Abstract
Objective
To examine the long-term effects of multiple health-behavior changes from the Mediterranean Lifestyle Program.
Methods
The randomized trial targeted postmenopausal women with type 2 diabetes (N = 279) at high risk for heart disease. The intervention featured a weekend retreat followed by regular meetings over 24 months to enhance healthful eating, physical activity (PA), stress management, and support behaviors.
Results
Long-term analyses indicated that significant improvements made in the targeted behaviors during the active treatment phase of the study (at 6, 12, and 24 months) were partially maintained during the non-treatment phase of the study, through 5 years post-intervention contact for dietary behavior and stress management, and 1 year post-treatment for PA.
Conclusions
This moderate-intensity group-based intervention produced health behavior changes that tended to plateau or return to baseline levels 1 to 5 years after treatment. Future research should explore innovative methods for sustaining change over the long term.
Keywords: multiple health behaviors, diabetes, long-term, women, randomized controlled trial
Improvements in lifestyle behaviors such as healthful eating and regular exercise are difficult to attain during behavioral interventions, and are even more difficult to maintain after formal intervention activities have ended.1-3 Yet, for individuals with type 2 diabetes, attaining and sustaining a healthful lifestyle over long periods of time are critical for improving risk factors4 and avoiding adverse consequences of illness progression, such as heart disease, blindness, and kidney damage.5 It is especially important for older adults who have heart disease or CHD risk factors to engage in long-term physical activity (PA) and dietary changes.6,7
Advancements have been made in developing interventions that achieve beneficial short-term changes; however, information is lacking on the long-term impact of diabetes self-management interventions, particularly beyond 1 to 2 years.8 Existing evidence suggests that lifestyle improvements achieved during interventions are seldom sustained post-treatment.5,8 Although people with diabetes and other chronic diseases engage in multiple health-risk behaviors,9,10 many interventions address only a single behavior and only a few address more than diet combined with PA. In particular, there is a lack of comprehensive lifestyle interventions for diabetes that also include other important health-risk factors, such as stress, smoking, and the social environment.
Long-term trials of multiple-risk-factor change are rare. Research questions concerning initial and sustained behavior change become more complex when interventions comprise several components designed to change multiple lifestyle characteristics.11 Daubenmier, Weidner, and Sumner et al12 addressed the issue of cross-behavioral effects in multi-component interventions. Efforts to change 2 or more behaviors concurrently could have synergistic effects, such as reduction in alcohol consumption along with smoking cessation, or could have competing effects, such as weight gain associated with smoking cessation. Successful behavior change in one domain might facilitate later change in another domain through a central mechanism, such as enhanced self-efficacy.11 Because lifestyle behavioral interventions and their associated outcomes might be influenced by factors in an individual’s environment, it is possible that those outcomes might differ in their trajectories of change after the end of active treatment. Answering questions about how different health behaviors might change across time requires a research design that provides long-term follow-up of several intervention outcomes.
The Mediterranean Lifestyle Program (MLP) was designed to study the effects of a multi-component lifestyle intervention on multiple outcomes of relevance for postmenopausal women with type 2 diabetes.13 The MLP promoted the “Mediterranean” diet (low in saturated fat), regular PA, stress-management practice, smoking cessation, and social support. Women who were randomly assigned to the MLP condition participated in weekly group meetings for 6 months and a faded schedule of meetings over an additional 18 months. Compared to a usual care (UC) control condition, the MLP intervention at 6-, 12-, and 24-month assessments revealed consistent and statistically significant greater improvement in terms of reduced fat and caloric intake, increased PA, more frequent stress-management practice, and greater perceived social support.14,15 The MLP intervention improved cardiovascular risk factors at 12 months, and was projected to reduce cardiovascular morbidity over the lifetime of the study participants (a gain of .02 quality-adjusted life-years per participant, achieved at a cost of $20,705/QALY).16 The current study was designed to assess the longer-term effects of the baseline- to 24-month comprehensive lifestyle improvements achieved in the original MLP. Studies exploring the long-term effects of multiple-health-behavior interventions, and the impact of these behavioral changes on diabetes and coronary heart disease outcomes, are exceedingly rare.
The primary research questions of this study were: (a) What are the patterns of change in health behaviors and psychosocial factors during the active (baseline to 24-months) treatment phase as well as during the post-intervention phase 3-7 years later? (b) Do patterns of long-term change differ across behavioral outcomes? and (c) What are the patterns of change in hypothesized mediating variables over time? Our main hypothesis was that, without continuing intervention, multiple-health-behavior changes gradually return to baseline levels.
METHODS
Participants
Participants were 279 postmenopausal women with type 2 diabetes in the Pacific Northwest, who received their medical care from participating primary care clinics. Eligible participants were postmenopausal, diagnosed with type 2 diabetes for at least 6 months, living independently, able to read English, not developmentally disabled, and residing within 30 miles of the intervention site. Eligible patients were sent a letter from their primary care physicians, followed by a telephone call inviting them to participate. Seventy percent of physician practices approached, agreed to participate. Fifty-one percent of the women who were contacted and found eligible agreed to participate.
All participants signed informed consent statements prior to participation. Research procedures were reviewed and approved by an institutional review board. Participants agreed to participate before they knew their assignment to condition, and received no external incentives.
Design
Details of the study design have been published elsewhere.17 A total of 116 participants were originally randomized to UC and 163 to the MLP. More participants were assigned to the MLP condition to accommodate the mid-study reassignment of MLP participants into 2 groups to compare long-term behavior change strategies. Assignment to experimental conditions was stratified on (a) physician practice, (b) smoking status, and (c) type of diabetes medication.
After 6 months of intervention, MLP participants were further randomized to either a faded schedule of group meetings led by lay leaders (“weekly meeting” condition) or to a personalized support-enhancement condition (“PSC”) which met 4 times over 18 months. MLP staff delivered the PSC intervention by using a specially designed interactive computer program that focused on enhancement of social resources to support a healthful lifestyle. Preliminary analyses revealed no meaningful differences between these 2 conditions; therefore, they were combined and compared to the UC condition in further analyses.
Once the active intervention and 24-month data collection were completed, study participants were assessed annually for 5 additional years; MLP women received no further treatment.
UC (Control) Condition
Control condition participants completed the same assessments as intervention participants, and received no treatment beyond usual diabetes care from their physicians.
MLP Intervention
Details of the MLP intervention have been previously reported.14,17 The intervention began with a 3-day retreat, during which women were taught all program components. Retreats were followed by 6 months of weekly meetings consisting of 1 hour each of PA, stress management, a Mediterranean diet potluck, and support groups. Participants received manuals that detailed each aspect of MLP.
