Abstract
The purpose of this study is to assess the successful incorporation of cages in patients after cervical or lumbar intercorporal fusion with positron-emission tomography/computed tomography (PET/CT). Twenty patients (14 female and 6 male; mean age 58 years, age range 38–73 years) with 30 cervical (n = 13) or lumbar (n = 17) intercorporal fusions were prospectively enrolled in this study. Time interval between last intercorporal intervention and PET/CT ranged from 2 to 116 months (mean 63; median 77 months). IRB approval was obtained for all patients, and written informed consent was obtained from all patients. About 30 min prior to PET/CT scanning, 97–217 MBq (mean 161 MBq) 18F-fluoride were administered intravenously. Patients were imaged in supine position on a combined PET/CT system (Discovery RX/STE, 16/64 slice CT, GE Healthcare). 3D-PET emission data were acquired for 1.5 and 2 min/bed position, respectively, and reconstructed by a fully 3D iterative algorithm (VUE Point HD) using low-dose CT data for attenuation correction. A dedicated diagnostic thin-slice CT was optionally acquired covering the fused region. Areas of increased 18F-fluoride uptake around cages were determined by one double-board certified radiologist/nuclear physician and one board certified radiologist in consensus. In 12/20 (60%) patients, increased 18F-fluoride uptake around cages was observed. Of the 30 intercorporal fusions, 15 (50%) showed increased 18F-fluoride uptake. Median time between intervention and PET/CT examination in cages with increased uptake was 37 months (2–116 months), median time between intervention and PET/CT examination in those cages without increased uptake was 91 months (19–112 months), p (Wilcoxon) = 0.01 (one-sided). 14/29 (48%) cages with a time interval > 1 year between intervention and PET/CT scan showed an increased uptake. In conclusion, PET/CT frequently shows increased 18F-fluoride uptake in cervical and lumbar cages older than 1 year (up to almost 8 years in cervical cages and 10 years in lumbar cages) possibly indicating unsuccessful fusion due to increased stress/microinstability.
Keywords: 18F-fluoride PET/CT, Cage, 18F-fluoride uptake, Spine surgery, Intercorporal fusion, Stress/microinstability, Cervical spine, Lumbar spine
Introduction
Cervical and lumbar intercorporal fusions are performed to treat symptomatic segmental degeneration or instability in the cervical and lumbar spine [1–4]. A large number of studies assessing outcome in patients after spine surgery clinically, to a lesser extent by (combined) morphological and functional imaging techniques, e.g. bone SPECT and [(18)F]fluoride positron-emission tomography/computed tomography (PET/CT), have been performed since the late 1980s. Special interest is put on patients who lack osseous fusion after surgery including intercorporal fusions [4–11].
18F-labeled NaF was already used for bone scintigraphy by Blau et al. in the early 1960s. Aftermath due to technical and availability reasons, 99mTc-labeled bone seeking agents like 99mTc-methylene diphosphonate (MDP) were preferred for bone scanning. In the early 1990s, 18F-fluoride was readopted for PET scanning [12].
18F-fluoride is a tracer depicting blood flow and osteoblastic activity. After i.v. administration, 18F-fluoride diffuses from the bone capillaries into the bone extracellular fluid (ECF). Its plasma clearance is more rapid and its single-passage extraction efficiency is higher compared to 99mTc-MDP due to its smaller molecular weight and its negligible protein binding. From the bone ECF, 18F-fluoride is taken up to form the mineral fluorapatite at the surface of bone crystals especially at sites of bone remodeling with high turnover. Its bone uptake is approximately twofold greater than that of the conventional tracer 99mTc-MDP and its blood to bone clearance reaches almost 100%, with the fast blood clearance resulting in a better target-to-background ratio. As a further advantage, 18F-fluoride allows imaging shortly (in our protocol about 30 min) after i.v. administration in contrast to 99mTc-MDP [13, 14]. The current work presents a prospective study analyzing 18F-fluoride uptake around cages in patients after cervical and/or posterior lumbar intercorporal fusion. It is hypothesized that increased stress/microinstability and thus missing or incomplete osseous intercorporal fusion shows concomitant increased 18F-fluoride uptake. It was investigated how long after last intercorporal intervention increased uptake can be observed.
