Abstract
Objective
To evaluate the effectiveness of a web-based protocol, Moderate Drinking (MD) (www.moderatedrinking.com) combined with use of the online resources of Moderation Management (MM) (www.moderation.org) as opposed to the use of the online resources of MM alone.
Method
We randomly assigned 80 problem drinkers to either the experimental or control group with follow-ups at 3, 6, and 12 months.
Results
Seventy-five participants (94%) had outcome data at one or more follow-up points and 59 (73%) were assessed at all three follow-ups. Comparing baseline measures to the average outcomes at follow-ups indicated a significant overall reduction in both groups in alcohol-related problems and consumption variables. Compared to the control group, the experimental group had better outcomes on percent days abstinent (PDA). There was an interaction between intensity of drinking at baseline and treatment in determining outcomes assessing drinking. Less heavy drinkers in the experimental group had better outcomes on log Mean BAC per drinking day compared to the control group. Heavier drinkers did not differentially benefit from the MD program on this measure. Mixed model analyses in general corroborated these outcomes.
Conclusion
The outcome data provide partial evidence for the effectiveness of the MD web application combined with MM, compared to the effectiveness of the resources available online at MM by themselves.
Keywords: computer-based intervention, Internet-based program, web-based program, problem drinkers, moderate drinking, Moderation Management
Non-dependent problem drinkers and moderate drinking protocols
Over 20 years ago the Institute of Medicine (1990) described non-dependent problem drinkers as a large but under-served group and identified the need to provide interventions for them. Since then the need for such interventions has increased. Although the prevalence of alcohol dependence is declining, the number of non-dependent problem drinkers is increasing (National Institute on Alcohol Abuse & Alcoholism (NIAAA), 2004).
Computer and Internet or web-based interventions are one way to address this under-served group of problem drinkers. Researchers have published a number of reviews of such interventions for problem drinking in the last several years. Bewick and colleagues examined studies published through mid-2006 and concluded that the evidence for web-based screening and brief interventions was inconsistent and that the methodological quality of the studies was relatively low (Bewick, Trusler, Barkham, Hill, Cahil, & Mulhern, 2008). More recently Rooke and colleagues conducted a meta-analysis of computer-based interventions and examined potential moderators (Rooke, Thorsteinsson, Karpin, Copeland, & Allsop, 2010). They reported an average effect size (d) of .26 for studies of alcohol interventions. Examining moderators they concluded that effect sizes did not vary significantly as a function of “treatment location, inclusion of entertaining elements, provision of normative feedback, availability of a discussion feature, number of treatment sessions, emphasis on relapse prevention, level of therapist involvement or follow-up period” (Rooke et al., 2010, p. 1381). They also found non-significant correlations between effect size and number of sessions, weeks of follow-up, and the methodological quality of the study. Studies that compared a computer intervention to another active intervention (as opposed to, say, a wait-list control group) found between group effect sizes close to zero, suggesting a comparability between the two interventions.
Vernon’s (2010) review found evidence that problem drinkers were interested in, and likely to use, web-based assessments and interventions, as well as evidence that program completers reduced their drinking. A review of web-based brief motivational interventions for heavy drinking college students found them to be generally as effective as other active alcohol-focused interventions (Carey, Scott-Sheldon, Elliott, Bolles, & Carey, 2009). The most recent studies have demonstrated that web-based interventions for problem drinkers are effective in helping them reduce their drinking, at least in the short term (Cunningham, Wild, Cordingley, Mierlo, & Humphreys, 2009, 2010; Hester, Delaney, Campbell, & Handmaker, 2009).
The evidence, however, comes with caveats. Little is known about what sort of drinker is most likely to benefit from a computer-based intervention, what sort of treatment protocols work best on a computer, and how computer-based interventions might best be used in combination with other approaches (e.g., mutual help groups) to achieve reductions in drinking. Methodological issues related to the investigation of web-based interventions also need to be examined, such as the contrast between the clinical and naturalistic settings in which the interventions are tested (Cunningham & Mierlo, 2009).
In this study we investigated the effectiveness of two web-based resources: a new web-application, ModerateDrinking.com (MD), and Moderation Management (MM). Because the correlation between drinking and alcohol-related problems is lower in non-dependent drinkers (Institute of Medicine, 1990), we considered reductions in alcohol-related problems to be a primary clinical outcome for these drinkers and consumption a secondary outcome. Alcohol-related problems are what motivate heavy drinkers to change and the bottom line is whether a person’s drinking has negative consequences. With respect to drinking outcomes, we examined how intensity of drinking might affect outcome. Are there differences in outcomes based on whether a person’s average baseline drinking meets NIAAA's (2004) definition of binge drinking (5 or more for men, 4 or more for women on any one occasion)?
Moderation Management (MM)
MM (www.moderation.org) is a mutual help group for drinkers interested in learning how to moderate their drinking. MM offers face-to-face and online meetings, a listserv, a forum, online drinking limit guidelines, a self-help book which can be ordered through the MM site (Rotgers, Kern, & Hoetzel, 2002), and an online calendar where users can report their drinking. MM tends to attract well educated, middle class heavy drinkers who have not sought treatment before. They have fewer symptoms of dependence and alcohol-related problems than treatment seekers (Humphreys & Klaw, 2001; Kosok, 2006).
ModerateDrinking.com (MD)
Our new web-based program, ModerateDrinking.com (www.moderatedrinking.com), is, like MM, based on principles of behavioral self-control training, but presents the material in a more structured, interactive and individualized way. It guides users to set goals, self-monitor their behavior, and get detailed feedback on their progress based on their input. MD has modules addressing motivation, identifying and managing triggers, developing alternatives, problem solving, dealing with lapses and relapses, considering abstinence, and self-monitoring one’s mood. It recommends first choosing a goal (abstinence or moderation), building motivation for change, doing a 30 (a self-imposed period of abstinence), setting drinking goals/limits, and then self-monitoring of drinking. Users are asked to enter their self-monitoring data when they log back onto the site which the program uses to generate detailed feedback about their progress. Although it recommends going through the modules in sequence, users can choose which modules might best meet their needs. More details are available in Hester et al. (2009). Readers interested in reviewing the program may contact the senior author for access.
Hypotheses
1. Both groups will reduce their alcohol-related problems and drinking relative to baseline levels at follow-ups. 2. The experimental group (MD + MM) will show a greater reduction in alcohol-related problems and drinking relative to the control group (MM only) at follow-ups.
Method
Planned study population
We planned this study as an effectiveness trial to increase its external validity. Thus we excluded dependent drinkers who were unlikely to benefit from the protocols, given prior research on moderation interventions in the U.S. (Hester, 2003; Miller et al., 1992). We also excluded drinkers with histories or current symptoms of severe co-morbid conditions as they would most likely need more intensive interventions than MD offers. We excluded current members of MM to better understand the effectiveness of these programs with problem drinkers who were encountering them for the first time.
Consistent with the membership of MM we planned to recruit a 50-50 gender split. We did not collect socioeconomic status data. Our primary recruitment tool was a display ad in the weekly TV guide section of the local newspaper that ran a banner headline asking “Are you concerned about your drinking?” Our recruitment window ran from May 2007 through February 2008.