Dietary practices
A registered dietitian taught participants the Mediterranean alpha-linolenic acid-rich diet.18 The diet recommended more bread; more root vegetables, green vegetables, and legumes; more fish; less red meat, replaced by poultry; fruit daily; and avoidance of butter and cream, replaced by olive/canola oil products.
PA
Participants were advised to build up to 1 hour of moderate aerobic activity per day, at least 3 days per week as recommended by Ornish et al19 However, women who engaged in no, or very little, activity were advised to set an initial target of 30 minutes of activity per day. An exercise physiologist led exercise sessions at the weekly meetings.
Stress management
Participants were instructed in yoga, progressive deep relaxation, meditation, and directed or receptive imagery.19 They were asked to practice the techniques for at least 1 hour per day, and received videotapes for home use.
Support groups
A professional with at least master’s-level training and one peer leader (eg, woman of similar age who had personal or family experience with diabetes) led each support group. Professional and peer leaders received extensive training in the supportive-expressive group therapy model used with the chronically and terminally ill. All leaders were supervised weekly.
Measures
Behavioral Outcomes
Dietary
The semi-quantitative food frequency questionnaire (FFQ) developed at the Fred Hutchinson Cancer Research Center20 was used to document percent of calories from saturated fat. This FFQ has been validated with 4-day food records and 24-hour dietary recalls (average r = .5). The concurrent validity of the percent of dietary saturated fat measured by the FFQ was assessed by saturated fatty acids from a plasma fatty acid profile. Using the control group only, the 24-month correlation between intake of saturated fat measured by the FFQ and plasma concentrations of saturated fatty acids was r = .26, P < .01. On a special 7-day self-monitoring log, participants were asked to record for 7 days their daily adherence to 4 components of the Mediterranean diet: whether they (a) had any fruit; (b) ate at least 2 vegetable servings; (c) limited fat to canola oil, olive oil, or olive- or canola-based margarine; and (d) avoided red meat. The number of days respondents adhered to each component was summed, and a mean computed as the self-monitoring diet adherence score (internal consistency alpha = .48). The Kristal Fat and Fiber Behavior Questionnaire21 was used to assess fat-intake behaviors.
PA
The CHAMPS Activities Questionnaire for Older Adults22 provided an estimate of kilocalories/kilogram/hour of exercise-related activities, which incorporates the 3 key components of PA: frequency, duration, and intensity. The sensitivity of the CHAMPS has been demonstrated in physically underactive seniors.22 A 7-day self-monitoring record of minutes engaged in PA also was collected. To validate the self-report PA variables, participants were monitored using more-objective PA measures for 7 days at each assessment point: From baseline through 24 months, the Yamax DW-500 pedometer (Yamax Corporation, Japan) was used to record the number of steps taken daily, and, from 36 to 84 months, the ActiGraph (AG; model 7164, version 2.2; AG Health Services, Fort Walton Beach, FL) accelerometer was used to measure PA via an internal accelerometer. The CHAMPS-derived self-report PA variable was reasonably and significantly correlated with these measures, r = .39 (P < .001) with pedometer step data (n = 277) and r = .44 (P < .001) with accelerometer count data (n = 210).
Stress management
Since objective measures of stress-management practices are not well established, a self-monitoring form was designed for this study.14 Participants indicated whether (or not) they performed each component of the stress-management routine which included at least: 20 minutes of yoga stretches, 15 minutes of progressive relaxation, and 5 minutes each of meditation and visualization. The total number of self-monitored minutes of stretching, relaxation, meditation, and visualization practices was computed from these binary data and averaged across 7 days for analysis.
Psychosocial Variables
Social support
The UCLA Social Support Inventory23 was used to measure several types, sources, and dimensions of supportive resources, as well as satisfaction with these resources. A total Positive scale, calculated as the sum of the satisfaction items, was used in the present analyses.
Problem-solving ability
The Diabetes Problem-Solving Interview was developed for adults with type 2 diabetes.24 For this study, the interview was modified to ask respondents to write a description of how they would react to 9 scenarios presenting potential challenges to program adherence. Coders scored responses to produce an average rating of problem-solving skill. Inter-rater reliability on these scores ranged from r = .57 to r = .90 and averaged r = .72. Six-month test-retest reliability using control group data was r = .51 for overall skill ratings.14
Self-efficacy
Confidence in Overcoming Challenges to Self-Care was used to assess confidence in overcoming obstacles to adhering to diet, PA, and stress management25 targets. This 49-item instrument assesses confidence in overcoming such factors as cost, time, social pressures, competing demands, and thoughts associated with achieving dietary, PA, and stress-management goals. Recent analyses of this instrument25 demonstrated reasonable psychometric properties (internal consistency alpha in the present study at baseline was .97). The total score was used in the present analyses.
Analyses
All data were entered and verified, and scores were calculated for multiple-item instruments according to previously established procedures. Descriptive analyses were used to clean data, and determine whether transformations were needed. Chi-square or t tests were used to evaluate differences between dropouts and those who completed the study at 7 years.
Long-term effects
Generalized estimating equations (GEE) models26 were used to compare long-term treatment effects on outcome measures from baseline to 5 years post-treatment. GEE models were specified using a first-order autoregressive correlation structure, and separate models were conducted to examine treatment group interactions with both linear and quadratic trends. Linear-trend results are presented here, as model results were similar for linear and quadratic trends. Age was covaried in all analyses, as it was found in univariate correlational analyses to be significantly associated with outcomes at baseline. Effect sizes (d) were calculated on difference scores from baseline only at time points where treatment effects were significant.
Missing data
The level of missing observations was not symmetrical across groups. Mean percent (averaged across 7 measures) of total observations missing at each assessment point were as follows: 0.1% UC vs. 0.9% MLP at baseline; 7.7% UC vs. 19.7% MLP at 6 months; 8.0% UC vs. 29.5% MLP at 12 months; 10.5% UC vs. 28.1% MLP at 24 months; 18.0% UC vs. 28.0% MLP at 36 months; 18.7% vs. 28.1% at 48 months; 20.2% vs. 31.4% at 60 months; 23.1% vs. 33.2% at 72 months; and 22.7% vs. 32.3% at 84 months. GEE analyses were performed 2 ways. First, a complete-case approach was used, in which participants with missing follow-up data on the outcome variable of interest were excluded from the analysis. Second, identical analyses were conducted after missing data were imputed using multiple imputation procedures via the expectation-maximization (EM) algorithm with NORM software.27 Both complete-case and intent-to-treat (imputed) results are presented in the tables for comparison.
Statistical analyses were performed using SPSS 12.0 (SPSS Inc., Chicago).
RESULTS
Participants
Of the 297 women who joined in the study, 207 completed the 84-month assessment, an attrition rate of 30%. Retention rates between treatment conditions did not differ significantly at the final (84-month) assessment (UC = 78% vs. MLP = 71%). Individuals were lost to follow-up for the following reasons: death (n = 22), failure to provide a follow-up contact (n = 8), or declined further participation (n = 42). Most participants who moved out of the area continued in the study by mail.
