Abstract
Background:
This cross-sectional survey assessed the adequacy of ophthalmology teaching in undergraduate medical education and evaluated the comfort level of family medicine residents in diagnosing and managing common ophthalmic conditions.
Methods:
Postgraduate year 1 and 2 family medicine residents at the University of Western Ontario were recruited for this study. The main outcome measures were hours of classroom and clinic-based instruction on ophthalmology during undergraduate medical education, and the comfort level in ophthalmic clinical skills and managing various ophthalmic conditions.
Results:
In total, 54 (33.3%) of 162 family medicine residents responded to the survey. Residents reported an average of 27.1 ± 35.1 hours and 39.8 ± 47.1 hours of classroom and clinical ophthalmology instruction, respectively. However, most residents (80%) responded as feeling only “somewhat comfortable” or “not at all comfortable” in assessing and managing common ophthalmic conditions, including ocular emergencies, such as acute angle closure glaucoma and ocular chemical burn. A positive correlation was seen between overall comfort level and hours of classroom instruction (P < 0.05).
Conclusion:
The number of hours of ophthalmology training received by family medicine residents during medical school meets the International Council of Ophthalmology Task Force recommendations. However, family medicine residents appear to be uncomfortable in handling treatable but potentially sight-threatening ocular conditions. Standardizing the undergraduate medical education ophthalmology curriculum and increasing hours of ophthalmology training during postgraduate family medicine residency may be useful in bridging this gap in knowledge.
Keywords: medical education, ophthalmology, needs assessment, primary care
Introduction
Ophthalmic conditions are common in primary care practice.1 Eye signs and symptoms are often the first recognized presentation of common systemic conditions, such as diabetes and hypertension. While many conditions affecting the eye can be treated, irreversible damage can occur if they are left unrecognized (eg, diabetic retinopathy, glaucoma).2 Despite the prevalence of such conditions, little time is devoted to ophthalmic training in undergraduate medical education.3 A recent study revealed that Canada does not have a standardized undergraduate medical education curriculum for medical schools, and that many residents of various specialties report not having confidence in managing ophthalmological cases.5
Prior studies have shown that Canadian medical students are not comfortable with ophthalmic clinical skills, such as the use of an ophthalmoscope.4,5 A recent study at a public medical school in California demonstrated that 26% of graduating students were “not at all comfortable” with performing screening eye examinations and that 57% were very interested in a skills refresher course in the future.6 This is consistent with a 1995 study which reported that, according to estimation by US primary care program directors, less than 50% of residents have adequate ophthalmic skills at the start of residency, despite 85% feeling that skills like a screening eye examination should be mastered during medical school.3 These findings support the importance of adequate undergraduate ophthalmology training.7–12
These studies suggest that medical students receive too little ophthalmic training and advocate increasing the exposure to ophthalmic knowledge and skills within the undergraduate medical education curriculum. The primary goal of our study was to quantify the adequacy of ophthalmic education for medical school graduates in training to be primary care physicians. Our study also aimed to highlight the ophthalmic training requirements of general family practitioners, and propose necessary changes to the Canadian medical school curricula accordingly.
Methods
An 85-item cross-sectional survey questionnaire was used in this study. Approval was granted by the University of Western Ontario Research Ethics Board. All current family medicine residents training at the University of Western Ontario, including those in postgraduate year (PGY) 1 and 2, were invited to participate in the study. Participants were excluded if they had previously applied to or been enrolled in an ophthalmology residency program. Informed consent was provided by all participants.
Using a paper-based questionnaire (see Appendix 1), subjects were asked to provide information on the following: year of postgraduate training in family medicine residency, country of origin of medical school prior to residency, number of hours of classroom or clinical exposure to ophthalmology during undergraduate medical education, as well as percentage of rotation time involving exposure to ophthalmological conditions during family medicine residency.
