Abstract
Although child impulsivity is associated with oppositional defiant disorder (ODD) symptoms, few studies have examined whether family processes moderate this association. To address this gap, we tested whether child-reported family routine moderated the relation between child hyperactivity/impulsivity (HI) and ODD symptoms among a sample of low-income, urban, ethnic-minority children (N=87, 51% male). Child HI and ODD symptoms were assessed using parent and teacher reports. HI also was indexed by a laboratory task. Family routine was assessed using child self-report. Hierarchical regression analyses indicated that family routine moderated child HI. Among children with higher levels of teacher-reported HI symptoms, lower levels of family routine were associated with higher levels of teacher-reported ODD symptoms compared to children with lower levels of teacher-reported HI symptoms. Children who self-reported higher levels of family routine were rated as low on teacher-reported ODD symptoms, regardless of teacher-reported HI levels. Parent report and laboratory measures of child HI did not produce significant interactions. Lower levels of family routine may confer risk for ODD symptoms among low-income, urban, ethnic-minority children experiencing higher levels of HI.
Keywords: Family routine, Impulsivity, Oppositional defiant disorder, Parenting
Impulsivity has been described as a deficit in behavioral inhibition (Barkley 2006; Olson et al. 1999). Children exhibiting impulsive behaviors are at greater risk of displaying externalizing problem behaviors (e.g., oppositionality, aggression, conduct disorder) compared to children without these behaviors (Ackerman et al. 2003; Eiraldi et al. 1997). Moreover, impulsivity is linked to both parent and teacher ratings of externalizing behaviors from early childhood through adolescence (Olson et al. 1999). Identifying contextual factors that moderate relations between impulsivity and externalizing behaviors in middle childhood may have important implications for interventions aimed at reducing pernicious externalizing behaviors in late childhood and adolescence, including conduct disorder, delinquency, and antisocial behavior (Lahey and Loeber 1994; White et al. 1994).
Studies linking attention-deficit/hyperactivity disorder (ADHD) and ODD symptoms provide evidence of relations between impulsivity and externalizing behaviors in childhood. Impulsivity is recognized as the underlying core behavioral deficit of ADHD (Barkley 2006) and often co-occurs with ODD (Angold and Costello 1996; Drabick et al. 2004; Gadow and Nolan 2002), which is characterized by defiant, hostile, and oppositional behaviors toward adults (American Psychiatric Association 2000). Importantly, children with the ADHD-combined subtype (hyperactivity-impulsivity and inattentive components) are more likely to meet diagnostic criteria for ODD than children without ADHD or those diagnosed with ADHD-predominantly inattentive subtype (Eiraldi et al. 1997; Gadow et al. 2004), suggesting that impulsivity may be more likely to covary with ODD symptoms. In addition, the co-occurrence of impulsivity and ODD symptoms is associated with numerous maladaptive correlates and outcomes, including higher levels of aggression, attention problems, depression, anxiety, peer and family difficulties, and academic problems (Carlson et al. 1997; Drabick et al. 2004; Gadow and Nolan 2002; Kuhne et al. 1997; Speltz et al. 1999). Thus, factors that may serve to decrease the association between child impulsivity and ODD symptoms could be protective against the emergence of ODD symptoms, as well as these negative correlates and sequelae.
Empirical work designed to identify family factors that maintain, exacerbate, or reduce ODD symptoms among impulsive children has long been encouraged (Frick et al. 1992), and much research demonstrates that parental discipline, monitoring, and control are associated with child externalizing problems (Chamberlain and Patterson 1995; Deater-Deckard and Dodge 1997; Patterson and Stouthamer-Loeber 1984; Pettit et al. 2001). However, little empirical work has evaluated the moderating role of familial factors on impulsivity (Bates et al. 1998; Johnston and Mash 2001). Although impulsivity has substantial biological influences (Barkley 2006; Winstanley et al. 2006) and its relation with ODD symptoms is well established (Eiraldi et al. 1997; Gadow et al. 2004), additional contextual factors (e.g., parenting variables) may moderate this relation. For example, parents of impulsive children may find it difficult to discipline their children because frequent impulsivity may lead to more negative parent behaviors (e.g., coercion, inconsistent discipline), which also increase the likelihood of children’s exhibiting ODD symptoms (Reid et al. 2002). Thus, the combination of child impulsivity and problematic parenting practices may lead to greater risk for ODD symptoms than the presence of either impulsivity or problematic parenting alone. Given this dearth of literature, we examined the possible role of child-reported family routine as a moderator of child impulsivity in the present study.
Family routine refers to the level at which parents provide structure, consistency, and organization in the home environment (Voydanoff et al. 1994) and has been examined across developmental periods spanning from preschool to adolescence (e.g., Brody and Flor 1997; Koblinsky et al. 2006; Taylor 1996). Given this description, child-reported family routine may be especially important among children exhibiting higher levels of impulsivity. Specifically, child-reported family routine may provide organization and predictability and thereby decrease risk of ODD symptoms. Structured routines increase child compliance by facilitating predictability of cues in the child’s environment and fostering the development of rule-governed behavior, which may consequently lead to lower levels of externalizing problems (Koblinsky et al. 2006; Sytsma et al. 2001; Taylor 1996; Taylor and Lopez 2005). Potentially, relations between consistent family routine and lower levels of externalizing behavior may be explained by promotion of self-regulation among children, which likely decreases impulsive behaviors (Brody and Flor 1997). The literature on family routine suggests that family routine is associated with lower levels of externalizing behaviors, but it is not clear whether this association extends to the relation between child-reported family routine and child impulsivity.
The importance of implementing structured routines also has been emphasized in behavioral clinical interventions. For example, behavioral parent training recommends provision of structured and consistent routines in both the home and school to reduce impulsivity, improve completion of tasks, and facilitate responsible behavior (Chronis et al. 2004; Pelham and Fabiano 2008). Child management skills often involve setting up a home environment that reinforces good behaviors in home and school, which indirectly increases structure in family routine and tasks (Barkley 1997). Such exposure to structured home environments may reduce the frequency of impulsivity among children, perhaps because children have fewer novel opportunities to engage in impulsive behaviors and may be better able to link their behaviors to consequences when predictable routines are followed. Thus, examining relations among child-reported family routines in the home environment and child impulsivity can contribute to the empirical framework for these clinical interventions and ensure that interventions are as effective as possible.
