Abstract
Background: Providing information that is congruent with patients’ needs is an important determinant for patient satisfaction and might also affect health-related quality of life (HRQoL) and anxiety and depression levels of cancer survivors.
Design: The authors systematically reviewed the available literature on the relationship between information provision and HRQoL, anxiety and depression. A PubMed literature search for original articles published until February 2010 was carried out. Twenty-five articles, all conducted between 1996 and 2009, which met the predefined inclusion criteria, were subjected to a quality checklist.
Results: Satisfied patients, patients with fulfilled information needs, and patients who experience less information barriers, in general have a better HRQoL and less anxiety and depression. Out of eight intervention studies that aimed to improve information provision, only one showed a positive association with better HRQoL.
Conclusion: Health care providers must pay more attention to patient-centred information provision. Additional research is needed to make definitive conclusions about information interventions as most results did not reach statistical significance due to methodological constraints. The quick development of the relatively young research field of patient-reported outcomes in cancer survivorship will make it possible to conduct better quality studies in the future.
Keywords: anxiety, depression, (health-related) quality of life; information provision; information needs; information satisfaction
introduction
The provision of information to patients is one of the most important factors of supportive cancer care across the whole cancer continuum. The goal of providing information is to prepare patients for their treatment, to increase adherence to therapy, to increase their abilities to cope with the illness and to promote recovery [1]. However, the results of a systematic review show that 6–93% of the cancer patients report adequate information provision as an unmet need throughout their cancer experience [2]. Patients frequently report barriers to receive the information needed [3]. Health care providers are often still reluctant to give the full amount of information about cancer and its treatment, while the majority of cancer patients want as much information as possible about their disease, treatment and rehabilitation [3]. The information needs of cancer patients vary by gender, age, cultural background, educational level, cancer type, stage of disease and coping style [4, 5]. Providing information that is congruent with patients’ needs is an important determinant for patient satisfaction and might also affect health-related quality of life (HRQoL) and anxiety and depression levels of cancer patients.
HRQoL is a multidimensional construct that covers the patients’ perceptions of his or her physical, emotional, social, and cognitive functions. HRQoL assessment is an important aspect of cancer care. HRQoL parameters providing prognostic information can facilitate clinical decision making in terms of better treatment selection for cancer patients [6–8]. Furthermore, cancer survivors often deal with adaptation problems and assessment of their HRQoL could help to improve aftercare [9]. Cancer survivors experience high levels of psychological distress, a range of feelings and emotions that people experience in reaction to cancer including depression and anxiety, with an important impact on HRQoL [10, 11]. In the past decade, the role of information provision in cancer care has been acknowledged. Several studies have investigated the relationship between information provision and HRQoL, anxiety and depression, but results seem inconsistent [12]. The evaluation of a possible relationship between HRQoL and information provision is difficult because of the conceptualisation of both constructs and methodological challenges in measuring these constructs. Throughout this review, information provision is defined as all cancer-related information provided by the health care provider/nurse in oral, written or other form. From the perspective of the patient, information provision is mostly measured in terms of ‘satisfaction with received information’, ‘barriers to receive information’,’ information needs’, ‘information quality’ and ‘information clarity’. Importantly, this review did not focus on information disclosure regarding the initial cancer diagnosis or end-of-life issues. The goal of our review was to provide a complete overview of the literature on the impact of information on the HRQoL, anxiety and depression levels of cancer survivors. We used the definition of the US National Coalition for Cancer Survivorship that defines a person as a survivor from the moment of diagnosis through the balance of his or her life (http://www.canceradvocacy.org/about/org/). We hypothesise that better information provision (fulfilled needs, less barriers, clear and high-quality information) is related to higher satisfaction levels of cancer survivors regarding information that may impact HRQoL, especially mental health, and anxiety and depression levels.
methods
search strategy
A computerised search of the literature through the search engines Pubmed and PsychINFO was carried out on 1 February 2010. The search strategy combined the term ‘cancer’ with other key terms related to information provision and HRQoL. For ‘information provision’, we included the terms information, information provision, information disclosure, information needs, information satisfaction, information level, information barriers, written information, oral information, audiotape information, CDROM. For the constructs of HRQoL, anxiety and depression we included the terms quality of life, health-related quality of life, health status, well-being, anxiety and depression.
The reference lists of all identified publications were checked to retrieve other relevant publications, which were not identified by means of the computerised search. There were no restrictions with regard to the years of publication. The search yielded 5732 hits.
selection criteria
Studies that met the following criteria were included: (i) if they evaluated the relation between information provision and HRQoL, anxiety and depression in adult cancer survivors, and this evaluation was one of the key objectives of the study; (ii) if the publication was an original article (no poster abstract, letter to the editor etc.); (iii) if the article was a full report published in English and (iv) if it was published in a peer-reviewed journal. Studies were excluded for the following reasons: (i) if they were individual case reports or articles that reviewed the literature, (ii) if the study was focused on end-stage cancer patients (terminal ill patients) because this patient group is dealing with specific end-of-life issues, (iii) if the study focused on communication aspects (e.g. body language), (iv) if the study focused on information provision to family members, (v) if the study focused on diagnosis or prognosis as primary information measure, or if (v) HRQoL was measured with one single item and was not a part of a validated questionnaire.
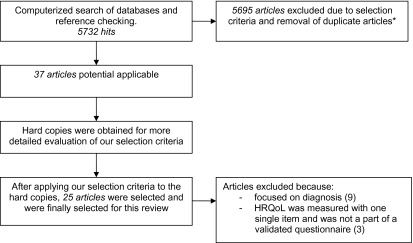
The described inclusion and exclusion criteria were applied to our initial 5732 hits. Based on their titles and abstracts, 37 articles met our criteria. The 37 hard copies were obtained and reviewed by three investigators. After careful review, 25 articles fulfilled our selection criteria and were included in this review [12–36]. The flow chart of this selection procedure is shown in Figure 1.