Patients and methods
Patient selection
20 patients (14 female and 6 male; mean age 58 years, age range 38–73 years) with 30 intercorporal cervical (13/30) or lumbar (17/30) fusions were prospectively enrolled in this study between March 2008 and March 2009 (Table 1). We received approval from our Institutional Review Board (IRB) as well as written informed consent of each patient. Time interval between last intercorporal intervention and PET/CT examination ranged from 2 to 116 months (mean 63 months; median 77 months). Patients had chronic back pain, the vast majority of the lower/lumbar spine. No clinical suspicion of infection was given. Only titan containing cages with autologous bone grafts had been implanted (Table 2).
Table 1.
20 patients with cervical and/or lumbar intercorporal fusions
| Patient no. | Gender | Age | MBq | Time of surgeries | No. of in-house-surgeries |
|---|---|---|---|---|---|
| 1 | f | 64 | 145 | 2000–2007 | 6 |
| 2 | m | 67 | 215 | 2004–2007 | 7 |
| 3 | m | 70 | 180 | 2004–2005 | 2 |
| 4 | f | 65 | 175 | 2007–2008 | 2 |
| 5 | f | 55 | 97 | 1999–2005 | 3 |
| 6 | m | 62 | 184 | 1999–2007 | 5 |
| 7 | f | 70 | 155 | 2002–2008 | 8 |
| 8 | m | 52 | 217 | 2001–2006 | 5 |
| 9 | f | 63 | 175 | 2002–2004 | 6 |
| 10 | f | 38 | 136 | 2006–2007 | 3 |
| 11 | f | 60 | 214 | 2001 | 1 |
| 12 | m | 48 | 158 | 1999–2002 | 2 |
| 13 | f | 62 | 125 | 2007 | 1 |
| 14 | f | 73 | 156 | 2000–2005 | 3 |
| 15 | f | 48 | 124 | 2000–2005 | 2 |
| 16 | f | 39 | 116 | 1998–2003 | 4 |
| 17 | f | 47 | 153 | 2001–2007 | 4 |
| 18 | f | 54 | 129 | 1999–2001 | 2 |
| 19 | f | 59 | 172 | 1998–2004 | 7 |
| 20 | m | 56 | 194 | 2004–2008 | 3 |
Gender (f female, m male), Age (in years), Activitiy administered (in MBq), time and number of in-house-surgeries
Table 2.
18F-fluoride uptake around cages in 20 patients with 30 cervical and/or lumbar intercorporal fusions
| Patient no. | Segment cervical spine | Segment lumbar spine | Time in months between last intercorporal intervention and PET/CT | Increased uptake, yes (1)/no (0) | Materiala |
|---|---|---|---|---|---|
| 1 | C4/5, 5/6, 6/7 | – | 92 (3×) | 0, 0, 1 | ID HWS Cage, Titanium (3×) |
| 2 | – | L5/S1 (left) | 17 | 1 | Telamon Titanium |
| 3 | C5/6, 6/7 | – | 30 (2×) | 1, 1 | ID HWS Cage, Titanium (2×) |
| 4 | – | L4/5 | 13 | 1 | Telamon Titanium |
| 5 | – | L4/5, L5/S1 | 102 (L4/5), 35 (L5/S1) | 0, 0 | ProSpace Titanium, Telamon Titanium |
| 6 | – | L4/5 | 107 | 0 | ProSpace Titanium |
| 7 | C5/6 | L2/3, L4/5 | 37 (C5/6), 2 (L2/3), 69 (L4/5) | 1, 1, 0 | ID HWS Cage, Titanium, KZC, Titaniumb, ProSpace Titanium |
| 8 | C3/4, C4/5 | L5/S1 | 79 (C3–5), 80 (L5/S1) | 1, 1, 0 | ID HWS Cage, Titanium (2×), ProSpace Titanium |
| 9 | – | L4/5 | 47 | 1 | Telamon Titanium |
| 10 | – | L5/S1 | 27 | 1 | Telamon Titanium |
| 11 | C5/6 | – | 90 | 0 | ID HWS Cage, Titanium |
| 12 | – | L5/S1 | 112 | 0 | Diapason Titanium |
| 13 | – | L4/5 | 19 | 0 | Telamon Titanium |
| 14 | – | L4/5 | 100 | 0 | ProSpace Titanium |
| 15 | C5/6, C6/7 | – | 34 (2×) | 0, 0 | ID HWS Cage, Titanium (2×) |
| 16 | – | L5/S1 | 116 | 1 | Harms Titanium |
| 17 | – | L5/S1 | 74 | 1 | ProSpace Titanium |
| 18 | C5/6 | – | 84 | 1 | ID HWS Cage, Titanium |
| 19 | C5/6 | L3/4 | 91 (C5/6), 106 (L3/4) | 0, 0 | ID HWS Cage, Titanium, ProSpace Titanium |
| 20 | – | L5/S1 | 14 | 1 | ProSpace Titanium |
ID Implant design
aMaterial named includes registered trademarks ®
bKZC Karl Zweifel Cage
Radiochemistry