In the present study, we examined a sample of first through third grade low-income, urban, ethnic-minority boys and girls for several reasons. First, because children residing in urban, low socioeconomic status (SES) neighborhoods are reportedly more likely to exhibit externalizing behaviors (Attar et al. 1994; Brody et al. 2001; Gorman-Smith and Tolan 1998), identifying factors that may moderate the effect of child impulsivity among contextually disadvantaged samples is especially warranted. Second, examining familial processes and child behaviors among an economically disadvantaged sample allows for the isolation of effects associated with poverty and other contextual variables (Dodge et al. 1994). For instance, the effect of impulsivity on juvenile delinquency is greater in poorer neighborhoods (Lynam et al. 2000). Third, individuals of lower SES who meet diagnostic criteria for ADHD are more likely to meet diagnostic criteria for ODD and CD than their higher SES counterparts (Eiraldi et al. 1997). Fourth, McCoy et al. (1999) reported that ineffective parenting practices largely mediated the effect of SES on conduct problems, suggesting that parenting practices are important to consider in research examining the relation between SES and externalizing problems. Last, living in urban, low SES neighborhoods is associated with numerous contextual disadvantages, such as physical and psychosocial stressors, deviant peer groups, and violence, each of which has been linked to child behavior problems (Attar et al. 1994; Brody et al. 2001; Gorman-Smith and Tolan 1998). Ethnic minorities are disproportionately affected by these issues, given that they are more likely to reside in poor, segregated neighborhoods in urban areas (Leventhal and Brooks-Gunn 2004). Thus, we evaluated the potential protective role of child-reported family routines among low income, urban youth who are at elevated risk for ODD symptoms.
Presently, there is also a lack of research on sex differences related to impulsivity in the context of family routine. Many past studies have either excluded girls or have not compared boys vs. girls, though boys tend to display higher levels of impulsivity than girls (Cote et al. 2002; Else-Quest et al. 2006; Hartung et al. 2002). Given sex differences in levels of child impulsivity, the association between family routine and impulsivity may differ across sex, which could in turn lead to differing levels of ODD symptoms among boys and girls.
Another issue that confounds understanding of childhood externalizing behaviors involves a typical reliance on single, rather than multiple, informants of child behaviors. This is a crucial limitation given that informants do not necessarily agree on the frequency and severity of child externalizing behaviors, and risk factors and correlates associated with childhood externalizing problems differ depending on informant (De Los Reyes and Kazdin 2005; Drabick et al. 2007, 2008). Research that considers multiple strategies for integrating parent- and teacher-reported ODD symptoms suggests that ODD symptoms may be better conceptualized as source- or informant-specific phenomena (Drabick et al. 2007; Offord et al. 1996). For example, studies considering source-specific ADHD and ODD symptoms (Drabick et al. 2004, 2007; Gadow et al. 2004; Offord et al. 1996) indicate that the correlates of ADHD and ODD differ based on informant used to rate child symptoms, suggesting that the processes that moderate symptoms may differ depending on the informant also. Possible explanations for informant differences include that children behave differently in different settings and contextual demands on the child likely vary between settings, which could lead to distinct correlates for child behaviors depending on context (De Los Reyes and Kazdin 2005). Contextual demands in school, combined with teachers’ experiences with many children, may contribute to greater specificity in teachers’ ratings of child symptoms and more differential prediction to outcomes (Drabick et al. 2007, 2008). To address these potential contextual and informant differences, we examined multiple informants for child HI and ODD symptoms in the present study.
Taking the gaps in the literature into account, the purpose of this study was to examine whether child-reported family routine moderated the relation between child impulsivity and ODD symptoms among low-income, urban, ethnic-minority girls and boys. We used multiple strategies for assessing child HI and ODD symptoms. We expected that children with higher, compared to lower, levels of HI symptoms would exhibit higher levels of ODD symptoms, consistent with previous literature. We also hypothesized that children exhibiting higher levels of impulsivity who reported higher levels of family routine would exhibit lower levels of ODD symptoms than children reporting lower levels of family routine. Also, we expected that children with higher levels of impulsivity and lower levels of family routine would engage in higher levels of ODD symptoms than those endorsing higher levels of family routine.
Method
Participants
The sample consisted of 87 children (M= 7.75, SD= 1.05 years; 51.1% male; 93.2% African-American, 6.8% Latino/a) and their primary caregivers (85% biological mothers) drawn from three public schools in Philadelphia. The urban neighborhoods in which families reside experience high levels of crime, poverty, and racial/ethnic homogeneity (primarily African-American and Latino families). Crime data for Philadelphia suggest that the participants reside in neighborhoods with the highest rates of aggravated assaults, robberies, burglaries, prostitution, narcotic arrests, and domestic abuse incidents (http://cml.upenn.edu/crimebase). Based on census data, neighborhood household income and education are consistent with the study sample (http://factfinder.census.gov). Neighborhood level data indicate that 42% of families report a household income that falls below poverty threshold, compared to 58% in the present sample, and 40% of adults report having less than a high school education, compared to 25% in the present sample. In terms of parental configurations, 51.7% percent of the children lived in single-parent households, 32.2% in intact (i.e., two-biological parent) households, 6.9% in blended households, and 9.2% in other family configurations (grandparental, adoptive). Sixteen percent of primary caregivers reported that they were married. About half of the caregivers had completed high school (51.8%), 25.3% had less than a high school education, and 23.9% had completed education beyond high school. Sixty-four percent of the children lived in families receiving public assistance. The majority of families reported an annual household income of less than $20,000 (66.3%); 18.1% reported income from $20,000–$29,999; 8.4% reported income from $30,000–$39,999; and 7.2% reported income over $40,000.
Procedure
The study was approved by Temple University’s Institutional Review Board. Families recruited for participation had a child enrolled in either first, second, or third grade in 1 of 3 elementary schools that participated in a partnership program with Temple University. Families were sent a description of the study, parental consent form, and a self-addressed, stamped postcard. Families interested in participating either returned the postcard with contact information or called the lab to make an appointment. The sample characteristics (i.e., ethnicity, sex, family SES) reflect the schools from which the families were drawn; nevertheless, due to confidentiality requirements, no information was available to compare those who self-selected into the study and those that did not. Interested families were scheduled for two visits at our research lab, each lasting 2–3 h. Caregivers and children provided consent and assent, respectively, prior to participation. Caregivers completed questionnaires related to their child, family, and themselves. Children worked with a trained research assistant on various tasks. Families were paid for their participation and reimbursed for transportation. Children received a small gift. Teachers were contacted following parental consent and were sent measures related to the child’s behaviors in school. Teachers were paid for each set of measures completed and a donation was made to the school for each child that participated.
Although teacher reports were requested for all participants, teacher reports were obtained for only a subset of children (n=64, 74%). Multiple attempts were made to obtain teacher reports, including sending several letters containing child measures to teachers, visiting teachers in school, offering bonus incentives, and principals’ making additional requests to the teachers. We requested reports from a total of 32 teachers. Number of reports requested from each teacher ranged from 1 to 9 (M=2.53, SD=2.02; Mdn=2; mode=1). Because of the timing of recruitment and family participation, children were drawn from two consecutive cohorts. As such, teachers from whom 4 or more reports were requested had children in two consecutive cohorts. Twenty-five teachers (78%) completed measures; on average, each teacher provided ratings for 2.63 children (SD=1.81) and completed 72% of the reports requested. Seven teachers completed none of the requested reports; of these 7, 6 had one report assigned, and 1 had 2 reports assigned. Analyses examining differences between the children for whom teacher measures were and were not completed revealed no significant differences for child sex or race/ethnicity (both χ2s<1.48, both ps>0.05), or for child age, household income, or primary caregiver education (all ts<1.01, all ps>0.05). Thus, there did not appear to be any systematic demographic differences between these groups. However, given that we asked teachers to report on multiple children, and thus children were nested within classrooms, we calculated intraclass correlations to determine whether we should address nesting (described below; Grawitch and Munz 2004; Kenny et al. 2002).