Figure 1.
Flow diagram of papers accepted and rejected during selection procedure. *The selection criteria are described in the methods section.
quality assessment
The methodological quality of each of the selected articles was independently assessed by all three investigators based on established criteria for systematic reviews (Table 1) [37, 38]. Each item of a selected study, that matched our criteria, was assigned 1 point. If an item did not meet our criteria or was described insufficiently or not at all, 0 points were assigned. The highest possible score was 13. Studies scoring 10 points or more were arbitrarily considered to be of ‘high quality’. Studies scoring between 6 and 10 points were rated as ‘adequate quality’. Studies scoring <6 points were considered to be of ‘low quality’.
Table 1.
List of criteria for assessing the methodological quality of studies on HRQoL, anxiety, depression and information provision among cancer survivors
| Positive if with respect to |
| HRQoL |
| A valid (health-related) quality of life, health status, anxiety or depression questionnaire is used. If items were deleted from the valid questionnaire, the new questionnaire must be validated |
| Information assessment |
| A valid ‘information provision’ questionnaire is used. If items were deleted from the valid questionnaire, the new questionnaire must be validated |
| Study population |
| A description is included of at least two sociodemographic variables (e.g. age, employment status, educational status) |
| A description is included of at least two clinical variables of the described patient population (e.g. tumour stage at diagnosis, treatment) |
| Inclusion and/or exclusion criteria are described |
| Participation and response rates for patient groups have to be described and have to be >75% |
| Information is given about the degree of selection of the patient sample (information is given about the ratio respondents versus non-respondents) |
| Study design |
| The study size is consisting of at least 50 patients (arbitrarily chosen) |
| The data is prospectively gathered |
| The process of data collection is described (interview or self-report, etc.) |
| Results |
| The results are compared between two groups or more (e.g. healthy population, groups with different treatment or age) and/or results are compared between at least two time points (e.g. pre- versus post-treatment). |
| Mean, median, standard deviations or percentages are reported for the most important outcome measures |
| Statistical proof for the findings is reported |
results
study characteristics
In total, 25 studies were included, all published between April 1996 and December 2009. Different questionnaires with different outcome measures to assess HRQoL, anxiety and depression were used. All studies used different instruments to measure one or more aspects of information provision. Prospective, cross-sectional, observational as well as intervention studies were included. The main findings are summarised in Table 2.
Table 2.
Overview of all included studies sorted on outcome
| First author [reference], country, year | Design | Study population | HRQoL, anxiety and/or depression instrument | Information provision instrument | Results | Quality score |
| HRQoL | ||||||
| Frodj [12], Sweden, 2009 | Prospective | 36 carcinoid tumour patients | EORTC QLQ-C30 | CASC | Satisfaction with doctors’ provision of information was positively related to emotional function, global QoL at T1–T3 | 9 |
| Llewellyn [27], UK, 2006 | Prospective | 82 newly diagnosed head and neck cancer patients; 47% had an early stage (1 or 2) | General Health Survey Questionnaire, Short Form (SF-12) | SCIP | Satisfaction with information before treatment was predictive of mental component summary scores 6–8 months after the end of treatment, but not of physical component scores | 13 |
| Yu [35], China, 2001 | Prospective | 211 nasopharyngeal carcinoma patients; 41% had an early stage (I or II), 59% had a higher stage | FACT-G | Medical Interview Satisfaction Scale | More satisfaction with the medical information provided an average of 1 month after the end of radiotherapy had a better QoL 4 months later | 10 |
| Kerr [26], Germany, 2003 | Prospective | 980 breast cancer patients, 93.3% had an early stage (is, I, or II) | EORTC QLQ-C30; EORTC BR-23 (breast cancer specific) | Self-developed: satisfaction with hospital stay, doctor communication and aftercare | 17 QoL variables were significantly worse, up to 4 years after diagnosis, for those patients reporting unclear information | 11 |
| Vogel [36] Germany, 2009 | Prospective | 135 breast cancer patients | EORTC QLQ-C30 | Patient satisfaction with communication 25-item Likert scale; Self-developed question about level of information | Patients who rated their level of information at baseline as high experienced a higher QoL after 3 and 6 months | 10 |
| Griggs [21], USA, 2007 | Cross-sectional | 235 breast cancer patients | SF-36; IES | Self-developed: satisfaction with information | Strong positive relationship between satisfaction with information and vitality, mental health, and a strong negative relationship with distress | 9 |
| Mallinger [28], USA, 2005 | Cross-sectional | 182 breast cancer survivors | SF-36 | Information needs scale for recently diagnosed breast cancer patients | Better mental health is associated with greater satisfaction with information about treatment and survivorship | 10 |
| Davies [18], UK, 2008 | Cross-sectional | 102 breast cancer; 112 prostate cancer patients | FACT-G | Adapted version of the Information Satisfaction Questionnaire | Information satisfaction is a predictor of global QoL and its four dimensions. Satisfaction is positively associated with QoL | 9 |
| Annunziata [13], Italy, 1998 | Cross-sectional | 175 patients (breast, gastrointestinal, leukaemia, genitourinary tumours, lung, other neoplasms) | Functional Living Index for Cancer; State-Trait Anxiety Inventory | Degree of information on diagnosis and status of disease | Level of information did not affect QoL, satisfaction with information was associated with better QoL | 8 |
| Bredart [17], France, 2001 | Cross-sectional | 97 cancer patients with different diagnoses and stages | EORTC QLQ-C30 | CASC | Lower physical functioning and emotional functioning predicted higher satisfaction with doctor’s information provision | 11 |
| Elf [19], Sweden, 2001 | Cross-sectional | 30 cancer patients undergoing chemotherapy | EORTC QLQ-C30 | Self-developed: questions on patients’ satisfaction with information; Miller Behavioral Styles Scale | No significant differences in QoL could be found between satisfied and dissatisfied patients | 9 |