18F-fluoride was produced by proton irradiation of 18O-enriched water (RWE Nukem) in a cyclotron (PETtrace 200, GE Medical systems). After an irradiation for other 18F tracers, the cyclotron target was rinsed with water for injection to recover the remaining 18F-fluoride. The recovered amount was sufficient for up to eight patients. The 18F-fluoride in the target flush water was then purified and formulated in 0.9% sodium chloride for injection by an automated synthesis unit (FASTlab, GE Medical systems). The quality control for the sodium 18F-fluoride injection solution was according to the European Pharmacopoeia. The radiochemical and radionuclide purity was >98.5 and >99.9%, respectively.
Fluoride PET/CT scanning
We used a combined PET/CT system (Discovery RX or Discovery STE, GE Healthcare, Milwaukee, WI). This device integrates a PET scanner with a multi-slice helical CT (16 or 64 slices) and permits the acquisition of coregistered CT and PET images in the same session. Scanning started approximately 30–45 min after the i.v. injection of a dose of 97–217 MBq, mean 161 MBq of 18F-fluoride. Patients were examined in supine position. Immediately following the low-dose CT acquisition (FOV 50 cm, 80 mA, 120 kV, slice thickness 3.75 mm, 0.5 s rotation time, standard reconstruction type), 3D-PET emission data were acquired for 1.5 and 2 min/bed position, respectively. The CT data were used for attenuation correction and images were reconstructed using a fully 3D iterative algorithm (VUE Point HD).
Additionally, a dedicated thin-slice CT (0.625 mm), FOV 50 cm, 0.5 s rotation time, smartmA (maximum 440 and 700 mA), 120 kV, was acquired optionally covering the fused region (standard and bone reconstruction type).
Diagnostic thin-slice CTs were available of cervical cages in 3/8 patients and of lumbar cages in all 15 patients. The acquired images were postprocessed with a dedicated software (Volume Viewer PET/CT, AW 4.4 workstation, GE Healthcare) providing multiplanar reformatted images of PET alone, CT alone and fused PET/CT with linked cursors.
PET/CT evaluation
PET/CT images were analyzed in consensus by a double-board certified radiologist and nuclear physician with special training in musculoskeletal radiology and 5 years experience in PET/CT reading and one board certified radiologist with 1 year experience in PET/CT reading. The readers were blinded regarding the results of any previous imaging. Attenuation-corrected PET images as well as fused PET/CT images were used for analysis, using the CT for anatomical correlation. Increased 18F-fluoride uptake around cages higher than normal appearing bone was interpreted as pathologic regardless of pathological changes on CT.
Statistical evaluation
Evaluation was done using nonparametric procedures in SAS 9.2. For comparisons between groups, Wilcoxon two-sample tests were applied using normal approximation to Z. Values for one-sided tests are displayed considering the alternative hypothesis of shorter time distance between intervention and PET/CT scan in patients with increased 18F-fluoride uptake around cages.
Results
PET/CT findings
In 12/20 (60%) patients, increased 18F-fluoride uptake around intercorporal fusion material was found. 15/30 (50%) cages showed increased fluoride uptake. Median time between intervention and PET/CT in cages with increased uptake was 37 months (2–116 months, N = 15, interquartile range = 62), median time between intervention and PET/CT in those cages without increased uptake was 91 months (19–112 months, N = 15, interquartile range = 67), p (Wilcoxon) = 0.01 (one-sided) (Table 2).
