Abstract
Minimally invasive lumbar fusion techniques have been developed in recent 20 years. The goals of these procedures are to reduce approach-related soft tissue injury, postoperative pain, and disability while allowing the surgery to be conducted in an effective manner. There have been no prospective clinical reports published on the comparison of minimally invasive transforaminal lumbar interbody fusion as revision surgery for patients previously treated by open discectomy and decompression or a traditional open approach. A prospective clinical study was performed by evaluating the clinical and radiographic results of minimally invasive transforaminal lumbar interbody fusion as an alternative new technique in the revision surgery for patients previously treated by open procedure. 52 patients (28 M, 24 F) with an average age of 55.7 (31–76) were prospectively evaluated. All patients who had previous discectomy (n = 13), hemilaminectomy (n = 16), laminectomy (n = 12) and facetectomy (n = 11) underwent monosegmental and bisegmental minimally invasive transforaminal lumbar interbody fusion (MiTLIF) (n = 25) or open transforaminal lumbar interbody fusion (OTLIF) (n = 27) by two experienced surgeons at one hospital, from March 2006 to October 2008 (minimum 12-month follow-up). The following data were compared between the two groups: the clinical and radiographic results, operative time, blood loss, X-ray exposure time, postoperative back pain, and complications. Clinical outcome was assessed using the visual analogue scale and the Oswestry disability index (ODI). The operative time and clinical and radiographic results were basically identical in both groups. Comparing with the OTLIF group, the MiTLIF group had significantly less blood loss and less postoperative back pain at the second day postoperatively. The radiation time was significantly longer in the MiTLIF group. Complications included three cases of small dural tear in the MiTLIF group. There were five cases of dural tear and two cases of superficial wound infection in the OTLIF group. One case of nonunion was observed from each group. Minimally invasive TLIF is a safe and effective procedure for treatment of selected revision patients previously treated by open surgery with some potential advantages. However, this technique needs longer X-ray exposure time.
Keywords: Comparison, Revision spine surgery, Minimally invasive transforaminal lumbar interbody fusion, Failed lumbar surgery
Introduction
In 1940, the first successful posterior lumbar interbody fusion (PLIF) was performed using a shaped spinous process autograft [1]. In 1951, Cloward [2] reported satisfactory results in more than 85% of 331 patients using this technique. In addition, because of the moderately high pseudoarthrosis rate encountered using stand-alone grafts, it has become common to augment the PLIF technique with pedicle screws [3]. Transforaminal lumbar interbody fusion (TLIF) was popularized by Harms et al. [4] as an alternative to PLIF. TLIF offers several advantages including decreased retraction of the dural sac, lessening the risk of postoperative radiculitis [5]. Irrespective of the exact method of arthrodesis, conventionally open lumbar surgery performed via a posterior approach is associated with significant soft tissue morbidity that can adversely affect patient outcomes [6–9]. A minimally invasive transforaminal lumbar fusion (MiTLIF) technique has been described to reduce the iatrogenic soft tissue injury that occurs with muscle stripping and retraction during routine spinal exposure [10–14]. Only four studies are currently available comparing MiTLIF to OTLIF as the first surgery [10, 12, 14, 15]. No study to date, however, has compared prospectively the MiTLIF using an expandable working channel and percutaneous pedicle screw system, to the OTLIF in revision surgery for patients previously treated by open discectomy and decompression of lumbar spine.