| Beckjord [16], USA, 2008 | Cross-sectional | 1040 cancer survivors (bladder, leukaemia, colorectal, non-Hodgkin’s lymphoma) | SF-36 | Self-developed: information needs | More information needs were associated with worse perceived mental and physical health | 8 |
| McInnes [29], USA, 2008 | Cross-sectional | 778 cancer survivors of six common cancers (bladder, breast, colorectal, prostate, uterine, melanoma); 3.1% in situ, 72.6% localised, 22.8% regional, 1.5% distant | SF-36 | Self-developed scales: information quality, information barriers, information needs | Worse physical and mental functioning was associated with greater need for information, worse ratings of information quality, and more barriers in obtaining information | 9 |
| Arora [14], USA, 2002 | Cross-sectional | 225 breast cancer patients; 80.4% had an early stage (is, I, or II) | Functional Assessment of Cancer Therapy (FACT) | Barriers to information access scale | Experience of greater barriers to accessing needed health information was significantly associated with lower emotional, functional and social/family well-being | 7 |
| Snyder [34], USA, 2007 | Cross-sectional | 117 cancer patients (breast, lung, prostate), 35.3% had an early stage, 14.7 locoregional, 50% metastatic | EORTC QLQ-C30 | Supportive Care Needs Survey | Better emotional function (not physical function) was associated with fewer unmet information needs | 7 |
| Anxiety and/or depression | ||||||
| Llewellyn [27], UK, 2006 | Prospective | 82 newly diagnosed head and neck cancer patients, 47% had an early stage (1 or 2) | HADS | SCIP | Satisfaction with information before treatment was predictive of depression 6–8 months after the end of treatment, but not of anxiety | 13 |
| Frodj [12],Sweden, 2009 | Prospective | 36 carcinoid tumour patients | HADS | CASC | Satisfaction with doctors’ provision of information was negatively related to anxiety and depression at T1–T3 | 9 |
| Vogel [36] Germany, 2009 | Prospective | 135 breast cancer patients | HADS | Patient satisfaction with communication 25 item Likert scale; self-developed question about level of information | Patients who rated their level of information at baseline as high were less depressed after 3 and 6 months | 10 |
| Sainio [33], Finland, 2003 | Cross-sectional | 273 cancer patients (81 breast, 73 haematological, 119 other); in 35%, cancer had recurred or metastases had appeared | Depression Scale | Self-developed questionnaire containing questions about obtained information and method of providing information | Both the respondents’ physical condition (positive) and depression (negative) were associated with receiving information | 9 |
| Jones [25], UK, 1999 | Cross-sectional | 525 cancer patients (309 breast, 129 prostate, 22 cervical, 65 laryngeal) | HADS | One question about satisfaction with information given | Depression was a predictor of dissatisfaction with information | 9 |
| Intervention studies | ||||||
| Haggmark [23], Sweden, 2001 | Prospective | 231 cancer patients (breast, bladder, prostate) | HADS; IES; Cancer Inventory of Problem Situations (CIPS II) | Self-developed: satisfaction with information questionnaire | No relation satisfaction and anxiety and depression | 10 |
| Molenaar [30], the Netherlands, 2001 | Prospective | 180 breast cancer patients | MOS20; EORTC QLQ-BR23 (breast cancer specific) | Self-developed: two instruments to measure satisfaction with information (general and treatment specific) | CDROM patients were more satisfied with breast cancer-specific information. At 3 and 9 months, a positive effect was found on general health. At 9 months, CDROM patients reported better physical functioning, less pain and fewer arm symptoms | 11 |
| Ong [31], the Netherlands, 2000 | Prospective | 201 cancer patients (gynaecologic or internal) | MOS20; Rotterdam Symptom Checklist | Patient Satisfaction Questionnaire | Patients provided with audio tape initial consultation were more satisfied than patients without the tape. The intervention did not have an effect on QoL | 10 |
| Hack [21], Canada, 2003 | Prospective | 628 breast cancer patients | Functional Assessment of Cancer Therapy (FACT-B); POMS | Patient Perception Scale | Audio tape of primary adjuvant treatment consultations to women with breast cancer was not significantly related to patient satisfaction with communication, mood state, or QoL at 12 weeks post-consultation and was not significantly affected by choice of receiving the audio tape | 10 |
| Hack [22], Canada, 2007 | Prospective | 425 prostate cancer patients; 76.2% had an early stage (I, or II), 14.6% had a high stage (III or IV) | Functional Assessment of Cancer Therapy (FACT-P); POMS | Patient Perception Scale | Audio tape of primary adjuvant treatment consultations to women with breast cancer was not significantly related to patient satisfaction with communication, mood state, or QoL at 12 weeks post-consultation and was not significantly affected by choice of receiving the audio tape | 11 |
| Iconomou [24], Greece, 2005 | Prospective | 145 cancer patients (lung, breast, colorectal, genitourinary, other); 50% had limited disease and 50% had advanced disease | EORTC-QLQ-C30; HADS | Single question about satisfaction with information provision | Patients provided with the information booklet reported significantly higher rates of satisfaction with information than control group, felt better and more informed, and perceived information received as being clearer and detailed. No significant benefits in anxiety, depression, QoL | 11 |
| Barlesi [15], France, 2008 | Prospective | 75 non-small-cell lung cancer patients | Psychologic Global Well-Being Index | Questionnaire of satisfaction of hospitalised patients; self-developed: question information satisfaction | No differences in QoL between non-small-cell lung cancer patients receiving oral information only as compared with oral plus written information | 10 |
| Passalacqua [32], Italy, 2009 | Prospective | 3197 cancer patients | HADS | One single question about satisfaction with received information | The per protocol analysis did show a reduction in psychological distress and dissatisfaction, for the patients in the PIS group compared to the control group, but differences were not significant | 9 |
CASC, Comprehensive Assessment of Satisfaction with Care; EORTC, European Organization for Research and Treatment of Cancer; FACT, Functional Assessment of Cancer Therapy; HADS, Hospital Anxiety and Depression Scale; HRQoL, health-related quality of life; SCIP, Satisfaction with information profile; IES, Impact of Event Scale; SF-36, Medical Outcomes Study Short Form 36; MOS20, Medical Outcomes Study 20; PIS, Point of Information and Support; POMS, Profile of Mood States.