Usual care vs. MLP
As reported in Toobert at al.,17 women randomized to the MLP and UC conditions had few baseline differences. Briefly, study participants were a high-risk group, with an average body mass index exceeding 35 kg/m2, and most had multiple chronic illnesses. Their average age was 61 years (range 39 to 74). Most were married (57%) and living with a spouse or partner (51%) or widowed (19%). The majority (94%) of the sample was non-Hispanic white, followed by Hispanic (2.9%) and Native American Indian (1.4%). Average income was in the range of $30,000-$39,000 (2002 dollars), with 38% employed and 43% retired. A minority (42%) had a college education. The only significant difference between conditions at baseline was the percent taking estrogen therapy (47% UC vs. 59% MLP, P < .05); estrogen therapy was not significantly correlated with outcomes, and therefore was not covaried in the present GEE analyses.
Characteristics of participants vs. dropouts
Participants who provided data at 84 months were older when diagnosed with diabetes and had been diagnosed with diabetes for less time than those who did not complete the 7-year assessment (see Table 1).
Table 1.
Baseline Characteristics of Study Completers vs. Dropoutsa
| Characteristic | Completed Study n = 206 M (SD) or % |
Dropped n = 73 M (SD) or % |
P Value |
|---|---|---|---|
| Age | 61.1 (7.9) | 60.7 (8.0) | .735 |
| Weight (kg) | 92.0 (22.2) | 95.6 (22.6) | .237 |
| Waist/Hip Ratio | .90 (.07) | .91 (.09) | .765 |
| Body Mass Index (kg/m2) | 34.8 (8.0) | 36.6 (8.4) | .124 |
| Age Diagnosed With Diabetes | 53.5 (10.1) | 50.7 (10.4) | .044 |
| Years Diagnosed With Diabetes | 7.6 (6.7) | 10.5 (9.8) | .025 |
| Current Smoker | 9.7% | 8.2% | .707 |
| Income | .216 | ||
| $0 to $19,999 | 30.6% | 50.0% | |
| $20,000 to $39.999 | 34.2% | 44.3% | |
| $40,000 or more | 35.1% | 15.7% | |
| Type of Glucose-Lowering Medication | .627 | ||
| None | 21.8% | 20.5% | |
| Oral Medical Only | 59.2% | 53.4% | |
| Insulin Only | 8.3% | 12.3% | |
| Insulin and Oral Medication | 10.7% | 13.7% | |
| % Living Alone | 26.2% | 27.4% | .472 |
| Level of Education Achieved | .084 | ||
| 0-11th Grade | 9.7% | 9.6% | |
| High School Graduate | 26.2% | 21.9% | |
| Some College/Graduate | 64.1% | 68.5% | |
| Caucasian | 94.6% | 95.9% | .673 |
| Medications | |||
| Lipid-Lowering | 45.1% | 37.5% | .260 |
| Blood Pressure-Lowering | 44.7% | 52.8% | .235 |
| Estrogen Replacement Therapy | 54.9% | 52.8% | .671 |
| Number of Comorbidities | .681 | ||
| No Other Disease | 4.9% | 4.1% | |
| 1-2 Other Diseases | 46.1% | 52.1% | |
| ≥3 Other Diseases | 49.0% | 43.8% |
Note.
Chi-square or t test as appropriate.
Dropout is defined as an individual who did not complete any portion of the 84-month assessment.
Behavioral Outcomes
Table 2 presents results on the following behavioral measures: (a) dietary behavior, (b) PA, and (c) stress management. Since each of the GEE models was significant for the MLP compared to the UC, parameter estimates for the treatment-by-linear-trend interactions at each time point were examined to reveal significant time points. Significance and conclusions from intent-to-treat analyses were similar to those from complete-case analyses.
Table 2.
Behavioral Outcomes for Usual Care (UC) and Intervention (MLP) Conditions from Baseline to 84 Months
| Base- line |
6 Mo. |
12 Mo. |
24 Mo. |
36 Mo. |
48 Mo. |
60 Mo. |
72 Mo. |
84 Mo. |
Group × Time P |
||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Calories from Saturated Fat | |||||||||||
| Complete Cases (n = 157) | <.001 | ||||||||||
| UC | M | .12 | .12 | .12 | .12 | .10 | .10 | .10 | .10 | .10 | |
| Adjusted M | [.12] | [.12] | [.12] | [.11] | [.11] | [.10] | [.10] | [.10] | |||
| SD | .04 | .04 | .04 | .04 | .03 | .03 | .03 | .03 | .02 | ||
| MLP | M | .13 | .10 | .11 | .11 | .10 | .10 | .10 | .10 | .10 | |
| Adjusted M | [.10] | [.10] | [.11] | [.10] | [.10] | [.09] | [.10] | [.10] | |||
| SD | .04 | .03 | .03 | .03 | .03 | .03 | .03 | .03 | .03 | ||
| ES | .67 | 1.00 | .33 | ||||||||
| Intent To Treat (Imputed Data; n = 272) | <.001 | ||||||||||
| UC | M | .13 | .12 | .12 | .12 | .11 | .11 | .10 | .10 | .11 | |
| Adjusted M | [.12] | [.12] | [.12] | [.11] | [.11] | [.10] | [.11] | [.11] | |||
| SD | .04 | .04 | .04 | .04 | .03 | .03 | .03 | .03 | .03 | ||
| MLP | M | .13 | .10 | .11 | .11 | .10 | .10 | .10 | .10 | .10 | |
| Adjusted M | [.10] | [.11] | [.11] | [.10] | [.10] | [.10] | [.10] | [.10] | |||
| SD | .04 | .03 | .03 | .03 | .03 | .03 | .03 | .03 | .03 | ||
| ES | .67 | .67 | .33 | ||||||||
| Diet: Eating Habits Score (Kristal) | |||||||||||
| Complete Cases (n = 166) | <.001 | ||||||||||
| UC | M | 2.07 | 2.00 | 2.01 | 2.01 | 2.00 | 2.00 | 1.98 | 1.97 | 2.03 | |
| Adjusted M | [2.04] | [2.05] | [2.01] | [2.03] | [2.04] | [2.01] | [2.00] | [2.06] | |||
| SD | .40 | .41 | .38 | .40 | .40 | .40 | .41 | .41 | .38 | ||
