Abstract
The release of the neurotransmitter norepinephrine (NE) is modulated by presynaptic adenosine receptors. In the present study we investigated the effect of a partial activation of this feedback mechanism. We hypothesized that partial agonism would have differential effects on NE release in isolated hearts as well as on heart rate in vivo depending on the genetic background and baseline sympathetic activity. In isolated perfused hearts of Wistar and Spontaneously Hypertensive Rats (SHR), NE release was induced by electrical stimulation under control conditions (S1), and with capadenoson 6 · 10−8 M (30 µg/l), 6 · 10−7 M (300 µg/l) or 2-chloro-N6-cyclopentyladenosine (CCPA) 10−6 M (S2). Under control conditions (S1), NE release was significantly higher in SHR hearts compared to Wistar (766+/−87 pmol/g vs. 173+/−18 pmol/g, p<0.01). Capadenoson led to a concentration-dependent decrease of the stimulation–induced NE release in SHR (S2/S1 = 0.90±0.08 with capadenoson 6 · 10−8 M, 0.54±0.02 with 6 · 10−7 M), but not in Wistar hearts (S2/S1 = 1.05±0.12 with 6 · 10−8 M, 1.03±0.09 with 6 · 10−7 M). CCPA reduced NE release to a similar degree in hearts from both strains. In vivo capadenoson did not alter resting heart rate in Wistar rats or SHR. Restraint stress induced a significantly greater increase of heart rate in SHR than in Wistar rats. Capadenoson blunted this stress-induced tachycardia by 45% in SHR, but not in Wistar rats. Using a [35S]GTPγS assay we demonstrated that capadenoson is a partial agonist compared to the full agonist CCPA (74+/−2% A1-receptor stimulation). These results suggest that partial adenosine A1-agonism dampens stress-induced tachycardia selectively in rats susceptible to strong increases in sympathetic activity, most likely due to a presynaptic attenuation of NE release.
Introduction
Sympathetic activity regulates heart rate and cardiac function via stimulation of a wide variety of G-protein coupled receptors, such as alpha- and beta-adrenergic receptors [1]. The only class of drugs to date to be widely used to modulate the activity of the sympathetic nervous system are beta blockers, mostly β1-selective, which act by postsynaptic blockade of beta-adrenoceptors in the heart. They do not influence presynaptic regulation of sympathetic activity and the release of the neurotransmitter norepinephrine (NE) [2], [3].
A different way of modulating sympathetic activity is the modulation of the release of NE from pre- or postganglionic nerve terminals. Moxonidine, for example, is thought to attenuate central sympathetic tone either by stimulating central I1-imidazoline receptors in the medulla oblongata [4], [5], [6], or via central presynaptic alpha-adrenoceptors [7], thereby reducing sympathetic tone in the central nervous system. Clonidine, a central α2-receptor agonist, also inhibits sympathetic tone by peripheral presynaptic inhibition of transmitter release from postganglionic neurons [8]. In the heart, NE is released from sympathetic nerve terminals upon stimulation and acts on the myocardium by modulating heart rate, myocardial contractility and calcium handling via alpha- and beta-adrenergic receptors [9]. Its exocytotic release is presynaptically modulated during myocardial ischemia via adenosine-A1 and adrenergic α2-receptors [10], [11]. Recently, agonists of the adenosine A1 receptor, either full or partial, have been tested in a variety of disease conditions [12]. Because of the potential modulation of NE release in the heart, agonists of the adenosine A1 receptor might offer a unique opportunity to selectively modulate sympathetic activity to the heart. In a recent phase-II study in patients with angina pectoris it was noted that the novel A1-agonist capadenoson (BAY 68-4986) selectively blunted the heart rate increase during treadmill exercise without altering baseline frequency [12], [13].
This effect of capadenoson on the heart rate could be due to a presynaptic modulation of the release of NE which is particularly effective under conditions of an increased sympathetic nerve activity. To test this hypothesis, the effects of the adenosine-A1 agonist capadenoson on the NE release in vitro as well as on heart rate in vivo was evaluated in two rat strains with genetically different levels of sympathetic activity, Wistar and Spontaneously Hypertensive rats (SHR). The latter strain has an increased sympathetic tone already at rest and exhibits a much stronger increase in sympathetic tone upon restraint stress than Wistar rats [14], [15].
Methods
Study drug
Capadenoson (molecular weight 520.0 g/mol) was provided by Bayer Schering Pharma AG (Wuppertal, Germany) as a research compound Bay 68-4986-EXTRUDAT Fa.20 Pt.041027 [16]. This water-soluble formulation contains 5% active substance by weight. For the in vitro experiments the substance was solubilised in dimethyl sulfoxide (DMSO) 10%, polyethylene glycol 30%, and physiologic (0.9%) sodium chloride 60% (all Sigma-Aldrich, Germany). The final concentration of DMSO in the perfusate did not exceed 0.01%. For the in vivo experiments Bay 68-4986-EXTRUDAT was weighed according to body weight and administered orally. A dose of 0.15 mg/kg was chosen on the basis of previous experiments which showed it not to induce bradycardia in Wistar rats. The formulation was prepared freshly each day before administration.
Stimulation-induced norepinephrine release
All animal experiments were conducted according to the Guide for the Care and Use of Laboratory Animals (NIH publication No. 86-23, revised 1985), and were approved by the Regierung von Oberbayern (Az 55.2-1-54-2531.3-15-07).
