Abstract
Using MRSA isolates submitted to our hospital microbiology laboratory January 2001–March 2010 and the number of our emergency department (ED) visits, quarterly community-associated (CA) and hospital-associated (HA) MRSA infections were modeled using Poisson regressions. For pediatric patients, approximately 1.85x (95% CI 1.45x–2.36x, adj. p<0.0001) as many CA-MRSA infections per ED visit occurred in the second two quarters as occurred in the first two quarters. For adult patients, 1.14x (95% CI 1.01x–1.29x, adj.p = 0.03) as many infections per ED visit occurred in the second two quarters as in the first two quarters. Approximately 2.94x (95% CI 1.39x–6.21x, adj.p = 0.015) as many HA-MRSA infections per hospital admission occurred in the second two quarters as occurred in the first two quarters for pediatric patients. No seasonal variation was observed among adult HA-MRSA infections per hospital admission. We demonstrated seasonality of MRSA infections and provide a summary table of similar observations in other studies.
Introduction
Seasonal variation in Staphylococcus aureus infections is controversial. Some studies have demonstrated a highly significant surge of such infections during the warmest months and during autumn in temperate and tropical settings [1]–[3]. However, a recent study did not find such a correlation [4]. We have observed peaks of community-associated methicillin-resistant S. aureus (CA-MRSA) infections during the summer and autumn and we set out to determine if there is a correlation between MRSA infections in patients of all ages and seasonality.
Results
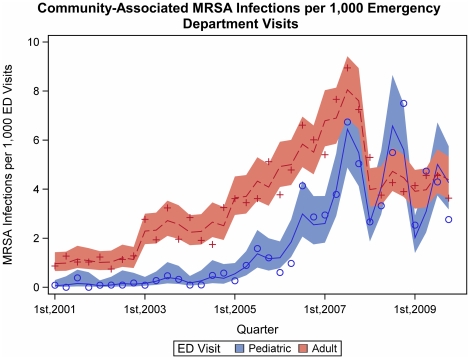
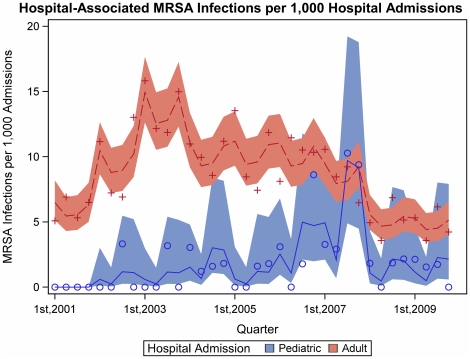
We found strong evidence of a seasonal effect in the rate of CA-MRSA isolates per ED visit in both pediatric and adult patients (Figure 1). For pediatric patients, a mean of approximately 1.85x (95% CI 1.45x–2.36x, adj. p<0.0001) as many CA-MRSA infections per ED visit occurred in the second two quarters as occurred in the first two quarters over the study period. For adult patients, the effect per number of ED visits was smaller (adj.p = 0.001), which indicated 1.14x (95% CI 1.01x–1.29x, adj.p = 0.03) as many infections per ED visit in the second two quarters as in the first two quarters. Hospital-associated MRSA (HA-MRSA) infections in pediatric patients had seasonal variation (Figure 2). A mean of approximately 2.94x (95% CI 1.39x–6.21x, adj.p = 0.015) as many HA-MRSA infections per hospital admission occurred in the second two quarters as occurred in the first two quarters over the study period. This reflected greater seasonal variation than we observed among adult HA-MRSA infections per hospital admission (adj.p = 0.011), in which the second two quarters did not differ from the first two quarters, 1.00x (95% CI 0.89x–1.12x, adj.p = 0.97).
Figure 1. Community-associated MRSA infections along with the model predictions and 95% confidence intervals.
Figure 2. Hospital-associated MRSA infections along with the model predictions and 95% confidence intervals.