Inclusion criteria
The inclusion criteria were: 1. Alcohol Use Disorder Identification Test (AUDIT) (Saunders et al., 1993) scores >7; 2. Drinking 10+ standard (14 grams) drinks per week in the previous 30 days; 3. Not currently abstaining; 4. Interest in moderating drinking; 5. Age 21+; and 6. A computer with Internet access at home.
Exclusion criteria
We excluded drinkers with a: 1. History of treatment for substance abuse; 2. Already a member of MM. 3. History of hospitalization for alcohol or drug dependence or detoxification; 4. Past or current diagnosis of drug abuse or dependence; 5. Evidence of past or present physical dependence (major withdrawal symptoms: delirium tremens (DTs), seizures, hallucinations); 6. Current indication of psychosis or bipolar disorder based on self-report; 7. Evidence of significant cognitive impairment from brain dysfunction (based on self-report and observation during screening interviews); 8. Evidence of health oriented contraindications to any further drinking (e.g., pregnancy, congestive heart failure). These remaining exclusion criteria were meant to assure that participants could provide the data necessary to conduct the trial: 9. English reading level below the 8th grade (assessed using the Slosson Oral Reading Test, (Slosson, 1990)); 10. Unwilling or unable to attend follow-ups; and 11. Unwilling or unable to provide one significant other (SO) for corroboration of their self-report of drinking.
Experimental design
We chose an additive design that compares the MD + MM programs in combination to MM alone. While it cannot tell us the absolute impact that MD alone would have, it can tell us how outcomes will improve above and beyond involvement in MM itself. This design reflects how we envision that most future participants will use the two resources, the MD program in tandem with MM participation. We considered having an assessment-only control group but decided against it for ethical reasons. We also considered having a 3 mo. wait-list control group but decided against it because of concerns that some or many participants in this group would go online and use the MM web site’s resources even though we had asked them to wait. This is, after all, a population of problem drinkers who are motivated enough to contact us about participating in a study to help them change their drinking.
Follow-ups were at 3, 6, and 12 months. On the basis of previous moderation studies, we anticipated that participants in the MD + MM condition would receive the majority of the benefit from using the MD web application by the 3-month follow-up. Participants were, however, able to use MD throughout the study so these follow-ups were technically post-baseline assessments.
Screening
Potential participants were screened over the phone using the Quick Screen from Project MATCH, and a questionnaire addressing inclusion criteria 2–6 and exclusion criteria 2–5, 8, 10, and 11. We invited those who passed the phone screening to schedule an appointment for a face-to-face meeting for the remaining screening items, to discuss the clinical trial in more detail, and to review and sign the Informed Consent. The in-person screening included the Michigan Alcohol Screening Test (MAST, Selzer, 1971), the AUDIT, the Brief Symptom Inventory (BSI-18) (Derogatis, 2000), the Slossen (when we had a question about the individual’s reading level), a brief medical history questionnaire, and the gathering of demographic data. This study was approved by our institutional review board.
Randomization
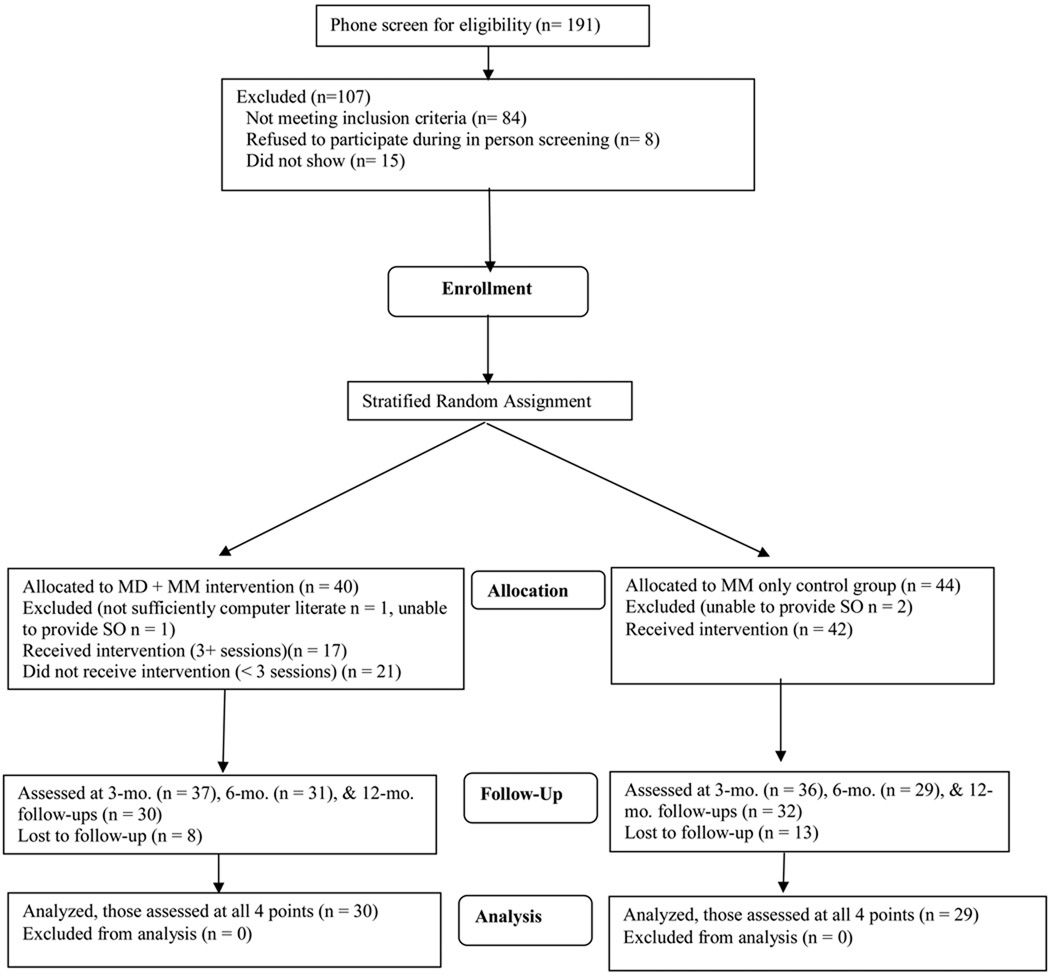
We used a stratified random assignment and classified participants into blocks based on the control factors of gender, ethnicity (White, Hispanic, or Other), and problem severity as measured by their AUDIT scores (<16 vs. 16+). Figure 1 is a flowchart of participants through the study.
Figure 1.