A total of 14 Wistar rats and 18 SHR (Charles River Inc., Germany; body weight 200–50 g, all female) underwent experiments to evaluate the exocytotic, stimulation-induced NE release during electrical field stimulation as described before [11]. Rats were killed by an injection of pentobarbital i.p. (0.5 ml/100 mg body weight, Merial, Germany), and hearts were rapidly excised, and placed in ice cold Krebs-Henseleit solution (KHL). They were quickly mounted on a Langendorff apparatus for retrograde perfusion with KHL. Perfusion rate was kept constant at 10 ml/min, the temperature was adjusted to 37°C, and the pH to 7.4 through bubbling with 5% CO2/95% O2. Via an inflow line desipramine (Sigma-Aldrich, Germany) at a concentration of 10−7 M was added to the perfusion buffer. After an equilibration period of 20 minutes, electrical field stimulation was commenced via two metal paddles adjacent to both sides of the beating heart for 1 minute (5V, 6 Hz). We collected the efflux in plastic tubes the minute before, during, and 3 minutes after the stimulation. These were rapidly frozen in liquid nitrogen and stored at −20°C till analysis. The NE release was calculated as the cumulative release induced by the electrical stimulation. After the first stimulation (S1), the study drug capadenoson at concentrations of 30 µg/l (6 · 10−8 M) or 300 µg/l (6 · 10−7 M), or 2-chloro-N6-cyclopentyladenosine (CCPA, 10−6 M, Sigma-Aldrich), respectively, were added via separate perfusion lines for 30 minutes. After this time a second stimulation (S2) was executed to determine the effect of the drugs on NE release compared to the first stimulation. The effect of each pharmacological intervention was analysed by calculating the ratio of NE release induced by the second and first stimulation (S2/S1 ratio).
Determination of norepinephrine concentration
Norepinephrine was detected in the samples using high-performance liquid chromatography (HPLC) with electrochemical detection (ECD) [17]. After thawing samples were prepared by a reagent kit for “catecholamines in plasma” (Chromsystems, Germany). Shortly, 1 ml of the sample was mixed with 500 µl extraction buffer plus 50 µl internal standard (IS), and extracted by solid phase extraction (SPE). Elution from SPE column was carried out by 120 µl elution buffer. Fifty µl of the eluted sample were separated by HPLC. Epinephrine and norepinephrine were detected by ECD, and quantified by an external standard involving the IS. The sensitivity of this assay is <15 pg/ml norepinephrine. Values are given as pmol per g wet heart weight.
Restraint stress experiments and in-vivo telemetry
The in vivo experiments were approved by Landesamt für Natur, Umwelt und Verbraucherschutz (Az 8.87-50.10.44.08.068). Female Wistar rats (n = 24) or SHR (n = 40) at a body weight of 200–220 g (breeder: Charles River, Germany) were included for a restraint stress test [18]. All animals were housed at an ambient temperature of ∼22°C, maintained on a 12-hour light/dark cycle with free access to standard laboratory rat chow and water ad libitum.
Animals were equipped with implantable radiotelemetry, and a data acquisition system (Data Sciences International, St. Paul MN, U.S.A.), comprised of a chronically implantable transducer/transmitter unit equipped with a fluid-filled catheter. Rats were instrumented at least one month prior to the experiments. The transmitter was implanted into the peritoneal cavity and the sensing catheter was inserted into the descending aorta. The animals were allocated to 4 groups:
1) Wistar rats with vehicle or 2) capadenoson 0.15 mg/kg (each n = 12)
3) Hypertensive SHR with vehicle or 4) capadenoson 0.15 mg/kg (each n = 20)
All animals were treated with vehicle or capadenoson for 5 days. Drug administration took place at 9.00 a.m. On day 5, all animals were placed into transparent restraint tubes for a period of 2 hr between 11:00 and 13:00. All animals experienced this treatment for the first time in their life. A dose of 0.15 mg/kg was chosen after prior dose-finding studies, which ruled out significant effects of capadenoson on blood pressure between 0.1 mg/kg and 0.3 mg/kg, whereas there was a significant reduction in resting blood pressure at higher doses (Fig. S1).
[35S]-GTPγS binding assay
Human frontal cortex was obtained from Analytical Biological Services Inc. (Wilmington, DE, USA). Membranes from the human cortex were prepared as described previously [19]. [35S]GTPγS binding was measured as described by Lorenzen [20]. Briefly, 5 µg of membrane protein was incubated in a total volume of 160 µl for 2 hr at 25°C in a shaking water bath. [35S]GTPγS binding in control incubations and in the presence of capadenoson showed a linear time course up to this incubation time. Binding buffer contained 50 mM Tris/HCl, pH 7.4, 2 mM triethanolamine, 1 mM EDTA, 5 mM MgCI2, 10 µM GDP, 1 mM dithiothreitol, 100 mM NaCl, 0.2 units/ml adenosine deaminase, 0.2 nM [35S]GTPγS, and 0.5% bovine serum albumin. Non-specific binding was determined in the presence of 10 µM GTPγS. Incubations were terminated through filtration of the samples over multiscreen FB glass fiber filters (Millipore, Billerica, MA, USA) followed by two washes with binding buffer. The filters were dried, coated with scintillator and counted for radioactivity. Binding curves of [35S]GTPγS were analyzed by nonlinear regression using GraphPad Prism (GraphPad Software Inc., San Diego, CA, USA).