Analyzing cervical and lumbar intercorporal fusions separately, there were 7/13 (54%) cervical cages showing increased uptake and 8/17 (47%) lumbar cages with increased uptake. Median time between intervention and PET/CT in cervical cages with increased uptake was 79 months (30–92 months, N = 7, interquartile range = 54), median time between intervention and PET/CT in cervical cages without increased uptake was 90.5 months (34–92 months, N = 6, interquartile range = 58), p (Wilcoxon) = 0.14 (one-sided). Median time between intervention and PET/CT in lumbar cages with increased uptake was 22 months (2–116 months, N = 8, interquartile range = 47), median time between intervention and PET/CT in lumbar cages without increased uptake was 100 months (19–112 months, N = 9, interquartile range = 37), p (Wilcoxon) = 0.02 (one-sided).
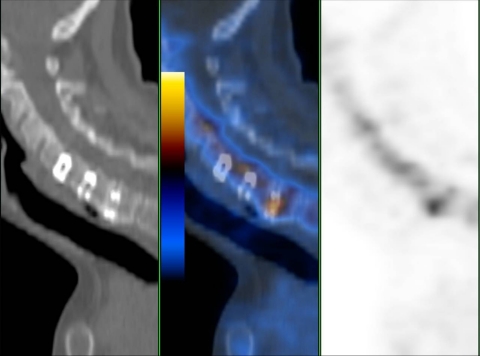
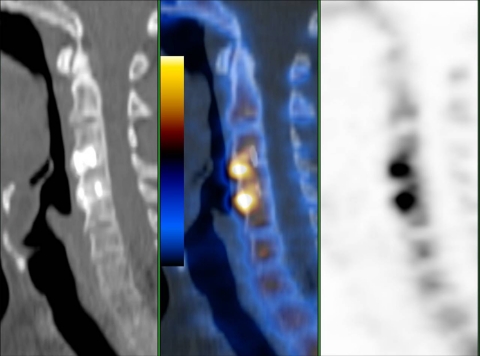
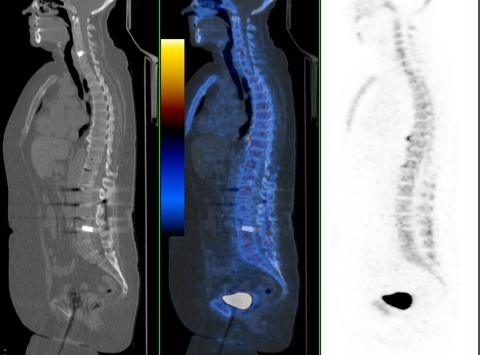
Regarding cervical intercorporal fusions, there were four patients with more than one intervertebral fusions, three with two adjacent segments either both with or without increased uptake. One patient had received three adjacent intercorporal fusions of which only the lowest showed increased uptake (Figs. 1, 2, 3).
Fig. 1.
64-year-old female patient 92 months postoperatively with the lowest of three cervical cages (C4/5, C5/6, C6/7) showing increased fluoride uptake (patient no. 1). Sagittal low-dose CT, fused PET/CT, PET
Fig. 2.
52-year-old male patient 79 months postoperatively with both cervical cages (C3/4, C4/5) showing increased uptake (patient no. 8). Sagittal low-dose CT, fused PET/CT, PET
Fig. 3.
48-year-old female patient 34 months postoperatively with no increased uptake around cervical cages (C5/6, C6/7) (patient no. 15). Sagittal low-dose CT, fused PET/CT, PET
Regarding lumbar intercorporal fusions, there were two patients with two intercorporal fusions showing either both no increased uptake or one an increased uptake (Figs. 4, 5). Three patients had received both cervical and lumbar intercorporal fusions only one of them showing no increased uptake in both regions (Fig. 6).
Fig. 4.
55-year-old female patient 102 and 35 months postoperatively with no increased uptake around both lumbar/lumbosacral cages (L4/5, L5/S1) (patient no. 5). Sagittal low-dose CT, fused PET/CT, PET
Fig. 5.