| MLP | M | 2.19 | 1.81 | 1.84 | 1.86 | 2.02 | 2.05 | 2.06 | 2.04 | 2.05 | |
| Adjusted M | [1.81] | [1.80] | [1.82] | [1.98] | [2.01] | [2.03] | [2.01] | [2.02] | |||
| SD | .36 | .36 | .34 | .39 | .39 | .42 | .38 | .37 | .38 | ||
| ES | .84 | .85 | .79 | ||||||||
| Intent To Treat (Imputed Data; n = 279) | <.001 | ||||||||||
| UC | M | 2.09 | 2.02 | 2.04 | 2.04 | 2.01 | 2.04 | 1.99 | 2.01 | 2.05 | |
| Adjusted M | [2.04] | [2.05] | [2.06] | [2.03] | [2.06] | [2.01] | [2.03] | [2.07] | |||
| SD | .40 | .42 | .40 | .41 | .42 | .46 | .42 | .42 | .40 | ||
| MLP | M | 2.15 | 1.81 | 1.82 | 1.85 | 1.98 | 2.05 | 2.01 | 2.01 | 2.02 | |
| Adjusted M | [1.79] | [1.81] | [1.83] | [1.96] | [2.03] | [1.99] | [1.99] | [2.01] | |||
| SD | .37 | .38 | .35 | .40 | .42 | .43 | .41 | .41 | .39 | ||
| ES | .73 | .75 | .69 | ||||||||
| Physical Activity: Weighted Frequency of All Activity | |||||||||||
| Complete Cases (n = 166) | <.001 | ||||||||||
| UC | M | 19.8 | 19.3 | 18.4 | 20.2 | 16.7 | 17.8 | 17.0 | 15.6 | 15.4 | |
| Adjusted M | [18.1] | [17.6] | [19.3] | [15.7] | [16.8] | [16.2] | [14.9] | [14.7] | |||
| SD | 13.1 | 12.4 | 10.9 | 11.4 | 10.2 | 12.2 | 11.1 | 11.2 | 12.2 | ||
| MLP | M | 16.4 | 26.9 | 22.8 | 24.1 | 20.7 | 17.0 | 17.0 | 16.4 | 15.5 | |
| Adjusted M | [28.1] | [23.7] | [25.0] | [21.7] | [18.0] | [17.8] | [17.1] | [16.2] | |||
| SD | 10.4 | 13.6 | 12.0 | 16.9 | 16.4 | 12.3 | 11.1 | 10.3 | 10.9 | ||
| ES | .92 | .64 | .50 | .56 | |||||||
| Intent To Treat (Imputed Data; n = 279) | <.001 | ||||||||||
| UC | M | 17.4 | 18.6 | 17.1 | 18.4 | 15.9 | 16.1 | 16.0 | 14.6 | 14.9 | |
| Adjusted M | [18.2] | [16.8] | [18.1] | [15.5] | [15.8] | [15.7] | [14.4] | [14.6] | |||
| SD | 12.4 | 12.6 | 10.5 | 10.8 | 10.6 | 11.7 | 10.7 | 10.5 | 11.3 | ||
| MLP | M | 16.3 | 25.8 | 22.0 | 23.1 | 20.1 | 16.7 | 16.7 | 15.5 | 14.4 | |
| Adjusted M | [26.2] | [22.3] | [23.4] | [20.4] | [17.1] | [17.0] | [15.8] | [14.7] | |||
| SD | 10.8 | 13.6 | 12.3 | 15.3 | 14.7 | 12.5 | 10.5 | 10.4 | 11.1 | ||
| ES | .67 | .47 | .41 | ||||||||
| Stress Management Practice (Minutes/Week) | |||||||||||
| Complete Cases (n = 148) | .004 | ||||||||||
| UC | M | 9.7 | 11.3 | 9.4 | 10.4 | 12.7 | 14.9 | 12.5 | 11.3 | 10.9 | |
| Adjusted M | [10.5] | [8.6] | [9.5] | [11.7] | [13.8] | [11.3] | [10.8] | [10.1] | |||
| SD | 19.0 | 20.1 | 22.1 | 18.9 | 17.6 | 27.0 | 18.5 | 25.7 | 24.1 | ||
| MLP | M | 5.8 | 21.0 | 17.2 | 18.2 | 18.2 | 12.4 | 14.6 | 13.2 | 14.5 | |
| Adjusted M | [21.9] | [18.0] | [19.1] | [19.2] | [13.4] | [15.7] | [13.7] | [15.3] | |||
| SD | 15.3 | 17.4 | 17.3 | 16.6 | 30.8 | 19.8 | 23.2 | 20.0 | 25.2 | ||
| ES | .66 | ||||||||||
| Intent To Treat (Imputed Data; n = 279) | .031 | ||||||||||
| UC | M | 11.2 | 12.8 | 9.5 | 11.5 | 14.1 | 14.1 | 14.2 | 12.3 | 13.7 | |
| Adjusted M | [12.2] | [9.1] | [11.0] | [13.6] | [13.6] | [13.6] | [12.2] | [13.3] | |||
| SD | 21.8 | 22.6 | 21.4 | 19.8 | 19.3 | 23.5 | 19.4 | 23.9 | 28.9 | ||
| MLP | M | 8.5 | 21.0 | 16.0 | 16.0 | 16.7 | 14.4 | 16.0 | 13.6 | 14.5 | |
| Adjusted M | [21.7] | [16.5] | [16.5] | [17.2] | [14.9] | [16.6] | [13.7] | [14.9] | |||
| SD | 18.2 | 18.5 | 17.0 | 16.5 | 25.1 | 19.4 | 20.0 | 18.8 | 22.6 | ||
| ES | No significant individual time points | ||||||||||
Note.
Age was covaried in all analyses. Tabled significance (P) values are based on treatment-group-by-linear-trend interaction results in GEE analyses, reflecting the effect over the total 7-year time period. Adjusted means (in brackets) are adjusted for age and for the baseline value of the outcome variable at the follow-up time point. Effect sizes are shown only for those specific time points that were significant, and were calculated on difference scores from baseline.
Dietary patterns
Long-term analysis of FFQ data indicated that the intervention condition achieved the recommended saturated fat intake level requirement at 6 months (10% calories from saturated fat), and maintained a level of 10-11% calories from saturated fat through the 7 years of the study. The UC condition consumed 12% calories from saturated fat on average through 36 months. The 2 conditions converged after 24 months in complete-case analyses and after 48 months in intent-to-treat analyses because of continued improvement in the UC, with effect sizes ranging from .25 to 1.00. Analysis of scores on the Kristal measure indicated that the MLP group also engaged in fewer fat-intake-related behaviors than the UC group from 6 to 24 months (unadjusted mean eating habits scores for MLP = 2.19, 1.81, 1.84, and 1.86 at baseline and 6, 12, and 24 months, respectively, vs. 2.07, 2.00, 2.01, and 2.01 for UC). Effect sizes at these time points ranged from .69 to .85. The 2 groups did not differ significantly for the remainder of the 7-year study period because the UC condition improved during longer follow-up time periods.