Measures
Income-to-needs ratio
Caregivers reported on household income using a background information questionnaire that also included questions related to parental education, occupation, marital status, and living arrangements. Families were asked to report on their annual household income using a scale from 1 (0 to $9,999) to 9 (Over $80,000). Using US Census Bureau data (www.census.gov), we determined the poverty thresholds for each family based on the number of adults and related children under age 18 living in the home. We then calculated the income-to-needs ratio by dividing reported income by poverty threshold. For the present sample, income-to-needs ratios ranged from 0.23 to 3.46 (M=0.99, SD=0.65). Based on the income-to-needs ratios, 58% of participating children were below 100% of the poverty threshold, and 75% of children were below 125% of the poverty threshold (compared to 14.3% and 18.3%, respectively, in PA).
Family structure
Using information from the background questionnaire, we coded primary caregivers’ reports of whether the participating child lived in a 2-parent household (0 = no, 1= yes; 32% (n=28) reported living in a 2-parent household).
Child IQ
The 2-subtest format of Vocabulary and Matrix Reasoning from the Wechsler Abbreviated Scale of Intelligence (WASI; Psychological Corporation 1999) was administered to estimate Full Scale IQ. The WASI two-subtest format Full Scale IQ correlates 0.81 with the Wechsler Intelligence Scale for Children-III.
Hyperactivity/Impulsivity
HI was operationalized using a definition consistent with ADHD-Predominantly Hyperactive-Impulsive subtype symptoms (ADHD-HI; APA 2000) and assessed using three strategies. Both parents and teachers rated the child’s HI symptoms using their respective versions of the Child Symptom Inventory-4 (CSI-4; Gadow and Sprafkin 1994, 2002), which contains the behavioral symptoms of most childhood disorders described in the Diagnostic and statistical manual of mental disorders-Fourth edition (DSM-IV; APA 1994). Individual items bear one-to-one correspondence with DSM-IV symptoms (i.e., high content validity). Nine items reflect ADHD-HI subtype symptoms. Sample items include, “Has difficulty awaiting turn in group activities,” “Interrupts people or butts into other children’s activities,” and “Blurts out answers to questions before they have been completed.” Items were rated from 0 (never) to 3 (very often). The sum of the responses to each item was used as an index of ADHD-HI symptoms (αs for parent-reported ADHD-HI = 0.92, for teacher-reported ADHD-HI = 0.95).
Children also completed the Intra/Extra Dimensional Set Shift (IED) subtest from the Cambridge Neuropsychological Test Automated Battery (CANTAB), a computer-based touch-screen system that has been shown to be reliable and valid among children (Luciana and Nelson 2002). The IED examines rule acquisition and ability to shift attentional set, and is similar to the Wisconsin Card Sort task. Participants are required to use computer-provided feedback to learn response contingencies. This test measures an individual’s ability to attend to specific attributes of compound stimuli, and to shift attention from one characteristic to another depending on the set criterion for each stage. Children with higher levels of impulsivity are expected to maintain similar patterns of responding even when given computer feedback that the responses are incorrect; that is, higher levels of impulsivity could lead to potential perseveration or difficulty inhibiting prepotent responses and shifting set when contingencies change on this task. The standardized score for the total number of errors was used as a third index of impulsivity.
Family routine
The Child Puppet Interview (CPI) was used to obtain children’s reports of family routine. The CPI is a developmentally sensitive and age-appropriate tool for assessing the subjective experiences of young children, and was developed in collaboration with the MacArthur Foundation Research Network on Psychopathology and Development (Sessa et al. 2001; Silk et al. 2004). The puppet interview is administered to children individually, and children’s responses are videotaped for later coding by trained research assistants (κs range from 0.98 to 1.00). In the interview, children are presented with two puppets that offer opposing statements and are asked to pick which puppet is more like them (Sessa et al. 2001). Responses were scored as 0 or 1, where 1 indicated the presence of a perceived structured routine. Items were summed to create a child-reported family routine score (6 items, α=0.53). Items involve events with which each child in first through third grade has experience (i.e., meals, bedtime, getting ready for school, homework) and ask whether children engage in these activities in similar ways each day. Sample items include, “I get ready for school the same way every day/I do not get ready for school the same way every day,” “I have to do homework at the same time every day/I do not have to do my homework at the same time every day,”“I get ready for bed the same way every night/I do not get ready for bed the same way every night,” and “I go to bed around the same time every night/I go to bed at different times every night.”
The CPI is a reliable and valid assessment instrument for children (Sessa et al. 2001; Silk et al. 2004). This interview was validated among three samples of children drawn from the same neighborhoods in which the present study was conducted, and ranging from preschool to third grade (N=260). In the measure validation samples, the child self-reported routine scale exhibited good internal consistency (α=0.74) and 4-week test–retest reliability (r=0.74). In addition, child self-reported parenting scales were more highly associated with observer-reported than parent-reported parenting behaviors among ethnic-minority families and families of low SES (Sessa et al. 2001). Given similarities between the measure validation samples and the sample in the present study, we selected the CPI to index child-reported family routine.
ODD symptoms
Parents and teachers reported on ODD symptoms using their respective versions of the CSI-4 (Gadow and Sprafkin 1994, 2002). Eight items reflect DSM-IV symptoms of ODD (e.g., “Argues with adults,” “Does things to deliberately annoy others,” and “Is angry and resentful”) and were rated on a scale from 0 (never) to 3 (very often). The sum of these items was used to create an ODD symptom severity score (αs=0.90 for parent report, 0.96 for teacher report). Because the goal of the present study was to examine processes associated with ODD symptoms, which even at sub-diagnostic levels are associated with increased levels of impairment (Angold et al. 1999), we chose to examine these symptoms dimensionally. Compared to scores derived from the community-based samples used to norm the CSI-4 (Gadow and Sprafkin 2002), the present sample was rated as exhibiting higher ODD symptom severity scores based on both parent and teacher reports. Specifically, boys in the current vs. normative sample, respectively, were on average elevated on parent-reported (7.1 vs. 5.4) and teacher-reported (6.6 vs. 2.6) ODD symptom severity scores. Similarly, girls in the current vs. normative sample, respectively, were on average elevated on parent-reported (5.5 vs. 4.4) and teacher-reported (5.8 vs. 1.1) ODD symptom severity scores.
Statistical analyses
Given that children were nested within classrooms, we first calculated intraclass correlations (ICCs) using ANOVA-based procedures recommended by Grawitch and Munz (2004), Kenny et al. (2002), and given unequal group sizes, Kenny and La Voie (1985), to determine whether we should control for nesting. Given that we obtained data from 25 teachers, sufficient power (0.80; α=0.05) for a large effect size (f=0.40) is attained with a sample size of 113 (Faul et al. 2007). Because of our smaller sample size, we followed recommendations (Grawitch and Munz 2004; Kenny et al. 2002) for minimizing Type II errors by using a more liberal alpha (0.25) as evidence of nonindependence.