methodological quality
The evaluation of the methodological quality of the studies by the three reviewers yielded disagreement on some items mostly due to differences in interpretation. These were solved through discussion in a consensus meeting. The quality scores ranged from 7 to 13 points (Table 2) and the mean quality score was 9.6. Not one of the studies had a low quality. Thirteen studies had a high quality [15, 17, 21, 22, 24, 26–28, 30, 31, 35, 36]. The remaining 12 studies had an adequate quality [12–14, 16, 18–20, 25, 29, 32–34]. General shortcomings of the included articles were the absence of a validated ‘information’ questionnaire, absence of information about the degree of selection of the patient sample, a cross-sectional design, and the lack of comparison between two groups or time points.
health-related quality of life
Fifteen studies, 5 prospective and 10 cross-sectional, examined the relation between information provision and HRQoL [12–14, 16–20, 26–29, 34–36]. Three prospective studies found a positive association between information satisfaction and HRQoL [12, 27, 35]. A Swedish study of 36 patients with a carcinoid tumour showed a positive relation between satisfaction with doctors’ provision of information and emotional function and global QoL at three of the four time points [12]. In a study among 82 head and neck cancer patients, satisfaction with information before treatment was predictive of better Mental Component Summary scores 6–8 months after the end of treatment but not to the Physical Component Summary scores [27]. The third study among 211 Chinese nasopharyngeal carcinoma patients found that more satisfaction with the medical information provided 1 month after the end of radiotherapy was related to a better QoL 4 months later [35].
Two other prospective studies focused on the clarity and quality of the information provided, and the need for information. Breast cancer patients reporting unclear information provision scored significantly worse, up to 4 years after diagnosis, on 17 of the 27 QoL variables, including emotional functioning, social functioning and global QoL [26]. Breast cancer patients who rated their level of information at baseline as high, experienced higher QoL after 3 (P < 0.001) and 6 months (P = 0.049) [36]. Overall, prospective studies showed that satisfied patients, patients who reported to receive clear and high levels of information, reported better mental HRQoL and global HRQoL. Positive associations between information provision and physical HRQoL have not been found.
Five of six cross-sectional studies found a positive relation between information satisfaction and HRQoL [13, 17–20, 28]. Two studies among breast cancer survivors found a strong positive association between satisfaction with treatment and survivorship information and mental health and vitality [20, 28]. A British study among 102 breast cancer and 112 prostate cancer patients concluded that after controlling for demographic and disease characteristics, information satisfaction explained 21% of the variance in global QoL, 12% in physical well-being, 13% in social well-being, 8% in emotional well-being, and 10% in functional well-being (all P < 0.001) [18]. This study, and an Italian study among a varied sample of 175 cancer patients, also found a positive association between satisfaction with information received and QoL [13, 18]. Besides, the Italian study found no differences in QoL of adequately versus inadequately informed patients [13]. A French study of cancer patients with different diagnoses showed that higher global scores for QoL were related to higher satisfaction with all aspects of care, including the information provision [17]. Contradictorily, lower physical and emotional functioning also predicted higher satisfaction with the doctors’ information provision in this study. One cross-sectional study among 30 cancer patients undergoing chemotherapy found no differences in QoL between satisfied and dissatisfied patients [19].
Four other cross-sectional studies focused on the clarity and quality of the information provided, and the need for information [14, 16, 29, 34]. Worse physical and emotional functioning were significantly associated with worse ratings of information quality, more barriers to obtain information and a greater need for information in two large American studies among a sample of diverse cancer survivors [16, 29]. Breast cancer patients who reported greater difficulty in accessing needed information or had greater unmet information needs experienced lower emotional, functional, and social well-being and worse physical, cognitive and role functioning as well as lower perceptions of health competence (P < 0.01) [14, 34]. In the cross-sectional studies, better mental, physical and global HRQoL were associated with fulfilled informational needs, satisfaction with the received information, the receipt of good quality and clear information and less information barriers. However, one study found no difference in HRQoL [19] and one study reported conflicting results [17].
anxiety and depression
Five studies, three prospective and two cross-sectional, focused on anxiety and depression in relation to information provision [12, 25, 27, 33, 36]. A study of 82 head and neck cancer patients found satisfaction with information before treatment, to be predictive of depression but not anxiety, 6–8 months after the end of treatment [27]. However, a study of 36 carcinoid tumour patients found a negative relation between satisfaction with doctors’ provision of information and anxiety and depression at the first three of four time points (T1–T3) [12]. Breast cancer patients who rated their level of information at baseline as high were less depressed after 3 (P = 0.010) and 6 months (P < 0.001) [36]. The studies with a prospective design showed that satisfaction with the received information and less information needs were independently related to less anxiety and depression.
