Abstract
Millions of low-income people of diverse ethnicities inhabit stressful old urban industrial neighborhoods. Yet we know little about the health impacts of built-environment stressors and risk perceptions in such settings; we lack even basic health profiles. Difficult access is one reason (it took us 30 months to survey 80 households); the lack of multifaceted survey tools is another. We designed and implemented a pilot vulnerability assessment tool in Worcester, Massachusetts. We answer: (1) How can we assess vulnerability to multiple stressors? (2) What is the nature of complex vulnerability—including risk perceptions and health profiles? (3) How can findings be used by our wider community, and what lessons did we learn? (4) What implications arise for science and policy? We sought a holistic picture of neighborhood life. A reasonably representative sample of 80 respondents captured data for 254 people about: demographics, community concerns and resources, time-activity patterns, health information, risk/stress perceptions, and resources/capacities for coping. Our key findings derive partly from the survey data and partly from our experience in obtaining those data. Data strongly suggest complex vulnerability dominated by psychosocial stress. Unexpected significant gender and ethnic disease disparities emerged: notably, females have twice the disease burden of males, and white females twice the burden of females of color (p < 0.01). Self-reported depression differentiated by gender and age is illustrative. Community based participatory research (CBPR) approaches require active engagement with marginalized populations, including representatives as funded partners. Complex vulnerability necessitates holistic, participatory approaches to improve scientific understanding and societal responses.
Keywords: Built environment, CBPR, disease burden, health disparities, marginalization, risk perception, vulnerability
1. BACKGROUND AND SIGNIFICANCE
In 2007, the world’s population reached a milestone with major implications for public health and urban development: for the first time in history, more people lived in urban environments than rural ones.(1) In degraded urban-industrial environments people are chronically exposed to multiple stressors that impact mental and physical health. These include: chemical and biological agents indoors and outdoors (the traditional focus of environmental health science and policy); physical stressors such as noise, blight, waste dumps, and trash in the streets; social stressors such as crime and over-crowding; economic stressors such as income poverty and employment insecurity; and political stressors such as discriminatory practices and policies. Residents in degraded inner-city environments often lack time, access to convenient facilities, and safe places to be active.(2,3) In addition, the residents of neighborhoods suffering from crime and insecurity become more confined indoors, increasing inactivity and exposure to household toxics. Millions worldwide reside in such neighborhoods yet studies that help us understand the rich context of life, environment, and health in such places are very scarce. This is partly because access to residents is difficult (people work multiple jobs, move frequently, and trust of researchers is low): it took us 30 months of learning about the difficulties and developing capabilities appropriate to the area to gather data from 80 households, capturing 254 people. Our target population is truly at the margins; in much community-based research work those who are more accessible or more connected to neighborhood organizations tend to be chosen, leaving out marginalized populations. It is also because single-discipline/single-focus research tools lack the diversity of data and analyses to yield holistic understanding: health surveys capture health data, risk perception surveys capture perception data, censuses capture socioeconomic/demographic data, and so on. The influential “Healthy People 2010” report recommends we develop and test new multistakeholder, multidisciplinary approaches for assessing how the built environment impacts human health(4) so health and environment policies can be more responsive to needs and local priorities. We present such an approach and findings.
The pilot work described here was one part of a five-part community-based participatory research (CBPR) effort called: “Strengthening vulnerable communities in the Worcester built environment—Neighborhood STRENGTH” (2004–2009). The four partners were: the Worcester Youth Center, the community-based nonprofit Regional Environmental Council, a local primary care provider Family Health Center, Inc., and Clark University. All are situated in the Main South/Piedmont neighborhood of Worcester. The full effort is described in Downs et al.(5)
1.1. Aims
For our target area we answer: (1) How can we assess vulnerability to multiple stressors? Generalizing, we also address: (2) What is the nature of complex vulnerability—including risk perceptions, health profiles, and a household index? (3) How can pilot findings be used by our wider community, and what lessons did we learn? (4) What implications arise for science and policy?
