Abstract
Total en bloc spondylectomy (TES) for vertebral tumour was previously reported by Tomita through a single posterior approach using a T-saw. A modified total en bloc spondylectomy (MTES) technique is reported in the present study. The disc puncture needle with a sleeve was used to obliquely puncture from the posterior to the anterior direction. A T-saw was inserted through the sleeve and led out to the operator’s side by the leading clamp. The disc was partially cut with the saw from its medial to lateral aspect. After a spinal fixation rod was applied on the operator’s side, the residual discs on the opposite side were cut as described above. Six patients with thoracic vertebral tumours were operated on using the MTES technique. Five patients showed improvement in their neurological deficits postoperatively. There was no evidence of tumour recurrence at the final follow-up. The MTES is technically feasible with improved practicality and safety.
Keywords: Modified total en bloc spondylectomy (MTES), Thoracic vertebral tumour, Treatment
Introduction
En bloc spondylectomy is a technique that enables wide or marginal resections of malignant lesions of the spine. In 1997, Tomita et al. reported a new technique, called total en bloc spondylectomy (TES), which employed a single posterior approach using a stainless-steel threadwire saw (T-saw) [5–7]. This technique consists of a posterior en bloc laminectomy after a bilateral pediculotomy using a T-saw and an en bloc corpectomy followed by posterior instrumentation and anterior fusion [5–9]. The advantages of TES include resection of the involved vertebra(e) in two major blocs, rather than in a piecemeal pattern, and completion of the procedure during one surgical session with a posterior incision.
However, two steps are inconvenient in the process of Tomita’s conventional TES using a single posterior approach. First, the intervertebral disc is convex, in contrast to the concave vertebral body, and the anterior longitudinal ligament and periosteum still attach to the spinal column after blunt dissection. These factors make it difficult to accurately control the T-saw on the desired intervertebral disc with an indirect view. Second, when the spinal column is cut from the anterior aspect to the posterior aspect using a T-saw, the cutting should be stopped just before completion. After a posterior fixation rod is applied to stabilize the cut space and to protect the spinal cord from a shearing force injury, the cutting is continued. Moreover, the spinal cord may be injured by the T-saw’s elastic force as soon as cutting is complete.
In the present study, Tomita’s “one-step dissection” TES, in which the dissection is performed from the anterior aspect of the spine to the posterior aspect using a T-saw in one step, was modified into a “two-step” dissection. The purpose of this study is to improve the practicality and safety of TES through a single posterior approach.
Materials and methods
Patient data
Six patients of thoracic tumour, three male and three female, were reported in this study (Table 1). The mean age of the patients at the time of the operation was 61.6 years (range 17–72 years), and the main symptom present was thoracic back pain. The tumours were classified as type 3 (one case), 4 (two cases) and 5 (three cases) according to the Tomita’s classification [7–9]. Preoperative X-ray and CT or MRI was obtained for all the six patients, additional CT-guided core biopsies were performed in two patients pre-operatively. Pathology from the preoperative biopsies and the intraoperative frozen sections showed one was an osteoblastoma, two were giant cell tumours, one was a malignant hemangioma, one was a metastasis from prostate cancer (Fig. 1) and one was a recurrent chordoma. In each of the six patients, there was no evidence of metastases other than the vertebral body lesion. For the prostate cancer metastasis, the original cancer was treated by orchis dissection and chemotherapy. All patients were followed up between postoperative months 10 and 35, respectively.
Table 1.
The patient’s data
| Patient number | Diagnosis | Location | Tomita classification | Frankel scale | |
|---|---|---|---|---|---|
| Pre-op | Post-op | ||||
| 1 | Osteoblastoma | T3 | 4 | E | E |
| 2 | Giant cell tumours | T7 | 4 | D | E |
| 3 | Malignant hemangioma | T9 | 3 | C | D |
| 4 | Giant cell tumours | T9 | 5 | A | A |
| 5 | Prostate cancer metastasis | T10 | 5 | C | E |
| 6 | Recurrent chordoma | T8 | 5 | D | E |
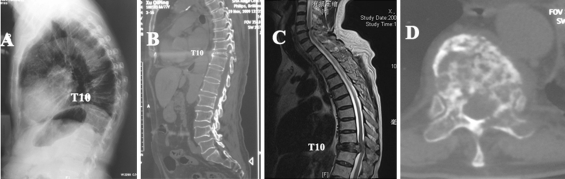
Fig. 1.