Materials and methods
Clinical data
The clinical study proposal was approved by the medical ethical committee of the authors’ institution. The written informed consents were obtained from all patients at study entry. In our country, it is difficult to use randomization principle because we cannot arrange surgical plans for all patients in outpatient department. We treated the patients by minimally invasive or open TLIF according to admission order of one by one. From March 2006 to October 2008, 52 consecutive patients with failed discectomy and decompression by open posterior midline approach were treated with Quadrant retractor system and Sextant percutaneous pedicle screw system (Medtronic Sofamor Danek, Memphis, TN, USA), with a mean age of 55.7 years. All patients included 13 cases after discectomy, 16 cases after hemilaminectomy, 12 cases after laminectomy, and 11 cases after facetectomy (more than 1/2 of facet joint removed). 25 patients underwent MiTLIF by one experienced surgeon, including 22 cases of single-level MiTLIF and 3 cases of two-level MiTLIF. 27 patients received OTLIF by other experienced surgeon at the same hospital, including 23 cases of one-level OTLIF and 4 cases of two-level OTLIF. All the patients in both groups presented low back pain as their predominant complaint, with varying degrees of radiating pain, neurological complaints, or a combination of these. All patients had to have been treated conservatively for at least 6 months without success before consideration for surgical intervention. The patients’ demographic characteristic and procedure data of these comparison groups are listed in Table 1.
Table 1.
Patient demographic data
| MiTLIF group | OTLIF group | |
|---|---|---|
| No. of patients | 25 | 27 |
| Mean age (years) | 54.8 ± 10.9 | 56.2 ± 13.6 |
| Gender (M/F) (% male) | 13/12 (52.0) | 15/12 (55.6) |
| Previous diagnoses [no. (%) of patients] | ||
| Lumbar disc herniation | 9 (36.0) | 11 (40.7) |
| Lumbar spinal stenosis | 16 (64.0) | 16 (59.3) |
| Duration after previous surgery (months) | 83.5 ± 17.4 | 90.2 ± 21.6 |
| Revision diagnoses [no. (%) of patients] | ||
| Recurrent disc herniation | 7 (28.0) | 8 (29.6) |
| Lumbar canal stenosis | 10 (40.0) | 9 (33.3) |
| Segmental instability | 5 (20.0) | 7 (25.9) |
| Spondylolisthesis (<grade 2) | 3 (12.0) | 3 (11.1) |
| Level of fusion [no. (%) of patients] | ||
| L3–L4 | 2 (8.0) | 2 (7.4) |
| L4–L5 | 11 (44.0) | 11 (40.7) |
| L5–S1 | 9 (36.0) | 10 (37.0) |
| Two-level fusion | 3 (12.0) | 4 (14.9) |
* P < 0.05, ** P < 0.01
Surgical techniques
Minimally invasive TLIF
After induction of general anesthesia, patients were positioned prone on a radiolucent frame. The anatomic midline, the pedicle outlines, the skin incision points (parallel to the middle of pedicles and between two pedicles above and below the affected disc space) were marked on the skin with C-arm fluoroscopic guidance at the spinal level to be decompressed and instrumented. This incision was used during decompression, disc space preparation, autograft, placement of interbody cage, and pedicle screws without making an additional incision. A 3 cm longitudinal paramedian incision was made for placement of Quadrant retractor system. The procedure was accomplished under direct visualization without microscope or microendoscope. Using an osteotome, the medial aspect of the facet joint on the symptomatic side was carefully excised. The lateral portion of the facet joint was then removed with a kerrison punch. A complete facetectomy were performed. If the facet joint had already been resected, the left part should be found and removed. Blund dissection could be used to help determine the location of laminectomy. It was often useful and very important to find the scar bony interface and begin to dissect the scar plane away from the normal bony structure. According to radicular symptoms of the patient, a pedicle-to-pedicle decompression, and/or lateral and central canal decompression were performed after identification of the lateral border of the dura, the traversing and exiting nerve roots. An aggressive full discectomy was then performed in the Kambin’s triangle [16]. Interbody distractors were introduced in the disc space. Sufficient autologous bone graft obtained from the removed facet (if need, autograft from iliac crest) was packed in the anterior third of the disc space. A single PEEK cage (OIC, Stryker Inc., USA) filled with autologus bone graft was inserted obliquely across the disc space. If there was radiculopathy on two side limbs, relatively worse radiculopathy side was chosen to receive interbody graft and cage. Decompression was then performed on the contralateral side.