Subjects were also asked to rate their comfort with respect to managing specific ophthalmology conditions and performing specific ophthalmic clinical skills on a Likert scale from 1–5 (1 = not comfortable at all; 2 = somewhat comfortable; 3 = moderately comfortable; 4 = comfortable; 5 = very comfortable). The conditions and skills asked about in the questionnaire were based on the topics covered in the undergraduate medical education ophthalmology reference text published by the American Academy of Ophthalmology.13
Statistical analysis
Descriptive statistics were generated using Microsoft Excel (Microsoft Corporation, Redmond, WA) and SAS software (SAS Institute, Cary, NC). Mann–Whitney U test was used to compare means between groups. The Spearman correlation test was performed to identify if there was an association between comfort level and number of hours of ophthalmology education in undergraduate medical education. A P value of less than 0.05 was considered statistically significant.
Results
Of the 162 family medicine residents in PGY 1 and 2 at the University of Western Ontario, 54 (33.3%) volunteered to participate in the study. No participant met the exclusion criteria. None of the completed surveys showed identical responses for all items. A summary of the demographic data is shown in Table 1.
Table 1.
Demographic data on participants
| Total | PGY-1 | PGY-2 | |
|---|---|---|---|
| UWO family medicine residents | 162 | 68 | 94 |
| Completed questionnaire | 54 | 35 (64.8%) | 19 (35.2%) |
| CMGsa | 32 | 23 (71.9%) | 9 (28.1%) |
| IMGs | 22 | 12 (54.5%) | 10 (45.5%) |
Notes: Percentages are expressed out of the total in first column.
Canadian medical school representation: UWO (n = 15), McMaster (n = 7), Toronto (n = 4), Manitoba (n = 2), McGill (n = 2), Queens (n = 1), Calgary (n = 1).
Abbreviations: CMGs, Canadian medical graduates; IMGs, international medical graduates; PGY, postgraduate year; UWO, University of Western Ontario.
Amount of undergraduate ophthalmology teaching
There was a large variation in the amount of classroom-based (range 0–200 hours) and clinic-based (range 0–300 hours) ophthalmology teaching during medical school. Overall, it appears that international medical graduates received more ophthalmology instruction than Canadian medical graduates (P < 0.05, Table 2).
Table 2.
Hours of instruction during undergraduate medical education
| Classroom-based instruction | Clinic-based instruction | |
|---|---|---|
| All respondents | 27.1 (35.1) | 39.8 (47.1) |
| PGY-1/PGY-2 | 23.5 (26.0)/33.4 (47.4) | 33.0 (27.2)/51.6 (68.8) |
| CMGs/IMGs | 17.5 (18.5)/44.1 (49.4)a | 30.5 (53.4)/55.8 (28.6)a |
Notes: Data reported as mean (standard deviation).
P < 0.05 by Mann–Whitney U test.
Abbreviations: CMGs, Canadian medical graduates; IMGs, international medical graduates; PGY, postgraduate year.
Overall comfort in managing ophthalmological conditions
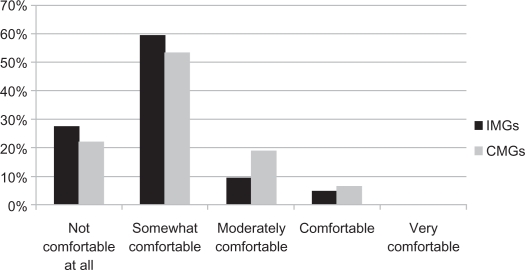
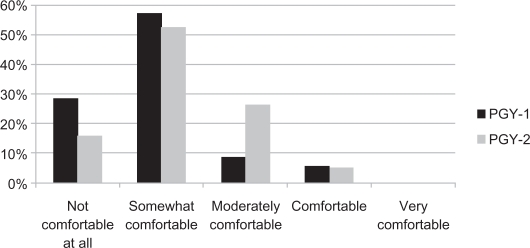
The subjects reported that, on average, 6.3% ± 9.2% of their postgraduate rotations in family medicine involve exposure to eye-related cases (6.9% ± 10.6% for PGY 1, 5.3% ± 5.7% for PGY 2). Eighty percent of subjects reported that they were either “somewhat comfortable” or “not comfortable at all” in dealing with ophthalmology-associated conditions. Very few subjects felt “moderately comfortable” (14.8% overall) or “comfortable” (5.6% overall). No subject reported being “very comfortable” with ophthalmology-associated issues (Figures 1 and 2). There was no statistically significant difference in average comfort level rating from the Likert scale between PGY 1 and PGY 2 (1.9 ± 0.8 and 2.2 ± 0.8, respectively) and between Canadian medical graduates and international medical graduates (1.9 ± 0.8 and 2.1 ± 0.8, respectively).