The receipt of information was positively associated with the cancer patients’ physical condition and negatively with mood and depression in a Finnish cross-sectional study [33]. A study among breast, prostate, cervical and laryngeal cancer patients showed that patients who were dissatisfied with the received information were much more likely to be depressed and were marginally more likely to be anxious [25]. The results of the cross-sectional studies support the results of the prospective studies.
interventions
Some studies examined the effect of different information interventions on the HRQoL or depression and anxiety levels of cancer patients [15, 21–24, 30–32]. In a Swedish study, 210 consecutive cancer patients were randomised to one of three information conditions before the start of curative radiation treatment [23]. Compared with patients receiving standard information or standard information plus an extra brochure, patients who received standard information plus group and repeated individual information were significantly more satisfied with the information. However, there were no differences with respect to anxiety, depression, subjective distress and QoL. A Dutch study investigated the effects of the Interactive Breast Cancer CDROM, compared with the standard oral information as a decision aid for 180 breast cancer patients with a choice between breast conserving therapy and mastectomy [30]. An overall positive effect of the CDROM was found on satisfaction with the general and breast cancer-specific information received. Furthermore, an overall positive effect of the CDROM condition was found on generic QoL as well as on breast cancer-specific QoL. Subsequent analyses revealed that at 3 and 9 months follow-up, patients in the CDROM condition reported better general health than control patients. Additionally, at 9 months follow-up, the CDROM condition reported better physical functioning, and less pain and arm symptoms.
Three studies tested the efficacy of an audiotaped consultation on the QoL of cancer patients showing no main effect of the intervention on QoL or mood state [21, 22, 31]. The first study showed that the provision of a taped initial consultation resulted in more satisfied patients than patients allocated to the control group [31]. The other two studies among breast and prostate cancer patients showed that the provision of an audio tape of their primary treatment consultation was not significantly related to patient satisfaction with communication and was not significantly affected by choice of receiving the audio tape [21]. Furthermore, the compliance was low with 40% of the patients who did not listen to the audio tapes, mainly because they felt emotionally not prepared to listen [21]. However, patients rated the audiotape intervention positively. Patients receiving the consultation audio tape reported having been provided with significantly more disease and treatment information in general and more information about treatment alternatives and treatment side-effects in particular, than patients who did not receive the audio tape [22].
A Greek study of 145 cancer patients who were randomised to receive a booklet about chemotherapy or not showed that patients provided with the information booklet reported significantly higher rates of satisfaction with information than the control group, felt better and more informed, and perceived the information received as being clearer and more detailed [24]. However, no significant benefits in anxiety, depression and QoL occurred. Another study randomised patients to receive oral information only or oral plus written information describing the disease and its associated surgery and outcomes [15]. There was no significant difference in QoL at baseline, during the postoperative period or at 3 months post-surgery. In addition, the QoL scores for each dimension (anxiety, depressed mood, positive well-being, self-control, general health and vitality) were not statistically different between both groups at each time of analysis.
In a cluster randomised trial, no statistically significant effects of a Point of Information and Support (PIS) on anxiety or dissatisfaction levels was observed [32]. However, 52% of centres in the experimental group did not implement the PIS in accordance with the protocol. The same study highlighted that a greater likelihood of dissatisfaction was associated with the presence of anxiety and/or depression [32].
discussion
The aim of this systematic review was to summarise and evaluate the results of all studies focussing on the relationship between information provision and HRQoL and psychological distress. All five prospective observational studies found a positive relation between appropriate information provision (satisfaction with the received information, fulfilled informational needs, high quality and clear information) and mental and global HRQoL and a negative relation between appropriate information provision and depression and anxiety. The results of all 12 cross-sectional observational studies are in accordance with the findings of the prospective studies; however, they also found a positive association between appropriate information provision and physical HRQoL. Only one of eight intervention studies found a positive effect of information on HRQoL.
The prospective observational studies found a strong positive relation between adequate information provision and mental health but not physical health. A better understanding of a patients’ situation after the information provision or the receipt of information aimed at learning to cope with cancer or reducing distress might be responsible for better mental health and lower levels of anxiety and depression [35]. Patients who had difficulties in obtaining the information they desire were found to have less confidence in their ability to deal with health-related issues [14]. Appropriate information provision lead to an improved health competence, a better sense of control over cancer and better symptom management [14, 20]. From the cross-sectional observational studies, the direction of the relationship is not clear. A lack of information, or information of low quality, can lead to anxiety, depression or a decreased mental and/or global HRQoL as suggested by the prospective studies. However, some information can elevate patients’ distress levels [39]. On the other hand, anxiety can inhibit information processing, patients with a poorer mental health may have more difficulty to understand the information even when the information is of high quality, while patients with better global health are more satisfied beforehand because of their better emotional state [20, 40].
The results of the observational studies were not confirmed by the intervention studies. This can be explained by the nature of the intervention studies. The objective of these studies was to test the efficiency of an information intervention in terms of information satisfaction, HRQoL, anxiety or depression, while the observational studies searched for a possible relation of information provision and HRQoL, anxiety or depression. Although patients in the experimental conditions overall rated the additional information positive, felt that they received more information and were satisfied with the overall received information, only one intervention study observed positive relations with HRQoL, anxiety or depression.
Most patients tend to adjust well to their disease and it is therefore possible that additional gains in HRQoL are not easily achieved [30]. A further explanation for these results might be the limited surplus value of the additional information given in the experimental conditions. Written information can be useful but is often non-specific and not tailored to patients’ information needs; this can lead to confusion or even elevation of anxiety and depression levels [31, 41]. Audio tapes seem to facilitate patients’ requests to clarify earlier provided information and might enhance the recall of information. Interventions that aim to empower patients might be more useful and effective to decrease anxiety and depression and enhance HRQoL [23]. Mostly, information is given in a neutral mode, with no direct attempt to promote active participation of the patient in the conversation and no attempts to influence patients’ inferences. The information provided has an impact on the cognitive level, with no emphasis on the effect or the emotions related to the receipt of medical information. The intervention study with a CDROM as decision aid operates both at the cognitive and affective level. Patients who exit their consultation with the belief that they played an active role had better HRQoL scores [21]. An intervention might therefore be more powerful with elements of counselling or psychotherapy [24].