Preoperative radiological photographs of the prostatic cancer metastasis at T10 with a thoracic spine kyphosis deformity. The T10 vertebral body was compressed into less than one-third of its original height. It was hard to dissect the thin T10 accurately by the conventional TES “one-step” method
Surgical technique
Under general anaesthesia, the patient was placed on a spine operation table in a prone position. Continuous intravenous methylprednisolone (5 mg/kg) was administered. After localization of the involved vertebral body using the C-arm, the posterior spine was exposed subperiosteally, including two vertebral bodies above and two below the affected vertebra. The biopsy tracts were resected carefully. Pedicle screws (Sofamer Danek, Memphis, TN) were inserted into the four vertebral bodies above and below the affected vertebra.
An area extending 5 cm on either side of the spinous process was exposed. This surgical field was wide enough to allow dissection under the surface of the transverse processes. The ribs at the affected level were transected 3–4 cm lateral to the costotransverse joint. At the lower thoracic spine, one rib on each side was cut; at the upper thoracic spine, two ribs on each side were cut. The pleura were carefully separated from the vertebra. The superior articular process of the uppermost vertebra was exposed. The spinous and inferior articular processes of the neighbouring vertebra were osteotomized and removed with dissection of the attached soft tissues, including the ligamentum flavum. The T-saw was carefully introduced through the intervertebral foramen in a cephalocaudal direction, as described by Tomita [7]. The entire posterior element of the spine was removed in one piece. For the No. 2 patient, which was scaled as Tomita 4 invasion, the vertebra posterior elements were dissected in piecemeal pattern with a safe margin. The surfaces of the cut pedicles were sealed with bone wax. Some tissue was curettaged for histopathological examination by frozen section when the pedicle was invaded.
The segmental arteries and veins were identified and ligated bilaterally. If the ligation failed, a bipolar current was used to help maintain homeostasis. The residual tip of the ligated intercostal vessels can be used as a marker while separating the aorta, from which they generate, from the vertebrae.
The intercostal nerve root was cut on the side from which the affected vertebra was planned to be removed by rotating. Blunt dissection through the plane between the pleura and the vertebral bodies was done on both the sides. The aorta was carefully separated posteriorly from the anterior aspect of the spinal column using spatula and fingers. The operator’s fingertips met with each other directly at the anterior aspect of the affected vertebral body and without any soft tissue between the two fingers. The blunt dissection could extend longitudinally along the spine column to widen the surgical field. A pair of long curved protective retractors was inserted with their anterior tips overlapping at the anterior aspect of the affected body. The surgical field was kept and the surrounding tissues and organs were protected.
The spinal cord was gently mobilized from its surrounding ligamentous tissue and the venous plexus was coagulated using a bipolar. In the case of the recurrent chordoma, the separation of dura mater from the surrounding adhesion tissue was performed from the normal spinal canal after partial laminectomy at the upper and lower vertebrae. After the desired disc was identified, a puncture needle with a sleeve (outer diameter 3 mm, inner diameter 1 mm) was inserted obliquely into the disc along the plane between the dura mater and the disc, with an angle of 45–60° relative to the horizontal plane (Figs. 2a, 3). The puncture port was located in the middle of the posterior aspect of the desired disc, namely the lowest of the spinal canal. When the needle pierced out of the disc, penetration could be felt. The needle and sleeve were stopped by the previously inserted protective retractor. Then, the needle was withdrawn and a T-saw was passed through the left sleeve. The tip of the T-saw could be seen from the opposite side by the assistant, and it was clamped using a specially designed long curved clamp and led out to the operator’s side (Figs. 2b, 3). This step is made more convenient by slightly withdrawing the sleeve. Then, the operator brought down the upper part of the T-saw to the horizontal plane and cut the disc with the T-saw in a reciprocating motion (Fig. 2c).