Flowchart of Participation through Trial
Assessment
Once enrolled, we gave participants a baseline assessment of their drinking and drinking-related issues using the Drinker’s Evaluation program, a web application we developed to collect baseline and follow-up data. The program consists of the following instruments: the AUDIT (baseline & 12 mo.); the Brief Drinker’s Profile (BDP) which measures quantity/frequency of drinking and drug use, family history, and other risk factors (baseline, 3, 6, & 12 mo.) (Miller & Marlatt, 1987a); the Drinker’s Inventory of Consequences (DrInC), a 50-item questionnaire that measures both lifetime and recent (previous 3 months) consequences (e.g., inter-and intrapersonal, social responsibility, physical) from drinking (baseline, 3, 6, & 12 mo.) (Miller et al., 1995); the Severity of Alcohol Dependence (community sample) (SADQ-C) measures symptoms of alcohol dependence (baseline, 6, & 12 mo.) (Stockwell et al., 1994); the Stages of Change and Readiness and Treatment Eagerness Scale (SOCRATES) measures motivation for change (baseline, 3, 6, & 12 mo.) (Miller & Tonigan, 1996); demographic data; and questions from the Form 90 (Miller, 1996) that ask about additional help (outside of the study) they have received during follow-up. We collected SO data by phone using the Collateral Interview Form (CIF) (Miller & Marlatt, 1987b). The CIF is a parallel instrument to the BDP for use with collaterals at baseline and follow-up.
Significant Others (SOs)
We asked participants for the name of a SO we could interview to corroborate the participant's self-report. We then contacted the SO to confirm his or her willingness to be interviewed.
Introduction of the Intervention
When participants finished the baseline assessment, we informed them of their treatment condition and then presented the appropriate intervention for their group. We designed these procedures to strike a balance between ensuring sufficient contact with the intervention materials and allowing a natural response similar to one that might occur through self-directed contact with the sites. We gave all participants a brief, 3-minute tour of the MM site to acquaint them with its resources. We also showed and enrolled them in the MM listserv. In order to ensure that they received a minimum dose of exposure to the treatment, we asked participants to read and/or post to the listserv at least twice a week for at least the first 12 weeks of the study. We then introduced experimental subjects to the MD program in a similar fashion as we had with the MM site. To minimize positive expectancies we did not encourage them to differentially attend to either site, although they often commented on the personalized nature of the MD program compared to more generic structure of the MM site.
We did not ask participants to keep track of their MM site activity on a daily basis, as we were concerned that this might weaken the external validity of the trial’s results. Instead we sent them an automated email each month that asked how much they had accessed the MM website and how much they felt they had benefitted from it.
Finally, we asked participants if they had any further questions or concerns. Participant response to this closing, open-ended part of the protocol varied widely. Some had no questions, others had only technical questions about how to operate the program, and some wanted to discuss their drinking with the research assistant (RA). This initial discussion at the outset of the study was problematic. Any discussion about their concerns with their drinking could have had a treatment effect. On the other hand, ignoring participants’ concerns might have reduced their engagement with the study. We decided on a middle path: the RA addressed, as briefly as possible, any concerns the participant had about their drinking, but did not solicit any further discussion, and always respectfully directed them to the study’s resources.
At the end, we set up a follow-up appointment, reminded participants that we would call their SOs in the next day or two, and sent them emails with links to the site(s) along with offers of assistance should they encounter any difficulties accessing them. We gave them a reminder call two or three days before their follow-up and resolved any scheduling conflicts. The follow-up appointments were typically 20 to 30 minutes long, although some participants wanted to prolong this and discuss their progress. Once again, the RA acknowledged their concerns and redirected them as described above. Participants’ desire for therapeutic contact from RAs, while problematic for any clinical trial, is fraught with hazards for the validity of the test of computer-based interventions. At the 12-month exit interview, however, we asked them to discuss their experiences with the programs and we asked for feedback about what, if anything, could have been more helpful.
Power analysis & sample size
See Hester et al. (2009) for details.
Dependent variables
We used four measures to assess outcomes: the DrInC Recent Total score which reflected alcohol-related problems, and three primary alcohol consumption measures (Percent Days Abstinent (PDA), log Mean Drinks per Drinking Day, and log Mean BAC per Drinking Day).
Data analysis plan
The primary analytic strategy was to conduct repeated measures analyses of variance for a design including two between-subject factors, each with two levels (Treatment, MD or MM; Binge drinker, Yes or No), and one within-subject factor with four levels (Time, baseline and 3, 6, or 12 months post). Because we anticipated that the major overall as well as differential impact of the treatments would occur in the first three months, an a priori contrast assessing the difference between the pre-measure and the average of the post measures was of most interest.
We also conducted a number of secondary analyses, including various analyses pertinent to comparisons between participants having complete data and those missing one or more follow-ups. There were no significant differences at baseline between these two groups on any primary dependent variables. Imputation of missing data using the average of the available follow-ups for the 16 participants having partial follow-up data available was carried out, and resulted in essentially the same pattern of significant results on tests of hypotheses as analyses conducted on only those participants having complete data. Thus, primary tests reported are those including only those participants having complete data. However, we also conducted mixed model analyses including participants having incomplete data. We did not exclude any participants from analyses on the basis of their level of use of the resources offered them.
Prior to conducting the primary statistical tests, we examined the distributions of variables to check for conformity with statistical assumptions. Several of the drinking measures were positively skewed. In particular, two measures of quantity of drinking, Mean Drinks per Drinking Day and Mean Peak BAC for Drinking Days, had skewness at baseline of 2.1 and 2.8, respectively. Thus, we log transformed such measures before analysis. This resulted in reducing the skewness for the log transformation of the baseline variables, such as log Mean Drinks per Drinking Day and log Mean Peak BAC for Drinking Days, to less than 1.0 in absolute value. These two variables were correlated, r =.63, but correlations among other variables were all less than .3 in absolute value.
Effect sizes for within-subject effects were computed by dividing differences from baseline to average post-baseline means by a pooled standard deviation reflecting between-subject variability averaged over the four assessments. Maxwell and Delaney (2004, pp. 315, 549) recommend this conservative procedure to avoid overestimation of effect sizes that results when variability in change but not typical level on the dependent variable is used in the denominator. We computed confidence intervals (CIs) for within-subject effect sizes using methods suggested by Bird (2002; cf. Algina & Keselman, 2003). Effect sizes for between-subject effects were computed by dividing differences between the two treatment conditions by a pooled within-group standard deviation, with CIs being estimated using methods suggested by Hedges and Olkin (1985).
Results
Study participant characteristics
Data were available on 80 participants at baseline. These included approximately equal numbers of females (n = 45, 56% of sample) and males (n = 35, 44%). Of the 80, 63 (79%) were non-Hispanic Caucasians, 15 (19%) Hispanics, and 2 (2%) other. Their mean age was 50 and the mean years of education was 15. The two treatment groups did not differ significantly on demographic variables or any of the continuous measures assessed at baseline as shown in Table 1.
Table 1.
Means (and Standard Deviations) on Continuous Measures at Baseline.
| Measure | Group | |
|---|---|---|
| MD + MM | MM only | |
| Age | 48.7 (10.1) | 52.1 (13.2) |
| Education in Years | 15.7 (2.9) | 15.1 (3.6) |
| MAST score | 14.1 (6.8) | 13.2 (8.0) |
| Drinks (SECs)/Week | 33.0 (19.2) | 35.4 (26.2) |
| Percent Days Abstinent (PDA) | 16.3 (21.0) | 16.2 (23.8) |
| Mean Drinks per Drinking Day | 5.5 (2.5) | 6.1 (4.0) |
| Mean Peak BAC per Drinking Day | 111.2 (73.4) | 119.5 (87.4) |
| Hours BAC > 80 mg% | 21.9 (30.4) | 26.1 (36.7) |
| DrInC Recent Total score | 24.3 (11.5) | 21.3 (10.6) |
| AUDIT score | 17.7 (5.6) | 18.3 (5.9) |
Results of primary analyses
To test our primary hypotheses, we conducted repeated measures analyses of variance using multivariate tests with the 59 participants having data at all four assessments.