Another explanation for the lack of intervention effects on HRQoL, anxiety and depression levels may be the short duration of some of the interventions. The information booklet about chemotherapy was presented for only 30 min [24]. A recent meta-analysis showed that psychosocial interventions should last 12 weeks or more to improve HRQoL [42]. When the information is offered for a short time, it seems reasonable that patients forget a substantive amount of that provided information. Furthermore, in six of eight intervention studies, cancer patients were randomised on individual level, which might result in contamination bias when the health care practitioner gives more than the usual standard information to the control group patients. When this happens, the effects of the experimental conditions might be underestimated. The CDROM study used a quasi-experimental pre-test/post-test design and the PIS study used cluster randomisation to overcome the problem of contamination bias and maximise internal validity [30, 32, 43].
In addition, in some of the intervention studies, the compliance was low; participants did not use the additional information. For example, just below 40% of the patients in the experimental group did not listen to the audio tapes [21], and the Italian PIS study showed that eventually only 48% of the centres indeed started a PIS [32]. Results favouring these interventions are therefore difficult to find. When the centres that did not comply with the PIS protocol were removed from the analyses, the intervention did improve patient-centred outcomes [32]. The intervention studies showed that it is not the quantity but the quality of information that is important for adequate information provision. The addition of general information, with limited surplus value, to the standard information provided did not have an influence on HRQoL or anxiety and depression levels. Instead of adding general information to the standard information provided, the interventions must be directed to give each patient the specific high-quality information they need.
Another important issue is the role of cross-cultural differences in information provision. Truth telling and honest disclosure of cancer information appears to remain controversial in southern and eastern (European) countries [44]. Awareness of a cancer diagnosis or prognosis is associated with more anxiety and depression, poorer physical, social and emotional QoL in those countries [45–47]. However, among the included papers, the association between information provision and HRQoL, anxiety and depression was not different between different countries.
There are several methodological issues that impede drawing strong conclusions on the relation between information provision and HRQoL. The included studies in this review all used different measures and questionnaires of information provision. There was only one validated information provision questionnaire, the satisfaction with information profile [27]. All other studies used subscales of (validated) questionnaires, self-developed and not yet validated questionnaires or single questions. This makes it difficult to compare the results of the different studies. Only recently, the European Organization for Research and Treatment of Cancer developed a questionnaire that evaluates the information received by cancer patients [48]. It might be helpful to use this validated questionnaire in future studies because it is available in many languages, which makes international comparison possible. Also, many different questionnaires are used to assess HRQoL. All these questionnaires claim to assess HRQoL or the individual’s perception about their position in life; however, many questionnaires measure different constructs and therefore comparison between the studies is difficult. Taken into account these methodological limitations, the overall picture suggests a positive association between information provision and HRQoL.
We can conclude that doctors should provide patients with the information patients desire in order to optimise patient satisfaction. Satisfied patients, patients with fulfilled information needs, and patients who experience less information barriers, in general have a better HRQoL and lower levels of depression and anxiety. The consistency of these associations indicates that further attention must be paid to more patient-centred information provision taking into account the differences in information needs by gender, age, cultural background, educational level, stage of disease and coping style. Additional research is needed to make definitive conclusions about information interventions as most results did not reach statistical significance due to methodological constraints. The recent emergence of cancer survivorship research and the increasing recognition of its importance will hopefully lead to more research focussing on good information provision interventions that are able to improve HRQoL and decrease psychological distress.
funding
Cancer Research Award from the Dutch Cancer Society (UVT-2009-4349 to L.V.v.d.P.-F.). Funding to pay the Open Access publication charges for this article was provided by the University of Tilburg, Oldendorff Research Institute (ORI).
disclosure
The manuscript has been prepared in accordance with the style of the journal, and all authors have approved of its contents. This manuscript is not being considered for publication elsewhere and the findings of this manuscript have not been previously published. The authors declare no conflict of interest.
References
- 1.van der Meulen N, Jansen J, van Dulmen S, et al. Interventions to improve recall of medical information in cancer patients: a systematic review of the literature. Psychooncology. 2008;17:857–868. doi: 10.1002/pon.1290. [DOI] [PubMed] [Google Scholar]
- 2.Harrison D. What are the unmet supportive care needs of people with cancer? A systematic review. Support Care Cancer. 2009;17(8):1117–1128. doi: 10.1007/s00520-009-0615-5. [DOI] [PubMed] [Google Scholar]