Figure 1.
Distribution of comfort level in managing ophthalmology cases.
Abbreviations: CMGs, Canadian medical graduates; IMGs, international medical graduates.
Figure 2.
Distribution of comfort level in managing ophthalmology cases (PGY 1 and 2).
Abbreviation: PGY, postgraduate year.
Hours of instruction versus comfort level
The Spearman correlation revealed a moderately positive correlation between the hours of classroom instruction received during undergraduate medical education and overall comfort in managing ophthalmology cases (P = 0.0012). The hours of clinic instruction alone and combined classroom and clinic instruction revealed small positive correlations, albeit not statistically significant (Table 3).
Table 3.
Correlation between comfort level and amount of ophthalmology instruction during undergraduate medical education
| Variables | Spearman’s correlation coefficient | P-value |
|---|---|---|
| Hours of classroom-setting instruction & comfort level | 0.45 (moderate) | 0.0012 |
| Hours of clinic-setting instruction & comfort level | 0.13 (small) | 0.37 |
| Total hours of instruction & comfort level | 0.26 (small) | 0.067 |
Management of specific ophthalmic conditions and ophthalmic clinical skills
There was a wide variation in the comfort level of family medicine residents in managing different ophthalmologic conditions (Table 4), as well as in performing relevant ophthalmic clinical skills (Table 5). When comparing the responses of both PGY 1 and PGY 2 in managing or coordinating care of ophthalmology-related issues, the median score differed for 22 of the 52 items. PGY 1 residents had a higher median score in 16 of all items, and PGY 2 residents higher in six items (Table 4). When asked about their comfort level surrounding various ophthalmologic procedures, the median scores between PGY 1 and PGY 2 differed in 8 of 21 items. PGY 1 residents scored higher in three of all items, whereas PGY 2 residents scored higher in five items (Table 5).
Table 4.
Median response for management of specific ophthalmic conditions
| All (n = 54) | CMGs (n = 32) | IMGs (n = 22) | PGY-1 (n = 32) | PGY-2 (n = 22) | |
|---|---|---|---|---|---|
| Orbit/lacrimal apparatus/lids/lashes | |||||
| Proptosis | 2 | 2 | 1 | 3 | 1 |
| Orbital Cellulitis | 3 | 3 | 3 | 3 | 3 |
| Ptosis | 2 | 3 | 2 | 3 | 2 |
| Preseptal cellulitis | 2 | 2 | 2 | 2 | 2 |
| Chalazion/stye | 3 | 3 | 3 | 3 | 4 |
| Blepharitis | 3 | 3 | 3 | 3 | 4 |
| Conjunctiva/sclera | |||||
| Dry eyes | 4 | 3 | 4 | 3 | 4 |
| Conjunctival lesions (eg, laceration/abrasion/nodule) | 3 | 3 | 3 | 3.5 | 3 |