Discussion
Seasonality of staphylococcal infections is not noted in many textbook chapters or review articles. Nevertheless, several investigators have demonstrated seasonal variation in S. aureus infections, particularly skin infections, with a preponderance of infections during the summer and autumn (Tables 1 and 2). As noted in Tables 1 and 2, seasonal variability has been observed in pediatric and adult patients in temperate and tropical climates. We found a two to three-fold increased incidence of MRSA infections in pediatric patients during the second two quarters over the last decade. A lesser degree of seasonal variation was observed in adult CA-MRSA infections. It is difficult to explain the seasonality of pediatric HA-MRSA infections; however, we suspect that many of these patients were colonized with MRSA at the time of hospitalization and infections developed while hospitalized. Since 90% of pediatric hospital visits in Rhode Island are at our hospital, our data represents the vast majority of pediatric MRSA infections seen at local hospitals.
Table 1. Seasonality and Staphylococcus aureus Mixed Infections, Bacteremia, and Upper Extremity Infections.
| Type of Infection | Age | Locale | Seasonality | Author |
| CA*-MRSA† (USA 300 & USA 400 strains) infections | All | Iowa | Peak incidence: Summer (47% of cases occurred Jun 21-Sep 22; p<0·001) | [1] |
| CA-MRSA severe infections | All | Georgia | Peak incidence: Summer (∼34% of casesoccurred Jul-Sep; ∼45% occurred Jul-Oct) | [5] |
| CA-MRSA infections in military recruits | Adult | Georgia | Peak incidence: Summer (∼ 41% of cases occurred Jul-Sep; ∼54% of cases occurred Jul-Oct) | [6] |
| CA- and HA‡-S. aureus infections | All | Scotland | Peak incidence: ‘Spring seasonal variation of MRSA’was observed but not for MSSA§ | [7] |
| CA- and HA-S. aureus infections requiring hospitalization | Adult | Maryland | Peak incidence: Jul-Sep (IRR 1·04; p = 0·5) | [4] |
| CA-S. aureus infections | Pediatric | Texas | Monthly peak incidence: 2002 = Jul; 2003 = Aug; 2004 = May | [8] |
| CA-S. aureus infections | Pediatric | Greece | Peak incidence: Summer (72% of cases occurred Jul-Sep) | [9] |
| CA-S. aureus bacteremia | All | Connecticut | Peak incidence: Jul-Sep (RR 1·0; p = non-significant) | [10] |
| CA-S. aureus bacteremia | Adult | Taiwan | Peak incidence: ‘Late autumn and early winter’(26% of cases occurred Jul-Sep; 42% of cases occurred Jul-Oct) | [11] |
| S. aureus bacteremia | All | Massachusetts | Peak incidence: ‘There was no peak of incidence atany season of the year’ | [12] |
| S. aureus pneumonia and secondary bacteremia | All | Maryland | Peak incidence: Summer and winter (30% of cases occurred May-June; 30% of cases occurred Nov-Dec) | [13] |
| Upper extremity (PVL gene positive) S. aureus infections | All | Greece | Peak incidence: Summer (56% of cases occurred Jun-Aug) | [14] |
*CA = Community-associated;
MRSA = Methicillin-resistant S. aureus;
HA = Hospital-associated;
MSSA = Methicillin-susceptible S. aureus.
Table 2. Seasonality and Staphylococcus aureus Skin Infections.