Given that we had complete data for all variables except for teacher-reported data (26% missing), we used multiple imputation. Use of certain strategies (e.g., complete casewise analysis or listwise deletion, complete case analyses or pairwise deletion, nonresponse weighting, mean imputation) may bias an analytic sample (Bodner 2008; Graham 2009; Little and Rubin 2002; Rubin 1987). Multiple imputation (MI) fills in missing data with predicted values based on available data, and then results are averaged across datasets to obtain final estimates of effects (Rubin 1987; Schafer 1997). The analytic benefit of MI over other types of imputation is that MI imputes multiple values for each missing value, allowing for variability resulting from both sampling error and model uncertainty. Based on previous recommendations (Graham 2009; Little and Rubin 2002; Schafer 1997), we included auxiliary variables in the MI that were consistent with our conceptual model. These variables included demographic and family-level variables (sex, age, income-to-needs ratio, family structure, race/ethnicity); child IQ; child-reported family routine; parent- and teacher-reported HI and ODD symptoms; and child IED performance.
We used recommendations by Bodner (2008) to estimate the number of imputations that would allow for relatively precise estimation and accurate significance levels given our sample size and percent of missing data. Based on these recommendations, we imputed 20 datasets. We used SAS Proc MI (SAS Institute Inc. 2006) to deal with missing data, and the remaining analyses were conducted in Mplus version 5.2 (Muthén and Muthén 1998–2007), which averaged results across the 20 imputed datasets. For the two teacher-reported variables that had missing data in the original data set, means, SDs, and ranges using MI (N= 1,740) vs. listwise deletion (n=64), respectively, were as follows: teacher-reported HI symptoms, Ms=7.33 and 6.64, SDs=6.71 and 6.93, ranges=0–27; and teacher-reported ODD symptoms, Ms=6.23 and 5.58, SDs=6.08 and 6.29, ranges=0–24. Because the other variables were not missing data, their means and SDs remained the same after MI.
We conducted descriptive statistics and bivariate correlations to examine relations among the predictor and outcome variables. To examine potential sex differences in predictor and outcome variables, we conducted independent sample t-tests. The primary analyses involved hierarchical linear regression analyses, for which parent- or teacher-rated ODD behaviors were the dependent variable. The child’s sex (0 = male, 1 = female); age; income-to-needs ratio; family structure (0 = not 2-parent household, 1 = 2-parent household); and IQ were entered in the first step. In the second step, the conditional child impulsivity and child-reported family routine variables and the cross-product interaction terms for each index of child HI and child-reported family routine were entered. To minimize multicollinearity, before inclusion in the multiple regression analyses, the independent variables were centered (M=0) and interaction terms were created using centered variables (Aiken and West 1991). For significant interaction terms, we followed post-hoc probing procedures outlined by Holmbeck (2002).
Results
We first calculated ICCs for each of the study variables to determine whether observations could be considered independent despite our requesting reports on multiple children from several teachers. None of the ICCs was significant, even at the more liberal level (p<0.25) recommended to decrease the chances of committing a Type II error (ICCs ranged from 0.05 to 0.99, ps ranged from 0.60 to 0.99). These findings suggest that the within-group observations were not correlated with each other and could be considered independent observations; thus, we did not control for nesting in the present sample.
Bivariate correlations, means, and standard deviations for study variables, combined across the 20 imputed datasets, are presented in Table 1. Teacher-reported ODD symptoms were associated with parent-reported ODD symptoms, teacher-reported HI symptoms, and parent-reported HI symptoms. Parent-reported ODD symptoms were associated with parent-reported HI symptoms and teacher-reported HI symptoms. In addition, parent- and teacher-reported HI symptoms were associated. Unexpectedly, age was negatively associated with IQ and family routine, suggesting that among this self-selected sample, older children scored more poorly on the WASI IQ subtests and reported lower levels of family routine. We controlled for age and IQ in subsequent regression analyses; however, the reason for these unexpected associations requires further research.
Table 1.
Bivariate correlations, means, and standard deviations for study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. TCSI-4 ODD symptoms | – | ||||||||
| 2. CSI-4 ODD symptoms | 0.29** | – | |||||||
| 3. Age | 0.12 | 0.20 | – | ||||||
| 4. WASI IQ | 0.03 | −0.12 | −0.29** | – | |||||
| 5. Income-to-needs ratio | 0.00 | 0.05 | 0.02 | 0.22* | – | ||||
| 6. TCSI-4 HI symptoms | 0.63*** | 0.41*** | 0.00 | 0.13 | 0.14 | – | |||
| 7. CSI-4 HI symptoms | 0.22* | 0.70*** | 0.18 | −0.08 | 0.05 | 0.45*** | – | ||
| 8. Intra/Extra Dimensional Set Shift | 0.11 | −0.01 | 0.15 | 0.32** | −0.02 | 0.06 | −0.13 | – | |
| 9. Family routine | −0.18 | 0.02 | −0.36*** | −0.07 | −0.06 | 0.03 | 0.09 | −0.17 | – |
| M | 6.23 | 6.31 | 7.75 | 88.07 | 0.99 | 7.33 | 8.87 | −0.80 | 4.12 |
| SD | 6.08 | 5.12 | 1.05 | 13.42 | 0.65 | 6.71 | 7.07 | 1.30 | 1.45 |
TCSI-4 ODD = teacher-reported ODD symptoms, CSI-4 ODD = parent-reported ODD symptoms, WASI IQ = Wechsler Abbreviated Scale of Intelligence, TCSI-4 HI = teacher-reported HI, CSI-4 HI = parent-reported HI
p<0.05
p<0.01
p<0.001
Independent sample t-tests (boys vs. girls) indicated that boys and girls differed on parent-reported HI symptoms, t (85)=2.11, p=0.04, Cohen’s d=0.46 (boys > girls); and teacher-reported HI symptoms, t(85) = 2.19, p = 0.03, Cohen’s d=0.48 (boys > girls). There were no significant sex differences in terms of ODD symptoms, IED task performance, child-reported family routine, or background variables (ts ranged from 0.08 to 1.43, ps ranged from 0.16 to 0.94).
The first set of hierarchical linear regression analyses considered parent-reported ODD symptoms as the outcome variable (Table 2). Child sex, age, IQ, income-to-needs ratio, and family structure were entered in Step 1. None of these variables significantly predicted parent-reported ODD symptoms. Step 2 included Step 1 variables and (a) one of the conditional HI variables (parent-reported HI, teacher-reported HI, or IED), (b) the conditional family routine variable, and (c) the respective HI × family routine interaction term. Parent-reported HI symptoms (β=0.69, p<0.001) and teacher-reported HI symptoms (β=0.41, p<0.01) were significantly associated with parent-reported ODD symptoms. None of the respective HI × family routine interaction terms was significant: parent-reported HI × routine (β=−0.12, p=0.17), teacher-reported HI × routine (β=0.02, p=0.87), and IED × routine (β=−0.10, p=0.36).
Table 2.