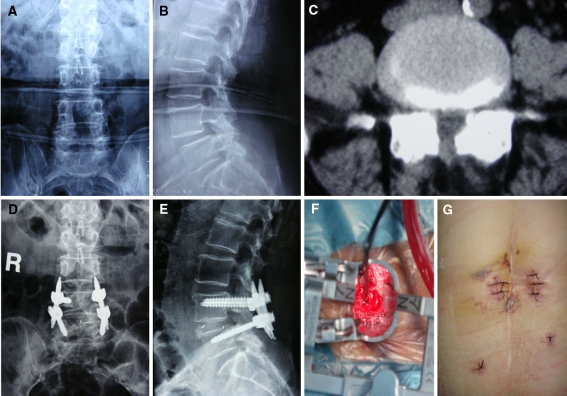
After the Quadrant system was removed, pedicle entry point was directly touched through the surgeon’s index finger within the same incision. A modified cannulated needle (used for percutaneous veterbroplasty) was advanced through the pedicle into the vertebral body under fluoroscopic guidance, followed by insertion of a blunt-tipped guidewire into the ventral third of the vertebral body and tapping of the screw path. Using the percutaneous pedicle screw system, the appropriately sized cannulated M-8 pedicle screws were placed along the guidewire into the pedicle under fluoroscopic guidance. A representative case is shown in Fig. 1.
Fig. 1.
Anteroposterior (a) and lateral (b) radiographs of a 71-year-old female with degenerative spondylolisthesis grade 1 after laminectomy. The preoperative CT (c) showed spinal canal stenosis. Anteroposterior (d) and lateral (e) radiographs after MiTLIF and percutaneous pedicle screw fixation showed reduction of the spondylolisthesis. The view under Quadrant system (f) attached with the light cables. The previous large midline skin incision and small skin incision of MiTLIF (g)
Open TLIF
The open TLIF approach was performed as described by Harms et al. [4] using a midline open approach. A longer skin incision (more than 10 cm) was made. Extensive dissection and resection of scar and paravertebral musculature was performed in order to expose the facet joints and provide the ideal lateral-to-medial orientation for optimal screw trajectory. The same implants were used for OTLIF group.
Clinical and radiological evaluation
The data collected prospectively for analysis were age, gender, previous diagnoses, revision diagnosis, duration after the first operation, level of fusion, operating time, intraoperative and postoperative blood loss, X-ray exposure time, clinical and radiographic results after revision surgery, and complications. Back and leg pain was quantified by visual analog scores (VAS) collected from the patients preoperatively, postoperatively, and in last follow-up. The Oswestry disability index (ODI), version 2.0, was used both before and after surgery to give surgeon information about how the patient’s leg (or back) trouble has affected his/her ability to manage in everyday life. The sex question (Section 8) is unacceptable in our culture, and most patients are reluctant to answer this section; therefore, it was omitted in this study. Therefore, the total possible score is 45.
Preoperative radiological evaluation included anteroposterior, lateral, and flexion–extension plain radiograph, CT scans, and magnetic resonance imaging (MRI). Fusion rates were assessed by an independent radiologist using static and dynamic plain X-rays at 6 and 12 months after surgery. Definitive fusion was identified by the formation of trabecular bony bridges between contiguous vertebral bodies at the instrumented levels, intact hardware, and less than 3° segmental movement according to the fusion criteria [11].
Statistical analysis
Statistical analyses were performed using SPSS 11.0 for windows. Data are shown as mean ± SEM. Student t test was used for the comparison of continuous variables. Fisher’s exact test was used to evaluate the differences of clinical outcomes and fusion rate between the two groups. P values below 0.05 were accepted for significance.
Results
The mean follow-up was 27.5 months with a range of 12–38 months. The age, gender, previous diagnoses, revision diagnoses, duration between the first and second operation, and levels of fusion showed a similar pattern in both groups. None of the patients in the MiTLIF group needed to be converted to the open surgery. There was no statistical difference in operating time, preoperative and latest back (or leg) pain VAS, preoperative and latest ODI between the two groups. The statistical evaluation showed a highly significant decrease in the intraoperative and postoperative blood loss (P < 0.01) with respect to the MiTLIF group. There was significant difference in the X-ray exposure time between both groups with an average of 73 s in the MiTLIF surgery and 39 s in the OTLIF surgery (P < 0.05). The patients in MiTLIF group had a lower mean back pain VAS score than the patients in OTLIF group at the second days after surgery (P < 0.05). All these details of clinical data are illustrated in Table 2.