PA
PA improvements in the MLP group, compared to the UC group, as measured by the CHAMPS, were greatest at 6 months and were maintained over 36 months, with unadjusted mean scores for the MLP of 16.4, 26.9, 22.8, 24.1, and 20.7 at baseline, and 6, 12, 24, and 36 months, respectively, compared to 19.8, 19.3, 18.4, 20.2, and 16.7 for the UC. Effect sizes ranged from .41 to .92. The 2 conditions converged at 48 months; the UC condition declined from 16.8 at 48 months to 14.7 at 84 months while the MLP declined from 18.0 to 16.2 over the same time points.
Stress management
Stress-management results from the 7-day self-monitoring log showed that MLP participants significantly increased the number of daily minutes they practiced stress-management techniques (yoga stretches, breathing, guided visualization, and meditation) compared to UC participants. At baseline and 6 months, MLP participants spent an unadjusted average of 6 and 21 minutes daily, respectively, practicing stress-management techniques, compared to 10 and 11 minutes for UC. The effect size at 6 months was .66. The 2 groups converged after 6 months due to the UC condition improving and the MLP condition performing stress management somewhat less often.
Psychosocial Variables
Table 3 presents results on the following psychosocial measures: (a) perceived support, (b) problem-solving ability, and (c) confidence in overcoming barriers (self-efficacy). As with behavioral outcomes, significance and conclusions from intent-to-treat analyses of psychosocial outcomes were very similar to those from complete-case analyses.
Table 3.
Psychosocial Outcomes for Usual Care (UC) and Intervention (MLP) Conditions from Baseline to 84 Months
| Base- line |
6 Mo. |
12 Mo. |
24 Mo. |
36 Mo. |
48 Mo. |
60 Mo. |
72 Mo. |
84 Mo. |
Group × Time P |
||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Social Support: UCLA Positive Summary Score | |||||||||||
| Complete Cases (n = 165) | <.001 | ||||||||||
| UC | M | 2.97 | 3.03 | 2.99 | 2.99 | 2.91 | 2.98 | 2.91 | 2.89 | 2.97 | |
| Adjusted M | [3.01] | [2.97] | [2.97] | [2.89] | [2.96] | [2.89] | [2.88] | [2.96] | |||
| SD | .58 | .72 | .76 | .68 | .60 | .67 | .66 | .62 | .69 | ||
| MLP | M | 2.91 | 3.44 | 3.34 | 3.23 | 2.91 | 2.90 | 2.98 | 2.97 | 2.94 | |
| Adjusted M | [3.46] | [3.36] | [3.25] | [2.92] | [2.92] | [3.00] | [2.99] | [2.96] | |||
| SD | .72 | .74 | .74 | .78 | .70 | .81 | .75 | .71 | .75 | ||
| ES | .76 | .60 | .45 | ||||||||
| Intent To Treat (Imputed Data; n = 279) | <.001 | ||||||||||
| UC | M | 2.96 | 3.02 | 2.99 | 2.99 | 2.88 | 2.95 | 2.87 | 2.85 | 2.89 | |
| Adjusted M | [3.01] | [2.99] | [2.98] | [2.88] | [2.95] | [2.87] | [2.84] | [2.89] | |||
| SD | .63 | .75 | .77 | .74 | .69 | .68 | .67 | .69 | .76 | ||
| MLP | M | 2.93 | 3.39 | 3.24 | 3.18 | 2.90 | 2.95 | 2.98 | 2.99 | 2.98 | |
| Adjusted M | [3.40] | [3.24] | [3.19] | [2.90] | [2.95] | [2.98] | [3.00] | [2.98] | |||
| SD | .72 | .70 | .69 | .78 | .71 | .77 | .73 | .67 | .74 | ||
| ES | .67 | .43 | |||||||||
| Quality of Problem-Solving Strategies | |||||||||||
| Complete Cases (n = 157) | .007 | ||||||||||
| UC | M | 3.6 | 3.7 | 4.0 | 3.9 | 3.9 | 3.9 | 4.2 | 4.0 | 4.0 | |
| Adjusted M | [3.7] | [4.0] | [3.9] | [3.9] | [3.9] | [4.2] | [4.0] | [4.1] | |||
| SD | .70 | .75 | .68 | .66 | .57 | .57 | .57 | .66 | .53 | ||
| MLP | M | 3.7 | 4.0 | 4.2 | 4.1 | 4.0 | 4.1 | 4.2 | 4.1 | 4.1 | |
| Adjusted M | [4.0] | [4.2] | [4.1] | [4.0] | [4.1] | [4.2] | [4.1] | [4.1] | |||
| SD | .69 | .73 | .59 | .64 | .57 | .58 | .58 | .56 | .57 | ||
| ES | .31 | .19 | .21 | ||||||||
| Intent To Treat (Imputed Data; n = 279) | .009 | ||||||||||
| UC | M | 3.6 | 3.6 | 3.9 | 3.8 | 3.8 | 3.8 | 4.1 | 3.9 | 4.0 | |
| Adjusted M | [3.6] | [3.9] | [3.8] | [3.8] | [3.9] | [4.1] | [3.9] | [4.0] | |||
| SD | .67 | .76 | .68 | .66 | .58 | .55 | .62 | .64 | .55 | ||
| MLP | M | 3.6 | 3.9 | 4.0 | 4.0 | 3.9 | 4.0 | 4.1 | 4.0 | 4.0 | |
| Adjusted M | [3.9] | [4.0] | [4.0] | [3.9] | [4.0] | [4.1] | [4.0] | [4.0] | |||
| SD | .72 | .78 | .68 | .68 | .65 | .58 | .64 | .58 | .55 | ||
| ES | .27 | .16 | .16 | ||||||||
| Self-Efficacy: Confidence to Overcome Challenges | |||||||||||
| Complete Cases (n = 161) | .012 | ||||||||||
| UC | M | 3.1 | 3.0 | 3.0 | 2.9 | 3.0 | 3.1 | 3.0 | 3.0 | 3.0 | |
| Adjusted M | [3.0] | [3.0] | [2.9] | [2.9] | [3.0] | [3.0] | [3.0] | [3.0] | |||
| SD | .71 | .81 | .79 | .80 | .72 | .74 | .77 | .75 | .68 | ||
| MLP | M | 3.0 | 3.1 | 3.2 | 3.2 | 3.1 | 3.0 | 3.0 | 3.0 | 3.0 | |
| Adjusted M | [3.1] | [3.2] | [3.2] | [3.1] | [3.0] | [3.1] | [3.0] | [3.0] | |||
| SD | .77 | .72 | .72 | .78 | .76 | .75 | .60 | .73 | .65 | ||
| ES | .44 | ||||||||||
| Intent To Treat (Imputed Data; n = 279) | .080 | ||||||||||
| UC | M | 3.0 | 2.9 | 2.9 | 2.9 | 2.9 | 3.0 | 2.9 | 3.0 | 3.0 | |
| Adjusted M | [2.9] | [2.9] | [2.9] | [2.9] | [3.0] | [2.9] | [2.9] | [3.0] | |||
| SD | .77 | .78 | .79 | .83 | .73 | .75 | .73 | .72 | .65 | ||
| MLP | M | 2.9 | 3.1 | 3.1 | 3.1 | 3.1 | 3.0 | 3.0 | 3.0 | 3.0 | |
| Adjusted M | [3.1] | [3.1] | [3.2] | [3.1] | [3.0] | [3.0] | [3.0] | [3.0] | |||
| SD | .79 | .74 | .76 | .82 | .77 | .78 | .66 | .71 | .70 | ||
| ES | .35 | .43 | |||||||||
Note.