Summary of hierarchical regression analyses for variables predicting parent-reported ODD symptoms
| Predictors | Parent-reported HI |
Teacher-reported HI |
IED |
|||
|---|---|---|---|---|---|---|
| β | R2 (f2) | β | R2 (f2) | β | R2 (f2) | |
| Step 1 | 0.08 (0.09) | 0.08 (0.09) | 0.08 (0.09) | |||
| Sex | −0.15 | −0.15 | −0.15 | |||
| Age | 0.18 | 0.18 | 0.18 | |||
| IQ | −0.08 | −0.08 | −0.08 | |||
| Income-to-needs ratio | 0.07 | 0.07 | 0.07 | |||
| Family structure | −0.05 | −0.05 | −0.05 | |||
| Step 2 | 0.51*** (1.04) | 0.24* (0.32) | 0.09 (0.10) | |||
| Sex | −0.02 | −0.04 | −0.16 | |||
| Age | 0.02 | 0.21 | 0.23 | |||
| IQ | −0.04 | −0.12 | −0.09 | |||
| Income-to-needs ratio | 0.02 | 0.03 | 0.08 | |||
| Family structure | 0.00 | −0.06 | −0.07 | |||
| Index of HIa | 0.69*** | 0.41** | 0.03 | |||
| Family routine | −0.07 | 0.08 | 0.13 | |||
| HI × routinea | −0.12 | 0.02 | −0.10 | |||
HI was indexed by parent-reported HI symptoms, teacher-reported HI symptoms, and child IED performance (see column headings)
Sex was coded as 0 (male) or 1 (female), family structure was coded as 0 (not 2-parent household) or 1 (2-parent household), HI = hyperactivity/impulsivity, IED = intra/extra dimensional set shift, effect size = f2
p<0.05
p<0.01
p<0.001
The second set of hierarchical regression analyses considered teacher-reported ODD symptoms as the outcome variable (Table 3). Among Step 1 variables, only family structure predicted teacher-reported ODD symptoms (β=−0.22, p<0.05). Step 2 included Step 1 variables and (a) one of the conditional HI variables (parent-reported HI, teacher-reported HI, or IED), (b) the conditional family routine variable, and (c) the respective HI × family routine interaction term. Teacher-reported HI symptoms (β=0.67, p<0.001) and family routine (β=−0.21, p<0.05) were associated with teacher-reported ODD symptoms in analyses considering teacher-reported HI symptoms. The parent-reported HI × family routine (β=0.09, p=0.49) and IED × family routine (β=−0.01, p=0.96) interaction terms were not significant.
Table 3.
Summary of hierarchical regression analyses for variables predicting teacher-reported ODD symptoms
| Predictors | Parent-reported HI |
Teacher-reported HI |
IED |
|||
|---|---|---|---|---|---|---|
| β | R2 (f2) | β | R2 (f2) | β | R2 (f2) | |
| Step 1 | 0.08 (0.09) | 0.08 (0.09) | 0.08 (0.09) | |||
| Sex | −0.07 | −0.07 | −0.07 | |||
| Age | 0.17 | 0.17 | 0.17 | |||
| IQ | 0.09 | 0.09 | 0.09 | |||
| Income-to-needs ratio | 0.00 | 0.00 | 0.00 | |||
| Family structure | −0.22* | −0.22* | −0.22* | |||
| Step 2 | 0.14 (0.16) | 0.53*** (1.13) | 0.10 (0.11) | |||
| Sex | −0.01 | 0.08 | −0.08 | |||
| Age | 0.10 | 0.07 | 0.10 | |||
| IQ | 0.05 | 0.01 | 0.03 | |||
| Income-to-needs ratio | −0.01 | −0.08 | 0.00 | |||
| Family structure | −0.18 | −0.20 | −0.21 | |||
| Index of HIa | 0.21 | 0.67*** | 0.08 | |||
| Family routine | −0.11 | −0.21* | −0.10 | |||
| HI × routinea | 0.09 | −0.20* | −0.01 | |||
HI was indexed by parent-reported HI symptoms, teacher-reported HI symptoms, and child IED performance (see column headings)
Sex was coded as 0 (male) or 1 (female), family structure was coded as 0 (not 2-parent household) or 1 (2-parent household), HI = hyperactivity/impulsivity, IED = intra/extra dimensional set shift, effect size = f2
p<0.05
p<0.001
The teacher-reported HI × routine interaction term was significant (β=−0.20, p=0.025). Thus, we followed procedures outlined by Aiken and West (1991) and Holmbeck (2002) for probing and graphing this 2-way interaction. We computed two new conditional moderator variables (±1 SD from the mean of child-reported family routine) and new interactions that incorporated the conditional variables. We then ran two post-hoc regressions, each of which involved simultaneous entry of teacher-reported HI, one of the conditional child-reported family routine variables, and the HI × conditional routine variable (Holmbeck 2002). From these analyses, we derived unstandardized betas (slopes) and regression equations among children reporting high (1 SD above the mean) and low (1 SD below the mean) family routine (Aiken and West 1991; Fig. 1). For high family routine, the slope was not significant (b=1.73, p=0.11). For low family routine, the slope was significantly different from zero (b=6.06, p<0.001). Examination of Fig. 1 indicates that children who reported high levels of family routine exhibited similar (and low) levels of teacher-reported ODD symptoms, regardless of their levels of teacher-reported HI symptoms. However, among children who reported lower levels of family routine, higher levels of teacher-reported HI symptoms were associated with higher levels of ODD symptoms, and lower levels of teacher-reported HI symptoms were associated with lower levels of ODD symptoms.
Fig. 1.
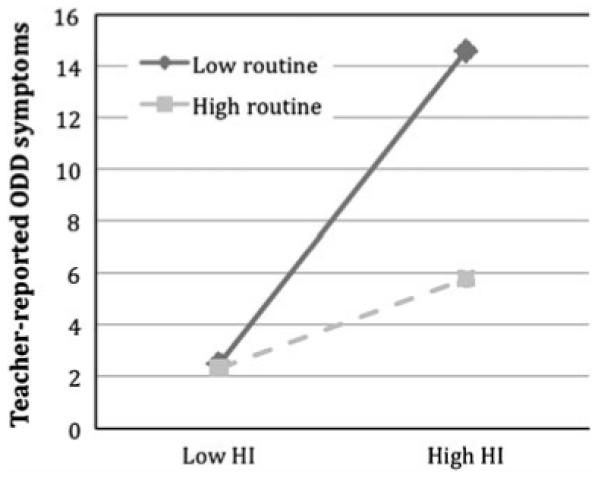
The relation between teacher-reported hyperactivity/impulsivity (HI) and teacher-reported ODD symptoms among children reporting low (1 SD below mean) vs. high (1 SD above mean) family routine
Discussion
Relations between child impulsivity and ODD symptoms are well established; however, little research has examined familial factors that may moderate the impulsivity-ODD association and potentially serve a protective function by mitigating or precluding the development of ODD symptoms. Clinical interventions recommend the implementation of family routines to reduce externalizing behaviors, but there is a paucity of research evaluating associations between family routine and ODD symptoms among impulsive children. To address this gap, we evaluated whether child-reported family routine moderated the association between child impulsivity and ODD symptoms. Examination of the significant impulsivity × routine interaction term indicated that in the context of lower levels of perceived family routine, higher levels of teacher-reported HI symptoms were associated with higher levels of teacher-reported ODD symptoms. However, children who reported higher levels of perceived family routine were rated by teachers as exhibiting low levels of ODD symptoms, regardless of teacher-reported HI levels. This pattern of findings suggests that despite the extensive literature linking HI and ODD symptoms (Angold and Costello 1996; Drabick et al. 2004; Gadow and Nolan 2002), associations between teacher-reported HI and ODD symptoms may be attenuated in the context of high levels of perceived family routine.