| Conjunctivitis | 4 | 4 | 4 | 4 | 4 |
| Episcleritis/scleritis | 3 | 2.5 | 3 | 3 | 3 |
| Subconjunctival hemorrhage | 3 | 3 | 4 | 3 | 4 |
| Cornea | |||||
| Corneal abrasion | 3 | 4 | 3 | 3 | 4 |
| Corneal ulcer | 2 | 2 | 2 | 3 | 2 |
| Herpetic keratitis (HSV/HZV) | 2 | 2 | 2 | 2.5 | 2 |
| Recurrent corneal erosions | 2 | 2 | 2 | 2 | 1 |
| Corneal foreign body/rust ring | 3 | 3 | 2 | 3 | 2 |
| Contact lens related issues | 3 | 3 | 2 | 3 | 3 |
| Neuro-ophthalmology | |||||
| Anisocoria | 2 | 2 | 2 | 2 | 2 |
| Relative afferent papillary defect | 2 | 2 | 2 | 2 | 2 |
| Visual field defects | 2 | 2 | 2 | 2 | 2 |
| Diplopia | 2 | 2.5 | 2 | 2 | 2 |
| Optic disc edema | 2 | 2 | 2 | 2 | 2 |
| Optic neuritis | 1 | 2 | 1 | 2 | 1 |
| Arteritic ischemic optic neuropathy/giant cell arteritis | 2 | 2.5 | 1 | 2 | 2 |
| Uveal tract | |||||
| Iritis | 2 | 2 | 1 | 2 | 2 |
| Pediatric ophthalmology | |||||
| Strabismus | 2 | 2 | 3 | 2 | 2 |
| Leukocoria | 2 | 2 | 1 | 2 | 2 |
| Amblyopia | 2 | 2 | 2 | 2 | 2 |
| Lens | |||||
| Cataract | 3 | 3 | 3 | 3 | 3 |
| Retina and vitreous | |||||
| Posterior vitreous detachment | 2 | 2 | 1 | 2 | 1 |
| Vitreous hemorrhage | 2 | 2 | 2 | 2 | 2 |
| Central retinal artery/vein occlusion | 1.5 | 1 | 2 | 2 | 2 |
| Age-related macular degeneration | 2 | 2 | 2 | 2 | 2 |
| Retinal detachment | 2 | 2 | 1 | 2 | 2 |
| Glaucoma | |||||
| Primary open angle glaucoma | 2 | 2 | 2 | 2.5 | 2 |
| Acute angle closure glaucoma | 2 | 2 | 2 | 2 | 2 |
| Ocular manifestations of systemic disease | |||||
| Thyroid ophthalmopathy | 3 | 3 | 3 | 2.5 | 3 |
| Diabetic retinopathy | 3 | 3 | 3 | 3 | 3 |
| Hypertensive retinopathy | 3 | 3 | 3 | 3 | 3 |
| Amaurosis fugax | 2 | 3 | 2 | 2.5 | 2 |
| Myasthenia gravis | 2 | 2 | 2 | 2.5 | 2 |
| Autoimmune diseases (eg, RA, Lupus, Sjogren’s, HLA-B27) | 2 | 2 | 2 | 2 | 2 |
| Migraine | 3 | 3 | 3 | 3 | 3 |
| Ocular trauma/emergencies | |||||
| Globe rupture/intraocular foreign bodies | 1 | 2 | 1 | 2 | 1 |
| Chemical burn | 2 | 2 | 1 | 2 | 2 |
| Hyphema | 2 | 2 | 1 | 2 | 2 |
| Blow out fractures | 1.5 | 2 | 1 | 2 | 1 |
| Endophthalmitis | 1 | 2 | 1 | 2 | 1 |
| Medications | |||||
| Topical NSAIDS | 2 | 2 | 2 | 2 | 2 |
| Topical steroids | 2 | 2 | 2 | 2 | 2 |
| Anti-glaucoma medications | 2 | 2 | 2 | 3 | 2 |
| Topical anti-infective medications | 3 | 3 | 3 | 3 | 3 |
Note: Based on a Likert scale from 1–5 (1 = not comfortable at all; 2 = somewhat comfortable; 3 = moderately comfortable; 4 = comfortable; 5 = very comfortable).
Abbreviations: CMGs, Canadian medical graduates; IMGs, international medical graduates; PGY, postgraduate year.
Table 5.
