Abstract
Extreme/direct lateral interbody fusion (X/DLIF) has been used to treat various lumbar diseases. However, it involves risks to injure the lumbar plexus and abdominal large vessels when it gains access to the lumbar spine via lateral approach that passes through the retroperitoneal fat and psoas major muscle. This study was aimed to determine the distribution of psoas major and abdominal large vessels at lumbar intervertebral spaces in order to select an appropriate X/DLIF approach to avoid nerve and large vessels injury. Magnetic resonance imaging scanning on lumbar intervertebral spaces was performed in 48 patients (24 males, 24 females, 54.2 years on average). According to Moro’s method, lumbar intervertebral space was divided into six zones A, I, II, III, IV and P. Thickness of psoas major was measured and distribution of abdominal large vessels was surveyed at each zone. The results show vena cava migrate from the right of zone A to the right of zone I at L1/2–L4/5; abdominal aorta was located mostly to the left of zone A at L1/2–L3/4 and divided into bilateral iliac arteries at L4/5; Psoas major was tenuous and dorsal at L1/2 and L2/3, large and ventral at L3/4 and L4/5. Combined with the distribution of nerve roots reported by Moro, X/DLIF approach is safe via zones II–III at L1/2 and L2/3, and via zone II at L3/4. At L4/5, it is safe via zones I–II in left and via zone II in right side, respectively.
Keywords: X/DLIF, Psoas Major, Abdominal large vessels, MRI Study
Introduction
Since Obenchain reported the first case of laparoscopic discectomy [1], minimally invasive anterior lumbar spinal surgery has evolved continuously. Due to many advantages such as less tissue trauma, less postoperative pain, shorter hospital stays and faster return to the activities of daily living, the technique is favored by some surgeons and patients. Therefore, the laparoscopic anterior and mini-open anterior lumbar interbody fusion (mini-ALIF) is performed more and more frequently [2–6]. In recent years, the application of ALIF has gradually increased. The technique reduces the incidence of pseudoarthrosis but also rebuilds the patients’ normal lumbar sagittal alignment [2, 7–15]. However, the widely application of this minimally invasive anterior lumbar spinal surgery is hampered by some potentially serious complications, such as large vessel injury [16] and nerve injury [17]. In 2006, Ozgur and his colleagues [18] reported a new minimally invasive ALIF technique, described as extreme lateral interbody fusion (XLIF). XLIF approach passes through the retroperitoneal space, separates the psoas major between the middle and anterior third of the psoas major and reaches the lumbar intervertebral spaces. Direct later lumbar interbody fusion (DLIF) is also a new ALIF technique, no significant technique variation between XLIF and DLIF [19]. With regard to X/DLIF, it is critical to accurately choose the point at which to pass through the psoas major. This precision is necessary to reach the lumbar intervertebral space to accomplish the operation and avoid the large vessel and nerve injury. If the puncture site is too anterior, it is easy to injure the large vessels. However, if the puncture site is too posterior, it is easy to injure the lumbar nerve roots that have descended inside the psoas major. In addition, the thickness of the psoas major at the location of the puncture site also affects the operation’s safety. If the psoas major is very thick, the peritoneum is easily dissected, the retroperitoneal space is larger, the operation is safer and the risk of peritoneal injury and abdominal viscera injury is reduced. The converse is true as well. However, the distribution of abdominal large vessels and the psoas major of each lumbar intervertebral space is inconsistent; a relevant anatomical study of their distribution has not yet been reported. Therefore, the purpose of this study is to comprehend precisely the distribution of psoas major and abdominal large vessels at lumbar intervertebral spaces L1/2, L2/3, L3/4 and L4/5 to select the appropriate X/DLIF approaches and to avoid complications such as vessel and nerve injury.
Materials and methods
Inclusion criteria
This protocol was approved by Changhai Hospital (Shanghai 200433, China). Patients with low back pain and/or radicular pain scheduled for magnetic resonance imaging (MRI) were included in this research. Patients with lumbar trauma, previous celiac or anterior lumbar surgery, lumbar tumours, Spondylolisthesis, degenerative lumbar scoliosis and lumbar tuberculosis (TB) were excluded. Forty-eight patients meeting with the standards were included in the research, including 24 males and 24 females, average age 54.2 years (26–64 years).