Because various contextual and informant processes likely contribute to informant discrepancies, consideration of parent and teacher reports of ODD symptoms, which provide the most context-dependent information about a child’s behavior, is important (Drabick et al. 2008). Child perceived family routine moderated relations between teacher-reported HI and ODD symptoms, but not parent-reported symptoms. It is possible that the effects of child-reported routine may be less salient in the home and instead better observed in more structured settings, such as the classroom. These findings are in line with previous research indicating that teacher reports may provide a more differentiated understanding of correlates associated with externalizing problems, including ADHD and ODD (Drabick et al. 2004, 2007; Gadow et al. 2004). Of course, informants differentially emphasize certain behaviors based on their beliefs regarding which behaviors warrant treatment, and children may behave differently in different settings because of distinct contextual demands and expectations (De Los Reyes and Kazdin 2005; Drabick et al. 2007). Thus, although our goal was to include multiple strategies to assess child HI and ODD symptoms, future research that systematically evaluates combined and source-specific informant reports is important for testing whether the moderating role of child-reported family routine differs based on the strategies used to combine ODD symptom information from multiple informants and sources.
Several limitations of this study should be taken into account. Impulsivity, routine, and ODD symptoms were assessed concurrently; therefore, no causal inferences about ODD symptoms can be drawn. Moreover, the association between parenting and child individual differences likely involves transactional effects (Reid et al. 2002), suggesting that child impulsivity also influences the degree of child-reported family routine provided by the parent (Johnston and Mash 2001). Also, future research should consider bidirectional relations between impulsivity and ODD, as it is possible that ODD symptoms contributed to levels of impulsivity. It is also unknown to what degree these factors influenced each other prior to the study. Thus, longitudinal studies are necessary to determine how these processes operate prior to middle childhood, whether child-reported family routine has an enduring effect on ODD symptoms, whether ODD symptoms maintain or exacerbate impulsivity, and whether interactions between impulsivity and child-reported routine variables change over time.
In addition, the internal consistency index (α) for child-reported family routine was lower than would be desired. We believed that it was important to use a parenting measure that had been validated among low-income, ethnic-minority children (Sessa et al. 2001; Silk et al. 2004). Also, we chose to consider the child’s perception of routine, as opposed to using an alternative index, given that children’s reports may better capture their perceptions of structure and perceived importance of adhering to rules and adult requests. We also wanted to include different reporters and methods to minimize the effects of shared variance. Future research should assess alternative ways of operationalizing family routine to determine whether the low internal consistency index (α) stemmed from the child puppet interview, use of child self-report, or sample characteristics (e.g., age, contextual risk), and whether prediction differs based on strategy for assessing routine. Finally, the sampling method (i.e., self selection) introduces the possibility of sampling biases, and additional studies are needed to determine whether the moderating effect of child-reported family routine generalizes to other SES and ethnic groups.
Despite these limitations, the results of this study have implications for clinical and empirical work. Current clinical interventions emphasize the utility of structured routines for reducing ODD symptoms (Barkley 1997; Brinkmeyer and Eyberg 2003), but this is the first study to our knowledge to empirically demonstrate that child-reported family routine moderates the relation between teacher-reported impulsivity and teacher-reported ODD symptoms. Child-reported family routine may provide impulsive children with an environment that fosters predictable consequences and facilitates the development of coping strategies that may decrease the display of ODD symptoms, particularly in the school setting. Parental behaviors are one of the more feasible points of change for clinicians and the present study provides additional support for continuing interventions aimed at modifying parental provision of family routine. Additionally, given our consideration of children’s self-report of family routine, inclusion of children in the development and implementation of family routine may be useful as well.
Future research also should examine parenting behaviors associated with routine and daily events in the home that may foster adaptive behaviors among children. Identifying additional parental behaviors that accompany family routine can increase our understanding of the processes by which parenting promotes structured routines that moderate impulsivity, which may prevent or mitigate ODD symptoms. For instance, parents who advocate structured routines in the home environment also may be more likely to be involved in their children’s schooling, which could influence achievement and behaviors in school. In addition, identifying the most effective ways in which parents with impulsive children can promote family routine is crucial. Indeed, our findings suggest that higher levels of perceived family routine are associated with lower levels of teacher-reported ODD symptoms, even among children who reportedly exhibit higher levels of teacher-reported impulsivity. Furthermore, exploring alternative pathways linking impulsivity and ODD symptoms is necessary. For instance, ODD symptoms may exacerbate children’s impulsivity, particularly if the perceived levels of family routine are low; that is, low levels of perceived family routine might contribute to lower levels of structure and rule-governed expectations, as well as increased opportunities to engage in disruptive behaviors. Future studies expanding this line of inquiry can address these issues and provide further support for interventions among children who exhibit co-occurring impulsivity and ODD symptoms.
In sum, the present study builds on research indicating that considering interactions between child and parenting factors can enhance our understanding of the development of externalizing behaviors among children. The findings suggest that one possible link between child impulsivity and ODD symptoms involves lower levels of child-reported family routine, though the patterns of results differed based on informant. Our focus on a contextually high-risk sample of children can inform etiological and prevention models for this population and suggests that further examination of structured routines in the home environment can facilitate efforts to minimize or preclude ODD symptoms among children exhibiting elevated levels of impulsivity.
Acknowledgments
This research was supported in part by grants from Temple University Office of the Vice President for Research and College of Liberal Arts and NIMH 1K01 MH073717-01A2 awarded to Dr. Drabick. We are particularly indebted to the families, principals, and school staff who participated in this research.
Contributor Information
H. Isabella Lanza, Department of Psychology, Temple University, Philadelphia, PA, USA; Integrated Substance Abuse Programs, Semel Institute for Neuroscience and Human Behavior, University of California, Los Angeles, 1640 S. Sepulveda Blvd., Ste. 200, Los Angeles, CA 90025, USA.