| Type of Infection | Age | Locale | Seasonality | Author |
| CA*-associated S. aureus ‘boil infections’ | All | Nigeria | Peak incidence: 33% of cases occurred during warmest recorded months (Jan–Mar) | [15] |
| CA-associated pyoderma | All | India | Peak incidence: Summer (40% of cases occurred Jun–Aug) | [16] |
| CA-associated pyoderma | All | Malawi | Peak incidence: Summer (Dec–Apr) | [17] |
| CA-associated pyoderma | Pediatric | India | Peak incidence: 68% of cases ‘reported during the hot and humid months of Jun–Sep' | [18] |
| Dermatitis cruris pustulosis exacerbation (87% culture-positive for S. aureus) | All | India | Peak incidence: Summer (87% of cases) | [19] |
| Impetigo | Pediatric | Nether-lands | Peak incidence in 1987 & 2001: Summer (‘incidence was significantly higher in summer’) | [20] |
| Impetigo | Pediatric | United Kingdom | Peak incidence: ‘Late Summer’ (∼37% of cases Jul–Sep; seasonal effect [p = 0·02]; correlation between impetigo andmean temperature the previous month [r = 0·55; p = 0·001]) | [3] |
| Impetigo | Pediatric | United Kingdom | Peak incidence: Autumn (Oct peak in 4 of 5 years studied); ∼1–2 months after the month with the highest average temperature | [21] |
| Impetigo | Pediatric | Alabama | Peak Incidence: Summer (33% of cases occurred in Aug; monitored Jul–Jan rather than the calendar year) | [22] |
| Impetigo | Pediatric | Australia | Peak incidence: 79% of cases occurred in summer and autumn | [23] |
| Impetigo | Pediatric | Pakistan | Peak incidence: Summer (2–3 fold increased incidence/100 person-wks of impetigo in Jul compared with May, Sep, or Oct) | [24] |
| Impetigo bullosa due to fusidic acid-resistant S. aureus | Pediatric | Norway | Peak incidence: ‘Marked seasonal fluctuation with the highest prevalence in early autumn’ (52% of 2001 cases in Aug) | [25] |
*CA = Community-associated.
We believe that it is the sequence of 3rd and 4th quarters which is important in demonstrating the peak in MRSA infections in temperate regions rather than just the warmest quarter of the year. We reviewed meteorologic data for Rhode Island during the decade of our study period and found that the 2nd quarter was warmer, on average, than the 4th quarter. Thus, we believe that it is the sequence of 3rd and 4th quarters that is important and not the 3rd quarter in isolation. We previously demonstrated transmission of an identical MRSA pulsotype in a large extended family living in different homes over 2–4 weeks [26]. One study found a correlation between impetigo and the mean ambient temperature during the previous month [r = 0·55; p = 0·001]; 3). Another study demonstrated a 1–2 month lag between peak temperature and peak incidence of impetigo in children and this was ascribed to more insect bites during peak temperatures [21]. Thus, an increased incidence of infection in autumn (4th quarter), may reflect a lag between Staphylococcal colonization and subsequent infection. Additionally, an increased incidence of viral respiratory infections in autumn, possibly reflecting transmission in more confined settings such as schools, may add to greater S. aureus transmission and subsequent infection during this time [27]. Hydration of the stratum corneum of the skin is an important in promoting microbial growth [28]. Hydration would be maximized when high temperatures promote sweat production and in high relative humidity. The presence of both factors may be critically important in providing the environmental conditions that facilitate heavy growth of S. aureus on skin [16]. Nevertheless, one investigator found an inverse correlation between humidity and S. aureus skin infections [15]. Some investigators did not observe any significant seasonality of S. aureus infections [4], [10], [12]. Since many reports of seasonality of S. aureus infections involve skin infections, it may be that these investigators had fewer such infections in their patient population thus masking the effect.
Grassley and Fraser [29] describe variables that explain seasonality of infectious diseases: pathogen survival outside the host; host behavior; host immune function; and abundance of vectors and non-human hosts. There is a correlation between the quantity of S. aureus in the nares and on clothing [30] and a correlation between the quantity of S. aureus in the nares, on skin, and the quantity of S. aureus in the surrounding air [30]–[32]. Increased S. aureus transmission during the summer months may reflect a greater density of this microbe on the skin, nares, throat, and/or perineum during warmer, and often more humid conditions [28], it may reflect other environmental conditions conducive to disease spread, or both. Some authors have not observed seasonal variation in S. aureus nasopharyngeal carriage [33]–[35] but these studies may have been underpowered to find such a difference and they did not assess colonization of other body sites.
It is hoped that the current study will prompt further investigation into the seasonality of S. aureus infections to better understand the biologic basis for this observation.
Methods
We collected microbiologic data on all clinical (i.e., non-surveillance) MRSA isolates submitted to our hospital microbiology laboratory between January 2001 and March 2010. MRSA isolates were identified using standard microbiologic methods. We also determined the number of visits to our adult and pediatric emergency departments (ED) during this time. We defined CA-MRSA as isolates obtained within 48 hours of hospitalization and HA-MRSA based on isolates obtained after 48 hours of hospitalization, or for surgical wound infections, those who had their procedure within the prior 30 days.