Test of hypothesis 1: Improvement in both groups over time
The overall reduction in alcohol-related problems averaging across both groups was highly significant, F(3,53) = 14.22, p < .001. The mean DrInC scores were 22.7, 17.1, 16.6, and 13.0 for the four assessments. While the change from baseline to the average of the follow-ups was highly significant (p < .001; d =.58; 95% CI: .35, .81), there was also evidence of significant additional improvement between 6 months and 12 months (p = .008; d = .29; 95% CI: .09, .50). The reduction in DrInC scores is clinically significant. Using DrInC norms from our online Drinker’s Check-up (Hester & Squires, 2008), study participants at baseline were at the 54th percentile for women and 65th percentile for men. At 12 months, they were at the 29th and 38th percentiles, respectively.
The multivariate test of the overall reduction in alcohol consumption averaging across both groups was highly significant, F(9, 47) = 8.14, p < .001. Separate analyses of the three drinking measures individually showed highly significant effects on all three measures: PDA, F(3,53) = 9.14, p < .001; log Mean Drinks per Drinking Day, F(3, 53) = 24.77, p < .001; and log Mean BAC per Drinking Day, F(3, 53) = 14.41, p < .001. In each case, the locus of the change over time was from the baseline to the average of the three follow-ups, p < .001, with there being no significant differences among the 3 follow-up periods, p > .2. The improvement from baseline to the average of the 3 follow-ups for PDA was from 14.8% to 33.0%. On the scale of the original variables, the reduction in Mean Drinks per Drinking Day was from 5.35 at baseline to 3.28 post-baseline, and the reduction in Mean BAC per Drinking Day was from 102mg% at baseline to 58mg% post-baseline. Effect sizes were: d = .57 (95% CI: .35, .79) for PDA, d = .93 (95% CI: .69, 1.17) for log Mean Drinks per Drinking Day , and d = .74 (95% CI: .50, .98) for log Mean BAC per Drinking Day.
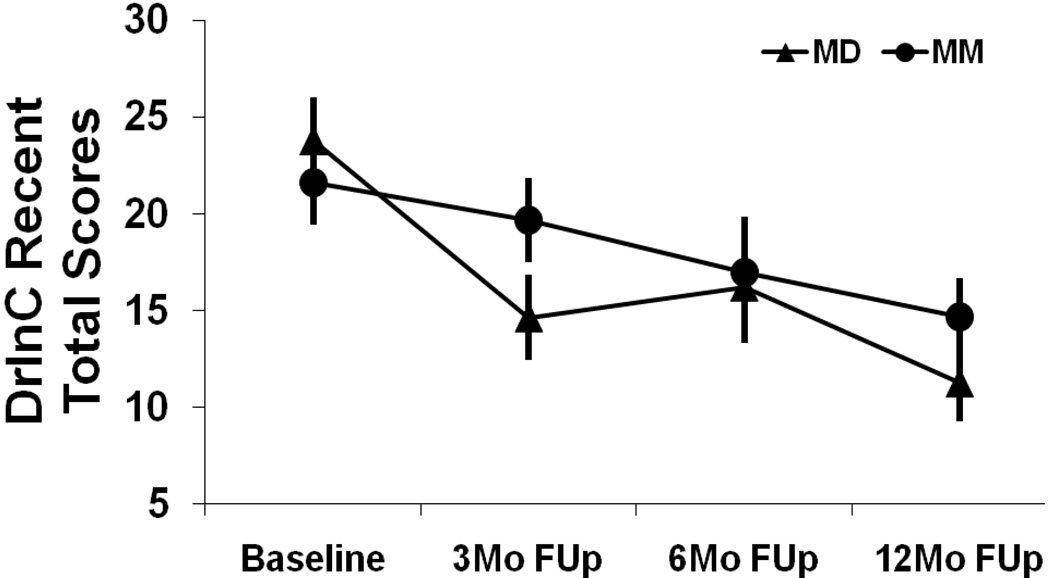
Tests of hypothesis 2: Differential effects of two treatment conditions
For the variable assessing alcohol-related problems, the Treatment×Time interaction was significant, F(3, 53) = 3.23, p = .030. The improvement from baseline to the average at follow-ups was twice as large in the experimental group (9.75) as in the control group (4.51), but the test of this pre-planned interaction contrast did not reach significance, F(1, 55) = 3.23, p = .078, d = .42 (95% CI: −.10,.93). Regarding the primary locus of the two-way interaction, there was a significant difference between the two groups, favoring MD, in amount of improvement from baseline to 3 months, F(1,55) = 6.84, p = 011, but interaction contrasts involving the later follow-ups were non-significant. The reduction in problems shown in Figure 2 for the MD + MM group is clinically significant. Using Hester & Squires (2008) DrInC norms, the females were at the 57th percentile and the males were at the 65th percentile at baseline. At 12 months they had dropped down to the 24th percentile and 30th percentile for women and men, respectively.
Figure 2.
Alcohol-Related Problems (DrInC Recent Total Scores) by Treatment Condition and Time of Assessment.
In combined multivariate tests of the three primary alcohol consumption variables, the test of the Time×Treatment interaction did not reach significance, F(9, 47) = 1.80, p = .093. However, this must be interpreted in light of the significant Time×Treatment×Binge Drinking Status interaction, F(9, 47) = 2.49, p = .021. These results will be presented by first noting the general form of the Time×Treatment interaction and then detailing results for each of the three consumption variables in turn.