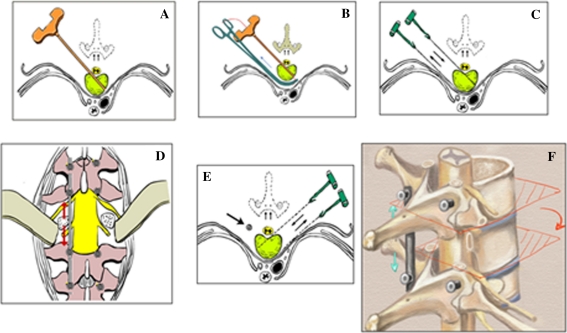
Fig. 2.
The detailed procedure of MTES. a The puncture needle with sleeve is inserted obliquely into the disc through the plane between the dura mater and disc. Then, the needle is pulled out and an oblique operating channel is established. b The T-saw is passed through the channel. The tip of the T-saw is gripped by a specially designed long curved clamp and led out to the operator’s side. c The punctured disc is cut partially by the T-saw from its medial aspect to its lateral aspect. d A posterior fixation rod is used to stabilize the spine on the cut side with appropriate distraction (arrows). e The residual disc is cut at the opposite side without disturbance from the fixation rod. With the fixation rod at the previously cut side (arrow), the spine is stabilized temporarily. f The affected vertebra is rotated around the spinal cord and removed carefully from the secondly punctured side
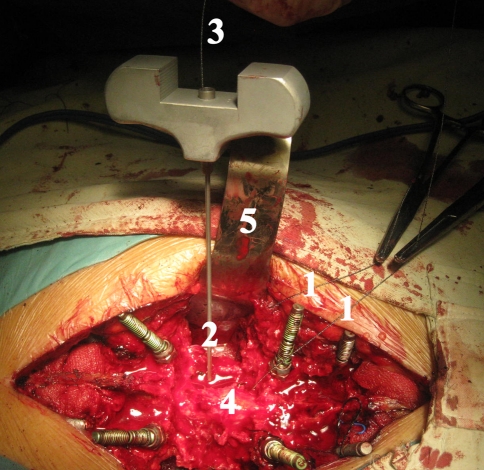
Fig. 3.
An intraoperative photograph. 1 The previously inserted T-saw was led out between the dura mater. 2 The obliquely punctured sleeve in the disc. 3 The inserted T-saw in the sleeve. 4 The spinal cord. 5 The protective retractor
The same procedure was performed on the neighboring disc. After the cutting was finished, one posterior fixation rod was used on the cut side to maintain stability after partial resection of the two discs. With appropriate distraction between the cut space, the disc puncture on the opposite side and rotation of the affected vertebral body around the spinal cord may be more convenient (Fig. 2d).
The needle and sleeve were then inserted obliquely at the opposite side. The puncture port was the same site of the previous puncture. As the disc has been cut partially and the cut space has been distracted, the needle and sleeve can be inserted into the previously cut space more easily than with the first puncture. The residual disc was then cut as previously described (Fig. 2e).
After all disc dissection was complete, the freed anterior column was rotated around the spinal cord and removed carefully from the second puncture side (Figs. 2f, 4). The total en bloc resection of the vertebral tumour was achieved, and another rod was used for fixation on this side.
Fig. 4.