Median response for ophthalmic clinical skills
| All (n = 54) | CMGs (n = 32) | IMGs (n = 22) | PGY-1 (n = 32) | PGY-2 (n = 22) | |
|---|---|---|---|---|---|
| Clinical assessment – history and physical | |||||
| Ophthalmological history-taking | 4 | 4 | 4 | 4 | 4 |
| Visual acuity | 4 | 4 | 4 | 4 | 4 |
| Pupil examination/swinging flash light test | 4 | 4 | 4 | 4 | 4 |
| Cover-uncover test/alternate cover test | 4 | 4 | 4 | 4 | 4 |
| Colour vision testing | 3 | 3 | 4 | 3 | 3 |
| Visual field | 4 | 4 | 4 | 4 | 4 |
| Interpretation of fluorescein staining | 4 | 4 | 3 | 4 | 4 |
| Direct ophthalmoscope | 3 | 3 | 3 | 3 | 3 |
| Tonometry (intra-ocular pressure) | 2 | 2 | 2 | 2 | 2 |
| Extra-ocular movements | 4 | 5 | 5 | 4 | 5 |
| Investigations | |||||
| Ordering/interpretation of bloodwork (including CBC, ESR, C-reactive protein) | 4 | 4 | 4 | 4 | 4 |
| Orbital CT scan | 3 | 3 | 3 | 2 | 3 |
| Carotid Doppler ultrasound | 3 | 3 | 3 | 3 | 3 |
| Echocardiogram | 3 | 3 | 4 | 3 | 4 |
| Medical/surgical referral, counseling and care | |||||
| Prescription of topical antibiotics | 4 | 4 | 4 | 4 | 4 |
| Prescription of topical steroids | 3 | 3 | 3 | 3 | 2 |
| Prescription of anti-glaucoma medications | 2 | 2.5 | 2 | 3 | 2 |
| Indications for ophthalmology referral | 3 | 3 | 3 | 3 | 3 |
| Indications and contraindications for certain surgical procedures | 2 | 2 | 3 | 2 | 3 |
| Preparation of patients for surgery and post-operative care | 3 | 3 | 3 | 2 | 3 |
| Explanations of common ophthalmological surgical procedures (eg, cataract surgery, vitrectomy) | 2 | 2 | 3 | 2.5 | 2 |
Note: Based on a Likert scale from 1–5 (1 = not comfortable at all; 2 = somewhat comfortable; 3 = moderately comfortable; 4 = comfortable; 5 = very comfortable).
Abbreviations: CMGs, Canadian medical graduates; IMGs, international medical graduates; PGY, postgraduate year.
Discussion
We were able to achieve a response rate of 33.3% from the entire study population, ie, 54 of 162 University of Western Ontario Family Medicine residents. There was good representation of both Canadian medical graduates (n = 32) and international medical graduates (n = 22), as well as from both PGY 1 (n = 35) and PGY 2 (n = 19) years of residency. Seven Canadian medical schools were represented among the study population.
The International Council of Ophthalmology provides guidance to increase ophthalmology training in medical schools. It recommends 40–60 hours of ophthalmology exposure during undergraduate medical education.11 Nonetheless, a recent survey by Welch and Eckstein revealed that medical schools in the UK did not comply with the recommended ophthalmology curriculum set out by the International Council of Ophthalmology.14
Compared with the International Council of Ophthalmology Task Force recommendation of 40–60 hours,11 our study participants received a satisfactory number of hours of both classroom-based (27.1 ± 35.1 hours) and clinic-based ophthalmology instruction (39.8 ± 47.1 hours). However, there was a wide variation in the hours of instruction reported, as reflected by the large standard deviations. Residents received from 0–200 hours of classroom instruction and 0–300 hours of clinic-based instruction on ophthalmology during medical school. This implies that some residents received instruction falling short of the task force recommendation. International medical graduates reported a higher amount of ophthalmologic instruction when compared with Canadian medical graduates, although there was no significant difference in the average level of comfort in managing ophthalmic diseases between the two groups. Our data suggest the need for standardizing the amount of ophthalmology instruction in undergraduate medical education.
Despite the amount of ophthalmology instruction in undergraduate medical education meeting the International Council of Ophthalmology recommendations, most (80%) of the residents in our study felt only “somewhat comfortable” or “not comfortable at all” in managing ophthalmology conditions. With the exception of dry eyes and conjunctivitis, residents felt “moderately comfortable” or less in managing all the specific conditions in our questionnaire. While it may be understandable that residents are not comfortable with all ocular conditions, there are certain diseases with which family medicine physicians should be familiar. For example, the Medical Council of Canada lists strabismus, pupil abnormalities, and eye redness among its learning objectives for medical students.15 Although residents felt comfortable in managing red eye, they only felt “somewhat comfortable” with relative afferent papillary defects, strabismus, and amblyopia. Other conditions which often threaten sight in the emergency setting, such as orbital cellulitis, corneal ulcer, acute angle closure glaucoma, ocular chemical burn, and ischemic optic neuropathy secondary to giant cell arteritis, also had low median scores. All of these diseases and presenting problems are important to recognize, owing to the high risk of vision loss and diminished quality of life.