Scanning and measurements
An MRI scanning machine (Magnetom symphony 1.5T) was used to transversely tomoscan intervertebral spaces L1/2, L2/3, L3/4 and L4/5 in 48 patients, to obtain T1- and T2-weighted images of the L1/2–L4/5 intervertebral spaces.
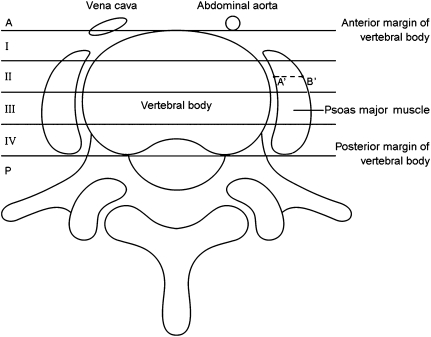
According to Moro’s method [20], lumbar intervertebral spaces were divided in six zones from the anterior to the posterior. The anterior aspect of the anterior margin of the vertebral body was defined as zone A; the posterior of the posterior margin as zone P; zones I, II, III, IV were distributed equally between the anterior margin and the posterior margin from the anterior to the posterior, respectively, as shown in Fig. 1. The distribution of abdominal large vessels at each zone of each lumbar intervertebral space was analyzed base on the MRI images; the thickness of the psoas major at each zone of each lumbar intervertebral space was measured via image analysis software (Synogo Fastview) on an MRI machine. The thickness of the psoas major was defined as the distance between the midpoints of the inner and outer margins of the psoas major at each zone.
Fig. 1.
According to Moro’s method, lumbar intervertebral spaces are divided in six zones from the anterior to the posterior, i.e., the zone between the anterior and posterior border of the vertebral body is divided in zones A, I, II, III and IV. The anterior surface of the anterior border of the vertebral body is defined as zone A, and the posterior surface of the posterior border of the vertebral body is defined as zone P. The vena cava was located at the juncture of the left of zone A and the left of zone I, the abdominal aorta at the left of zone A. A’ is the midpoint of the inner margin of the left psoas major in zone II, B’ is the midpoint of the outer margin of the left psoas major in zone II, the distance between A’ and B’ is the thickness of the left psoas major in zone II
Statistics
Two-factor variance analysis of repeated measurements was used via SPSS10.0 to compare the differences in thickness of the psoas major under age, gender and lumbar intervertebral space factors, respectively.
Results
Distribution of vena cava
Vena cava migrate from the right of zone A to the right of zone I at L1/2–L4/5. At the intervertebral spaces L1/2 and L2/3, it was completely located to the right of zone A and at the juncture of the right of zone A and the right of zone I. At the L3/4 intervertebral space, 6.2% of vena cava were located completely to the right of zone I; the rest (93.8%) were located to the right of zone A and at the juncture of the right of zone A and the right of zone I; at the L4/5 intervertebral space, 29.2% of vena cava were located completely to the right of zone I, and the rest (70.8%) were located to the right of zone A and at the juncture of the right of zone A and the right of zone I. These results are shown in Table 1 and Fig. 4a.
Table 1.
Distribution of vena cava at L1/2–L4/5 intervertebral spaces for 48 patients
| Distribution | L1/2 | L2/3 | L3/4 | L/4/5 | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| The right of zone A | 34 | 70.8 | 21 | 43.8 | 14 | 29.2 | 9 | 18.8 |
| The right of zone A + the right of zone I | 14 | 29.2 | 27 | 56.2 | 31 | 64.6 | 25 | 52.0 |
| The right of zone I | 0 | 0 | 0 | 0 | 3 | 6.2 | 14 | 29.2 |
| Total | 48 | 100 | 48 | 100 | 48 | 100 | 48 | 100 |
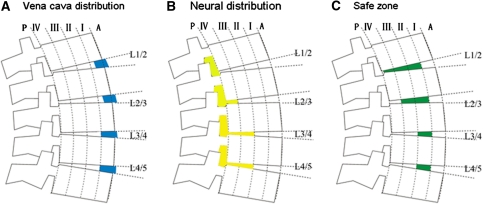
Fig. 4.