1.2. Study Area
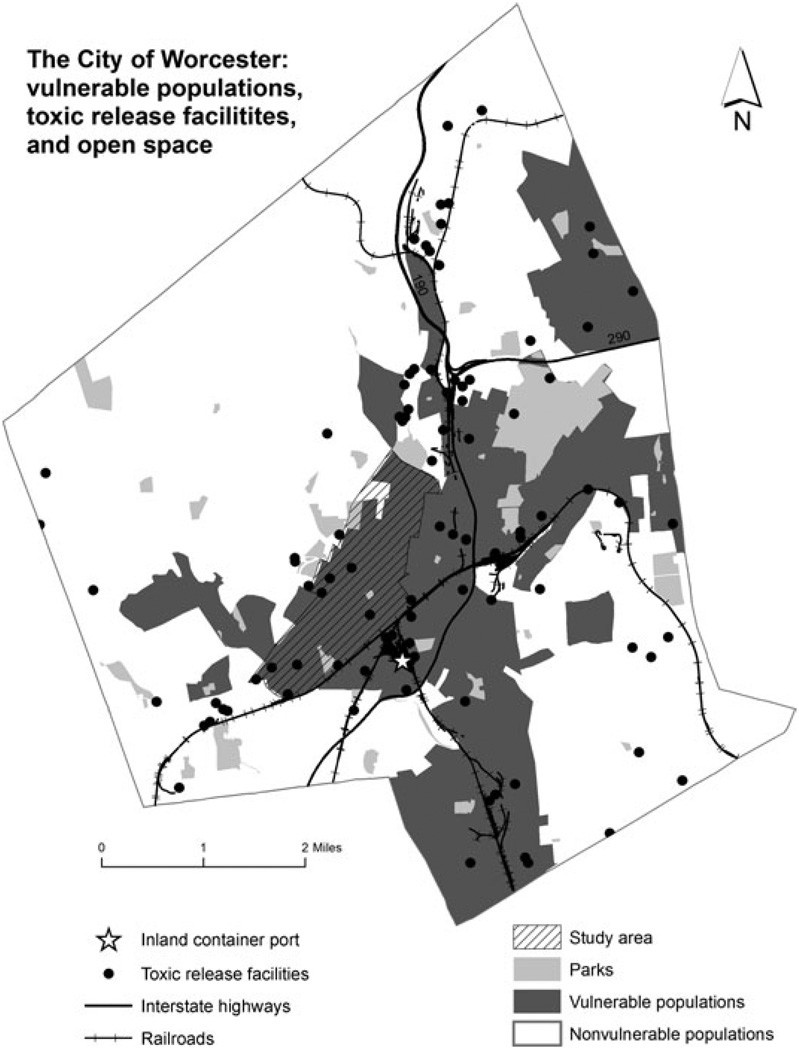
Worcester, Massachusetts is the second largest city (2006 population 175,500) in New England. In the mid-late 19th century, Worcester and the Blackstone River Valley were the birthplace of the U.S. Industrial Revolution, a bustling place of canals, mills, and factories. This history, however, also means it suffers from an inherited, persistent pollution burden (e.g., lead in much of the soil, PCBs in some pond/lake sediments). Main South/Piedmont census tracts included in the study area—7,313, 7,314, 7,315—have much larger proportions of people of color (70, 75, and 60%, respectively), and people living below the poverty line (40, 38, and 34%, respectively), compared to the city as a whole (30% people of color, and 18% in poverty; Table I).(6) Main South (7,313) and Main Middle/Piedmont (7,314) are 44.3% and 47.7% Latino, respectively, compared to 15.0% citywide. The study area—the university’s local community—enjoys a highly ethnically diverse population, including recent immigrants from Albania and West Africa, refugees from Sudan, and immigrants from Vietnam, Brazil, and the Dominican Republic. Fig. 1 shows the study site within the City of Worcester, and some spatial attributes of interest, like TRI sites and greenspace.
Table I.
