mean oral hygiene index of chewers was 2.12 ± 0.86 while that of non-chewers was 1.54 ± 1.12, the difference being statistically significant (P < 0.001).
Table 1.
Oral hygiene measures adopted by subjects
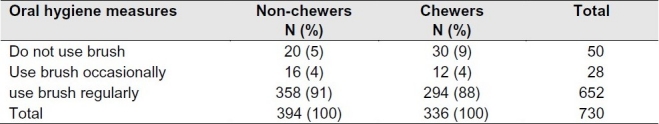
Table 2.
Oral hygiene status of the chewers and non-chewers

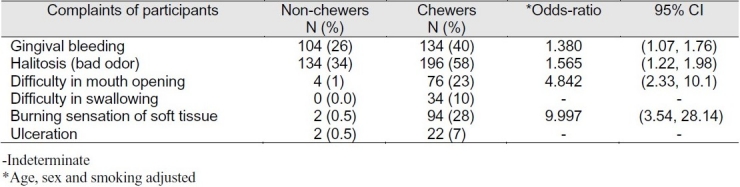
Table 3 shows the different complaints of the subjects related to the oral cavity. The incidence of gingival bleeding was significantly higher in khat-chewers than in non-chewers, and more chewers (58%) had halitosis. About 23% of chewers com-plained of difficulty in mouthopening, as compared with only about 1% of non-chewers. Furthermore, 10% of chewers had difficulty in swallowing solid food, whereas none of the non-chewers had this problem. A burning sensation in the soft tissues was also found in a higher proportion of khat-chewers than in non-chewers. Similarly, ulcers on the oral mucosa were present in about 7% of chewers, as compared to 0.5% of non-chewers. Logistic regression analysis revealed that, in general, chewers had significant odds ratios for the various oral complaints studied with respect to non-chewers after adjustment for age, sex and smoking (Table 3). Sex and smoking did not have any significant impact on the odds ratio. Furthermore, age had no significant impact on the odds ratio for difficulty in mouth-opening, difficulty with swallowing, burning sensation in soft tissues, and ulceration.
Table 3.
Distribution of subjects according to their complaints
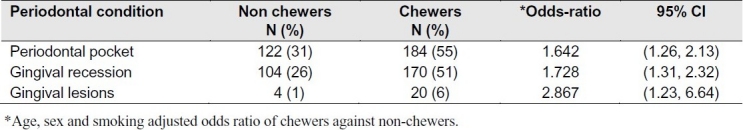
An effect of khat-chewing on the periodontium, i.e., the occurrence of periodontal pockets, gingival lesions and gingival recession, was observed clinically. Periodontal pockets, occurrence of gingival lesions, as well as gingival recession also had a higher incidence in khat-chewers than in non-chewers (Table 4). Gingival recession was present in about 51% and 26% of chewers and non-chewers, respectively. Logistic regression analysis also showed significant odds ratios for these conditions for chewers as compared with non-chewers (Table 4). This analysis showed that khat-chewers are at higher risk for the various conditions studied, irrespective of sex, indicating a causative role of khat in periodontal diseases.
Table 4.
Periodontal condition of chewers and non-chewers
Discussion
The present study revealed a number of interesting and relevant findings. There is no significant difference between khat-chewers and non-chewers with respect to oral hygiene measures used. However, the mean value of the OHI among the chewers was higher than that among non-chewers. This suggests that khat-chewers had a poorer oral hygiene status than non-chewers, even though both groups undertook almost the same oral hygiene measures, and that khat-chewing plays a significant role in deterioration of oral hygiene. Complaints such as gingival bleeding, halitosis, difficulty with mouth-opening and swallowing solid food, and the burning sensation in the soft tissues were significantly more common among chewers than among non-chewers.