Deborah A. G. Drabick, Department of Psychology, Temple University, Philadelphia, PA, USA
References
- Ackerman BP, Brown E, Izard CE. Continuity and change in levels of externalizing behavior in school of children from economically disadvantaged families. Child Development. 2003;74:694–709. doi: 10.1111/1467-8624.00563. [DOI] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Sage; Newbury Park: 1991. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington: 1994. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. Fourth edition. Author; Washington: 2000. Text revision. [Google Scholar]
- Angold A, Costello EJ. Toward establishing an empirical basis for the diagnosis of oppositional defiant disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:1205–1212. doi: 10.1097/00004583-199609000-00018. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ, Farmer EMZ, Burns BJ, Erkanli A. Impaired but undiagnosed. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:129–137. doi: 10.1097/00004583-199902000-00011. [DOI] [PubMed] [Google Scholar]
- Attar BK, Guerra NG, Tolan PH. Neighborhood disadvantage, stressful life events, and adjustment in urban elementary-school children. Journal of Clinical Child Psychology. 1994;23:391–400. [Google Scholar]
- Barkley RA. Defiant children: A clinician’s manual for assessment and parent training. Guilford; New York: 1997. [Google Scholar]
- Barkley RA. Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment. 3rd ed. Guilford; New York: 2006. [Google Scholar]
- Bates JE, Pettit GS, Dodge KA, Ridge B. Interaction of temperamental resistance to control and restrictive parenting in the development of externalizing behavior. Developmental Psychology. 1998;34:982–995. doi: 10.1037//0012-1649.34.5.982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodner TE. What improves with increased missing data imputations? Structural Equation Modeling. 2008;15:651–675. [Google Scholar]
- Brinkmeyer MY, Eyberg SM. Parent–child interaction therapy for oppositional children. In: Kazdin AE, Weisz JR, editors. Evidence-based psychotherapies for children and adolescents. Guildford; New York: 2003. pp. 204–223. [Google Scholar]
- Brody GH, Flor DL. Maternal psychological functioning, family processes, and child adjustment in rural, single-parent African American families. Developmental Psychology. 1997;33:1000–1011. doi: 10.1037//0012-1649.33.6.1000. [DOI] [PubMed] [Google Scholar]
- Brody GH, Ge X, Conger R, Gibbons FX, Murry VM, Gerrard M, et al. The influence of neighborhood disadvantage, collective socialization, and parenting on African American children’s affiliation with deviant peers. Child Development. 2001;72:1231–1246. doi: 10.1111/1467-8624.00344. [DOI] [PubMed] [Google Scholar]
- Carlson CL, Tamm L, Gaub M. Gender differences in children with ADHD, ODD, and co-occurring ADHD/ODD identified in a school population. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1706–1714. doi: 10.1097/00004583-199712000-00019. [DOI] [PubMed] [Google Scholar]
- Chamberlain P, Patterson GR. Discipline and child compliance in parenting. In: Bornstein MH, editor. Handbook of parenting, Vol. 4: Applied and practical parenting. Erlbaum; Mahwah: 1995. pp. 205–225. [Google Scholar]
- Chronis AM, Chacko A, Fabiano GA, Wymbs BT, Pelham WE. Enhancements to the behavioral parent training paradigm for families of children with ADHD: review and future and directions. Clinical Child and Family Psychology Review. 2004;7:1–27. doi: 10.1023/b:ccfp.0000020190.60808.a4. [DOI] [PubMed] [Google Scholar]
- Cote T, Tremblay RE, Nagin D, Zoccolillo M, Vitaro F. The development of impulsivity, fearfulness, and help-fulness during childhood: patterns of consistency and change in the trajectories of boys and girls. Journal of Child Psychology and Psychiatry. 2002;43:609–618. doi: 10.1111/1469-7610.00050. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: a critical review, theoretical framework, and recommendations for further study. Psychological Bulletin. 2005;131:483–509. doi: 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- Deater-Deckard K, Dodge KA. Externalizing behavior problems and discipline revisited: nonlinear effects and variation by culture context, and gender. Psychological Inquiry. 1997;8:16–175. [Google Scholar]
- Dodge KA, Pettit GS, Bates JE. Socialization mediators of the relation between socioeconomic status and child conduct problems. Child Development. 1994;65:649–665. [PubMed] [Google Scholar]
- Drabick DAG, Gadow KD, Carlson GA, Bromet EJ. ODD and ADHD symptoms in Ukranian children: external validators and comorbidity. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:735–743. doi: 10.1097/01.chi.0000120019.48166.1e. [DOI] [PubMed] [Google Scholar]
- Drabick DAG, Gadow KD, Loney J. Source-specific oppositional defiant disorder: comorbidity and risk factors in referred elementary schoolboys. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:92–101. doi: 10.1097/01.chi.0000242245.00174.90. [DOI] [PubMed] [Google Scholar]
- Drabick DA, Gadow KD, Loney J. Co-occurring ODD and GAD symptom groups: source-specific syndromes and cross-informant comorbidity. Journal of Clinical Child and Adolescent Psychology. 2008;37:314–326. doi: 10.1080/15374410801955862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eiraldi RB, Power TJ, Nezu CM. Patterns of comorbidity associated with subtypes of attention-deficit/hyperactivity disorder among 6- to 12-year-old children. Journal of the American Academy of Child and Adolescence Psychiatry. 1997;36:503–514. doi: 10.1097/00004583-199704000-00013. [DOI] [PubMed] [Google Scholar]
- Else-Quest NM, Hyde JS, Goldsmith HH, Van Hulle CA. Gender differences in temperament: a meta-analysis. Psychological Bulletin. 2006;132:33–72. doi: 10.1037/0033-2909.132.1.33. [DOI] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang A-G, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Lahey BB, Loeber R, Stouthamer-Loeber M, Christ MAG, Hanson K. Familial risk factors to oppositional defiant disorder and conduct disorder: parental psychopathology and maternal parenting. Journal of Consulting and Clinical Psychology. 1992;60:49–55. doi: 10.1037//0022-006x.60.1.49. [DOI] [PubMed] [Google Scholar]
- Gadow KD, Nolan EE. Differences between preschool children with ODD, ADHD, and ODD+ADHD symptoms. Journal of Child Psychology and Psychiatry. 2002;43:191–201. doi: 10.1111/1469-7610.00012. [DOI] [PubMed] [Google Scholar]
- Gadow KD, Sprafkin J. Child Symptom Inventories manual. Checkmate Plus; Stony Brook: 1994. [Google Scholar]
- Gadow KD, Sprafkin J. Child Symptom Inventory-4 screening and norms manual. Checkmate Plus; Stony Brook: 2002. [Google Scholar]
- Gadow KD, Drabick DAG, Loney J, Sprafkin J, Salisbury H, Azizian A, et al. Comparison of ADHD symptom subtypes as source-specific syndromes. Journal of Child Psychology and Psychiatry. 2004;45:1135–1149. doi: 10.1111/j.1469-7610.2004.00306.x. [DOI] [PubMed] [Google Scholar]
- Gorman-Smith D, Tolan P. The role of exposure to community violence and developmental problems among inner-city youth. Development and Psychopathology. 1998;10:101–116. doi: 10.1017/s0954579498001539. [DOI] [PubMed] [Google Scholar]