A specimen of the prostatic cancer metastasis at T10 (Fig. 2) obtained by MTES. a The lateral view of the compressed T10 vertebral body. As it was too thin to stand alone, a puncture needle was needed to support it. b The axial view of the destructed T10 vertebra. The tip of the puncture needle indicates the oblique trace remained by the first puncture. There is no similar trace on the opposite side because the cut space has been distracted and the sleeve is inserted into the empty space in a second puncture
After any active bleeding was completely stopped, a titanium mesh cylinder (MOSS® Miami, DePuy Motech, Warsaw, IN) of an appropriate length was selected and filled with autogenous bone graft or harvested healthy rib not affected by tumour. The filled titanium mesh cylinder was placed in the middle of the cut space. After verifying the placement radiographically with a C-arm, the posterior instrumentation was adjusted slightly to compress the inserted mesh. In cases in which the pleura were breached, a chest tube was inserted. Finally, a biological protein glue (Bard, Billerica, MA) was sprayed on the surgical field to reduce bleeding after the operation. A drain was placed and the incision was closed.
Postoperative care
Draining by suction was maintained for 2–3 days after surgery. The patient was allowed to begin walking according to his/her own ability with a brace 1 week postoperatively. The brace should be kept for 2–3 months until the bony union or incorporation of the mesh is confirmed radiographically.
Results
The mean time of surgery was 7.6 h, ranging from 5–10.3 h. The mean blood loss was 1,750 mL, with a range of 900–3,300 mL. The pleura of two patients were disrupted during blunt dissection, and were repaired by suture. Back pain symptoms in all patients were relieved postoperatively. No dura mater rupture or cerebrospinal fluid fistula occurred. No one had a nervous syndrome aggravated after surgery. All patients, except the Frankel A case, showed at least one grade of neurological improvement on the Frankel scale. No recurrence was found during the follow-up period.
Discussion
Spinal tumours account for 5% of all bone tumours. The spine is one of the most frequent sites of metastases from carcinoma; 36% of patients who died due to neoplastic disease were found to have spinal metastases [10]. With the specially designed T-saw, the tumour recurrence is less likely as compared to Gigli Saw and scalpel when the intralesional tumour cutting cannot be avoided [1]. Another advantage of the T-saw is that it can cut the tissue that is encased in it completely in one cut, while the osteotome, chisel, rongeur and even the high speed bur cannot do so [2–5]. During the T-saw’s cutting in a reciprocating motion, no impact or heat produced and transference to the spinal cord.
Conventional TES technique with a T-saw is a technically demanding procedure. Tomita et al. made grooves along the desired cutting line using a v-notched osteotome after the correct disc level had been identified, and then used a teeth-cord protector, which has teeth on both edges, to prevent the T-saw from slipping. They also used a spinal cord spatula to protect the spinal cord while cutting the anterior column of the vertebra and the anterior and posterior longitudinal ligaments with the T-saw [7]. There are three advantages of the modified total en bloc spondylectomy (MTES) technique. First, it’s convenient and reliable to introduce and keep the T-saw in the desired cutting line from the beginning to end. At the same disc level, the second puncture port can be overlapped with the first one because the disc has already been cut and the intervertebral space is empty. With appropriate distraction in the cut space, the second puncture can be made more conveniently. The accuracy of T-saw cutting can be ensured and its slipping can be avoided with MTES. The operating time may be saved and blood loss may be reduced.
Second, after one disc or vertebra is completely cut in the conventional TES pattern, at least one posterior fixation rod should be used to protect spinal cord from injury due to instability. With the MTES technique, after the disc or vertebra is cut at one side, the posterior instrument rod can be fixed on that side with slight distraction. Besides facilitating the second puncture, appropriate distraction between the cut spaces is helpful to remove the lesion vertebra by rotating it around the spinal cord easily. Regarding the lytic and destructive tumour, the vertebral lesion is fragile and may be broken during being removed by rotation around the spinal cord, thus, the surgical field may be contaminated during the last step of TES. MTES can not only ensure spinal temporary stability, but also provide the convenience for removing lesion mass without disturbance.
Third, the MTES is much safer when cutting the disc from medial to lateral aspect. Actually, in our experience with MTES, even the traditional Gigli saw is capable of performing the disc cutting without injury to the dura mater and spinal cord. With MTES, it is also unnecessary to use spatula or other devices to protect the spinal cord in the limited space between dura and disc.