- 3.Jenkins V, Fallowfield L, Saul J. Information needs of patients with cancer: results from a large study in UK cancer centres. Br J Cancer. 2001;84:48–51. doi: 10.1054/bjoc.2000.1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miller SM. Monitoring versus blunting styles of coping with cancer influence the information patients want and need about their disease. Implications for cancer screening and management. Cancer. 1995;76:167–177. doi: 10.1002/1097-0142(19950715)76:2<167::aid-cncr2820760203>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 5.Mills ME, Sullivan K. The importance of information giving for patients newly diagnosed with cancer: a review of the literature. J Clin Nurs. 1999;8:631–642. doi: 10.1046/j.1365-2702.1999.00296.x. [DOI] [PubMed] [Google Scholar]
- 6.Montazeri A, Milroy R, Hole D, et al. Quality of life in lung cancer patients: as an important prognostic factor. Lung Cancer. 2001;31:233–240. doi: 10.1016/s0169-5002(00)00179-3. [DOI] [PubMed] [Google Scholar]
- 7.Montazeri A, Milroy R, Hole D, et al. How quality of life data contribute to our understanding of cancer patients' experiences? A study of patients with lung cancer. Qual Life Res. 2003;12:157–166. doi: 10.1023/a:1022232624891. [DOI] [PubMed] [Google Scholar]
- 8.Quinten C, Coens C, Mauer M, et al. Baseline quality of life as a prognostic indicator of survival: a meta-analysis of individual patient data from EORTC clinical trials. Lancet Oncol. 2009;10:865–871. doi: 10.1016/S1470-2045(09)70200-1. [DOI] [PubMed] [Google Scholar]
- 9.Holzner B, Kemmler G, Kopp M, et al. Quality of life in breast cancer patients–not enough attention for long-term survivors? Psychosomatics. 2001;42:117–123. doi: 10.1176/appi.psy.42.2.117. [DOI] [PubMed] [Google Scholar]
- 10.Brown LF, Kroenke K, Theobald DE, et al. The association of depression and anxiety with health-related quality of life in cancer patients with depression and/or pain. Psychooncology. 2010;19:734–741. doi: 10.1002/pon.1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holland JC. Preliminary guidelines for the treatment of distress. Oncology (Williston Park) 1997;11:109–114. discussion 115–107. [PubMed] [Google Scholar]
- 12.Frojd C, Lampic C, Larsson G, von Essen L. Is satisfaction with doctors' care related to health-related quality of life, anxiety and depression among patients with carcinoid tumours? A longitudinal report. Scand J Caring Sci. 2009;23:107–116. doi: 10.1111/j.1471-6712.2008.00596.x. [DOI] [PubMed] [Google Scholar]
- 13.Annunziata MA, Foladore S, Magri MD, et al. Does the information level of cancer patients correlate with quality of life? A prospective study. Tumori. 1998;84:619–623. doi: 10.1177/030089169808400601. [DOI] [PubMed] [Google Scholar]
- 14.Arora NK, Johnson P, Gustafson DH, et al. Barriers to information access, perceived health competence, and psychosocial health outcomes: test of a mediation model in a breast cancer sample. Patient Educ Couns. 2002;47:37–46. doi: 10.1016/s0738-3991(01)00170-7. [DOI] [PubMed] [Google Scholar]
- 15.Barlesi F, Barrau K, Loundou A, et al. Impact of information on quality of life and satisfaction of non-small cell lung cancer patients: a randomized study of standardized versus individualized information before thoracic surgery. J Thorac Oncol. 2008;3:1146–1152. doi: 10.1097/JTO.0b013e3181874637. [DOI] [PubMed] [Google Scholar]
- 16.Beckjord EB, Arora NK, McLaughlin W, et al. Health-related information needs in a large and diverse sample of adult cancer survivors: implications for cancer care. J Cancer Surviv. 2008;2:179–189. doi: 10.1007/s11764-008-0055-0. [DOI] [PubMed] [Google Scholar]
- 17.Bredart A, Razavi D, Robertson C, et al. Assessment of quality of care in an oncology institute using information on patients' satisfaction. Oncology. 2001;61:120–128. doi: 10.1159/000055362. [DOI] [PubMed] [Google Scholar]
- 18.Davies NJ, Kinman G, Thomas RJ, Bailey T. Information satisfaction in breast and prostate cancer patients: implications for quality of life. Psychooncology. 2008;17:1048–1052. doi: 10.1002/pon.1305. [DOI] [PubMed] [Google Scholar]
- 19.Elf M, Wikblad K. Satisfaction with information and quality of life in patients undergoing chemotherapy for cancer. The role of individual differences in information preference. Cancer Nurs. 2001;24:351–356. doi: 10.1097/00002820-200110000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Griggs JJ, Sorbero ME, Mallinger JB, et al. Vitality, mental health, and satisfaction with information after breast cancer. Patient Educ Couns. 2007;66:58–66. doi: 10.1016/j.pec.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 21.Hack TF, Pickles T, Bultz BD, et al. Impact of providing audiotapes of primary adjuvant treatment consultations to women with breast cancer: a multisite, randomized, controlled trial. J Clin Oncol. 2003;21:4138–4144. doi: 10.1200/JCO.2003.12.155. [DOI] [PubMed] [Google Scholar]
- 22.Hack TF, Pickles T, Bultz BD, et al. Impact of providing audiotapes of primary treatment consultations to men with prostate cancer: a multi-site, randomized, controlled trial. Psychooncology. 2007;16:543–552. doi: 10.1002/pon.1094. [DOI] [PubMed] [Google Scholar]
- 23.Haggmark C, Bohman L, Ilmoni-Brandt K, et al. Effects of information supply on satisfaction with information and quality of life in cancer patients receiving curative radiation therapy. Patient Educ Couns. 2001;45:173–179. doi: 10.1016/s0738-3991(01)00116-1. [DOI] [PubMed] [Google Scholar]
- 24.Iconomou G, Viha A, Koutras A, et al. Impact of providing booklets about chemotherapy to newly presenting patients with cancer: a randomized controlled trial. Ann Oncol. 2006;17:515–520. doi: 10.1093/annonc/mdj098. [DOI] [PubMed] [Google Scholar]