These data indicate a potential role of khat-chewing in oral health status. Previously, Hill and Gibson,14 reported that khat-chewing was associated with a higher prevalence of gingival bleeding. The hardness of the khat and friction mechanism with mucosal and periodontal tissues might be responsible for the poor periodontal status of chewers.7 Khat, which contains alkaloids, in addition to the presence of pesticides in khat leaves might have a significant causative role in periodontal diseases along with other variables such as the level of oral hygiene, halitosis and gingival bleeding. This lends support to the earlier findings of pigmentation on the khat chewing site which is directly related to mechanical and chemical components in the khat leaves. I believe that such chemicals may also contribute to the development of oral white changes.
The present study also indicated deterioration of periodontal condition among khat-chewers. Periodontal pockets, gingival lesions and gingival recession were more prevalent among chewers than among non-chewers, even though both groups adopted approximately the same oral hygiene measures. Furthermore, loss of periodontal attachment and greater calculus formation has also been reported in khat-chewers.15 Hill et al. reported a higher prevalence of attachment loss in older age groups than in younger age groups,14 suggesting that age could be a factor affecting such changes. The present study also suggests that age has a significant impact on the prevalence of oral complaints and periodontal conditions. The age, sex and smoking adjusted odds ratios for khat-chewers against non-chewers were statistically significant for various complaints and conditions, suggesting a role of the chewing habit in the deterioration of periodontal status as well as various oral conditions in khat-chewers compared with non-chewers. Furthermore, khat containing pesticides might be cytotoxic to periodontal fibroblasts and thus, exacerbate preexisting periodontal disease as well as impair periodontal reattachment.16 The present study indicated that chewing khat has a potentially causative role in the development of oral lesions, and deterioration of oral hygiene and periodontal status, as higher odds ratios were observed for various lesions and peri-odontal status after adjustment for age and sex.
The hardness of the khat leaves and friction mechanism with mucosal tissues might act as a predis-posing factor in the occurrence of ulcers among chewers. These ulcers usually observed at the khat chewing sites only. Clinically, this type of ulcers is characterized by burning like lesions.
The Clinicopathological effects of khat habit on the oral mucosa are well documented.17 These effects include different grades of keratotic white lesions, keratinization of non-keratinized oral mucosa and epithelial dysplasia. Recent genetic study showed that khat consumption, especially when accompanied by tobacco consumption might be a potential cause of oral malignancy.18 This finding was supported by another study, which demonstrated the khat habit as a probable contributing etiological factor of squamous cell carcinoma.19
The findings of present study support the need for health education and promotion programs to increase the awareness of the problem in the population. Positive long term lifestyle changes, including physical exercise should be established early in life since khat habit tends to start in childhood and progress into adulthood.
Health education programs disseminated by the mass media to raise the public awareness should focus on the real impact of the habit on students and the misconception that khat enhanced productivity and achievement. More studies are needed to explore other social and educational prospective issues so that more comprehensive preventive strategies could be established.
Future studies are needed to investigate the effects of different types of pesticides that used to facilitate rapid growing of kaht on oral and general health.
Conclusion
The present study revealed that the oral hygiene status of non-chewers was significantly better than that of chewers. In addition, this study also indicated deterioration of periodontal condition among khat-chewers.