GTP shift assay
Preparation of brain membrane: Crude synaptosomal membranes from rat brain were prepared according to the method described by Lohse [21]. Male Wistar rats (150–250 g) were killed be cervical dislocation, the brain cortex was quickly removed and immediately placed in 0.32 mol/l sucrose (4°C). The tissue was homogenized in 10 volumes sucrose in a glass/teflon homogenizer (clearing 0.2 mm; 500 rpm for 30 s). The homogenate was centrifuged at 1000 x g for 10 min to remove the nuclear fraction and the supernatant centrifuged at 30000 x g for 30 min to give the P2 fraction. The pellets were resuspended in 10 ml of water and left on ice for 30 min to give synaptosomal membranes. After a final centrifugation step at 48000 x g for 10 min the membranes were resuspended in 50 mmol/l Tris-HCl buffer, pH 7.4 and incubated with 2 U/ml adenosine deaminase (ADA) at 37°C for 30 min. The membranes were frozen in small aliquots and stored at −80°C until binding assay. Protein was measured according to Bradford, using a BIOrad assay kit.
Receptor binding studies: The adenosine A1 receptor binding assay was carried out on rat brain cortical membranes and with 0.4 nM [3H] 8-cyclopentyl-1,3-dipropylxanthine (DPCPX, Kd = 0.28 nM) as the radioligand. The assay was performed as originally described by Lohse et al. [22] and modified by van der Wenden et al. [23]. 10 µg of membrane protein were incubated at 37°C for 20 min with 0.4 nM [3H]DPCPX and adenosine A1 agonist in different concentrations in buffer (50 mM Tris-HCl, pH 7.4, 2 U/ml ADA) in the presence and absence of GTP. Nonspecific binding was determined in the presence of 10 µM R-PIA. Incubation was terminated by rapid filtration through GF/B glass fibre filter plates. Filters were washed three times with icecold Tris-HCl buffer 50 mM, pH 7.4. Radioactivity of the filter plate was counted with 100 µl scintillation cocktail in a Microbeta TriLux beta counter (PerkinElmer, Massachusetts, USA).
Statistical analysis
All values are expressed as mean +/− standard error of means, unless otherwise indicated. Means were compared with ANOVA, unless a nonparametric distribution was assumed. In this case Kruskal-Wallis-test was performed. For the comparison of norepinephrine values from second to first stimulation a paired t-test was used. A p-value <0.05 was considered statistically significant.
Results
Effect of capadenoson on stimulation-induced NE release
The effect of capadenoson on stimulation-induced NE release was evaluated in isolated perfused rat hearts of Wistar and SHR strains.
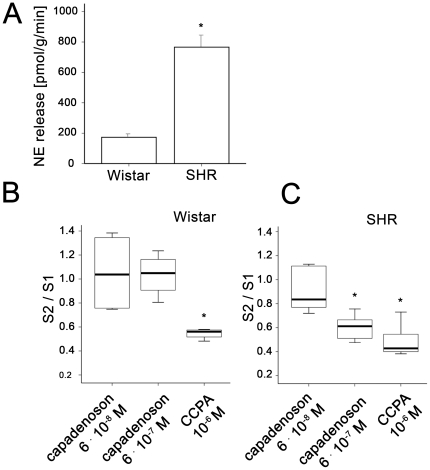
Under basal conditions without pharmacological modulation of A1 receptors, the NE release was 4-times higher in SHR compared to Wistar rats (SHR 766+/−87 pmol/g, n = 18, vs. 173+/−18 pmol/g, n = 14; p<0.01, fig. 1A). There was no indication for depletion of norepinephrine under control conditions without pharmacological intervention (Fig. S2).
Figure 1. Norepinephrine release from isolated rat hearts is modulated by adenosine agonists.
A) Mean of absolute NE concentration released during electrical field stimulation without pharmacologic modulation (Wistar n = 18, SHR n = 14; p<0.01). B) The effect of capadenoson and CCPA (capadenoson 6 · 10−8 M n = 6, capadenoson 6 · 10−7 M n = 4, CCPA 10−6 M n = 4) in Wistar rats. C) The effect of capadenoson and CCPA (capadenoson 6 · 10−8 M n = 6, capadenoson 6 · 10−7 M n = 5, CCPA n = 7) in SHR. The first stimulation (S1) served as an individual control without intervention; the second stimulation (S2) was performed after 30 minutes pretreatment with either capadenoson or CCPA. S2/S1 expressed as means +/− SEM, * p<0.01 for NE release with pharmacological modulation vs NE release without.
As demonstrated in Fig. 1B, capadenoson had no effect on NE release in Wistar rats, whereas addition of CCPA at a concentration of 10−6 M led to a robust decrease in the amount of NE release (S2/S1 = 1.1+/−0.11 for capadenoson 6 · 10−8 M, n = 6, p = 0.9; S2/S1 = 1.0+/−0.09 for capadenoson 6 · 10−7 M, n = 4, p = 0.8; S2/S1 = 0.5+/−0.02 for CCPA 10−6 M, n = 4, p = 0.007).