Illustration of right-side XLIF approaches as related to anatomical structure: a vena cava distribution, b neural distribution, and c safe zone
Distribution of abdominal aortas
The abdominal aortas at intervertebral spaces L1/2, L2/3 and L3/4 were located mostly to the left of zone A (95.8, 85.4, 79.1%, respectively); at the L4/5 intervertebral space, about 62.6% of the abdominal aortas divided into bilateral iliac arteries: these branches were located at zone A. More specifically, 48.0% of the abdominal aortas divided into bilateral iliac arteries at this location and these branches were located to both the left and right of zone A. The other 14.6% divided into bilateral iliac arteries but these branches adhered tightly just together in the anterior surface of the vertebral body. These results are shown in Table 2 and Fig. 5a.
Table 2.
Distribution of abdominal aortas at L1/2–L4/5 intervertebral spaces for 48 patients
| Distribution | L1/2 | L2/3 | L3/4 | L/4/5 | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| The left of zone I + the left of zone A | 1 | 2.1 | 1 | 2.1 | 1 | 2.1 | 0 | 0 |
| The left of zone A | 46 | 95.8 | 41 | 85.4 | 38 | 79.1 | 14 | 29.2 |
| The midpoint of zone A | 1 | 2.1 | 5 | 10.4 | 8 | 16.7 | 7 | 14.6 |
| The left of zone A + the right of zone A | 0 | 0 | 0 | 0 | 1 | 2.1 | 25 | 52.0 |
| The right of zone A | 0 | 0 | 1 | 2.1 | 0 | 0 | 2 | 4.2 |
| Total | 48 | 100 | 48 | 100 | 48 | 100 | 48 | 100 |
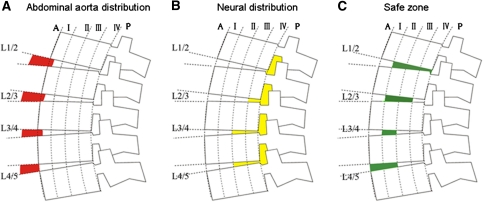
Fig. 5.
Illustration of left-side XLIF approach associated with anatomical structure: a distribution of abdominal aorta, b neural distribution, and c safe zone
Thickness and distribution of psoas major at each zone of the L1/2–L4/5 intervertebral spaces
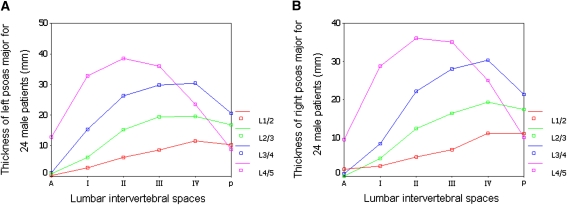
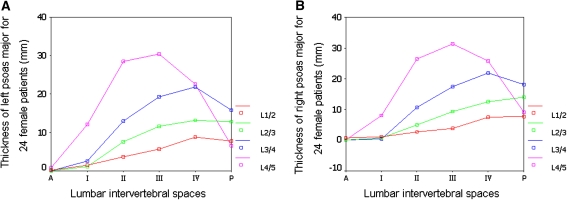
Two-factor variance analysis of repetitive measurements on SPSS10.0 (at the significance level α = 0.05 and in two-tailed test) was used to analyze the thickness of the psoas major at each zone of the L1/2–L4/5 intervertebral spaces for 48 patients, and the results showed no statistical significance for the age factor, but showed statistical significance for the gender factor and lumbar intervertebral space factor. The psoas major of male were much thicker than female’s; The psoas major was tenuous and near the dorsa at the intervertebral spaces L1/2 and L2/3, large and near the ventral aspect at the intervertebral spaces L3/4 and L4/5. For 24 male patients, the thickness of the left and right psoas major at each intervertebral zone of L1/2–L4/5 intervertebral spaces demonstrated a variation of increase first and then decrease from zone A to zone P. The peak of L1/2–L3/4 was located at zone IV and the peak of L4/5 was located at zone II, as shown in Fig. 2a, b. For 24 female patients, the thickness of left psoas major at each intervertebral zone for L1/2–L4/5 lumbar intervertebral spaces also demonstrated first increase and then decrease from zone A to zone P. The peak of L1/2–L3/4 was located at zone IV and the peak of L4/5 was located at zone III, as shown in Fig. 3a. The thickness of right psoas major at each intervertebral zone of L1/2–L2/3 lumbar intervertebral spaces demonstrated variation with the gradual increase from zone A to zone P, the peak located at zone P, while the thickness of the right psoas major at L3/4–L4/5 lumbar intervertebral spaces demonstrated a variation of increase first and then decrease from zone A to zone P, with the peak of L3/4 located at zone IV and the peak of L4/5 at zone III, as shown in Fig. 3b.