- Graham JW. Missing data analysis: making it work in the real world. Annual Review of Psychology. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- Grawitch MJ, Munz DC. Are your data nonindependent? A practical guide to evaluating nonindependence and within-group agreement. Understanding Statistics. 2004;3:231–257. [Google Scholar]
- Hartung CM, Willcutt EG, Lahey BB, Pelham WE, Loney J, Stein MA, et al. Sex differences in young children who meet criteria for attention deficit hyperactivity disorder. Journal of Clinical Child and Adolescent Psychology. 2002;31:453–464. doi: 10.1207/S15374424JCCP3104_5. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN. Post-hoc probing of significant moderational and meditational effects in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Johnston C, Mash E. Families of children with attention-deficit/hyperactivity disorder: review and recommendations. Clinical Child and Family Psychology Review. 2001;4:183–205. doi: 10.1023/a:1017592030434. [DOI] [PubMed] [Google Scholar]
- Kenny DA, La Voie L. Separating individual and group effects. Journal of Personality and Social Psychology. 1985;48:339–348. [Google Scholar]
- Kenny DA, Mannetti L, Pierro A, Livi S, Kashy DA. The statistical analysis of data from small groups. Journal of Personality and Social Psychology. 2002;83:126–137. [PubMed] [Google Scholar]
- Koblinsky SA, Kuvalanka KA, Randolph SM. Social skills and behavior problems of urban African American preschoolers: role of parenting practices, family conflict, and maternal depression. American Journal of Orthopsychiatry. 2006;76:554–563. doi: 10.1037/0002-9432.76.4.554. [DOI] [PubMed] [Google Scholar]
- Kuhne M, Schachar R, Tannock R. Impact of comorbid oppositional or conduct problems on attention-deficit hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1715–1725. doi: 10.1097/00004583-199712000-00020. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Loeber R. Framework for a developmental model of oppositional defiant disorder and conduct disorder. In: Routh DK, editor. Disruptive behavior disorders in childhood. Plenum; New York: 1994. pp. 139–180. [Google Scholar]
- Leventhal T, Brooks-Gunn J. A randomized study of neighborhood effects on low-income children’s educational out-comes. Developmental Psychology. 2004;40:488–507. doi: 10.1037/0012-1649.40.4.488. [DOI] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical analyses with missing data. 2nd ed. Wiley; New York: 2002. [Google Scholar]
- Luciana M, Nelson CA. Assessment of neuropsychological function through use of the Cambridge Neuropsychological Testing Automated Battery: performance in 4- to 12-year old children. Developmental Neuropsychology. 2002;22:595–624. doi: 10.1207/S15326942DN2203_3. [DOI] [PubMed] [Google Scholar]
- Lynam DR, Caspi A, Moffitt TE, Wikstrom PH, Loeber R. The interaction between impulsivity and neighborhood context on offending: the effects of impulsivity are stronger in poorer neighborhoods. Journal of Abnormal Psychology. 2000;109:563–574. doi: 10.1037//0021-843x.109.4.563. [DOI] [PubMed] [Google Scholar]
- McCoy MG, Frick PJ, Loney BR, Ellis ML. The potential mediating role of parenting practices in the development of conduct problems in a clinic-referred sample. Journal of Child and Family Studies. 1999;8:477–494. [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 5th ed. Muthén & Muthén; Los Angeles, CA: 1998-2007. [Google Scholar]
- Offord DR, Boyle MH, Racine Y, Szatmari P, Fleming JE, Sanford M, et al. Integrating assessment data from multiple informants. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:1078–1085. doi: 10.1097/00004583-199608000-00019. [DOI] [PubMed] [Google Scholar]
- Olson SL, Schilling EM, Bates JE. Measurement of impulsivity: construct coherence, longitudinal stability, and relationship with externalizing problems in middle childhood and adolescence. Journal of Abnormal Child Psychology. 1999;27:151–165. doi: 10.1023/a:1021915615677. [DOI] [PubMed] [Google Scholar]
- Patterson GR, Stouthamer-Loeber M. The correlation of family management practices and delinquency. Child Development. 1984;55:1299–1307. [PubMed] [Google Scholar]
- Pelham WE, Fabiano GA. Evidence-based psychosocial treatments for attention deficit/hyperactivity disorder. Journal of Clinical Child and Adolescent Psychology. 2008;37:184–214. doi: 10.1080/15374410701818681. [DOI] [PubMed] [Google Scholar]
- Pettit GS, Laird RD, Dodge KA, Bates JE, Criss MM. Antecedents and behavior-problem outcomes of parental monitoring and psychological control in early adolescence. Child Development. 2001;72:583–598. doi: 10.1111/1467-8624.00298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Psychological Corporation . Wechsler Abbreviated Scale of Intelligence. Harcourt Assessment; San Antonio: 1999. [Google Scholar]
- Reid JB, Patterson GR, Snyder J. Antisocial behavior in children and adolescents. American Psychological Association; Washington: 2002. [Google Scholar]
- Rubin DB. Multiple imputation for nonresponse in surveys. Wiley; New York: 1987. [Google Scholar]
- SAS Institute Inc. SAS/ETS user’s guide, Version 9. SAS Institute Inc.; Cary, NC: 2006. [Google Scholar]
- Schafer JL. Analyses of incomplete multivariate data. Chapman and Hall; London: 1997. [Google Scholar]
- Sessa FM, Avenevoli S, Steinberg L, Morris AS. Correspondence among informants on parenting: preschool mothers, children, and observers. Journal of Family Psychology. 2001;15:53–68. doi: 10.1037//0893-3200.15.1.53. [DOI] [PubMed] [Google Scholar]
- Silk JS, Sessa FM, Morris AS, Steinberg L, Avenevoli S. Neighborhood cohesion as a buffer against hostile maternal parenting. Journal of Family Psychology. 2004;18:135–146. doi: 10.1037/0893-3200.18.1.135. [DOI] [PubMed] [Google Scholar]
- Speltz ML, McClellan J, DeKlyen M, Jones K. Preschool boys with oppositional defiant disorder: clinical presentation and diagnostic change. Journal of the American Academy of Child and Adolescent Psychology. 1999;38:838–845. doi: 10.1097/00004583-199907000-00013. [DOI] [PubMed] [Google Scholar]
- Sytsma SE, Kelley ML, Wymer JH. Development and validation of the child routines inventory. Journal of Psychopathology and Behavioral Assessment. 2001;23:241–251. [Google Scholar]
- Taylor RD. Adolescents’ perceptions of kinship support and family management practices: association with adolescent adjustment in African American families. Developmental Psychology. 1996;32:687–695. [Google Scholar]
- Taylor RD, Lopez EI. Family management practice, school achievement, and problem behavior in African American adolescents: mediating processes. Applied Developmental Psychology. 2005;26:39–49. [Google Scholar]
- Voydanoff P, Fine MA, Donnelly BW. Family structure, family organization, and quality of family life. Journal of Family and Economic Issues. 1994;15:175–200. [Google Scholar]
- White JL, Moffitt TE, Caspi A, Jeglum JB, Needles DJ, Stouthamer-Loeber M. Measuring impulsivity and examining its relationship to delinquency. Journal of Abnormal Psychology. 1994;103:192–205. doi: 10.1037//0021-843x.103.2.192. [DOI] [PubMed] [Google Scholar]
- Winstanley CA, Eagle DM, Robbins TW. Behavioral models of impulsivity in relation to ADHD: translation between clinical and preclinical studies. Clinical Psychology Review. 2006;26:379–395. doi: 10.1016/j.cpr.2006.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