To the contrary, in SHR, capadenoson led to a significant concentration-dependent decrease of NE, as shown in Fig 1C. (S2/S1 = 0.9+/−0.07 for capadenoson 6 · 10−8 M, n = 6, p = 0.1; S2/S1 = 0.6+/−0.05 for capadenoson 6 · 10−7 M, n = 5, p = 0.03; S2/S1 = 0.5+/−0.05 for CCPA 10−6 M, n = 7, p = 0.003).
Thus, we observed a reduction of stimulation-induced NE release by capadenoson at a dose of 6 · 10−7 M in SHR only. This reduction was comparable to the effect of 10−6 M CCPA.
Effect of capadenoson on stress-induced increase of heart rate
In the in vivo experiments, Wistar rats and SHR were pre-treated with capadenoson at a concentration of 0.15 mg/kg for 5 days. On day 5, a stress test (physical restraint) was performed for 2 hours. The plasma concentration of capadenoson measured 3 hours after drug intake remained constant in the 5 days prior to the restraint stress test and averaged 7.63 µg/l on day 4 and 5, respectively.
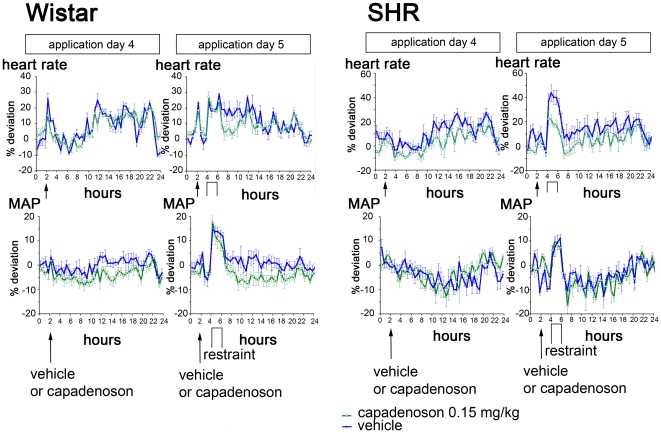
As listed in Table 1, mean heart rate was not affected by capadenoson during resting condition, neither in Wistar nor in SHR. During the 2 hours of physical restraint, we observed an increased heart rate in both strains (Wistar and SHR), which remained elevated throughout the restraint period (Fig. 2). After release from restraint, the rats recovered slowly, and heart rate fell to normal levels within 24 hours. As can be seen in Figure 2 and Table 1, in Wistar rats there was no difference in the increase in heart rate between animals treated with vehicle and animals treated with capadenoson at a dose of 0.15 mg/kg (relative increase in heart rate during stress: 18+/−3% in vehicle-treated animals, 15+/−2% in capadenoson-treated animals). In contrast, in SHR we observed a profound blunting of the stress-induced heart rate increase compared to vehicle-treated animals (relative increase in heart rate during stress: 36+/−4% in vehicle-treated animals, 20+/−4% in capadenoson treated animals; p<0.05).
Table 1. Heart rate and blood pressure during physical restraint in Wistar rats and SHR.
| Group | Heart rate (1/min) | MAP (mmHg) | |||||
| baseline | stress | relative change (%) | baseline | stress | relative change (%) | ||
| Wistar | vehicle | 372+/−10 | 432+/−8 | 18+/−3 | 90+/−2 | 104+/−1 | 16+/−2 |
| Capadenoson | 374+/−8 | 427+/−5 | 15+/−2 | 100+/−1 | 116+/−2 | 16+/−2 | |
| SHR | vehicle | 324+/−11 | 438+/−7 | 36+/−4 | 164+/−5 | 189+/−3 | 16+/−12 |
| Capadenoson | 328+/−6 | 391+/−8* | 20+/−4* | 175+/−7 | 189+/−6 | 9+/−10 | |
Values are means +/− SEM. n = 20 for Wistar groups, n = 12 for SHR groups. MAP mean arterial pressure.
*p = 0.001 for comparison of the absolute and relative differences of heart rate during restraint stress in capadenoson-treated vs vehicle-treated SHR.
Figure 2. Telemetry data from Wistar and SHR during restraint experiment.
Shown are the mean heart rate (as percent deviation from resting normal), and mean arterial pressure the day before, and on the day of the experiment. Blue lines depict vehicle-treated animals, green lines capadenoson-treated animals (0.15 mg/kg). Shown on the left side are data from Wistar rats (heart rate, above; MAP, below), on the right side the corresponding values from SHR. Wistar: vehicle and capadenoson each n = 20. SHR: vehicle and capadenoson each n = 12.
During stress, MAP increased in all groups, without any statistical difference between animals treated with vehicle or capadenoson, either in SHR or in Wistar (Fig. 2 and Table 1). However, there was a tendency towards a smaller increase of blood pressure during stress in SHR treated with capadenoson. In SHR, blood pressure was already elevated before the stress experiment, as expected in these animals.