Fig. 2.
Curves of the thickness of left and right psoas major for 24 male patients: a left and b right
Fig. 3.
Curves of the thickness of left and right psoas major for 24 female patients: a left and b right
Discussion
Distribution of lumbar nerve roots at each L1/2–L4/5 intervertebral space
Moro and his colleagues [20] reported the anatomical studies of lumbus plexus associated with laparoscopic peritoneal posterior lumbar spine surgery; the results revealed that the lumbus plexus was located at zone P of the L1/2 intervertebral space, at zone IV and the posterior surface of zone IV of L2/3, at zone III and the posterior surface of zone III for the L3/4 and L4/5. Benglis and his colleagues [21] reported the anatomical studies of lumbosacral plexus associated with minimally invasive lumbar surgery via the psoas major approaches. The results showed the length ratios between location of lumbosacral plexus and full length of intervertebral space were 0 at L1/2, 0.11 at L2/3, 0.18 at L3/4 and 0.28 at L4/5, respectively. According to Moro’s zone division, the ratio was 0 at L1/2, that is to say, the lumbus plexus was located at zone P of L1/2; the ratio was 0.11 at L2/3 and 0.18 at L3/4, respectively, that is, the lumbus plexus was located within 1/4 of the full length of the intervertebral space, i.e., and the posterior of zone IV. The ratio was 0.28 at L4/5, that is, the lumbus plexus was located at within 1/2 of full length of the intervertebral space at L4/5, i.e., at zone III and the posterior surface of zone III (Figs. 4b, 5b).
Safe zones of right-side X/DLIF approaches at each L1/2–L4/5 intervertebral space
Based on the distribution of vena cava above, the right-side X/DLIF approach does not injure the vena cava at zones II–P of intervertebral spaces L1/2, L2/3, L3/4 and L4/5 (Fig. 4a). Combined with the distribution of the nerve roots that Benglis and Moro reported on, the safe zone of right-side X/DLIF approaches was located at zones II–IV of L1/2, at zones II–III of L2/3, at zone II of L3/4 and L4/5 (Fig. 4c). For convenient operation, it may pass through the psoas major via the location between zone II and zone III of both lumbar intervertebral spaces of L1/2 and L2/3. This would not injure the vena cava and nerve plexus; the approach must pass through the psoas major at zone II of both L3/4 and L4/5 to avoid injury to the vena cava and plexus. Combined with the distribution of psoas major above, the peak of the male right psoas major is located at zone IV of L1/2–L3/4 intervertebral spaces. Therefore, for male right-side X/DLIF approaches to L1/2–L3/4 intervertebral spaces, the needle should be inserted to separate the psoas major at the anterior surface of the peak of the psoas major. The peak of the male psoas major is located at zone II of the L4/5 intervertebral space, therefore, for male right-side X/DLIF approaches of the L4/5 intervertebral space we should insert the needle to separate the psoas major at the peak of the psoas major. The peak of the right psoas major in females is located at zone P of L1/2 and L2/3 intervertebral spaces, the peak at zone IV of the L3/4 intervertebral space, and the peak at zone III of the L4/5 intervertebral space. Therefore, for all female right-side X/DLIF approaches, it is advisable to insert the needle to separate the psoas major at the anterior surface of the peak of the psoas major. The needle insertion point at L1/2 and L2/3 intervertebral spaces has to have a little bit removed from the peak.