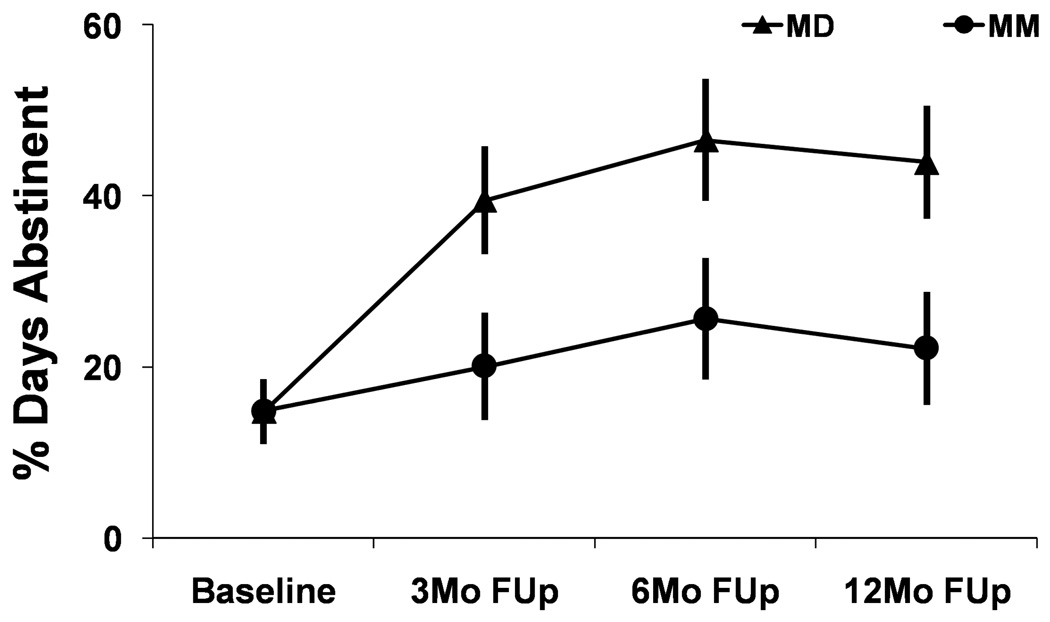
In terms of the overall two-way interaction, the pattern for all three alcohol consumption variables was for there to be a trend toward greater overall improvement from baseline to the follow-ups in the experimental group than the control group. For PDA, this two-way Time×Treatment interaction was significant, F(3, 53) = 3.26, p = .029. As seen in Figure 3 which presents the plot of means as a function of Treatment condition and Time, the form of the trends across the post assessments was virtually identical in the two treatment groups (p > .8) but the change from baseline to the average of the three follow-ups was significantly greater in the MD + MM condition (28.6) than in the MM only condition (7.8), F(1, 55) = 9.22, p = .004, yielding a between-group effect size of d = .65 (95% CI: .12, 1.16). From a clinical perspective, PDA nearly tripled in the MD + MM group from 14.7% to 43.9% (from 1 to 3 days per week) while PDA in the MM only group went up from 14.8% to 22.6% (from 1 to 1.5 days per week).
Figure 3.
Percent Days Abstinent by Treatment Condition and Time of Assessment.
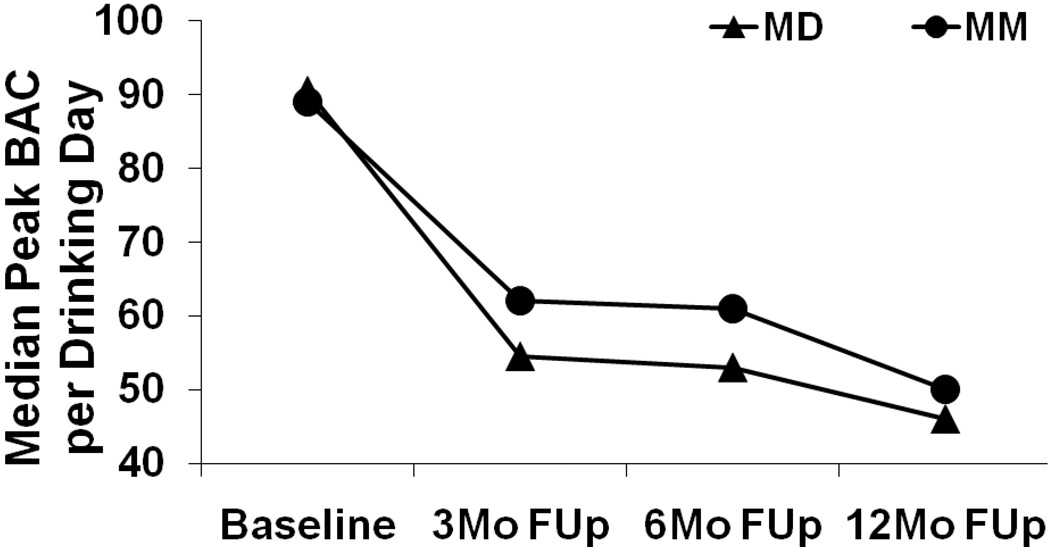
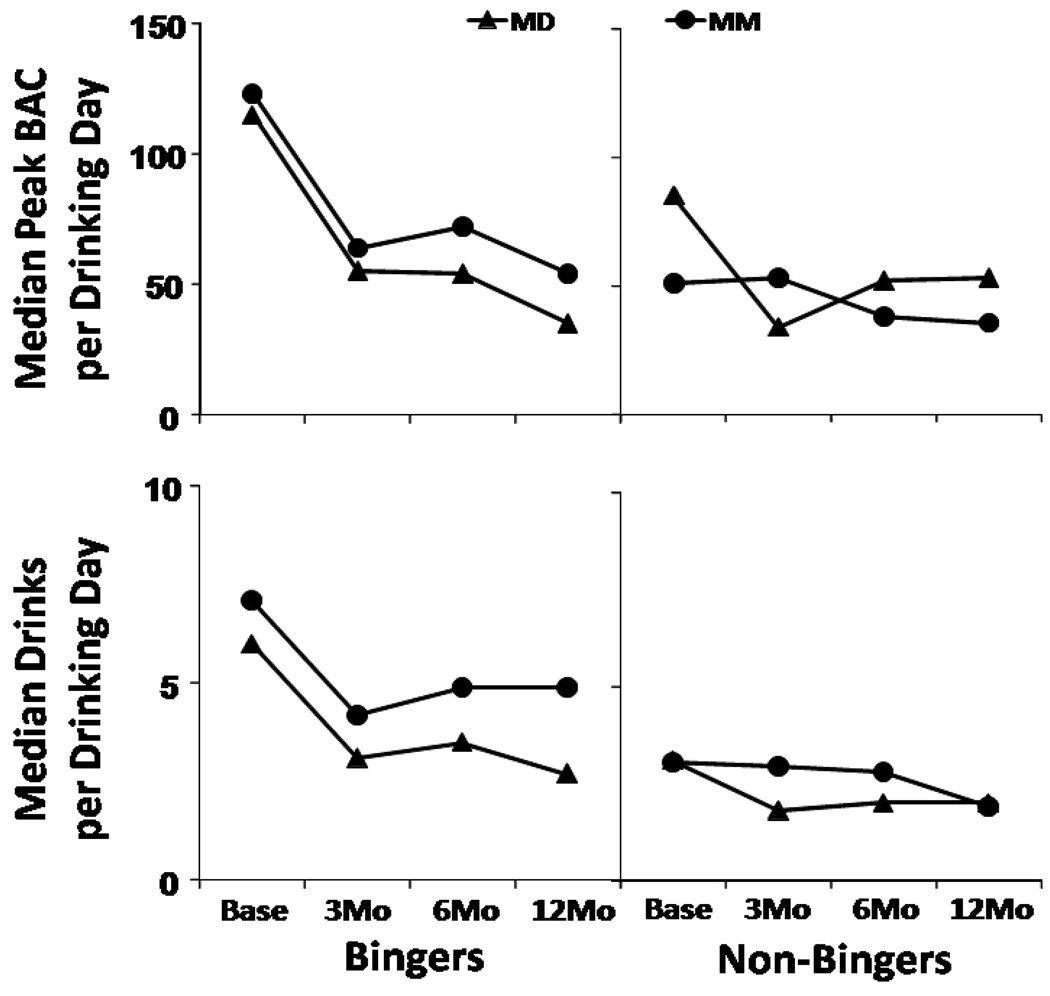
For the other two alcohol consumption variables, the Time×Treatment×Binge Drinking Status three-way interaction was significant. For log Mean BAC per Drinking Day, the test of the three-way interaction yielded F(3, 53) = 5.00, p = .004. The form of the two-way interaction is suggested by Figure 4, which shows the median on the original variable as a summary for each cell because, like the log, the median is relatively unaffected by skewness. As with PDA, the overall trend was for the improvement from baseline to the follow-ups to be greater in the MD + MM condition than in the MM only condition. The omnibus test of Time×Treatment did not reach significance F(3, 53) = 2.66, p = .058. but the test of the a priori interaction contrast was significant, F(1,55) = 5.91, p = .018, d = .62 (95% CI: .09, 1.14). The MD + MM group reduced their median peak BAC by nearly half (49%) to 46mg% at 12 months.