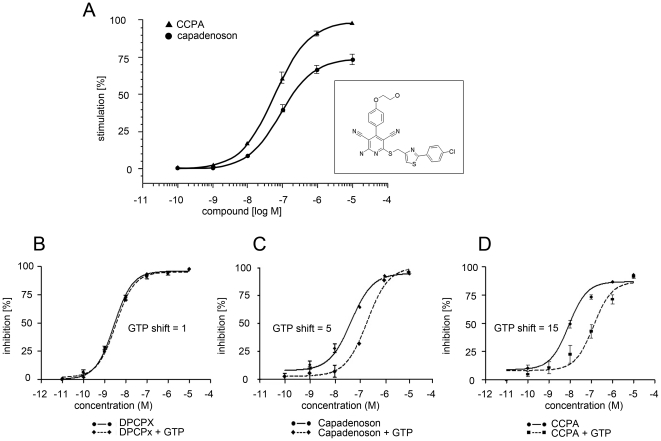
Determination of partial adenosine-A1 agonism of capadenoson
Capadenoson is known to be a selective agonist of adenosine-A1 receptors [16]. To study the binding efficacy of capadenoson to A1 adenosine receptors, we measured ligand dependent G protein activation by binding of [35S]GTPγS to membranes of human brain cortex. CCPA, a well described full agonist of A1 adenosine receptors, was used as control to determine maximal [35S]GTPγS binding. As shown in Fig. 3A, capadenoson stimulated [35S]GTPγS binding only to 74±2% of the full effect of CCPA, suggesting partial agonism.
Figure 3. Capadenoson is a partial adenosine-A1 receptor agonist.
A)Stimulation of [35S]GTPγS binding to human cortex membranes. Shown are means +/− SEM. B) GTP shift assay of the full antagonist DPCPX with and without addition of 1 mM GTP. C) GTP shift assay of the capadenoson, and D) of CCPA, with and without 1 mM GTP. Shown are means +/− SEM. Insert in panel A: Chemical structure of capadenoson.
To further elucidate the pharmacological properties of capadenoson, GTP shift assays were performed with the standard full A1-agonist CCPA and the A1-antagonist 8-cyclopentyl-1,3-dipropylxanthine (DPCPX). CCPA showed a Ki value of 4.2 nM in the binding assay on rat cortical brain membranes (Fig. 3D). In the presence of 1 mM GTP this Ki value shifted to a value of 64 nM. Therefore the GTP shift for CCPA is 15. DPCPX showed a GTP shift of 1 with virtually identical Ki values in the absence and presence of GTP (Fig. 3B). Capadenson showed a Ki value of 24 nM in the binding assay. In the presence of 1 mM GTP this Ki value shifted to a value of 116 nM resulting in a GTP shift of 5 for Capadenoson (Fig. 3C). Therefore capadenoson could be demonstrated to be a partial agonist at the adenosine A1 receptor.
Discussion
In the present study we could demonstrate that the partial adenosine A1-receptor agonist capadenoson leads to a profound reduction of stimulation-induced NE release in vitro as well as to blunted restraint stress-induced tachycardia in SHR, but not in Wistar rats. In a recent phase-II study of the same compound it was noted, that capadenoson specifically blunted the heart rate increase during exercise in a concentration dependent manner [13]. Together, these observations suggest that activation of presynaptic adenosine A1-receptors by a partial agonist may be a route to specifically dampen increases in heart rate caused by a high sympathetic tone.
Because the sympathetic nervous system has a major role in controlling heart rate, the present study was designed to evaluate the effect of capadenoson on the sympathetic tone in detail in an animal model of increased sympathetic activity. An established model in which an activated sympathetic tone plays a major role is the SHR strain, which develops hypertensive blood pressure levels at 5 to 6 weeks of age, followed by cardiac and vascular hypertrophy and ultimately end-organ failure later in life, if the hypertension remains untreated [24]. In SHR, an increased NE overflow from postganglionic nerve terminals has already been shown before [14], [15]. Thus, we chose SHR to study the effects of the novel adenosine-A1 agonist on the regulation of the sympathetic tone, and compared them to the effects in Wistar rats. We hypothesized, that activation of the cardiac adenosine-A1 receptor by capadenoson would reduce stimulation-induced NE release and consequently blunt the heart rate response during physical stress particularly in SHR.
As hypothesized, the stress-induced increase of the heart rate was significantly blunted by capadenoson in SHR. This in vivo effect of capadenoson was paralleled by a significant reduction of NE release upon stimulation in isolated hearts of SHR. The effects of adenosine agonists on norepinephrine release in Wistar rats have been characterized before. Burgdorf et al.[10] showed that activation of adenosine-A1 receptors by CCPA or the non-selective adenosine analogue R(-)N(6)-(2-phenylisopropyl)adenosine (R-PIA) decrease stimulation-induced NE release by about 50%, similar to the effect of CCPA we observed in the present study. Besides an activation of presynaptic A1-receptors, the attenuation of stimulation-induced norepinephrine release in the presence of desipramine as an uptake-1 inhibitor may also be explained by an activated extraneuronal uptake in SHR. [25] However, there is no evidence that capadenosone activates this extraneuronal uptake, whereas the presence of A1-receptors presynaptically is well described. It has been described that the mean concentration of norepinephrine is higher in the right ventricle and ventricular septum of SHR hearts compared with hearts of Wistar rats [26]. However, the functional meaning of the tissue concentration of norepinephrine is not clear, since the adrenergic activation may be more dependent on the release and turnover of norepinephrine as well as on the postsynaptic receptors than on the total amount of norepinephrine in the heart. Agonists of adenosine A2- and A3-receptor subtype seem to play no role in the modulation of cardiac NE release [27]. Adenosine has been shown to exert protective effects during ischemia and reperfusion through its potential to limit the release of norepinephrine[10], and is beneficial in preventing hypertrophic changes under catecholamine stimulation in vitro [28]. Thus, interventions aimed at a specific modulation of cardiac NE release would be highly promising in the treatment of various cardiac diseases, e.g. tachycardia-associated myocardial ischemia. Compared to a selective β1-blockade, a modulation of NE release would avoid the negative inotropic effects on the cardiomyocyte [29], [30].