70-year-old female patient 2 and 69 months postoperatively with increased uptake around one lumbar cage (L2/3) and no increased uptake around the other lumbar cage (L4/5) (patient no. 7). Sagittal low-dose CT, fused PET/CT, PET. Note additional increased uptake in fractured end-plate L1
Fig. 6.
59-year-old female patient 91 and 106 months postoperatively with no increased uptake either around her cervical (C5/6) or lumbar cage (L3/4) (patient no 19). Sagittal low-dose CT, fused PET/CT, PET
Discussion
This study shows that even in those cervical and lumbar cages with a time interval of more than 1 year between surgery and fluoride PET/CT, increased 18F-fluoride uptake can be observed. The longest time interval in lumbar cages with increased uptake was 116 months (almost 10 years) and in cervical cages 92 months (almost 8 years), though there was a significant difference in median time between PET/CT and last intercorporal intervention between the group of cages with and without increased uptake (p = 0.01). If one takes the group of cervical and lumbar cages separately, only the group of lumbar cages shows a significant difference in median time between PET/CT and last intercorporal intervention (p = 0.14 in cervical cages, p = 0.02 in lumbar cages). Median time between PET/CT and last intercorporal intervention in cages with increased uptake is 37 months in all cages, 79 months in cervical and 22 months in lumbar cages. In contrast, median time between PET/CT and last intercorporal intervention in cages without increased uptake is 91 months in all cages, 90.5 months in all cervical and 100 months in all lumbar cages. This is a small study group and it needs to be verified whether incorporation of cervical cages indeed takes longer than in lumbar cages. These results show that even many years after cage implantation, there can be increased fluoride uptake which is likely an expression of increased stress, overcharge and microinstability even in morphologically unsuspicious segments. It is also possible that cages show increased uptake after having formerly been metabolically silent due to secondary loosening. This information is only obtained by the functional PET part. Until now, most studies focus on morphological imaging techniques to evaluate the healing process of intercorporal fusions. Obviously, there seems to be no uniform radiological criteria for assessing intercorporal fusion by plain radiographs or CT [10, 15–18]. 18F-fluoride PET/(CT) on the contrary has mostly been used in the assessment of malignant bone abnormalities [19–23]. However, promising results are also found in benign bone disorders, e.g. in the spine [11]. Considering our study results, 18F-fluoride PET/CT might potentially play an increasing role in the evaluation of the postoperative spine, supporting and complementing diagnostic criteria to assess intercorporal fusion after surgery. The supplement of PET to CT information in this study seems to help either to support diagnosis of non-fusion or to confirm the diagnosis of complete fusion. As 18F-fluoride is taken up to form the mineral fluorapatite at the surface of bone crystals especially at sites of bone remodeling with high turnover [14], segments with increased uptake around cages compared to adjacent bony structures might be considered as non-fused and those with the same uptake as fused in a metabolic sense. Hence, 18F-fluoride PET/CT possibly has an impact on therapeutic decisions. By avoiding unnecessary surgery, costs would decrease [24].
Although we did not correlate increased uptake with pain in the present study, it is possible that fluoride PET/CT can provide additional functional information to explain persistent pain in patients after intercorporal fusion surgery. In this study group, no difference was made concerning different cage types or graft material, due to the limited number and as only titanium containing cages and autologous grafts were used for fusion. A next step would be to compare fusion rates in different cage types and grafts (autologous, allogenic, bone graft substitutes) [25–30].
This study has several limitations. The study group is limited. No correlation with surgical re-exploration was done. Patients had mostly more than one spinal surgery (Table 1). Therefore, a bias concerning study population cannot be excluded. Also, only attenuation-corrected images were evaluated. Nevertheless, it was possible to differentiate cages with and without surrounding uptake in one patient (Figs. 1, 5).
Additional non-attenuation-corrected images might help diagnosing cases with rather faint surrounding uptake. Furthermore, it would be of interest to differentiate fusion rates in cages with and without additional (multisegmental) anterior or posterior fusion.