Figure 4.
Median Peak BAC per Drinking Day by Treatment Condition and Time of Assessment.
The form of the three-way interaction for two measures of intensity of drinking on drinking days is shown in Figure 5 which plots the median across individuals of the participant's Mean BAC per Drinking Day and Mean Drinks per Drinking Day as a function of Time and Treatment separately for Binge drinkers and Non-Binge drinkers. For log Mean BAC per Drinking Day, the test of the difference across groups in improvement from baseline to the average of the follow-ups was not significant for Binge drinkers, F(1, 56) = 0.30, p = .585 (although the improvement from baseline to post was highly significant for Binge drinkers in both treatments). On the other hand, for Non-Binge drinkers, the difference between the two treatment conditions was more pronounced, particularly in the change from baseline to 3 months, as shown in the upper right panel of Figure 5. For the Non-Binge drinkers, the simple effects test of the difference in improvement from Baseline to the average of the Follow-ups was significantly different across groups, F(1, 56) = 7.45, p = .008, which corresponds to a large between-group effect size d = 1.00. The median peak BAC per drinking day in the MD + MM group went from 85mg% to an average of 46mg%, whereas the MM group’s improvement was more modest from 51mg% pre to an average of 42 mg% post. The MD + MM group of non-bingers, admittedly, had more room for improvement on this variable.
Figure 5.
Three-way Interactions for Median Peak BAC per Drinking Day (upper panels) and Median Drinks per Drinking Day (lower panels) by Treatment Condition, Time of Assessment, and Binge-Drinking Status.
For the final consumption measure, log Mean Drinks per Drinking Day, the overall Time×Treatment interaction did not approach significance F(3,53) = 1.19, p =.324, nor did the test of the a priori contrast assessing differential improvement, F(1,55) = 1.91, p = .173, d = .33 (95%CI: −.19, .84); however, the Time×Treatment×Binge Drinking Status was again significant F(3, 53) = 2.99, p = .039. The form of the simple two-way interactions was similar to those seen with log Mean BAC per Drinking Day. The Time×Treatment interaction was less pronounced for Binge drinkers than for Non-Binge drinkers. For Binge drinkers, the Time×Treatment interaction on Mean Drinks per Drinking Day is shown in the bottom left panel of Figure 5. The overall improvement from baseline to the average of the follow-ups was equal across treatment groups for Bingers, F = 0.
For Non-Bingers on the other hand there was again a trend toward more immediate improvement in the experimental group than the control group as shown in bottom right panel of Figure 5. However, the test of the difference across groups in change from baseline to the average of the follow-ups did not reach significance for Non-Bingers, F(1,56) = 3.48, p = .067, d = .68 (95% CI: .15, 1.19).
Additional Analyses
Analyses of participants with partial follow-up data
We also conducted mixed model analyses to incorporate those participants (n = 16) having only partial follow-up data. In general, these tests corroborated the results for the drinking variables but not for the measure of alcohol-related problems. The mixed model test of the Treatment×Time interaction for PDA was significant (p = .042), as was the mixed model test of the Treatment×Binger×Time three-way interaction for log Mean BAC per Drinking Day (p = .021). However, the mixed model test of the three-way interaction did not reach significance for log Mean Drinks per Drinking Day (p = .069). The most striking difference between the mixed model and MANOVA approaches was with regard to the DrInC where the mixed model test of the Treatment×Time interaction did not approach significance (p =. 383). We conducted post hoc analyses of the data on the DrInC comparing the 14 participants with partial follow-up data who had a 3-month assessment across the two treatment conditions and also with the 59 participants with complete data. Means on the four primary dependent variables are shown for the participants with partial follow-up data in Table 2. Although not surprising given the small numbers of participants, tests of the difference in improvement across groups were not significant for any variable. Differences, which favored the MM condition, were small for the three drinking variables but substantial for the DrInC. Perhaps of most interest was the low level of alcohol-related problems at 3 months for this subset of participants. At 3 months, 6 of the 14 (42%) with partial data (2 MD + MM and 4 MM only participants) reported having no alcohol-related consequences (a DrInC score of 0), whereas only two of the 59 with complete data did so, a highly significant difference (Fisher’s exact p < .001).
Table 2.
Means (and Standard Deviations) on Dependent Measures at Baseline and Three Months for Participants with Partial Follow-up Data.
| MD (n = 7) | MM (n = 7) | |||
|---|---|---|---|---|
| Baseline | 3 Months | Baseline | 3 Months | |
| Percent Days Abstinent | 23.66 (23.52) | 20.27 (32.05) | 5.91 (10.86) | 12.17 (22.02) |
| Log Mean Drinks per Drinking Day | .853 (.081) | .633 (.442) | .736 (.129) | .312 (.413) |
| Log Mean BAC per Drinking Day | 1.91 (.328) | 1.39 (.980) | 2.04 (.195) | .87 (1.11) |
| DrInC Recent Total | 24.86 (7.90) | 18.57 (14.42) | 22.57 (11.69) | 2.71 (4.72) |
Note: The assessment interval for these variables is one month prior to the assessment.
Significant others
Substantial numbers of significant others (SOs) were assessed at each time period: 76 at baseline, 59 at 3 months, 51 at 6 months, and 55 at 12 months. Correlations between SOs' and clients' reports tended to increase over time. Averaging the correlations for four measures of drinking at each assessment time revealed a mean correlation between SO and client report at baseline of .41; at 3 months, .47; at 6 months, .48; and at 12 months, .77.
Analyses of the SOs' reports of the participants' drinking generally corroborated the analyses of the participants' self-reports regarding treatment differences. For example, tests of improvement over time were consistently highly significant and tests of a contrast comparing baseline with the average of the follow-ups indicated significantly greater improvement in the experimental group than in the control group for PDA, F(1, 42) = 10.53, p = .002, and for log Mean Drinks per Drinking Day, F(1, 42) = 5.36, p = .026.
Potential moderators
We conducted exploratory analyses to assess whether the differences between the two groups might be moderated by participant age, or social support. None of the tests of the relevant interactions were significant for any of our primary dependent variables.