Age was covaried in all analyses. Tabled significance (P) values are based on treatment-group-by-linear-trend interaction results in GEE analyses, reflecting the effect over the total 7-year time period. Adjusted means (in brackets) are adjusted for age and for the baseline value of the outcome variable at the follow-up time point. Effect sizes are shown only for those specific time points that were significant, and were calculated on difference scores from baseline.
Social support
GEE analyses revealed significant improvement for the MLP group in perceived social support as measured by the UCLA Positive support scale (unadjusted mean score = 2.9, 3.4, 3.3, and 3.2 for MLP at baseline, and 6, 12, and 24 months, respectively, vs. 3.0, 3.0, 3.0, and 3.0 for UC). Effect sizes ranged from .31 to .76. The groups did not significantly differ at 36 months and beyond. In general, the lack of significant between-condition effects at longer term was due to a return to near-baseline levels of perceived support in the MLP condition following the 24-month follow-up.
Problem-solving ability
GEE analysis indicated that the MLP group made significantly larger improvements in the quality of their problem-solving strategies compared to the UC group at 6, 12, and 24 months in the complete-cases analyses (unadjusted mean score = 3.7, 4.0, 4.2, and 4.1 for MLP at baseline, and 6, 24, and 48 months, respectively, compared to 3.6, 3.7, 4.0, and 3.9 for the UC group), and at 6, 24, and 48 months in the intent-to-treat analyses. Effect sizes ranged from .16 to .31. Underlying the inconsistent differences at longer-term assessments was that the UC condition improved problem-solving scores after the 6-month follow-up while the MLP condition maintained but did not enhance the initial gains made at 6 months.
Confidence to overcome barriers
Barriers-based self-efficacy as measured by the Confidence to Overcome Challenges measure significantly improved in the MLP group compared to the UC group. Higher mean efficacy levels were found for the MLP relative to UC at 6 months in intent-to-treat analysis and at 24 months in both complete-case and intent-to-treat analysis (unadjusted mean score = 3.0 and 3.2 for MLP at baseline and 24 months, respectively, vs. 3.1 and 2.9 for UC in complete-cases analyses). Thereafter, the 2 groups converged due to a decrease in self-efficacy among the MLP condition. Effect sizes ranged from .35 to .44.
Multiple Behavioral Outcomes
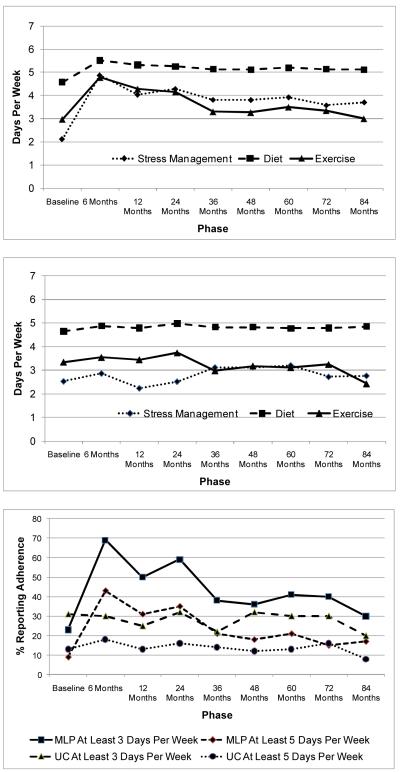
Figure 1 illustrates the extent to which study participants adhered to the 3 primary program targets (ie, Mediterranean diet, PA, and stress management), based on self-monitoring data. These variables were chosen for illustration instead of the previously reported outcomes because they were measured on the same scale and are readily interpreted. Graphs 1 and 2 show the self-monitored number of days per week that participants in the MLP (graph 1) and UC (graph 2) conditions adhered to the 3 primary program targets; graph 3 shows the proportion of MLP and UC participants who adhered to each of the 3 targets for at least 3 or 5 days per week.
Figure 1.
Adherence to Diet, PA, and Stress-management Targets
Note.
Graph 1 = MLP self-monitored days/week of achieving PA, diet, and stress-management targets. Graph 2 = UC self-monitored days/week of achieving PA, diet, and stress-management targets. Graph 3 = Percent of MLP and UC adhering to each of the 3 targets at least 3 or 5 days per week.
As shown in graphs 1 and 2, during the 24-month active intervention phase, significant improvements were seen in diet, PA, and stress-management practices in the MLP condition compared to the UC control condition. For both conditions, adherence to the dietary target was better maintained than PA, with stress-management practice falling in between. Although there were no longer significant differences between conditions at the later assessments, the patterns differed across behaviors. For diet, the UC condition remained essentially flat after 24 months; for PA, the MLP condition relapsed to baseline levels while the UC condition dropped below baseline levels at 84 months; and, for stress management, there was partial relapse in the MLP compared with moderate improvement in UC.
Graph 3 shows that, when behaviors were combined, about 22-32% of the UC condition reported meeting the targets at least 3 days/week throughout the study while in the MLP condition the proportions were considerably greater during the first 24 months: 69% at 6 months, 50% at 12 months, and 59% at 24 months. A similar pattern obtained for the proportions meeting targets at least 5 days/week. About 12-18% of the UC condition reported meeting the targets at least 5 days/week during the first 24 months, whereas in the MLP condition the proportions were 43% at 6 months, 31% at 12 months, and 35% at 24 months. Around 36-48 months, the 2 conditions converged.
DISCUSSION
Interventions that target multiple risk behaviors may better address the health needs of high-risk individuals and populations than single-risk-factor interventions,28 but there is a paucity of information about long-term effects in multiple-risk-factor trials. Our long-term (7-year) evaluation of a multiple-risk-behavior intervention was designed to track the natural history of initial multiple-behavior change with special attention to relations between the outcome variables.