Safe zones of left-side X/DLIF approaches at each L1/2–L4/5 intervertebral space
Combined with the distribution of the aorta above, left-side X/DLIF approaches at zones II–P of L1/2–L3/4 intervertebral spaces and at the I–P zone of L4/5 intervertebral space does not injure the aorta, as shown in Fig. 5a. Combined with the distribution of nerve roots Moro and Benglis reported on, the safe zones of left-side X/DLIF approaches are at zones II–IV of L1/2, at zone II and zone III of L2/3, at zone II of L3/4, and at zone I and zone II of L4/5, as shown in Fig. 5c. For convenient operation, the approach might pass through the psoas major via the location between zone II and zone III of both L1/2 and L2/3 lumbar intervertebral spaces, and this would not injure the aorta and nerve roots. The approach must pass through the psoas major at zone II of L3/4 to avoid the aorta and nerve root injury, or else pass through the psoas major at zones I–II of L4/5. Combined with the distribution of psoas major above, the peak of the male left psoas major is located at zone IV of L1/2–L3/4 intervertebral spaces, therefore, for male left-side X/DLIF approaches of L1/2–L3/4 intervertebral spaces, should involve insertion of the needle to separate the psoas major via the anterior surface of the peak of the psoas major. The peak of male psoas major of L4/5 intervertebral space is located at zone II, therefore, for male left-side X/DLIF approaches of L4/5 intervertebral space, has to involve the insertion of a needle to separate the psoas major via the peak or slight to the anterior surface of the psoas major. The peak of female left psoas major of L1/2–L3/4 intervertebral spaces is located at zone P, and the peak of L4/5 intervertebral space is at zone III. Therefore, for female X/DLIF approaches we should insert all needles to separate the psoas major via the anterior surface of the peak of the psoas major.
Probability of genitofemoral nerve injury
According to Moro’s research on genitofemoral nerves, the genitofemoral nerves at L1/2 and L2/3 intervertebral spaces are located at zone IV and zone P. Therefore, for X/DLIF approaches of L1/2 and L2/3 intervertebral spaces, it does not injure the genitofemoral nerves to separate the psoas major via the location between zone II and zone III. For X/DLIF approaches to L4/5 intervertebral space, it should separate the psoas major at zone II, and at this time the genitofemoral nerves have ascended on the surface of the psoas major and are less easy to injure. At L3/4 intervertebral space, the genitofemoral nerves pass obliquely through the psoas major via the posterior surface to reach its anterior surface. Therefore, X/DLIF approaches of L3/4 intervertebral space are likely to injure genitofemoral nerves if the approach passes through the psoas major via the location between zones II.
Limitations
The limitations in this study are small sample size, the influence of racial difference and the height and weight of patients were not excluded. All the subjects involved in this study were Chinese, thus the results are more suitable for Asians. The data of this study revealed a general conclusion about X/DLIF surgical approach. Due to the limitations of this study, the conclusion cannot be directly incorporated in individual patient’s treatment. For individual patients, the X/DLIF surgical approach needs to be adjusted according to individual patient’s MRI. We suggest the surgeons to perform a MRI scan at the aimed disc to get the precise abdominal vessels and psoas major information when performing X/DLIF, and then refer to the result of this study in order to select a safer individualized X/DLIF approach.
Conflict of interest
The authors declare that they have no competing interests.
References
- 1.Obenchain TG. Laparoscopic lumbar discectomy: case report. J Laparoendosc Surg. 1991;1:145–149. doi: 10.1089/lps.1991.1.145. [DOI] [PubMed] [Google Scholar]
- 2.Regan JJ, Aronoff RJ, Ohnmeiss DD, Sengupta DK. Laparoscopic approach to L4–L5 for interbody fusion using BAK cages: experience in the first 58 cases. Spine (Phila Pa 1976) 1999;24:2171–2174. doi: 10.1097/00007632-199910150-00018. [DOI] [PubMed] [Google Scholar]