Discussion
The outcome data clearly support hypothesis 1. Both groups at follow-up reduced their alcohol-related problems and drinking relative to baseline levels. The magnitude of the reductions in drinking corresponded to medium-to-large effect sizes (average within-subject d = .70). This support, however, is tempered by the limitations discussed below.
Support for hypothesis 2 was mixed; nonetheless, the average between-group effect size across the four dependent variables was d = .51, approximately twice that (.26) reported by Rooke et al. (2010) for computer-based alcohol interventions. Compared to the control group, the experimental group experienced a greater increase in Percent Days Abstinent at follow-up (a medium-to-large between-group effect d = .65). There was also some evidence of a greater reduction in levels of drinking and in alcohol-related problems at follow-up in the experimental group, but only with a subset of participants. For two measures of intensity of drinking, the experimental group had better outcomes for those whose average baseline drinking levels did not meet criteria for binge drinking (average between-group effect for non-bingers was large d = .84).
For the measure of alcohol problems, a greater beneficial effect of the MD program was suggested for the three fourths of participants who had complete follow-up data (d = .42, a small to medium effect, significant only at 3 months), but was not seen at all for the other one fourth of participants, 40% of whom dropped out after reporting at 3 months that they no longer had any alcohol-related problems. The reductions in alcohol-related problems in the experimental group are clinically significant. Using the DrInC norms from the Drinker's Check-up (Hester & Squires, 2008), the experimental group went from the 61st percentile at baseline to the 27th percentile at 12 months. Given that alcohol-related problems are the major criteria for the diagnosis of alcohol abuse (APA, 1994), the magnitude of reduction of alcohol-related problems is noteworthy. Functional impairment and distress have been at the core of the conceptualization of alcohol use disorders since their inception. Huss (1849) first described alcoholism as a syndrome characterized by alcohol-related problems. In addition, the DSM-IV diagnostic system recognizes adverse consequences of drinking are conceptually independent from symptoms of alcohol dependence and pathological drinking (Miller et al., 1995, p. 2). Furthermore the severity of alcohol-related problems is not well predicted by consumption or dependence measures (Miller et al., 1995). Thus the primary goal of moderation protocols is the reduction of alcohol-related problems.
While the relatively greater increase in abstinence in the experimental group is encouraging, the picture is more mixed on the consumption variables. Those whose drinking, on average, did not meet NIAAA's definition of binge drinking had somewhat better outcomes in the experimental group, which had access to more resources to learn moderate drinking skills. The outcomes with respect to the binge drinkers is consistent with other moderate drinking research in the U.S.: more significant problem drinkers benefit less from moderation protocols than do less severe problem drinkers (see Hester, 2003 for a review). Examination of the baseline characteristics of these two groups indicated that the heavier drinking sub-group had higher mean MAST scores (14.8 vs. 11.2, p = .046), and higher scores on the SADQ which measures dependence (4.9 vs. 3.1, p = .037) compared to the non-binge drinkers.
We did not see a clear dose-response relationship between the use of the MD program and outcomes. Some participants who logged in only once or twice had positive outcomes but others did not benefit from their minimal use of the program. Others used the program frequently and had positive outcomes but not all frequent users of the program were successful in reducing their drinking. The varied patterns of use of the MD protocol are to be expected of any self-directed intervention, especially one designed for a clinical issue that may present in a variety of ways. Unfortunately, this makes it difficult to identify specific mechanisms of change in the program.
External validity
The results of this study have external validity for three reasons. First, the study sample was similar to those who are attracted to MM (Kosok, 2006). The study sample was diverse, including a large proportion of women (56%). The study participants were representative of at-risk drinkers in that they reported medical conditions and psychological symptoms frequently observed among problem drinking populations. Second, the web application used in this study will be the same which will be available to future users of the program. Third, a computer-based intervention, by its nature, interacts with users in the same way over time; hence there is no "drift" from the protocol.
Limitations
Our study has a number of limitations. First, we excluded drinkers with more significant histories of alcohol and/or drug problems. Consequently we cannot generalize these findings to dependent drinkers or to those with concurrent diagnoses of drug abuse or dependence. Second, while we chose to not have an assessment-only control group because of ethical concerns, this decision precludes us from a clear test of the effectiveness of MM alone. Third, future users of the MD program may not have the same level of motivation or commitment that is required of participants entering and following through with a clinical trial. Fourth, study participants in both groups may have experienced assessment reactivity, and positive expectancies conceivably may have been induced by the contact with the experimenters. Fifth, participants were, on average not only less alcohol dependent, but also somewhat older and better educated than one might expect from a typical sample of problem drinkers. They were also all computer literate. Still, this is the population that has been drawn to MM in the past (Humphreys & Klaw, 2001; Kosok, 2006), and the population we expect to achieve the most benefit from the MD program in the future. Another limitation is that the data are based on self-report. However, analyses of the collateral data from SOs were correlated and consistent with the findings of overall pre-post changes, and between group differences over time. Another limitation is that we avoided monitoring the use of MM resources to minimize the assessment burden, potential assessment reactivity, and to avoid altering what would otherwise be a typical pattern of use. This makes it difficult to know precisely which participants in the experimental group benefitted more from MM, and which from MD or some combination of the two.
Future Research
Our results suggest several possible avenues for future research with regards to moderation and web-based interventions for problem drinkers. The interactions between intensity of drinking at baseline and outcomes means that we need to more clearly understand which drinkers can benefit solely from web-based interventions and which might need additional assistance. For example, heavier drinkers may benefit from the use of additional resources such as face-to-face therapy. They may also benefit from more encouragement to focus on increasing non-drinking days (PDA) and more consideration of a goal of abstinence. A number of participants sought additional assistance during the study but their numbers were too small to detect any patterns.
Although we did not see a dose response relationship in the MD + MM condition, our anecdotal data suggest that drinkers may benefit from more frequent use of the MD program. In the 12-month exit interviews some participants expressed a desire for a feature that would have prompted them to use the program more. Many others, when asked about such a feature, thought it would have helped them stay engaged with the program and facilitated their process of change. They asked whether such a system might also suggest what components of the program would be most beneficial to them. In response to this we have added an idiographic email reminder system to the program. We recommend incorporating such a feature in future web-based interventions and evaluating its impact.
Conclusion
The outcomes of our study are consistent with the body of treatment outcome research in moderation training protocols. Non-dependent problem drinkers can learn how to reduce their consumption and alcohol-related problems. There are a number of ways to accomplish these goals: in-person therapies, bibliotherapies, software programs, and now a web-based program. While we still have much to learn about how to increase the effectiveness of web-based programs, future research should also investigate how evidence-based web programs can be widely implemented.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ccp
This publication was supported by grant R44AA014305 from the National Institute of Alcohol Abuse and Alcoholism (NIAAA). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIAAA.