The MLP, a moderately intensive group intervention, successfully promoted multiple-health-behavior change. During the 24-month active intervention, significant behavioral improvements were seen compared to the control condition. Improvements were greatest in the most intense phase of intervention (first 6 months; mean ES = .64 in complete-case analyses and .55 in intent-to-treat analyses). Between 6 and 24 months, patterns of change among the targeted behavioral outcomes showed only subtle differences. For example, 6-month improvement in saturated fat consumption was fairly well maintained. However, saturated fat consumption in the control condition also improved (decreased) at the longer-term assessments, possibly a result of periodic self-monitoring, which eliminated any advantage of intervention. Stress-management practices remained higher in the MLP relative to the UC throughout the 7 years of the study. While minutes of daily practice in the MLP declined over the years, they remained above baseline levels. In contrast, the 6-month treatment gains in PA gradually declined to baseline levels. With no additional intervention, treatment and control conditions converged near the 4-year assessment and remained similar throughout the 7-year assessment.
Group means over 7 years showed no indication of “competing” effects across behaviors, that is, gains in one outcome (eg, PA) did not appear to impair improvements in another outcome (eg, fat consumption). This study was not designed to examine how different treatment deliveries, such as sequential rather than concurrent behavior change, would impact treatment effects. It is possible that effects become diluted when spread over many intervention activities directed at many outcomes simultaneously, as in this intervention.29 On the other hand, synergistic beneficial effects may occur when comprehensive interventions such as the MLP integrate multiple components into a unified effort to change a whole lifestyle.5,17 Of primary interest in this study is that the patterns of behavior change and long-term effects in the MLP were similar, with dietary behavior better maintained than PA or stress-management outcomes.
Several explanations may be put forward for the tendency of health-behavior improvements to plateau or decline after the cessation of active intervention. Different processes may underlie initial change and maintenance. Some researchers have posited that initial behavior change requires effortful behavior while the success of long-term maintenance rests on the development of habitual behavior.30 It is also possible that social environmental factors may “wear one down” if the intervention relies on individual change without also addressing the social environment.31
The focus of the present analyses was on change in the MLP and UC groups as a whole. Planned future analyses will be aimed at identifying subgroups within the MLP that may exhibit different long-term patterns, such as those who show no change, those who respond strongly to the intervention and maintain healthful behaviors over time, and those who change behavior initially but then gradually relapse. Analytic approaches such as mixture modeling are well suited to revealing growth trajectories and predictors of change.32
The major strength of this study was its basis on 7 years of data on multiple intervention outcomes. Other strengths were the 70% retention rate, the use of GEE analyses, and the finding of similar results across complete-case and intent-to-treat analyses using imputed data. A limitation of the study was the use of primarily self-report measures. Most of these measures have been validated against more objective standards, but it is not known whether possible inaccuracies of self-reporting in this study influenced the observed results.
Future Directions
Most multiple-health behavior research focuses on short-term change. More studies should examine how multiple-health behavior change is sustained over the long term. The hope of achieving permanent lifestyle changes from a relatively brief intervention might be unrealistic. Some populations, such as those at extreme risk or who live and work in unhealthful environments, may require ongoing intervention.33 Just as pharmacological treatment for chronic illnesses generally is prescribed for long periods, health-behavior intervention may require long active treatment with continued contact to achieve sustained maintainance.8,34 To be feasible, long-term behavioral interventions must be affordable and fit within the demands of daily living. Even short-term behavioral interventions should include components to enhance long-term maintenance of initial behavior change. The MLP, for example, could have encouraged more use of community resources for PA and stress-management during the active intervention phase, with the expectation that participants would continue to avail themselves of these resources post-treatment.
Because individual-level interventions produce health-behavior changes that tend to plateau or return to baseline levels post-treatment, alternative methods for achieving long-term outcomes are needed. Such a program might target environmental influences (eg, media, industry, schools, home, community, government) that encourage unhealthful lifestyle practices. Changes at the systems level, combined with individual-level change, hold promise for improving sustainability. Future studies should aim at discovering the most effective mix of intervention types to produce lasting change. Designing and testing multi-component, sustainable behavioral interventions for postmenopausal women with type 2 diabetes in medical and community settings are highly encouraged. This type of research will require “fully tackling the challenges that really matter in the long term,” according to Altman.1 We should explore new ways to tackle the problem through systems interventions and address the factors that impede sustainable solutions.
Acknowledgments
This study was supported by a grant from the National Heart, Lung, and Blood Institute (1-R01-HL077120). The authors acknowledge the invaluable contributions of the staff of the MLP, including Melda DeSalvo, Katie Geiser, Sally Skolnick, Shannon McCarthy, Shari Reyna, Debbie Proctor, and Phil Warner. We are deeply indebted to the 279 dedicated and committed women who participated in the MLP.
REFERENCES
- 1.Altman DG. Challenges in sustaining public health interventions. Health Educ Behav. 2009;36:24–28. doi: 10.1177/1090198107299788. [DOI] [PubMed] [Google Scholar]
- 2.Roumen C, Corpeleijn E, Feskens EJM, et al. Impact of 3-year lifestyle intervention on postprandial glucose metabolism: the SLIM study. Diabet Med. 2008;25:597–605. doi: 10.1111/j.1464-5491.2008.02417.x. [DOI] [PubMed] [Google Scholar]
- 3.Wilcox S, Parra-Medina D, Thompson-Robinson M, Will J. Nutrition and physical activity interventions to reduce cardiovascular disease risk in health care settings: a quantitative review with a focus on women. Nutr Rev. 2001;59:197–214. doi: 10.1111/j.1753-4887.2001.tb07012.x. [DOI] [PubMed] [Google Scholar]