In the present study we could demonstrate that capadenoson modulates NE release and stress-induced heart rate changes especially in SHR as a model for a high sympathetic tone, while heart rate in Wistar rats was not affected by capadenoson. Heart rate at rest was not affected in either strain. Such a selective attenuation of sympathetic activity as observed in the present study might be explained by the partial agonism of capadenoson on the adenosine-A1 receptor. The lack of effect of a partial agonist, as opposed to the action of a full agonist, on NE release in Wistar rats may be explained by the circumstance that the majority of the presynaptic A1 receptors are already activated by the endogenous full agonist adenosine, resulting in an effective feedback dampening of efferent sympathetic activity. By contrast, the presynaptic A1 receptors may be occupied to a much less extent by adenosine in SHR, which allows for the high sympathetic tone. Under these circumstances, a partial agonist such as capadenoson would be capable to activate unoccupied presynaptic adenosine A1 receptors during states of increased activity (e.g. during restraint stress or during stimulation in the in vitro experiments) at a significantly lower concentration than in Wistar rats. Other possible mechanisms underlying the strain-dependent actions of capadenoson on the stress response and NE release of SHR could be differences in the density or the molecular architecture of adenosine A1 receptors [31], or higher plasma concentrations of adenosine in SHR [32]. In a previous study, a similar effect of a different partial adenosine-A1 agonist, CVT-2759, was noted for the effects of adrenergic stimulation by isoproterenol in guinea pig myocytes. Similar to the present study, the partial adenosine A1 agonist had no effect on basal myocardial function, but attenuated isoproterenol-induced arrhythmias, also in a concentration-dependent manner [33]. Since only female rats were used, the results of the present study are limited to the female sex. Gender differences have been well described for the autonomic control of the cardiovascular system [34]. Therefore, future studies on the effect of capadenosone should taken into account the gender differences in sympathetic control.
In conclusion, we observed a selective reduction of stimulation-induced NE release by the partial adenosine A1-receptor agonist capadenoson in isolated SHR hearts as compared to hearts from Wistar rats. This effect translates into a blunted heart rate increase in vivo upon physical restraint in SHR during adenosine A1 agonism, whereas no effect was observed in Wistar rats. These results suggest that partial adenosine A1 agonism may be a new way to modulate the sympathetic control of cardiac function.
Supporting Information
Norepinephrine release after control stimulation in the absence of pharmacological intervention. The second stimulation was performed 30 minutes after the first one without any pharmacological intervention apart from desipramine (10−7 M) for inhibition of neuronal uptake of norepinephrine. Shown is the ratio of norepinephrine overflow after a first (S1) and second (S2) stimulation. S2/S1 expressed as means +/− SEM, p = ns.
(TIF)
Dose-response curves of capadenoson on mean arterial pressure. A) Dose-response curves of 2 different concentrations in Wistar rats (n = 6 each), and controls. B) Dose-response curves of 4 different concentrations in SHR (n = 12 each), and controls.
(TIF)
Footnotes
Competing Interests: L. Bott-Flügel received travel fees from Bayer Schering Pharma GmbH. H. Ehmke serves as consultant to Bayer Schering Pharma GmbH. K. Zimmermann, A. Knorr, B. Albrecht-Küpper, and R. Kast are employees of Bayer Schering Pharma GmbH. Bayer Schering Pharma provided funding for the in vivo studies and took part in the design, data aquisition and analysis of the in vivo experiments. The principal investigators (L. Bott-Flügel, H. Ehmke, and Melchior Seyfarth) had access to the raw data, and Bayer Schering had no role in the interpretation of the data and decision to publish. The authors declare that funding by Bayer Schering Pharma does not influence their adherence to the PLoS ONE policies on sharing data and materials.
Funding: The in vitro experiments were funded by 1. Medizinische Klinik and Institut für Klinische Chemie und Pathobiochemie, Klinikum rechts der Isar, TU München. Bayer Schering Pharma provided funding for the in vivo studies and took part in the design and data aquisition/analysis of the in vivo experiments. Bayer Schering had no role in data interpretation and decision to publish.