Tomita classified spinal tumours into seven types according to the scope of tumour invasion [4, 5, 7]. They reported that TES was principally indicated in Tomita lesions type 2–5, and lesion types 1 and 6 were only relatively indicated. The indication for this MTES is similar with the conventional TES. But MTES may be of more value for type 1–4 lesions when compared to the conventional TES. The vertebra posterior elements can be removed piecemeal by an extralesional dissection according to the preoperative planning on CT and MRI, as well as intraoperative frozen sections. When the dura and spinal cord are exposed and can be separated from the cut space safely, the residual vertebra and tumour can be dissected in the “two-step” method with MTES. It may be safer and more time saving than conventional TES with bilateral pediclectomy using T-saw. Although no lumbar tumours were reported in the present study, we believe that MTES can be applied to lumbar vertebrae 1, 2 and 3.
In summary, the MTES is technically feasible with improved practicality and safety compared with the conventional TES.
Acknowledgments
Conflict of interest None.
References
- 1.Abdel-Wanis Mel S, Tsuchiya H, Kawahara N, Tomita K. Tumor growth potential after tumoral and instrumental contamination: an in vivo comparative study of T-saw, Gigli saw, and scalpel. J Orthop Sci. 2001;6(5):424–429. doi: 10.1007/s007760170009. [DOI] [PubMed] [Google Scholar]
- 2.Melcher I, Disch AC, Khodadadyan-Klostermann C, Tohtz S, Smolny M, Stöckle U, Haas NP, Schaser KD. Primary malignant bone tumors and solitary metastases of the thoracolumbar spine: results by management with total en bloc spondylectomy. Eur Spine J. 2007;16(8):1193–1202. doi: 10.1007/s00586-006-0295-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Samartzis D, Marco RA, Benjamin R, Vaporciyan A, Rhines LD. Multilevel en bloc spondylectomy and chest wall excision via a simultaneous anterior and posterior approach for Ewing sarcoma. Spine. 2005;30(7):831–837. doi: 10.1097/01.brs.0000158226.49729.6c. [DOI] [PubMed] [Google Scholar]
- 4.Sundaresan N, Rosen G, Huvos AG, Krol G. Combined treatment of osteosarcoma of the spine. Neurosurgery. 1988;23:714–719. doi: 10.1227/00006123-198812000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Tomita K, Kawahara N. The threadwire saw: a new device for cutting bone. J Bone Joint Surg Am. (1996);78((12)):1915–1917. [PubMed] [Google Scholar]
- 6.Tomita K, Kawahara N, Baba H, Tsuchiya H, Nagata S, Toribatake Y. Total en bloc spondylectomy for solitary spinal metastases. Int Orthop. 1994;18(5):291–298. doi: 10.1007/BF00180229. [DOI] [PubMed] [Google Scholar]
- 7.Tomita K, Kawahara N, Baba H, Tsuchiya H, Fujita T, Toribatake Y. Total en bloc spondylectomy. A new surgical technique for primary malignant vertebral tumors. Spine. 1997;22((3)):324–333. doi: 10.1097/00007632-199702010-00018. [DOI] [PubMed] [Google Scholar]
- 8.Tomita K, Kawahara N, Murakami H, Demura S. Total en bloc spondylectomy for spinal tumors: improvement of the technique and its associated basic background. J Orthop Sci. 2006;11(1):3–12. doi: 10.1007/s00776-005-0964-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T. Surgical strategy for spinal metastases. Spine. 2001;26(3):298–306. doi: 10.1097/00007632-200102010-00016. [DOI] [PubMed] [Google Scholar]
- 10.Wong DA, Fornasier VL, MacNab I. Spinal metastases: the obvious, the occult, and the impostors. Spine. 1990;15(1):1–4. doi: 10.1097/00007632-199001000-00001. [DOI] [PubMed] [Google Scholar]