Residents reported feeling comfortable with performing the ophthalmologic examination. Of the 21 ophthalmologic skills or procedures asked about, they reported feeling “comfortable” with nine of them and “moderately comfortable” with another eight. They reported feeling “somewhat comfortable” in four specific areas, ie, tonometry, prescription of antiglaucoma medications, indications and contraindications for surgical procedures, and explaining common ophthalmological surgical procedures. Emphasis should be placed on getting family medicine residents more familiar and comfortable with using a tonometer, because one of the important learning objectives of the College of Family Physicians of Canada is to perform a focused examination and investigations to evaluate a red eye, including the measurement and evaluation of intraocular pressure.16
A similar study assessing the comfort level of Canadian family medicine residents with conditions pertaining to otolaryngology/head and neck surgery also revealed low levels of comfort for important conditions and procedures.17 Our results reflect the same phenomenon, ie, primary care trainees are not fully comfortable with assessing or managing some of the commonly encountered subspecialty conditions which often require acute management.
When comparing the different modes of instruction (classroom versus clinic), we found that classroom-based instruction had a positive effect on raising comfort in managing ophthalmological cases. Perhaps by standardizing and enriching the undergraduate medical education ophthalmology curriculum in medical schools, or by increasing the percentage of ophthalmology teaching during residency, trainees will be more confident in handling eye-related cases in the primary care setting. Medical schools may consider utilizing innovative methods of education, such as computer-assisted or web-based learning, which has shown promising effectiveness in subspecialty training.18 Further studies will have to be conducted to validate newer approaches to knowledge transfer in medical education.
The questionnaire was administered to residents approximately 1–2 years following the conclusion of their undergraduate medical training. Potential exists for recall bias for responses regarding past undergraduate medical education. However, the responses were consistent with previous studies of undergraduate medical education ophthalmology training in other countries, which suggests validity of the results.3,4,6 Our sample was limited in that it represented a selection of residents from a single postgraduate institution, although there was representation of graduates from a broad spectrum of domestic and international medical schools. It would be interesting to compare the level of comfort of residents in different family medicine residency programs.
Conclusion
Despite having received an adequate number of hours of ophthalmological instruction according to recommendations by the International Council of Ophthalmology, family medicine residents lack comfort in managing ophthalmic conditions. Many of these conditions are common and could result in loss of vision if not treated properly, including cataracts, strabismus, pupil abnormalities, acute angle closure glaucoma, and giant cell arteritis. These specific conditions should be the focus of educational interventions, such as lectures, computer-assisted learning, continuing medical education, and refresher courses.
Our study reinforces the need for standardized ophthalmological education across Canadian medical schools. There was wide variance in self-reported number of hours of instruction. Furthermore, some residents in our study reported having received an inadequate amount of ophthalmological training during their undergraduate medical education. Standardizing undergraduate ophthalmology training in Canada will ensure that medical students are graduating with adequate exposure to the subspecialty.5
As primary care practitioners, family physicians play an important role in managing patients with ocular conditions. Given the rising number of elderly patients, focus needs to be placed on training all physicians, including family physicians, to be aware of signs and symptoms of conditions that can lead to vision loss.19 Raising family physicians’ comfort level with ocular conditions will help facilitate the prompt management of ocular conditions and appropriate referrals to ophthalmologists. Standardizing undergraduate ophthalmology training and using effective teaching methods tailored towards primary care should help raise the comfort level of family physicians. More research is needed to evaluate various educational interventions and their effectiveness in increasing comfort in managing and referring ocular conditions.
Appendix.
Appendix 1 Ophthalmology in family medicine questionnaire for family medicine residents.
At what medical school are you currently pursuing your residency? ________________
- What year of residency are you presently in?
- □ PGY 1 □ PGY 2 □ PGY 3+
- Have you ever applied to a postgraduate training program in ophthalmology?