The effective dose equivalent for 18F-fluoride is 0.023 mSv/MBq, which corresponds to a maximum effective dose equivalent of about 5 mSv in this study [31]. With this protocol, the radiation burden of a fluoride PET/CT is slightly superior to conventional SPECT/CT [12]. An administered activity of 100–200 MBq (corresponding to an effective dose equivalent of about 2.3–4.6 mSv) is quite adequate to provide diagnostic images. Another advantage is the short uptake time of 18F-fluoride allowing imaging quickly after administration [13]. One clear limitation is the limited availability of 18F-fluoride and number of PET/CT systems as well as the higher incremental costs of 18F-fluoride PET compared to planar and SPECT bone scintigraphy (BS). Nevertheless, 18F-fluoride PET/(CT) is an imaging modality which outperforms SPECT BS at least regarding spatial resolution and generates increasing interest with the worldwide shortage of molybdenum supply [12, 14, 32, 33].
Conclusion
Even around cages with a long time interval between surgery and fluoride PET/CT imaging (close to 8 years in cervical cages and 10 years in lumbar cages), increased uptake could be observed possibly indicating increased stress/microinstability and thus missing/incomplete osseous fusion.
This study was approved by the Institutional Review Board (IRB) and Swissmedic was duly notified. Amendments to the protocol for this study, suppressing bone scans and extending the number of subjects were also approved by the IRB; however, it was omitted to notify Swissmedic about these amendments.
Acknowledgments
We thank Sabine Knöfel for all technical support.
Conflict of interest None of the authors has any potential conflict of interest .
References
- 1.Song KJ, Taghavi CE, Hsu MS, Lee KB, Kim GH, Song JH (2010) Plate augmentation in anterior cervical discectomy and fusion with cage for degenerative cervical spinal disorders. Eur Spine J. doi:10.1007/s00586-010-1283-3 [DOI] [PMC free article] [PubMed]
- 2.Carragee EJ, Hurwitz EL, Cheng I, Carroll LJ, Nordin M, Guzman J, Peloso P, Holm LW, Cote P, Hogg-Johnson S, van der Velde G, Cassidy JD, Haldeman S (2008) Treatment of neck pain: injections and surgical interventions: results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine (Philadelphia, PA, 1976) 33:S153–S169. doi:10.1097/BRS.0b013e31816445ea [DOI] [PubMed]
- 3.Hahnel H, Muschik M, Zippel H, Gutsche H. Lumbar segmental spondylodesis—isolated ventral or combined dorsoventral? A comparison of results. Z Orthop Ihre Grenzgeb. 1991;129:197–203. doi: 10.1055/s-2008-1040183. [DOI] [PubMed] [Google Scholar]
- 4.Lied B, Roenning PA, Sundseth J, Helseth E. Anterior cervical discectomy with fusion in patients with cervical disc degeneration: a prospective outcome study of 258 patients (181 fused with autologous bone graft and 77 fused with a PEEK cage) BMC Surg. 2010;10:10. doi: 10.1186/1471-2482-10-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lusins JO, Danielski EF, Goldsmith SJ. Bone SPECT in patients with persistent back pain after lumbar spine surgery. J Nucl Med. 1989;30:490–496. [PubMed] [Google Scholar]
- 6.Even-Sapir E, Martin RH, Mitchell MJ, Iles SE, Barnes DC, Clark AJ. Assessment of painful late effects of lumbar spinal fusion with SPECT. J Nucl Med. 1994;35:416–422. [PubMed] [Google Scholar]
- 7.Slizofski WJ, Collier BD, Flatley TJ, Carrera GF, Hellman RS, Isitman AT. Painful pseudarthrosis following lumbar spinal fusion: detection by combined SPECT and planar bone scintigraphy. Skel Radiol. 1987;16:136–141. doi: 10.1007/BF00367762. [DOI] [PubMed] [Google Scholar]