References
- Algina J, Keselman HJ. Approximate confidence intervals for effect sizes. Educational and Psychological Measurement. 2003;63:537–553. [Google Scholar]
- Bewick BM, Trusler K, Barkham M, Hill AJ, Cahill J, Mulhern B. The effectiveness of web-based interventions designed to decrease alcohol consumption—A systematic review. Preventive Medicine. 2008;47:17–26. doi: 10.1016/j.ypmed.2008.01.005. [DOI] [PubMed] [Google Scholar]
- Bird KD. Confidence intervals for effect sizes in analysis of variance. Educational and Psychological Measurement. 2002;62:197–226. [Google Scholar]
- Carey KB, Scott-Sheldon LAJ, Elliott JC, Bolles JR, Carey MP. Computer-delivered interventions to reduce college student drinking: a meta-analysis. Addiction. 2009;104:1807–1819. doi: 10.1111/j.1360-0443.2009.02691.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham JA, Wild TC, Cordingley J, Van Mierlo T, Humphreys K. A randomized controlled trial of an internet-based intervention for alcohol abusers. Addiction. 2009;104:2023–2032. doi: 10.1111/j.1360-0443.2009.02726.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham JA, Wild TC, Cordingley J, Van Mierlo T, Humphreys K. Twelve month follow-up results of a randomized controlled trial of a brief personalized feedback intervention for problem drinkers. Alcohol & Alcoholism. 2010;45(3):258–262. doi: 10.1093/alcalc/agq009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham JA, van Mierlo T. Methodological issues in the evaluation of internet-based interventions for problem drinking. Drug and Alcohol Review. 2009;28:12–17. doi: 10.1111/j.1465-3362.2008.00001.x. [DOI] [PubMed] [Google Scholar]
- Cunningham JA, Breslin FC. Only one in three people with alcohol abuse or dependence ever seek treatment. Addictive Behaviors. 2004;29:221–223. doi: 10.1016/s0306-4603(03)00077-7. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. BSI-18: Administration, scoring and procedures manual. Minneapolis, MN: National Computer Systems, Inc; 2000. [Google Scholar]
- Hedges LV, Olkin I. Statistical methods for meta-analysis. San Diego: Academic Press; 1985. [Google Scholar]
- Hester RK. Handbook of alcoholism treatment approaches: Effective alternatives. third ed. Needham Heights, MA: Allyn & Bacon; 2003. Self-control training; pp. 152–164. [Google Scholar]
- Hester RK, Delaney HD, Campbell W, Handmaker N. A web application for moderation training: Initial results of a randomized clinical trial. Journal of Substance Abuse Treatment. 2009;37(3):266–276. doi: 10.1016/j.jsat.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hester RK, Squires DD. Web-based norms for the Drinker Inventory of Consequences from the Drinker’s Check-up. Journal of Substance Abuse Treatment. 2008;35:322–327. doi: 10.1016/j.jsat.2007.10.005. [DOI] [PubMed] [Google Scholar]
- Humphries K, Klaw E. Can targeting non-dependant problem drinkers and providing internet-based services expand access to Assistance for alcohol problems? A study of the Moderation Management self-help/mutual aid organization. Journal of Studies on Alcohol. 2001;62:528–532. doi: 10.15288/jsa.2001.62.528. [DOI] [PubMed] [Google Scholar]
- Huss M. Alcoholismus chronicus. Chronisk alkoholisjukdom: Ett bidrag till dyskrasiarnas kaandom. [Chronic alcoholism. Chronic alcohol sickness: A contribution to diagnosis.] Stockholm, Sweden: Bonnier/Norstedt; 1849. [Google Scholar]
- Institute of Medicine. Broadening the base of treatment for alcohol problems. Washington, D.C.: National Academy Press; 1990. [PubMed] [Google Scholar]
- Kosok A. The Moderation Management programme in 2004: What type of drinker seeks controlled drinking? The International Journal of Drug Policy. 2006;17:295–303. [Google Scholar]
- Maxwell SE, Delaney HD. Designing experiments and analyzing data: A comparison perspective. 2nd ed. Mahwah, NJ: Lawrence Erlbaum Associates; 2004. [Google Scholar]
- Miller WR. Form 90. Project MATCH Monograph Series 5. NIHPubNo. 96-4004. Bethesda, MD: National Institutes of Health; 1996. [Google Scholar]
- Miller WR, Leckman AL, Delaney HD, Tinkcom M. Long-term follow-up of behavioral self-control training. Journal of Studies on Alcohol. 1992;53:249–261. doi: 10.15288/jsa.1992.53.249. [DOI] [PubMed] [Google Scholar]
- Miller WR, Marlatt GA. Manual supplement for Brief Drinker Profile, Follow-up Drinker Profile, and Collateral Interview Form. 1987a, b Retrieved from the Center on Alcoholism, Substance Abuse and Addictions assessments instruments page at http://casaa.unm.edu/inst.html. [Google Scholar]
- Miller WR, Tonigan S. Assessing drinkers’ motivation for change: The stages of change readiness and treatment eagerness scale (SOCRATES) Psychology of Addictive Behaviors. 1996;10(2):81–89. [Google Scholar]
- Miller WR, Tonigan S, Longabaugh R. The drinker inventory of consequences (DrInC). Project MATCH Monograph Series 4. NIHPubNo. 95-3911. Bethesda, MD: National Institutes of Health; 1995. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Alcohol abuse increases, dependence declines across decade. 2004 Retrieved June 16, 2004 from http://www.niaaa.nih.gov/press/2004/NESARCNews.htm.
- National Institute on Alcohol Abuse and Alcoholism. Binge drinking defined. 2004 Retrieved April 7, 2010 from http://pubs.niaaa.nih.gov/publications/Newsletter/winter2004/Newsletter_Number3.pdf.
- Rooke S, Thorsteinsson E, Karpin A, Copeland J, Allsop J. Computer-delivered interventions for alcohol and tobacco use: A meta-analysis. Addiction. 2010;105(8):1381–1390. doi: 10.1111/j.1360-0443.2010.02975.x. [DOI] [PubMed] [Google Scholar]
- Rotgers F, Kern M, Hoeltzel R. Responsible drinking: The path to moderation. Berkeley, CA: New Harbinger; 2002. [Google Scholar]
- SAMSHA. Screening, brief intervention, and referral to treatment. 2007 Retrieved February 9, 2009 from http://www.sbirt.samhsa.gov/about.htm.
- Saunders JB, Aaasland OB, Babor TF, De La Fuente JR, Grant M. Development of the Alcohol User Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption I. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Selzer ML. The Michigan Alcoholism Screening Test: The quest for a new diagnostic instrument. American Journal of Psychiatry. 1971;127:1653–1658. doi: 10.1176/ajp.127.12.1653. [DOI] [PubMed] [Google Scholar]
- Slosson RL. Slosson oral reading test Revised. Slosson Educational Publications, Inc; 1990. [Google Scholar]
- Stockwell T, Sitharthan T, McGrath D, Lang E. The measurement of alcohol dependence and impaired control in community samples. Addiction. 1994;89:167–174. doi: 10.1111/j.1360-0443.1994.tb00875.x. [DOI] [PubMed] [Google Scholar]
- Vernon M. A review of computer-based alcohol problem services designed for the general public. Journal of Substance Abuse Treatment. 2010;38:203–211. doi: 10.1016/j.jsat.2009.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]