- □ Yes □ No
- Have you ever been trained in a dedicated ophthalmology postgraduate training program outside of your regular curriculum?
- □ Yes □ No
- Have you ever worked as an ophthalmologist (within Canada or abroad)?
- □ Yes □ No
- Please indicate which medical school you attended prior to beginning this residency:
- School name: ______________________________
- City: ______________________________
- Province: ______________________________
- Country: ______________________________
- How many hours of classroom-based ophthalmology instruction did you receive during medical school?
- _____hours
- How many total hours of clinical ophthalmology instruction did you receive during medical school (ie, through observerships, clerkship, electives, etc)?
- _____hours
- What percentage of your family medicine rotations can be classified as managing ophthalmology-associated issues (eg, acute red eye, floaters, etc)
- ______%
- How comfortable do you feel managing ophthalmology associated issues?
□ not comfortable at al □ somewhat comfortable □ moderately comfortable □ comfortable □ very comfortable -
Using the table below, please indicate how comfortable you feel managing/coordinating the care for these issues based on your present knowledge:
(1 = not at all comfortable, 2 = somewhat comfortable, 3 = moderately comfortable, 4 = comfortable, 5 = very comfortable)Orbit/lacrimal apparatus/lids/lashes 1 2 3 4 5 Proptosis Orbital cellulites Ptosis Preseptal cellulites Chalazion/stye Blepharitis Conjunctiva/sclera Dry eyes Conjunctival lesions (eg, laceration/abrasion/nodule) Conjunctivitis Episcleritis/scleritis Subconjunctival hemorrhage Cornea Corneal abrasion Corneal ulcer Herpetic keratitis (herpes simplex or zoster virus) Recurrent corneal erosions Corneal foreign body/rust ring Contact lens-related issues Neuro-ophthalmology Anisocoria Relative afferent papillary defect Visual field defects Diplopia Optic disc edema Optic neuritis Arteritic ischemic optic neuropathy/giant cell arteritis Uveal tract Iritis Pediatric ophthalmology Strabismus Leukocoria Amblyopia Lens Cataract Retina and vitreous Posterior vitreous detachment Vitreous hemorrhage Central retinal artery/vein occlusion Age-related macular degeneration Retinal detachment Glaucoma Primary open angle glaucoma Acute angle closure glaucoma Ocular manifestations of systemic disease Thyroid ophthalmopathy Diabetic retinopathy Hypertensive retinopathy Amaurosis fugax Myasthenia gravis Autoimmune diseases (eg, rheumatoid arthritis, lupus, Sjogren’s, HLA-B27) Migraine Ocular trauma/emergencies Globe rupture/intraocular foreign bodies Chemical burn Hyphema Blowout fractures Endophthalmitis Medications Topical nonsteroidal anti-inflammatory drugs Topical steroids Antiglaucoma medications Topical anti-infective medications -
Using the table below, please indicate how comfortable you feel performing the following ophthalmology-related skills:
(1 = not at all comfortable, 2 = somewhat comfortable, 3 = moderately comfortable, 4 = comfortable, 5 = very comfortable)Clinical assessment – history and physical 1 2 3 4 5 Ophthalmological history-taking Visual acuity Pupil examination/swinging flash light test Cover-uncover test/alternate cover test Color vision testing Visual field Interpretation of fluorescein staining Direct ophthalmoscopy Tonometry (intraocular pressure) Extraocular movements Investigations Ordering/interpretation of bloodwork including full blood count, ESR, C-reactive protein Orbital computed tomography scan Carotid Doppler ultrasound Echocardiogram Medical/surgical referral, counseling, and care Prescription of topical antibiotics Prescription of topical steroids Prescription of antiglaucoma medications Indications for ophthalmology referral Indications and contraindications for certain surgical procedures Preparation of patients for surgery and postoperative care Explanations of common ophthalmological surgical procedures (eg, cataract surgery, vitrectomy)