Demographic Profile of Study Site(6)
| City of Worcester | Census Tract 7,313 (Main South) |
Census Tract 7,314 (Main Middle/Piedmont) |
Census Tract 7,315 (Piedmont) |
Census Tract 7,316 (Elm Park/Piedmont) |
|
|---|---|---|---|---|---|
| Population | 172,648 | 3,679 | 4,516 | 4,801 | 6,791 |
| Race/ethnicity | |||||
| % White alone | 70.1 | 30.2 | 25.2 | 39.6 | 70 |
| % Black alone | 6.4 | 7.6 | 14.3 | 12.7 | 6.8 |
| % Asian alone | 4.5 | 11.5 | 7.8 | 5.1 | 5.4 |
| % Latino | 15 | 44.3 | 47.7 | 39.6 | 12.4 |
| Place of birth | |||||
| % Native | 85.4 | 80.8 | 74.4 | 69.8 | 79.1 |
| % Puerto Rican | 5.5 | 19.8 | 18.9 | 14.5 | 3.8 |
| % Foreign born | 14.5 | 19.1 | 25.5 | 30.1 | 20.8 |
| Median household income | 35,623 | 23,029 | 17,754 | 19,599 | 22,188 |
| % below poverty level | 17.9 | 40.4 | 38.1 | 33.6 | 35.0 |
| 100% count of housing units | 70,723 | 1,380 | 1,831 | 2,078 | 2,782 |
| Median year housing built | 1946 | Before 1940 | Before 1940 | 1942 | Before 1940 |
| Occupancy status—% vacant | 5.2 | 10.1 | 12.1 | 10.0 | 6.7 |
| Tenure—% owner-occupied | 43.3 | 13.6 | 12.9 | 12.1 | 11.0 |
| Median gross rent as% of household income | 25.1 | 29.8 | 28.1 | 27.2 | 31.2 |
| Population density (no./sq. mile) | 4,600 | 12,640 | 16,129 | 20,517 | 14,480 |
Fig. 1.
Study area in Worcester City. Shows paucity of green space, toxics release inventory (TRI) sites (2006 data), and roads. Vulnerable groups are designated as “environmental-justice populations” according to U.S. Census socioeconomic data.(6) Map prepared by Yelena Ogneva-Himmelberger. From Ref. 5, used by permission of Elsevier Ltd.
Main South has population density 12,600/sq. mile, compared with 4,600/sq. mile for the city as a whole (Table I). Most of the housing units are old (pre-1940) triple-deckers (wood-framed three-story dwellings built to house working families), and are renter-occupied. Their age means lead paint exists inside and outside, posing the major hazard of lead poisoning, especially for infants and small children; lead paint for houses was not banned until 1978. Green space is scarce: in Main South, only 3.4% of the land, or 13.7 acres is park space; in Piedmont, a mere 1.2% of the land, or 3.2 acres is green.(7) Crime data show that Main South and Piedmont have the highest number of reported incidents of any neighborhood (roughly 25% of all incidents in 2000) and the highest number of arrests for violent crimes like assault and battery (27%) and simple assault/threatening (22%).(8)
2. METHODS
We obtained Clark University IRB approval for the work and informed consent from all research participants.
2.1. Frameworks
Together with our community partners, we used community-based participatory research (CBPR) to design and implement our survey tool. Our community partners were actively involved in the design of the survey tool and this allowed us to develop a balanced set of questions about assets and liabilities that met our collective needs while de-emphasizing negative risk/stress/health aspects that can reinforce disempowerment among respondents. CBPR is increasingly being recognized by health scholars and donors as a potent approach to collaboratively studying and acting to address health disparities.(9) Fawcett et al.(10) outline how building collaborations and community partnerships serve as a catalyst to understanding community needs for health and development, and contribute significantly to community empowerment. CBPR rests on a firm experiential foundation of participatory methods.(9,10,11)
Biosocial and ecosystem approaches to health are appropriate because the “health” of natural and built environments directly and indirectly impinges on human health.(12,13) We used “vulnerability theory” as our theoretical framework. An extension of risk theory, it lends itself to holistic, systems-based models. Vulnerability comprises: (1) differential exposure to stressors; (2) differential susceptibility and sensitivity to adverse outcomes if exposed (susceptibility relates to predisposition of outcomes occurring if exposed; sensitivity to how probability and degree change with changes in exposure); (3) differential preparedness to respond; and (4) differential “coping,” “resilience,” “adaptability” or ability to recover from impacts.(14,15) A function of adaptive capacity, vulnerability links directly to the need for capacity building. In this way, “vulnerability” and “sustainability” may be seen as two halves of the same coin: building societal capacity reduces vulnerability and increases relative sustainability.(13) Perceptions of risk are a key aspect of risk-induced stress so we also investigate perceptions in our questionnaire.