References
- 1.Brodde OE, Michel MC. Adrenergic and muscarinic receptors in the human heart. Pharmacol Rev. 1999;51:651–690. [PubMed] [Google Scholar]
- 2.Prichard BN. Bisoprolol: a new beta-adrenoceptor blocking drug. Eur Heart J . 1987;8(Suppl M):121–129. doi: 10.1093/eurheartj/8.suppl_m.121. [DOI] [PubMed] [Google Scholar]
- 3.Richardt G, Waas W, Kranzhofer R, Cheng B, Lohse MJ, et al. Interaction between the release of adenosine and noradrenaline during sympathetic stimulation: a feed-back mechanism in rat heart. J Mol Cell Cardiol. 1989;21:269–277. doi: 10.1016/0022-2828(89)90742-6. [DOI] [PubMed] [Google Scholar]
- 4.Armah BI, Hofferber E, Stenzel W. General pharmacology of the novel centrally acting antihypertensive agent moxonidine. Arzneimittelforschung. 1988;38:1426–1434. [PubMed] [Google Scholar]
- 5.Head GA, Burke SL, Chan CK. Central imidazoline receptors and centrally acting anti-hypertensive agents. Clin Exp Hypertens. 1997;19:591–605. doi: 10.3109/10641969709083172. [DOI] [PubMed] [Google Scholar]
- 6.Ernsberger P, Haxhiu MA. The I1-imidazoline-binding site is a functional receptor mediating vasodepression via the ventral medulla. Am J Physiol. 1997;273:R1572–1579. doi: 10.1152/ajpregu.1997.273.5.R1572. [DOI] [PubMed] [Google Scholar]
- 7.Guyenet PG. Is the hypotensive effect of clonidine and related drugs due to imidazoline binding sites? Am J Physiol. 1997;273:R1580–1584. doi: 10.1152/ajpregu.1997.273.5.R1580. [DOI] [PubMed] [Google Scholar]
- 8.Szabo B. Imidazoline antihypertensive drugs: a critical review on their mechanism of action. Pharmacol Ther. 2002;93:1–35. doi: 10.1016/s0163-7258(01)00170-x. [DOI] [PubMed] [Google Scholar]
- 9.Hattori Y, Kanno M. Role of alpha1-adrenoceptor subtypes in production of the positive inotropic effects in mammalian myocardium: implications for the alpha1-adrenoceptor subtype distribution. Life Sci. 1998;62:1449–1453. doi: 10.1016/s0024-3205(98)00088-5. [DOI] [PubMed] [Google Scholar]
- 10.Burgdorf C, Richardt D, Kurz T, Seyfarth M, Jain D, et al. Adenosine inhibits norepinephrine release in the postischemic rat heart: the mechanism of neuronal stunning. Cardiovasc Res. 2001;49:713–720. doi: 10.1016/s0008-6363(00)00309-6. [DOI] [PubMed] [Google Scholar]
- 11.Seyfarth M, Feng Y, Hagl S, Sebening F, Richardt G, et al. Effect of myocardial ischemia on stimulation-evoked noradrenaline release. Modulated neurotransmission in rat, guinea pig, and human cardiac tissue. Circ Res. 1993;73:496–502. doi: 10.1161/01.res.73.3.496. [DOI] [PubMed] [Google Scholar]
- 12.Elzein E, Zablocki J. A1 adenosine receptor agonists and their potential therapeutic applications. Expert Opin Investig Drugs. 2008;17:1901–1910. doi: 10.1517/13543780802497284. [DOI] [PubMed] [Google Scholar]
- 13.Tendera M, Sosnowski M, Gaszewska-Zurek E, Parma Z, Neuser D, et al. The oral adenosine A1 receptor agonist, BAY68-4986, reduces heart rate at peak exercise in patients with chronic stable angina. J Am Coll Cardiol 49: A. 2007;232 [Google Scholar]
- 14.Zsoter TT, Wolchinsky C, Lawrin M, Sirko S. Norepinephrine release in arteries of spontaneously hypertensive rats. Clin Exp Hypertens A. 1982;4:431–444. doi: 10.3109/10641968209060753. [DOI] [PubMed] [Google Scholar]
- 15.Zugck C, Lossnitzer D, Backs J, Kristen A, Kinscherf R, et al. Increased cardiac norepinephrine release in spontaneously hypertensive rats: role of presynaptic alpha-2A adrenoceptors. J Hypertens. 2003;21:1363–1369. doi: 10.1097/00004872-200307000-00026. [DOI] [PubMed] [Google Scholar]
- 16.Nell P, Albrecht-Küpper B. Lawton G, Witty DR, editors. The Adenosine A1 Receptor and its Ligands. Progress in Medicinal Chemistry: Elsevier. 2009. pp. 164–201. [DOI] [PubMed]
- 17.Elworthy PM, Hitchcock ER. Estimation of plasma catecholamines by high-performance liquid chromatography with electrochemical detection in patients with subarachnoid haemorrhage. J Chromatogr. 1986;380:33–41. doi: 10.1016/s0378-4347(00)83622-1. [DOI] [PubMed] [Google Scholar]
- 18.McDougall SJ, Paull JR, Widdop RE, Lawrence AJ. Restraint stress : differential cardiovascular responses in Wistar-Kyoto and spontaneously hypertensive rats. Hypertension. 2000;35:126–129. doi: 10.1161/01.hyp.35.1.126. [DOI] [PubMed] [Google Scholar]
- 19.Lorenzen A, Fuss M, Vogt H, Schwabe U. Measurement of guanine nucleotide-binding protein activation by A1 adenosine receptor agonists in bovine brain membranes: stimulation of guanosine-5′-O-(3-[35S]thio)triphosphate binding. Mol Pharmacol. 1993;44:115–123. [PubMed] [Google Scholar]