Quarterly CA-MRSA and HA-MRSA infection counts were modeled using Poisson regressions, offset with the log number of ED visits or log number of admissions with lengths of stay of three or more days, respectively, to adjust for changes in the number of patients seen. For CA-MRSA infections, the log number of ED visits for each quarter was used as an offset variable, making the prediction rates per ED visit. Models included effects for ED visits (pediatric vs. adult), categorical year, categorical quarter, and the interactions between ED and year, and ED and quarter. For HA-MRSA infections, the log number of hospital admissions with lengths of stay of three or more days for each quarter was used as an offset variable, making the prediction rates hospital admission. Models included effects for hospital admission of three or more days (pediatric vs. adult), categorical year, categorical quarter, and the interactions between hospital admission and year, and hospital admission and quarter. Models and hypothesis tests were adjusted for slight overdispersion based on the Pearson Chi-Square. Complex comparisons were used to test whether quarters 1 and 2 were significantly different from quarters 3 and 4 within each (i.e., adult or pediatric) ED visit or hospital admission and to test for a difference between ED visit or hospital admission in the size of these effects. Alpha was maintained at 0.05 across all three hypothesis tests using the Holm test (alpha per comparison = 0.0167). This study was approved by the Rhode Island Hospital Institutional Review Board. Informed consent was not obtained as patient-specific data is not reported and data had already been abstracted in our infection control software program.
Acknowledgments
The authors acknowledge Nicole Lundstrom for administrative assistance in preparing the manuscript.
Footnotes
Competing Interests: Dr. Mermel has served as a consultant for 3M Healthcare and Sage. No other authors have any competing interest to disclose. This does not alter the authors' adherence to all the PLoS ONE policies on sharing data and materials.
Funding: The authors have no support or funding to report.
References
- 1.Van De Griend P, Herwaldt LA, Alvis B, DeMartino M, Heilmann K, et al. Community-associated methicillin-resistant Staphylococcus aureus, Iowa, USA. Emerg Infect Dis. 2009;15:1582–1589. doi: 10.3201/eid1510.080877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Szczesiul JM, Shermock KM, Murtaza UI, Siberry GK. No decrease in clindamycin susceptibility despite increased use of clindamycin for pediatric community-associated methicillin-resistant Staphylococcus aureus skin infections. Pediatr Infect Dis J. 2007;26:852–854. doi: 10.1097/INF.0b013e318124aa5c. [DOI] [PubMed] [Google Scholar]
- 3.Loffeld A, Davies P, Lewist A, Moss C. Seasonal occurrence of impetigo: a retrospective 8-year review (1996-2003). Clin Exp Dermatol. 2005;30:512–514. doi: 10.1111/j.1365-2230.2005.01847.x. [DOI] [PubMed] [Google Scholar]
- 4.Perencevich EN, McGregor JC, Shardell M, Furuno JP, Harris AD, et al. Summer peaks in the incidences of gram-negative bacterial infection -among hospitalized patients. Infect Control Hosp Epidemiol. 2008;29:1124–1131. doi: 10.1086/592698. [DOI] [PubMed] [Google Scholar]
- 5.Wiersma P, DAngelo MT, Daley WR, Tuttle J, Arnold KE, et al. Surveillance for severe community-associated methicillin-resistant Staphylococcus aureus infection. Epidemiol Infect. 2009;137:1674–1678. doi: 10.1017/S0950268809002490. [DOI] [PubMed] [Google Scholar]