Table 2.
Comparison of clinical data between the MiTLIF and OTLIF groups
| MiTLIF group | OTLIF group | |
|---|---|---|
| Operating time (min) | 139 ± 27 | 143 ± 35 |
| Intraoperative blood loss (ml) | 291 ± 86** | 652 ± 150 |
| Postoperative blood loss (ml) | 25 ± 10** | 147 ± 58 |
| X-ray time (s) | 73 ± 21* | 39 ± 16 |
| Preoperative back pain VAS | 7.1 ± 2.4 | 6.9 ± 1.7 |
| Back pain VAS at the second day | ||
| After surgery | 2.2 ± 0.6* | 4.3 ± 0.5 |
| Latest back pain VAS | 1.3 ± 0.5 | 1.5 ± 0.4 |
| Latest leg pain VAS | 1.0 ± 0.3 | 1.3 ± 0.4 |
| Preoperative ODI | 39.7 ± 10.1 | 37.9 ± 8.2 |
| Latest ODI | 12.4 ± 3.6 | 11.5 ± 4.2 |
* P < 0.05, ** P < 0.01
Three cases of small dural tear occurred in MiTLIF group during spinal decompression. The overlying fascia was closed tightly without additional exposure and repair. Postoperatively, the patients remained supine on strict bed rest for a few days. Cerebrospinal fluid leakage only lasted 3 or 5 days without any neurological sequelae or wound complication. There were five cases of dural tear and two cases of superficial wound infection in OTLIF group. Dural repairs were intraoperatively performed with a water-tight closure using 5-0 nonabsorbable suture and fibrin glue. Postoperative cerebrospinal fluid leakage stopped within 1 week without clinical sequelae. Two cases of superficial wound infection needed no further surgical treatment and were eradicated using corresponding antibiotics within 2 weeks without secondary complication. One case of nonunion was observed from each group. These nonunion cases were determined by more than 3° segmental motion on flexion–extension lateral radiographs and lack of trabecular bony bridging. Both patients refused revision surgery because of no obvious complaints of low back pain.
Discussion
Revision surgeries are defined as secondary operations for the patients who have undergone previous traditional discectomy, hemilaminectomy, laminectomy, and facetectomy without fusion. Reasons for revision surgery were recurrent disc herniation, spinal stenosis, segmental instability, and spondylolisthesis occurring at the same and adjacent level in our revision series. To date there are no reports available that have compared MiTLIF with OTLIF used as revision surgery after discectomy and decompression of the lumbar spine, although four studies are currently available comparing MiTLIF to OTLIF as the first surgery [10, 12, 14, 15].
Traditionally, open posterior fusion techniques are commonly used. However, decompression, disc preparation, insertion of interbody cage and implantation of spinal instrumentation requires extensive tissue dissection to gain access to the disc space and provide the ideal lateral-to-medial orientation for optimal screw trajectory. Excessive intraoperative dissection lateral to the facet joints and retraction of the paraspinal musculature can lead to denervation and atrophy, which result in an increased risk of “fusion disease” [6–9]. Open surgery with significant blood loss and an increased risk of infection are not uncommon [17]. Mayer et al. [18] demonstrated long-term radiographic atrophy of the operated muscle segment on CT scanning after cases requiring extensive posterior surgical exposure. Recent studies analyzed the amount of muscle damage, via measurements of creatine kinase (CK), which occurs with various types of spine surgery. Open lumbar fusions had a significantly higher amount of CK (muscle damage) in comparison to other minimally invasive procedures [19].