- 20.Lorenzen A, Guerra L, Vogt H, Schwabe U. Interaction of full and partial agonists of the A1 adenosine receptor with receptor/G protein complexes in rat brain membranes. Mol Pharmacol. 1996;49:915–926. [PubMed] [Google Scholar]
- 21.Lohse MJ, Lenschow V, Schwabe U. Interaction of barbiturates with adenosine receptors in rat brain. Naunyn Schmiedebergs Arch Pharmacol. 1984;326:69–74. doi: 10.1007/BF00518781. [DOI] [PubMed] [Google Scholar]
- 22.Lohse MJ, Klotz KN, Lindenborn-Fotinos J, Reddington M, Schwabe U, et al. 8-Cyclopentyl-1,3-dipropylxanthine (DPCPX)–a selective high affinity antagonist radioligand for A1 adenosine receptors. Naunyn Schmiedebergs Arch Pharmacol. 1987;336:204–210. doi: 10.1007/BF00165806. [DOI] [PubMed] [Google Scholar]
- 23.Van der Wenden EM, Hartog-Witte HR, Roelen HC, von Frijtag Drabbe Kunzel JK, Pirovano IM, et al. 8-substituted adenosine and theophylline-7-riboside analogues as potential partial agonists for the adenosine A1 receptor. Eur J Pharmacol. 1995;290:189–199. doi: 10.1016/0922-4106(95)00064-x. [DOI] [PubMed] [Google Scholar]
- 24.Conrad CH, Brooks WW, Hayes JA, Sen S, Robinson KG, et al. Myocardial fibrosis and stiffness with hypertrophy and heart failure in the spontaneously hypertensive rat. Circulation. 1995;91:161–170. doi: 10.1161/01.cir.91.1.161. [DOI] [PubMed] [Google Scholar]
- 25.Grundemann D, Koschker AC, Haag C, Honold C, Zimmermann T, et al. Activation of the extraneuronal monoamine transporter (EMT) from rat expressed in 293 cells. Br J Pharmacol. 2002;137:910–918. doi: 10.1038/sj.bjp.0704926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tsuboi H, Ohno O, Ogawa K, Ito T, Hashimoto H, et al. Acetylcholine and norepinephrine concentrations in the heart of spontaneously hypertensive rats: a parasympathetic role in hypertension. J Hypertens. 1987;5:323–330. doi: 10.1097/00004872-198706000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Lorbar M, Chung ES, Nabi A, Skalova K, Fenton RA, et al. Receptors subtypes involved in adenosine-mediated modulation of norepinephrine release from cardiac nerve terminals. Can J Physiol Pharmacol. 2004;82:1026–1031. doi: 10.1139/y04-108. [DOI] [PubMed] [Google Scholar]
- 28.Gan XT, Rajapurohitam V, Haist JV, Chidiac P, Cook MA, et al. Inhibition of phenylephrine-induced cardiomyocyte hypertrophy by activation of multiple adenosine receptor subtypes. J Pharmacol Exp Ther. 2005;312:27–34. doi: 10.1124/jpet.104.073122. [DOI] [PubMed] [Google Scholar]
- 29.Packer M, Lee WH, Kessler PD, Gottlieb SS, Bernstein JL, et al. Role of neurohormonal mechanisms in determining survival in patients with severe chronic heart failure. Circulation. 1987;75:IV80–92. [PubMed] [Google Scholar]
- 30.Persson H, Andreasson K, Kahan T, Eriksson SV, Tidgren B, et al. Neurohormonal activation in heart failure after acute myocardial infarction treated with beta-receptor antagonists. Eur J Heart Fail. 2002;4:73–82. doi: 10.1016/s1388-9842(01)00196-9. [DOI] [PubMed] [Google Scholar]
- 31.Kobayashi S, Umemura S, Toya Y, Hirawa N, Hayashi S, et al. Adenosine A1 receptor and its gene expression in ventricles from spontaneously hypertensive rats. Am J Physiol. 1996;271:R704–709. doi: 10.1152/ajpregu.1996.271.3.R704. [DOI] [PubMed] [Google Scholar]
- 32.Yamada K, Goto A, Ishii M, Yoshioka M, Matsuoka H, et al. Plasma adenosine concentrations are elevated in conscious spontaneously hypertensive rats. Clin Exp Pharmacol Physiol. 1992;19:563–567. doi: 10.1111/j.1440-1681.1992.tb00505.x. [DOI] [PubMed] [Google Scholar]
- 33.Song Y, Wu L, Shryock JC, Belardinelli L. Selective attenuation of isoproterenol-stimulated arrhythmic activity by a partial agonist of adenosine A1 receptor. Circulation. 2002;105:118–123. doi: 10.1161/hc0102.101392. [DOI] [PubMed] [Google Scholar]
- 34.Dart AM, Du XJ, Kingwell BA. Gender, sex hormones and autonomic nervous control of the cardiovascular system. Cardiovasc Res. 2002;53:678–687. doi: 10.1016/s0008-6363(01)00508-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Norepinephrine release after control stimulation in the absence of pharmacological intervention. The second stimulation was performed 30 minutes after the first one without any pharmacological intervention apart from desipramine (10−7 M) for inhibition of neuronal uptake of norepinephrine. Shown is the ratio of norepinephrine overflow after a first (S1) and second (S2) stimulation. S2/S1 expressed as means +/− SEM, p = ns.
(TIF)
Dose-response curves of capadenoson on mean arterial pressure. A) Dose-response curves of 2 different concentrations in Wistar rats (n = 6 each), and controls. B) Dose-response curves of 4 different concentrations in SHR (n = 12 each), and controls.
(TIF)