- 25.Jones R, Pearson J, McGregor S, et al. Cross sectional survey of patients' satisfaction with information about cancer. BMJ. 1999;319:1247–1248. doi: 10.1136/bmj.319.7219.1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kerr J, Engel J, Schlesinger-Raab A, et al. Communication, quality of life and age: results of a 5-year prospective study in breast cancer patients. Ann Oncol. 2003;14:421–427. doi: 10.1093/annonc/mdg098. [DOI] [PubMed] [Google Scholar]
- 27.Llewellyn CD, McGurk M, Weinman J. How satisfied are head and neck cancer (HNC) patients with the information they receive pre-treatment? Results from the satisfaction with cancer information profile (SCIP) Oral Oncol. 2006;42:726–734. doi: 10.1016/j.oraloncology.2005.11.013. [DOI] [PubMed] [Google Scholar]
- 28.Mallinger JB, Griggs JJ, Shields CG. Patient-centered care and breast cancer survivors' satisfaction with information. Patient Educ Couns. 2005;57:342–349. doi: 10.1016/j.pec.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 29.McInnes DK, Cleary PD, Stein KD, et al. Perceptions of cancer-related information among cancer survivors: a report from the American Cancer Society’s Studies of Cancer Survivors. Cancer. 2008;113:1471–1479. doi: 10.1002/cncr.23713. [DOI] [PubMed] [Google Scholar]
- 30.Molenaar S, Sprangers MA, Rutgers EJ, et al. Decision support for patients with early-stage breast cancer: effects of an interactive breast cancer CDROM on treatment decision, satisfaction, and quality of life. J Clin Oncol. 2001;19:1676–1687. doi: 10.1200/JCO.2001.19.6.1676. [DOI] [PubMed] [Google Scholar]
- 31.Ong LM, Visser MR, Lammes FB, et al. Effect of providing cancer patients with the audiotaped initial consultation on satisfaction, recall, and quality of life: a randomized, double-blind study. J Clin Oncol. 2000;18:3052–3060. doi: 10.1200/JCO.2000.18.16.3052. [DOI] [PubMed] [Google Scholar]
- 32.Passalacqua R, Caminiti C, Campione F, et al. Prospective, multicenter, randomized trial of a new organizational modality for providing information and support to cancer patients. J Clin Oncol. 2009;27:1794–1799. doi: 10.1200/JCO.2007.15.0615. [DOI] [PubMed] [Google Scholar]
- 33.Sainio C, Eriksson E. Keeping cancer patients informed: a challenge for nursing. Eur J Oncol Nurs. 2003;7:39–49. doi: 10.1054/ejon.2002.0218. [DOI] [PubMed] [Google Scholar]
- 34.Snyder CF, Garrett-Mayer E, Brahmer JR, et al. Symptoms, supportive care needs, and function in cancer patients: how are they related? Qual Life Res. 2008;17:665–677. doi: 10.1007/s11136-008-9331-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yu CL, Fielding R, Chan CL, Sham JS. Chinese nasopharyngeal carcinoma patients treated with radiotherapy: association between satisfaction with information provided and quality of life. Cancer. 2001;92:2126–2135. doi: 10.1002/cncr.1554. [DOI] [PubMed] [Google Scholar]
- 36.Vogel BA, Leonhart R, Helmes AW. Communication matters: the impact of communication and participation in decision making on breast cancer patients' depression and quality of life. Patient Educ Couns. 2009;77:391–397. doi: 10.1016/j.pec.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 37.Mols F, Vingerhoets AJ, Coebergh JW, van de Poll-Franse LV. Quality of life among long-term breast cancer survivors: a systematic review. Eur J Cancer. 2005;41:2613–2619. doi: 10.1016/j.ejca.2005.05.017. [DOI] [PubMed] [Google Scholar]
- 38.Den Oudsten BL, Van Heck GL, De Vries J. Quality of life and related concepts in Parkinson's disease: a systematic review. Mov Disord. 2007;22:1528–1537. doi: 10.1002/mds.21567. [DOI] [PubMed] [Google Scholar]
- 39.Leydon GM, Boulton M, Moynihan C, et al. Cancer patients' information needs and information seeking behaviour: in depth interview study. BMJ. 2000;320:909–913. doi: 10.1136/bmj.320.7239.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.van der Molen B. Relating information needs to the cancer experience. 2. Themes from six cancer narratives. Eur J Cancer Care (Engl) 2000;9:48–54. doi: 10.1046/j.1365-2354.2000.00190.x. [DOI] [PubMed] [Google Scholar]
- 41.McHugh P, Lewis S, Ford S, et al. The efficacy of audiotapes in promoting psychological well-being in cancer patients: a randomised, controlled trial. Br J Cancer. 1995;71:388–392. doi: 10.1038/bjc.1995.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rehse B, Pukrop R. Effects of psychosocial interventions on quality of life in adult cancer patients: meta analysis of 37 published controlled outcome studies. Patient Educ Couns. 2003;50:179–186. doi: 10.1016/s0738-3991(02)00149-0. [DOI] [PubMed] [Google Scholar]
- 43.Godwin M, Ruhland L, Casson I, et al. Pragmatic controlled clinical trials in primary care: the struggle between external and internal validity. BMC Med Res Methodol. 2003;3:28. doi: 10.1186/1471-2288-3-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Iconomou G, Viha A, Koutras A, et al. Information needs and awareness of diagnosis in patients with cancer receiving chemotherapy: a report from Greece. Palliat Med. 2002;16:315–321. doi: 10.1191/0269216302pm574oa. [DOI] [PubMed] [Google Scholar]
- 45.Lheureux M, Raherison C, Vernejoux JM, et al. Quality of life in lung cancer: does disclosure of the diagnosis have an impact? Lung Cancer. 2004;43:175–182. doi: 10.1016/j.lungcan.2003.08.018. [DOI] [PubMed] [Google Scholar]
- 46.Montazeri A, Tavoli A, Mohagheghi MA, et al. Disclosure of cancer diagnosis and quality of life in cancer patients: should it be the same everywhere? BMC Cancer. 2009;9:39. doi: 10.1186/1471-2407-9-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tavoli A, Mohagheghi MA, Montazeri A, et al. Anxiety and depression in patients with gastrointestinal cancer: does knowledge of cancer diagnosis matter? BMC Gastroenterol. 2007;7:28. doi: 10.1186/1471-230X-7-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Arraras JI, Kuljanic-Vlasic K, Bjordal K, et al. EORTC QLQ-INFO26: a questionnaire to assess information given to cancer patients a preliminary analysis in eight countries. Psychooncology. 2007;16:249–254. doi: 10.1002/pon.1047. [DOI] [PubMed] [Google Scholar]