- 6.Morrison-Rodriguez SM, Pacha LA, Patrick JE, Jordan NN. Community-associated methicillin-resistant Staphylococcus aureus infection at an army training installation. Epidemiol Infect. 2010;138:721–729. doi: 10.1017/S0950268810000142. [DOI] [PubMed] [Google Scholar]
- 7.Monnet DL, MacKenzie FM, Lopez-Lozano JM, Beyaert A, Camacho M, et al. Antimicrobial drug use and methicillin-resistant Staphylococcus aureus, Aberdeen, 1996-2000. Emerg Infect Dis. 2004;10:1432–1441. doi: 10.3201/eid1008.020694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaplan SL, Hulten KG, Gonzalez BE, Hammerman WA, Lamberth L, et al. Three-year surveillance of community-acquired Staphylococcus aureus infections in children. Clin Infect Dis. 2005;40:1785–1791. doi: 10.1086/430312. [DOI] [PubMed] [Google Scholar]
- 9.Sdougkos G, Chini V, Papanastasiou DA, Christodoulou G, Stamatakis E, et al. Community-associated Staphylococcus aureus infections and nasal carriage among children: molecular microbial data and clinical characteristics. Clin Microbiol Infect. 2008;14:995–1001. doi: 10.1111/j.1469-0691.2008.02064.x. [DOI] [PubMed] [Google Scholar]
- 10.Morin CA, Hadler JL. Population-based incidence and characteristics of community-onset Staphylococcus aureus infections with bacteremia in 4 Metropolitan Connecticut Areas, 1998. J Infect Dis. 2001;184:1029–1034. doi: 10.1086/323459. [DOI] [PubMed] [Google Scholar]
- 11.Chi CY, Wong WW, Fung CP, Yu KW, Liu CY. Epidemiology of community-acquired Staphylococcus aureus bacteremia. J Microbiol Immunol Infect. 2004;37:16–23. [PubMed] [Google Scholar]
- 12.Skinner D, Keefer CS. Significance of bacteremia caused by Staphylococcus aureus. Arch Intern Med. 1941;5:851–875. [Google Scholar]
- 13.Cluff LE, Reynolds RC, Page DL, Breckenridge JL. Staphylococcal bacteremia: demographic, clinical and mirobiological features of 185 cases. Trans Am Clin Climatol Assoc. 1968;79:205–215. [PMC free article] [PubMed] [Google Scholar]
- 14.Dailiana ZH, Rigopoulos N, Varitimidis SE, Poultsides L, Petinaki E, et al. Clinical and epidemiological features of upper-extremity infections caused by Staphylococcus aureus carrying the PVL gene: A four-year study in Greece. Med Sci Monit. 2008;14:CR511–514. [PubMed] [Google Scholar]
- 15.Elegbe IA. Influence of seasonal and weather variation on the incidence of coagulase positive staphylococci isolates among Nigerians with boil infections. J R Soc Health. 1983;103:118–119. doi: 10.1177/146642408310300308. [DOI] [PubMed] [Google Scholar]
- 16.Singh G. Heat, Humidity and Pyodermas. Dermatologica. 1973;147:342–347. doi: 10.1159/000251891. [DOI] [PubMed] [Google Scholar]
- 17.Kristensen JK. Scabies and pyoderma in Lilongwe, Malawi – prevalence and seasonal fluctuation. Int J Dermatol. 1991;30:699–702. doi: 10.1111/j.1365-4362.1991.tb02612.x. [DOI] [PubMed] [Google Scholar]
- 18.Kakar N, Kumar V, Mehta G, Sharma RC, Koranne RV. Clinico-bacteriological study of pyodermas in children. J Dermatol. 1999;26:288–293. doi: 10.1111/j.1346-8138.1999.tb03474.x. [DOI] [PubMed] [Google Scholar]
- 19.Kaimal S, D'Souza M, Kumari R, Parija SC, Sistla S, et al. Dermatitis cruris pustulosa et atrophicans revisited: our experience with 37 patients in South India. Int J Dermatol. 2009;48:1082–1090. doi: 10.1111/j.1365-4632.2009.04156.x. [DOI] [PubMed] [Google Scholar]
- 20.Koning S, Mohammedamin RS, van der Wouden JC, van Suijlekom-Smit LW, Schellevist FG, et al. Impetigo: incidence and treatment in Dutch general practice in 1987 and 2001-results from two national surveys. Br J Dermatol. 2006;154:239–243. doi: 10.1111/j.1365-2133.2005.06766.x. [DOI] [PubMed] [Google Scholar]