References
- 1.Weir S. London: British Museum Publications; 1985. Qat in Yemen: consumption and social change. [Google Scholar]
- 2.Nencini P, Grassi MC, Botan AA, Asseyr AF, Paroli E. Khat chewing spread to the Somali community in Rome. Drug Alcohol Depend. 1989;23(3):255–8. doi: 10.1016/0376-8716(89)90089-6. [DOI] [PubMed] [Google Scholar]
- 3.Kalix P. Khat: scientific knowledge and policy issues. Br J Addict. 1987;82(1):47–53. doi: 10.1111/j.1360-0443.1987.tb01436.x. [DOI] [PubMed] [Google Scholar]
- 4.Kalix P. Leaf of Allah: Khat & agricultural transformation in Harerge. In: Gebissa E, editor. The pharmacology of khat. Ohio: Ohio State University Press; 2004. pp. 69–73. [Google Scholar]
- 5.Mekasha A. Proceedings of the International Symposium on khat. Addis Ababa, Ethiopia: 1984. Dec 15, Clinical aspects of khat (Catha edulis forsk) pp. 77–83. [Google Scholar]
- 6.Elmi AS. The chewing of khat in Somalia. J Ethno-pharmacol. 1983;8(2):163–76. doi: 10.1016/0378-8741(83)90052-1. [DOI] [PubMed] [Google Scholar]
- 7.Al-Bekairi AM, Abulaban FS, Qureshi S, Shah AH. The toxicity of of catha edulis (Khat). A review. Fitoterapia. 1991;62(4):291–300. [Google Scholar]
- 8.Giannini AJ, Miller NS, Turner CE. Treatment of khat addiction. J Subst Abuse Treat. 1992;9(4):379–82. doi: 10.1016/0740-5472(92)90034-l. [DOI] [PubMed] [Google Scholar]
- 9.Al Motarreb A, Briancon S, Al Jaber N, Al Adhi B, Al Jailani F, Salek MS, et al. Khat chewing is a risk factor for acute myocardial infarction: a case-control study. Br J Clin Pharmacol. 2005;59(5):574–81. doi: 10.1111/j.1365-2125.2005.02358.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nencini P, Ahmed AM, Elmi AS. Subjective effects of khat chewing in humans. Drug Alcohol Depend. 1986;18(1):97–105. doi: 10.1016/0376-8716(86)90118-3. [DOI] [PubMed] [Google Scholar]
- 11.Halboub E, Dhaifullah E, Abdulhuq M. Khat chew-ing and smoking effect on oral mucosa: a clinical study. Acta Medica (Hradec Kralove) 2009;52(4):155–8. doi: 10.14712/18059694.2016.122. [DOI] [PubMed] [Google Scholar]
- 12.Alsharabi AK. Khartoum: Khartoum University; Khartoum: Khartoum University; 2002. Oral and para-oral lesions caused by takhzeen Al-Qat.[Thesis] [Google Scholar]
- 13.Peter S. Essentials of Preventive Community Dentistry. In: Peter S, editor. Indices in dental epidemiology. New Delhi: Arya (Medi) Publishing House; 2004. pp. 127–240. [Google Scholar]
- 14.Hill CM, Gibson A. The oral and dental effects of q'at chewing. Oral Surg Oral Med Oral Pathol. 1987;63(4):433–6. doi: 10.1016/0030-4220(87)90255-6. [DOI] [PubMed] [Google Scholar]
- 15.Anerud A, Loe H, Boysen H. The natural history and clinical course of calculus formation in man. J Clin Periodontol. 1991;18(3):160–70. doi: 10.1111/j.1600-051x.1991.tb01128.x. [DOI] [PubMed] [Google Scholar]
- 16.Kennedy JG, Teague J, Rokaw W, Cooney E. A medical evaluation of the use of qat in North Yemen. Soc Sci Med. 1983;17(12):783–93. doi: 10.1016/0277-9536(83)90029-1. [DOI] [PubMed] [Google Scholar]
- 17.Ali AA, Al Sharabi AK, Aguirre JM, Nahas R. A study of 342 oral keratotic white lesions induced by qat chewing among 2500 Yemeni. J Oral Pathol Med. 2004;33(6):368–72. doi: 10.1111/j.1600-0714.2004.00145.x. [DOI] [PubMed] [Google Scholar]
- 18.Kassie F, Darroudi F, Kundi M, Schulte- Hermann R, Knasmüller S. Khat (Catha edulis) consumption causes genotoxic effects in humans. Int J Cancer. 2001;92(3):329–32. doi: 10.1002/ijc.1195. [DOI] [PubMed] [Google Scholar]
- 19.Nasr AH, Khatri ML. Head and neck squamous cell carcinoma in Hajjah, Yemen. Saudi Med J. 2000;21(6):565–8. [PubMed] [Google Scholar]