- 3.Lieberman IH, Willsher PC, Litwin, Salo PT, Kraetschmer BG. Transperitoneal laparoscopic exposure for lumbar interbody fusion. Spine (Phila Pa 1976) 2000;25:509–514. doi: 10.1097/00007632-200002150-00019. [DOI] [PubMed] [Google Scholar]
- 4.Olsen D, McCord D, Law M. Laparoscopic discectomy with anterior interbody fusion of L5–S1. Surg Endosc. 1996;10:1158–1163. doi: 10.1007/s004649900270. [DOI] [PubMed] [Google Scholar]
- 5.Zdeblick TA, David SM. A prospective comparison of surgical approach for anterior L4–L5 fusion: laparoscopic versus mini anterior lumbar interbody fusion. Spine (Phila Pa 1976) 2000;25:2682–2687. doi: 10.1097/00007632-200010150-00023. [DOI] [PubMed] [Google Scholar]
- 6.Zucherman JF, Zdeblick TA, Bailey SA, Mahvi D, Hsu KY, Kohrs D. Instrumented laparoscopic spinal fusion. Preliminary results. Spine (Phila Pa 1976) 1995;20:2029–2034. doi: 10.1097/00007632-199509150-00015. [DOI] [PubMed] [Google Scholar]
- 7.Mayer HM. A new microsurgical technique for minimally invasive anterior lumbar interbody fusion. Spine (Phila Pa 1976) 1997;22:691–699. doi: 10.1097/00007632-199703150-00023. [DOI] [PubMed] [Google Scholar]
- 8.McAfee PC. Complications of anterior approaches to the thoracolumbar spine. Emphasis on Kaneda instrumentation. Clin Orthop Relat Res. 1994;306:110–119. [PubMed] [Google Scholar]
- 9.McAfee PC, Regan JJ, Geis WP, Fedder IL. Minimally invasive anterior retroperitoneal approach to the lumbar spine. Emphasis on the lateral BAK. Spine (Phila Pa 1976) 1998;23:1476–1484. doi: 10.1097/00007632-199807010-00009. [DOI] [PubMed] [Google Scholar]
- 10.McAfee PC, Regan JR, Zdeblick T, Zuckerman J, Picetti 3rd GD, Heim S, Geis WP, Fedder IL (1995) The incidence of complications in endoscopic anterior thoracolumbar spinal reconstructive surgery. A prospective multicenter study comprising the first 100 consecutive cases. Spine (Phila Pa 1976) 20:1624–1632 [DOI] [PubMed]
- 11.Olinger A, Hildebrandt U, Mutschler W, Menger MD. First clinical experience with an endoscopic retroperitoneal approach for anterior fusion of lumbar spine fractures from levels T12 to L5. Surg Endosc. 1999;13:1215–1219. doi: 10.1007/PL00009624. [DOI] [PubMed] [Google Scholar]
- 12.Regan JJ, Guyer RD. Endoscopic techniques in spinal surgery. Clin Orthop Relat Res. 1997;335:122–139. [PubMed] [Google Scholar]
- 13.Regan JJ, McAfee PC, Guyer RD, Aronoff RJ. Laparoscopic fusion of the lumbar spine in a multicenter series of the first 34 consecutive patients. Surg Laparosc Endosc. 1996;6:459–468. doi: 10.1097/00019509-199612000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Regan JJ, Yuan H, McCullen G. Minimally invasive approaches to the spine. Instr Course Lect. 1997;46:127–141. [PubMed] [Google Scholar]
- 15.Regan JJ, Yuan H, McAfee PC. Laparoscopic fusion of the lumbar spine: minimally invasive spine surgery: a prospective multicenter study evaluating open and laparoscopic lumbar fusion. Spine (Phila Pa 1976) 1999;24:402–411. doi: 10.1097/00007632-199902150-00023. [DOI] [PubMed] [Google Scholar]
- 16.Baker JK, Reardon PR, Reardon MJ, Heggeness MH. Vascular injury in anterior lumbar surgery. Spine (Phila Pa 1976) 1993;18:2227–2230. doi: 10.1097/00007632-199311000-00014. [DOI] [PubMed] [Google Scholar]
- 17.Christensen FB, Bunger CE. Retrograde ejaculation after retroperitoneal lower lumbar interbody fusion. Int Orthop. 1997;21:176–180. doi: 10.1007/s002640050145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ozgur BM, Aryan HE, Pimenta L, Taylor WR. Extreme Lateral Interbody Fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J. 2006;6:435–443. doi: 10.1016/j.spinee.2005.08.012. [DOI] [PubMed] [Google Scholar]
- 19.Knight RQ, Schwaegler P, Hanscom D, Roh J. Direct lateral lumbar interbody fusion for degenerative conditions: early complication profile. J Spinal Disord Tech. 2009;22:34–37. doi: 10.1097/BSD.0b013e3181679b8a. [DOI] [PubMed] [Google Scholar]
- 20.Moro T, Kikuchi S, Konno S, Yaginuma H. An anatomic study of the lumbar plexus with respect to retroperitoneal endoscopic surgery. Spine (Phila Pa 1976) 2003;28:423–428. doi: 10.1097/01.BRS.0000049226.87064.3B. [DOI] [PubMed] [Google Scholar]
- 21.Benglis DM, Vanni S, Levi AD. An anatomical study of the lumbosacral plexus as related to the minimally invasive transpsoas approach to the lumbar spine. J Neurosurg Spine. 2009;10:139–144. doi: 10.3171/2008.10.SPI08479. [DOI] [PubMed] [Google Scholar]