- 21.Elliot AJ, Cross KW, Smith GE, Burgess IF, Fleming DM. The association between impetigo, insect bites and air temperature: a retrospective 5-year study (1999-2003) using morbidity data collected from a sentinel general practice network database. Fam Pract. 2006;23:490–496. doi: 10.1093/fampra/cml042. [DOI] [PubMed] [Google Scholar]
- 22.Dillon HC., Jr Impetigo contagiosa: suppurative and non-suppurative complications. I. Clinical, bacteriologic, and epidemiologic characteristics of impetigo. Am J Dis Child. 1968;115:530–541. doi: 10.1001/archpedi.1968.02100010532002. [DOI] [PubMed] [Google Scholar]
- 23.Rogers M, Dorman DC, Gapes M, Ly J. A three-year study of impetigo in Sydney. Med J Aust. 1987;147:63–65. doi: 10.5694/j.1326-5377.1987.tb133260.x. [DOI] [PubMed] [Google Scholar]
- 24.Luby S, Agboatwalla M, Schnell BM, Hoekstra RM, Rahbar MH, et al. The effect of antimicrobial soap on impetigo incidence, Karachi, Pakistan. Am J Trop Med Hyg. 2002;67:430–435. doi: 10.4269/ajtmh.2002.67.430. [DOI] [PubMed] [Google Scholar]
- 25.Tveten Y, Jenkins A, Kristiansen BE. A fusidic acid-resistant clone of Staphylococcus aureus associated with impetigo bullosa is spreading in Norway. J Antimicrob Chemother. 2002;50:873–876. doi: 10.1093/jac/dkf217. [DOI] [PubMed] [Google Scholar]
- 26.Dietrich DW, Auld DB, Mermel LA. Community-acquired methicillin-resistant Staphylococcus aureus in southern New England children. Pediatrics. 2004;113:e347–352. doi: 10.1542/peds.113.4.e347. [DOI] [PubMed] [Google Scholar]
- 27.Bassetti S, Bischoff WE, Walter M, Bassetti-Wyss BA, Mason L, et al. Dispersal of Staphylococcus aureus into the air associated with a rhinovirus infection. Infect Control Hosp Epidemiol. 2005;26:196–203. doi: 10.1086/502526. [DOI] [PubMed] [Google Scholar]
- 28.Taplin D, Zaias N, Rebell G. Environmental influences on microbiology of the skin. Arch Environm Hlth. 1965;11:546–550. doi: 10.1080/00039896.1965.10664255. [DOI] [PubMed] [Google Scholar]
- 29.Grassly NC, Fraser C. Seasonal infectious disease epidemiology. Proc R Soc B. 2006;273:2541–2550. doi: 10.1098/rspb.2006.3604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.White A. Relation between quantitative nasal cultures and dissemination of staphylococci. J Lab Clin Med. 1961;58:273–277. [PubMed] [Google Scholar]
- 31.Ehrenkranz NJ. Person-to person transmission of staphylococcus aureus. Quantitative characterization of nasal carriers spreading infection. N Eng J Med. 1964;271:2 25–230. doi: 10.1056/NEJM196407302710503. [DOI] [PubMed] [Google Scholar]
- 32.Solberg CO. A study of carriers of staphylococcus aureus with regard to quantitative bacterial estimations. Acta Med Scand Suppl. 1965;436:1–96. [PubMed] [Google Scholar]
- 33.Noble WC, Valkenburg HA, Wolters HL. Carriage of Staphylococcus aureus in random samples of a normal population. J Hyg. 1967;65:567–573. doi: 10.1017/s002217240004609x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Harrison LM, Morris JA, Telford DR, Brown SM, Jones K. The nasopharyngeal bacterial flora in infancy: effects of age, gender, season, viral upper respiratory tract infection and sleeping position. FEMS Immunol Med Microbiol. 1999;25:19–28. doi: 10.1111/j.1574-695X.1999.tb01323.x. [DOI] [PubMed] [Google Scholar]
- 35.Levy RM, Leyden JJ, Margolis DJ. Colonisation rates of Streptococcus pyogenes and Staphylococcus aureus in the oropharynx of a young adult population. Clin Microbiol Infect. 2005;11:153–155. doi: 10.1111/j.1469-0691.2004.01042.x. [DOI] [PubMed] [Google Scholar]