This is the end of the questionnaire. Thank you for taking the time to complete our survey.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Dart J. Eye disease at a community health centre. BMJ. 1986;293:1477–1480. doi: 10.1136/bmj.293.6560.1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sheldrick JH, Sharp A. Glaucoma screening clinic in general practice: Prevalence of occult disease, and resource implications. Br J Gen Pract. 1994;44:561–565. [PMC free article] [PubMed] [Google Scholar]
- 3.Stern GA. Teaching ophthalmology to primary care physicians. The Association of University Professors of Ophthalmology Education Committee. Arch Ophthalmol. 1995;113:722–724. doi: 10.1001/archopht.1995.01100060048029. [DOI] [PubMed] [Google Scholar]
- 4.Gupta RR, Lam WC. Medical students’ self-confidence in performing direct ophthalmoscopy in clinical training. Can J Ophthalmol. 2006;41:169–174. doi: 10.1139/I06-004. [DOI] [PubMed] [Google Scholar]
- 5.Noble J, Somal K, Gill HS, Lam WC. An analysis of undergraduate ophthalmology training in Canada. Can J Ophthalmol. 2009;4:513–518. doi: 10.3129/i09-127. [DOI] [PubMed] [Google Scholar]
- 6.Lippa LM, Boker J, Duke A, Amin A. A novel 3-year longitudinal pilot study of medical students’ acquisition and retention of screening eye examination skills. Ophthalmology. 2006;113:133–139. doi: 10.1016/j.ophtha.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 7.Vernon SA. Eye care and the medical student: Where should emphasis be placed in undergraduate ophthalmology? J R Soc Med. 1988;81:335–337. doi: 10.1177/014107688808100612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Quillen DA, Harper RA, Haik BG. Medical student education in ophthalmology: Crisis and opportunity. Ophthalmology. 2005;112:1867–1868. doi: 10.1016/j.ophtha.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 9.Mottow-Lippa L. Ophthalmology in the medical school curriculum: Reestablishing our value and effecting change. Ophthalmology. 2009;116:1235–1236. doi: 10.1016/j.ophtha.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 10.Bellan L. Ophthalmology undergraduate education in Canada. Can J Ophthalmol. 1998;33:3–7. [PubMed] [Google Scholar]
- 11.International Council of Ophthalmology Principles and guidelines of a curriculum for ophthalmic education for medical students. Klin Monatsbl Augenh. 2006;223(S5):1–9. doi: 10.1055/s-2006-951844. [DOI] [PubMed] [Google Scholar]
- 12.Jacobs DS. Teaching doctors about the eye: Trends in the education of medical students and primary care residents. Surv Ophthalmol. 1998;42:383–389. doi: 10.1016/s0039-6257(97)00121-5. [DOI] [PubMed] [Google Scholar]
- 13.Bradford CA. 8th ed. San Francisco, CA: American Academy of Ophthalmology; 2004. Basic Ophthalmology for Medical Students and Primary Care Residents. [Google Scholar]
- 14.Welch S, Eckstein M. Ophthalmology teaching in medical schools: A survey in the UK. Br J Ophthalmol. 2010 Dec 13; doi: 10.1136/bjo.2010.195628. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 15.Medical Council of Canada Objectives for the Qualifying Examination. 3rd ed. 2011. 3.3.1. Available from: http://www.mcc.ca/Objectives_Online/objectives.pl?lang=english&loc=contents#O. Accessed January 5, 2011.
- 16.College of Family Physicians of Canada Priority topics and key features for assessment in Family Medicine. Available from: http://www.cfpc.ca/local/files/Education/Key%20Features.pdf. Accessed September 20, 2010.
- 17.Glicksman JT, Brandt MG, Parr J, Fung K. Needs assessment of undergraduate education in otolaryngology among family medicine residents. J Otolaryngol Head Neck Surg. 2008;37:668–675. [PubMed] [Google Scholar]
- 18.Glicksman JT, Brandt MG, Moukarbel RV, Rotenberg B, Fung K. Computer-assisted teaching of epistaxis management: A randomized controlled trial. Laryngoscope. 2009;119:466–472. doi: 10.1002/lary.20083. [DOI] [PubMed] [Google Scholar]
- 19.Clarkson JG. Training in ophthalmology is critical for all physicians. Arch Ophthalmol. 2003;121:1327. doi: 10.1001/archopht.121.9.1327. [DOI] [PubMed] [Google Scholar]