- 4.Wing RR, Epstein LH, Nowalk MP, Koeske RH. Behavior change, weight loss, and psychological improvements in type II diabetic patients. J Consult Clin Psychol. 1985;53:111–122. doi: 10.1037//0022-006x.53.1.111. [DOI] [PubMed] [Google Scholar]
- 5.Gaede P, Vedel P, Larsen N, et al. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;348:383–393. doi: 10.1056/NEJMoa021778. [DOI] [PubMed] [Google Scholar]
- 6.Van Horn L, McCoin M, Kris-Etherton PM, et al. The evidence for dietary prevention and treatment of cardiovascular disease. J Am Diet Assoc. 2008;108:287–331. doi: 10.1016/j.jada.2007.10.050. [DOI] [PubMed] [Google Scholar]
- 7.Niebauer J, Hambrecht R, Velich T, et al. Attenuated progression of coronary artery disease after 6 years of multifactorial risk intervention: Role of physical exercise. Circulation. 1997;96:2534–2541. doi: 10.1161/01.cir.96.8.2534. [DOI] [PubMed] [Google Scholar]
- 8.Norris SL, Lau J, Smith SJ, et al. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25:1159–1171. doi: 10.2337/diacare.25.7.1159. [DOI] [PubMed] [Google Scholar]
- 9.De Vries H, van’t Riet J, Spigt M, et al. Clusters of lifestyle behaviors: results from the Dutch SMILE study. Prev Med. 2008;46:203–208. doi: 10.1016/j.ypmed.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 10.Rosal MC, Ockene JK, Luckmann R, et al. Coronary heart disease multiple risk factor reduction. Am J Prev Med. 2004;27:54–60. doi: 10.1016/j.amepre.2004.04.020. [DOI] [PubMed] [Google Scholar]
- 11.Prochaska JJ, Spring B, Nigg CR. Multiple health behavior change research: an introduction and overview. Prev Med. 2008;46:181–188. doi: 10.1016/j.ypmed.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Daubenmier JJ, Weidner G, Sumner MD, et al. The contribution of changes in diet, exercise, and stress management to changes in coronary risk in women and men in the multisite cardiac lifestyle intervention program. Ann Behav Med. 2007;33:57–68. doi: 10.1207/s15324796abm3301_7. [DOI] [PubMed] [Google Scholar]
- 13.Toobert DJ, Strycker LA, Glasgow RE, Bagdade JD. If you build it, will they come? Reach and adoption associated with a comprehensive lifestyle management program for women with type 2 diabetes. Patient Educ Couns. 2002;48:1–7. doi: 10.1016/s0738-3991(02)00120-9. [DOI] [PubMed] [Google Scholar]
- 14.Toobert DJ, Strycker LA, Glasgow RE, et al. Effects of the Mediterranean Lifestyle Program on multiple risk behaviors and psychosocial outcomes among women at risk for heart disease. Ann Behav Med. 2005;29:128–137. doi: 10.1207/s15324796abm2902_7. doi: 10.1186/1479-5868-4-1 PMCID: PMC1783667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Toobert DJ, Glasgow RE, Strycker LA, et al. Long-term effects of the Mediterranean Lifestyle Program: a randomized clinical trial for postmenopausal women with type 2 diabetes. Int J Behav Nutr Phys Act. 2007 doi: 10.1186/1479-5868-4-1. doi:10.1186/1479-5868-4-1 PMCID: PMC1557654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jacobs-van der Bruggen MAM, van Baal PH, Hoogenveen RT, et al. Cost-effectiveness of lifestyle modification in diabetic patients. Diabetes Care. 2009;32:1453–1458. doi: 10.2337/dc09-0363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Toobert DJ, Strycker LA, Glasgow RE, et al. Enhancing support for health behavior change among women at risk for heart disease: the Mediterranean Lifestyle Trial. Health Educ Res. 2002;17:574–585. doi: 10.1093/her/17.5.574. [DOI] [PubMed] [Google Scholar]
- 18.de Lorgeril M, Renaud S, Mamelle N, et al. Mediterranean alph-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet. 1994;343:1454–1459. doi: 10.1016/s0140-6736(94)92580-1. [DOI] [PubMed] [Google Scholar]
- 19.Ornish D., Dr. Dean Ornish’s Program for Reversing Heart Disease. Ballantine Books; New York: 1990. [Google Scholar]
- 20.Patterson RE, Kristal A, Tinker LF, et al. Measurement characteristics of the Women’s Health Initiative Food Frequency Questionnaire. Ann Epidemiol. 1999;9:178–187. doi: 10.1016/s1047-2797(98)00055-6. [DOI] [PubMed] [Google Scholar]
- 21.Shannon J, Kristal AR, Curry SJ, Beresford SAA. Application of a behavioral approach to measuring dietary change: the Fat- and Fiber-Related Diet Behavior Questionnaire. Cancer Epidemiol Biomarkers Prev. 1997;6:355–361. [PubMed] [Google Scholar]
- 22.Stewart AL, Verboncoeur CJ, McLellan BY, et al. Physical activity outcomes of CHAMPS II: a physical activity promotion program for older adults. J Gerontol. 2001;56:M465–M470. doi: 10.1093/gerona/56.8.m465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schwarzer R, Dunkel-Schetter C, Kemeny ME. The multidimensional nature of received social support in gay men at risk of HIV infection and AIDS. Am J Community Psychol. 1994;22:319–339. doi: 10.1007/BF02506869. [DOI] [PubMed] [Google Scholar]
- 24.Glasgow RE, Toobert DJ, Barrera M, Strycker LA. Assessment of problem solving: a key to successful diabetes self-management. J Behav Med. 2004;27:477–490. doi: 10.1023/b:jobm.0000047611.81027.71. [DOI] [PubMed] [Google Scholar]
- 25.Glasgow RE, Toobert DJ, Gillette CD. Psychosocial barriers to diabetes self-management and quality of life. Diab Spectrum. 2001;14:33–41. [Google Scholar]
- 26.Zeger SL, Liang KY. The analysis of discrete and continuous longitudinal data. Biometrics. 1986;42:121–130. [PubMed] [Google Scholar]
- 27.Schafer JL. NORM: multiple imputation of incomplete multivariate data under a normal model, version 2.03, software for Windows 95/98/NT. 1999 Available from < www.stat.psu.edu/~jls/misoftwa.html>.
- 28.Rohm-Young D, Vollmer WM, King AC, et al. Can individuals meet multiple physical activity and dietary behavior goals? Am J Health Behav. 2009;33:277–286. doi: 10.5993/ajhb.33.3.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prochaska JO. Multiple health behavior research represents the future of preventive medicine. Prev Med. 2008;46:281–285. doi: 10.1016/j.ypmed.2008.01.015. [DOI] [PubMed] [Google Scholar]
- 30.Rothman AJ. Toward a theory-based analysis of behavioral maintenance. Health Psychol. 2000;19:64–69. doi: 10.1037/0278-6133.19.suppl1.64. 2000. [DOI] [PubMed] [Google Scholar]
- 31.Orleans CT. Promoting the maintenance of health behavior change: recommendations for the next generation of research and practice. Health Psychol. 2000;19:76–83. doi: 10.1037/0278-6133.19.suppl1.76. [DOI] [PubMed] [Google Scholar]
- 32.Muthén B, Brown CH, Masyn K, et al. General growth mixture modeling for randomized preventive interventions. Biostatistics. 2002;3:459–475. doi: 10.1093/biostatistics/3.4.459. [DOI] [PubMed] [Google Scholar]
- 33.Bellg AJ. Maintenance of health behavior change in preventive cardiology: internalization and self-regulation of new behaviors. Behav Mod. 2003;27:103–131. doi: 10.1177/0145445502238696. [DOI] [PubMed] [Google Scholar]
- 34.Turk MW, Yang K, Hravnak M, et al. Randomized clinical trials of weight loss maintenance: a review. J Cardiovasc Nurs. 2009;24:58–80. doi: 10.1097/01.JCN.0000317471.58048.32. [DOI] [PMC free article] [PubMed] [Google Scholar]