The minimally invasive spinal surgery was developed as a potential solution to the above-mentioned problem by reducing the amount of iatrogenic soft tissue injury. MiTLIF is a relatively new technique attracting increased interest in less invasive surgical fusion techniques [11, 13, 21]. Some studies revealed a significant less blood loss, postoperative pain, and shorter length of hospital stay in MiTLIF group in comparison to open TLIF technique [10, 12, 14, 15]. Selznick et al. found that minimally invasive lumbar interbody fusion as revision surgery was technically feasible and was not associated with more blood loss or neurologic morbidity [20]. The results from our study compare well with those reported by the aforementioned studies as we also found a significant difference in blood loss and postoperative pain at the second day after reoperation between the two groups. The main advantage with less muscular trauma seems to be within the immediate post-operative period, where a significant reduction in pain is conspicuous [21]. Although lessening the approach-related morbidity is a primary aim of minimally invasive spine surgery, this must be accomplished without compromising the efficacy of the procedure. Minimally invasive spinal fusion using the MiTLIF technique is efficacious and safe. Our study showed identical clinical and radiological results based on VAS, ODI scores, and plain radiographs.
The need for intraoperative fluoroscopy poses disadvantages. Our study indeed found longer X-ray exposure times in the MiTLIF group. At this point, however, the surgeons’ experience in minimally invasive surgery is very helpful to reduce radiation. It is stressed that potential cumulative effects of radiation exposure on the patient and operating team should not be neglected. Our study found no significant difference in operating time between both groups, although there was less operating time in MiTLIF group compared with OTLIF group. Dural tear was the most common complications in both groups. There was a higher incidence of dural tears in OTLIF group compared with MiTLIF group. Extensive dissection of paravertebral musculature and fibrotic scar increased the risk of dural tears in OTLIF group. Meanwhile, significant blood loss, and tissue trauma might increase complications of wound infection.
MiTLIF is safe and reliable with comparable results as revision surgery in skilled hands. It needs practice, but also tools to do it. Due to less tissue trauma and structure damage, MiTLIF may reduce the amount of iatrogenic injury while still safely accomplishing the goals of the conventional open TLIF. However, the outcome of the open technique after the short term is equal and preferable for those who cannot do the minimally invasive surgery. It is a drawback that open and minimally invasive TLIF were separately performed by two experienced operators in our study. A randomized controlled trial should be considered in order to provide convincible evidence-based conclusions.
Acknowledgments
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Footnotes
The device(s)/drug(s) is/are FDA-approved or approved by corresponding national agency for this indication.
References
- 1.Cloward RB. History of PLIF: forty years of personal experience. In: Lin PM, editor. Posterior lumbar interbody fusion. Springfield: Charles C Thomas; 1982. pp. 58–71. [Google Scholar]
- 2.Cloward RB. The treatment of ruptured intervertebral discs by vertebral body fusion: Part I—indications, operative technique, after care. J Neurosurg. 1953;10:154–168. doi: 10.3171/jns.1953.10.2.0154. [DOI] [PubMed] [Google Scholar]
- 3.Steffee AD, Sitkowski DJ. Posterior lumbar interbody fusion and plates. Clin Orthop. 1988;227:99–102. [PubMed] [Google Scholar]
- 4.Harms JG, Jeszenszky D. The unilateral transforaminal approach for posterior lumbar interbody fusion. Orthop Traumatol. 1998;6:88–89. [Google Scholar]