- 8.Inamdar DN, Alagappan M, Shyam L, Devadoss S, Devadoss A. Posterior lumbar interbody fusion versus intertransverse fusion in the treatment of lumbar spondylolisthesis. J Orthop Surg (Hong Kong) 2006;14:21–26. doi: 10.1177/230949900601400106. [DOI] [PubMed] [Google Scholar]
- 9.France JC, Yaszemski MJ, Lauerman WC, Cain JE, Glover JM, Lawson KJ, Coe JD, Topper SM (1999) A randomized prospective study of posterolateral lumbar fusion. Outcomes with and without pedicle screw instrumentation. Spine (Philadelphia, PA, 1976) 24:553–560 [DOI] [PubMed]
- 10.Madan S, Boeree NR. Outcome of posterior lumbar interbody fusion versus posterolateral fusion for spondylolytic spondylolisthesis. Spine (Philadelphia, PA, 1976) 2002;27:1536–1542. doi: 10.1097/00007632-200207150-00011. [DOI] [PubMed] [Google Scholar]
- 11.Gamie S, El-Maghraby T. The role of PET/CT in evaluation of facet and disc abnormalities in patients with low back pain using (18)F-fluoride. Nucl Med Rev Cent East Eur. 2008;11:17–21. [PubMed] [Google Scholar]
- 12.Grant FD, Fahey FH, Packard AB, Davis RT, Alavi A, Treves ST. Skeletal PET with 18F-fluoride: applying new technology to an old tracer. J Nucl Med. 2008;49:68–78. doi: 10.2967/jnumed.106.037200. [DOI] [PubMed] [Google Scholar]
- 13.Groves AM, Win T, Haim SB, Ell PJ. Non-[18F]FDG PET in clinical oncology. Lancet Oncol. 2007;8:822–830. doi: 10.1016/S1470-2045(07)70274-7. [DOI] [PubMed] [Google Scholar]
- 14.Even-Sapir E, Mishani E, Flusser G, Metser U. 18F-fluoride positron emission tomography and positron emission tomography/computed tomography. Semin Nucl Med. 2007;37:462–469. doi: 10.1053/j.semnuclmed.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 15.Chafetz N, Cann CE, Morris JM, Steinbach LS, Goldberg HI, Ax L. Pseudarthrosis following lumbar fusion: detection by direct coronal CT scanning. Radiology. 1987;162:803–805. doi: 10.1148/radiology.162.3.3809497. [DOI] [PubMed] [Google Scholar]
- 16.Buchowski JM, Liu G, Bunmaprasert T, Rose PS, Riew KD (2008) Anterior cervical fusion assessment: surgical exploration versus radiographic evaluation. Spine (Philadelphia, PA, 1976) 33:1185–1191. doi:10.1097/BRS.0b013e318171927c [DOI] [PubMed]
- 17.Carter JD, Swearingen AB, Chaput CD, Rahm MD. Clinical and radiographic assessment of transforaminal lumbar interbody fusion using HEALOS collagen-hydroxyapatite sponge with autologous bone marrow aspirate. Spine J. 2009;9:434–438. doi: 10.1016/j.spinee.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 18.Carreon LY, Glassman SD, Schwender JD, Subach BR, Gornet MF, Ohno S. Reliability and accuracy of fine-cut computed tomography scans to determine the status of anterior interbody fusions with metallic cages. Spine J. 2008;8:998–1002. doi: 10.1016/j.spinee.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 19.Schirrmeister H, Guhlmann A, Kotzerke J, Santjohanser C, Kuhn T, Kreienberg R, Messer P, Nussle K, Elsner K, Glatting G, Trager H, Neumaier B, Diederichs C, Reske SN. Early detection and accurate description of extent of metastatic bone disease in breast cancer with fluoride ion and positron emission tomography. J Clin Oncol. 1999;17:2381–2389. doi: 10.1200/JCO.1999.17.8.2381. [DOI] [PubMed] [Google Scholar]
- 20.Schirrmeister H, Glatting G, Hetzel J, Nussle K, Arslandemir C, Buck AK, Dziuk K, Gabelmann A, Reske SN, Hetzel M. Prospective evaluation of the clinical value of planar bone scans, SPECT, and (18)F-labeled NaF PET in newly diagnosed lung cancer. J Nucl Med. 2001;42:1800–1804. [PubMed] [Google Scholar]