- 5.Humphreys SC, Hodges SD, Patwardhan AG, et al. Comparison of posterior and transforaminal approaches to lumbar interbody fusion. Spine. 2001;26:567–571. doi: 10.1097/00007632-200103010-00023. [DOI] [PubMed] [Google Scholar]
- 6.Kawaguchi Y, Matsui H, Tsuji H. Back muscle injury after posterior lumbar spine surgery. A histologic and enzymatic analysis. Spine. 1996;21:941–944. doi: 10.1097/00007632-199604150-00007. [DOI] [PubMed] [Google Scholar]
- 7.Kawaguchi Y, Matsui H, Tsuji H. Back muscle injury after posterior lumbar spine surgery. Part 2: histologic and histochemical analyses in humans. Spine. 1994;19:2598–2602. doi: 10.1097/00007632-199411001-00018. [DOI] [PubMed] [Google Scholar]
- 8.Sihvonen T, Herno A, Paljiarvi L, et al. Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine. 1993;18:575–581. doi: 10.1097/00007632-199304000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Styf JR, Willen J. The effects of external compression by three different retractors on pressure in the erector spine muscles during and after posterior lumbar spine surgery in humans. Spine. 1998;23:354–358. doi: 10.1097/00007632-199802010-00014. [DOI] [PubMed] [Google Scholar]
- 10.Isaacs RE, Podichetty VK, Santiago P, et al. Minimally invasive microendoscopy-assisted transforaminal lumbar interbody fusion with instrumentation. J Neurosurg Spine. 2005;3:98–105. doi: 10.3171/spi.2005.3.2.0098. [DOI] [PubMed] [Google Scholar]
- 11.Schwender JD, Holly LT, Rouben DP, et al. Minimally invasive transforaminal lumbar interbody fusion (TLIF): technical feasibility and initial results. J Spinal Disord Tech. 2005;18(Suppl):S1–S6. doi: 10.1097/01.bsd.0000132291.50455.d0. [DOI] [PubMed] [Google Scholar]
- 12.Scheufler KM, Dohmen H, Vougioukas VI. Percutaneous transforaminal lumbar interbody fusion for the treatment of degenerative lumbar instability. Neurosurgery. 2007;60:203–212. doi: 10.1227/01.NEU.0000255388.03088.B7. [DOI] [PubMed] [Google Scholar]
- 13.Ozgur BM, Yoo K, Rodriguez G, et al. Minimally invasive technique for transforaminal lumbar interbody fusion (TLIF) Eur Spine J. 2005;14:887–894. doi: 10.1007/s00586-005-0941-3. [DOI] [PubMed] [Google Scholar]
- 14.Schizas C, Tzinieris N, Tsiridis E, et al. Minimally invasive versus open transforaminal lumbar interbody fusion: evaluating initial experience. Int Orthop. 2008;33:1683–1688. doi: 10.1007/s00264-008-0687-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peng CWB, Yue WM, Poh SY, Yeo WM, et al. Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine. 2009;34:1385–1389. doi: 10.1097/BRS.0b013e3181a4e3be. [DOI] [PubMed] [Google Scholar]
- 16.Kambin P. Arthroscopic microdiscectomy of the lumbar spine. Clin Sports Med. 1993;12:143–150. [PubMed] [Google Scholar]
- 17.Lee SH, Choi WG, Lim SR, et al. Minimally invasive anterior lumbar interbody fusion followed by percutaneous pedicle screw fixation for isthmic spondylolisthesis. Spine J. 2004;4:644–649. doi: 10.1016/j.spinee.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 18.Mayer TG, Vanharanta H, Gatchel RJ, et al. Comparison of CT scan muscle measurements and isokinetic trunk strength in postoperative patients. Spine. 1989;14:33–36. doi: 10.1097/00007632-198901000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Arts MP, Nieborg A, Brand R, et al. Serum creatine phosphokinase as an indicator of muscle injury after various spinal and nonspinal surgical procedures. J Neurosurg. 2007;7:282–286. doi: 10.3171/SPI-07/09/282. [DOI] [PubMed] [Google Scholar]
- 20.Selznik LA, Shamji MF, Isaacs RE. Minimally invasive interbody fusion for revision lumbar surgery. J Spinal Disord Tech. 2009;22:207–213. doi: 10.1097/BSD.0b013e318169026f. [DOI] [PubMed] [Google Scholar]
- 21.Ringel F, Stoffel M, Stuer C, et al. Minimally invasive transmuscular pedicle screw fixation of the thoracic and lumbar spine. Neurosurgery. 2006;59(4 Suppl 2):ONS361–ONS366. doi: 10.1227/01.NEU.0000223505.07815.74. [DOI] [PubMed] [Google Scholar]