- 21.Even-Sapir E, Metser U, Mishani E, Lievshitz G, Lerman H, Leibovitch I. The detection of bone metastases in patients with high-risk prostate cancer: 99mTc-MDP planar bone scintigraphy, single- and multi-field-of-view SPECT, 18F-fluoride PET, and 18F-fluoride PET/CT. J Nucl Med. 2006;47:287–297. [PubMed] [Google Scholar]
- 22.Beheshti M, Vali R, Waldenberger P, Fitz F, Nader M, Loidl W, Broinger G, Stoiber F, Foglman I, Langsteger W. Detection of bone metastases in patients with prostate cancer by 18F fluorocholine and 18F fluoride PET–CT: a comparative study. Eur J Nucl Med Mol Imag. 2008;35:1766–1774. doi: 10.1007/s00259-008-0788-z. [DOI] [PubMed] [Google Scholar]
- 23.Schirrmeister H, Guhlmann A, Elsner K, Kotzerke J, Glatting G, Rentschler M, Neumaier B, Trager H, Nussle K, Reske SN. Sensitivity in detecting osseous lesions depends on anatomic localization: planar bone scintigraphy versus 18F PET. J Nucl Med. 1999;40:1623–1629. [PubMed] [Google Scholar]
- 24.Etminan M, Girardi FP, Khan SN, Cammisa FP., Jr Revision strategies for lumbar pseudarthrosis. Orthop Clin North Am. 2002;33:381–392. doi: 10.1016/S0030-5898(02)00005-6. [DOI] [PubMed] [Google Scholar]
- 25.Park HW, Lee JK, Moon SJ, Seo SK, Lee JH, Kim SH (2009) The efficacy of the synthetic interbody cage and Grafton for anterior cervical fusion. Spine (Philadelphia, PA, 1976) 34:E591–E595. doi:10.1097/BRS.0b013e3181ab8b9a [DOI] [PubMed]
- 26.Shen HX, Buchowski JM, Yeom JS, Liu G, Lin N, Riew KD (2010) Pseudarthrosis in multilevel anterior cervical fusion with rhBMP-2 and allograft: analysis of one hundred twenty-seven cases with minimum two-year follow-up. Spine (Philadelphia, PA, 1976) 35:747–753. doi:10.1097/BRS.0b013e3181bc3420 [DOI] [PubMed]
- 27.Niu CC, Liao JC, Chen WJ, Chen LH (2010) Outcomes of interbody fusion cages used in 1 and 2-levels anterior cervical discectomy and fusion: titanium cages versus polyetheretherketone (PEEK) cages. J Spinal Disord Technol. doi:10.1097/BSD.0b013e3181af3a84 [DOI] [PubMed]
- 28.Magin MN, Delling G (2001) Improved lumbar vertebral interbody fusion using rhOP-1: a comparison of autogenous bone graft, bovine hydroxylapatite (Bio-Oss), and BMP-7 (rhOP-1) in sheep. Spine (Philadelphia, PA, 1976) 26:469–478 [DOI] [PubMed]
- 29.Suchomel P, Barsa P, Buchvald P, Svobodnik A, Vanickova E. Autologous versus allogenic bone grafts in instrumented anterior cervical discectomy and fusion: a prospective study with respect to bone union pattern. Eur Spine J. 2004;13:510–515. doi: 10.1007/s00586-003-0667-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Berven S, Tay BK, Kleinstueck FS, Bradford DS (2001) Clinical applications of bone graft substitutes in spine surgery: consideration of mineralized and demineralized preparations and growth factor supplementation. Eur Spine J 10(Suppl 2):S169–S177. doi:10.1007/s005860100270 [DOI] [PMC free article] [PubMed]
- 31.Hoegerle S, Juengling F, Otte A, Altehoefer C, Moser EA, Nitzsche EU. Combined FDG and [F-18]fluoride whole-body PET: a feasible two-in-one approach to cancer imaging? Radiology. 1998;209:253–258. doi: 10.1148/radiology.209.1.9769840. [DOI] [PubMed] [Google Scholar]
- 32.Stafford N. Isotope shortage is limiting nuclear medicine across Europe. BMJ. 2008;337:a1575. doi: 10.1136/bmj.a1575. [DOI] [PubMed] [Google Scholar]
- 33.Perkins A, Hilson A, Hall J. Global shortage of medical isotopes threatens nuclear medicine services. BMJ. 2008;337:a1577. doi: 10.1136/bmj.a1577. [DOI] [PubMed] [Google Scholar]