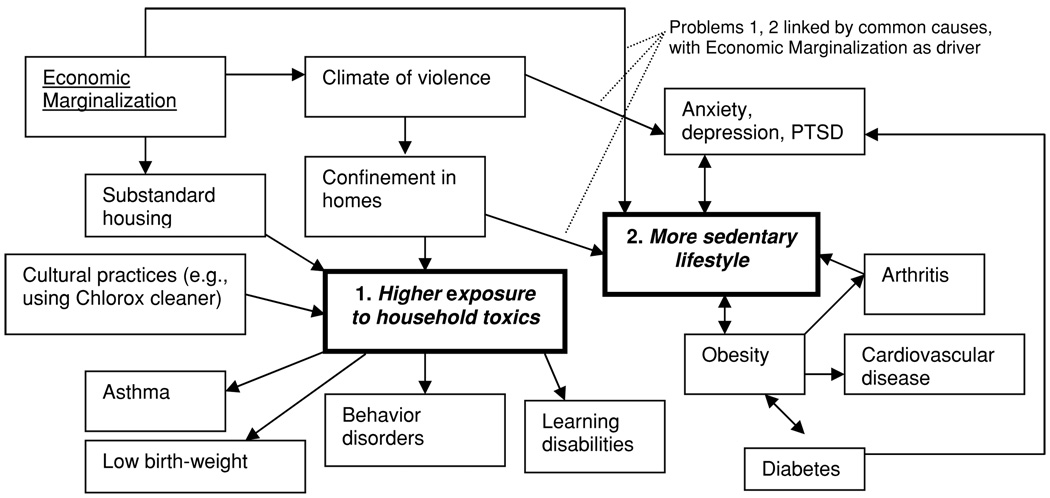
To inform questionnaire design, we employed an objectives-oriented project planning (ZOPP) approach to draw portions of the Main South/Piedmont vulnerability system with a group of teens at the Worcester Youth Center (Fig. 1). ZOPP is a popular problem-tree approach used by international development professionals (originating with Germany’s GTZ—Deutsche Gesellschaft für Technische Zusammenarbeit) to identify priority problems, causes, and consequences with stakeholders, then design strategies to solve them.(16,17) In the focus group we held an open dialogue about neighborhood concerns and needs, and what we might do about them, then modeled them with ZOPP. The group was facilitated by Ross and a graduate student; Ross has a close working relationship of trust with the Center and its attendees. In Fig. 2, two connected problem trees—toxics and sedentary lifestyle—are linked by a common cause, confinement to homes. Confinement results from a climate of violence and economic marginalization. This illustrates how a climate of violence—a social environmental stressor—reinforces other sources of environmental risk, and is a contributing indirect cause of multiple environmental health effects that reinforce each other. Evidence from the literature provided specific health outcomes to the model. Teens who expressed interest in tackling the issues were invited to join our youth group: “The A Team” (“A” for Action). A cohort of 6–8 members per year received stipends as youth action researchers for the parent project’s four-year duration.(5,18)
Fig. 2.
Dialogue-defined model of vulnerability system. Two problems—exposure to toxics and sedentary lifestyle—share common psychosocial causes/drivers. Identifying problems and drivers resulted from dialogue with teens from the Youth Center, while outcomes came from literature. From Ref. 13, used by permission of Blackwell Publishing.
Based on that exercise, other scoping with focus groups,(19) and ongoing dialogue among project partners, we grouped local stressors into four categories: pollution stressors (e.g., particulate matter in outdoor air, lead in homes); physical environment stressors (e.g., trash, lack of green space); social stressors (e.g., crime, racial discrimination); and economic stressors (e.g., low-income jobs, high unemployment).
2.2. Questionnaire
The 148-question vulnerability tool had six sections: demographic data; local knowledge, concerns, and resources; time-activity patterns; health information; risk and stress perception; and existing capacity and resources (Appendix). We translated the tool into Spanish, and students with Vietnamese, Portuguese, and Albanian language skills helped with some surveys. The graduate students employed were native speakers with high linguistic capacity and cultural awareness. In addition, project partner Family Health Center helped design the tool and orient the interviewers as to the nature of each immigrant group and how best to engage with it. Face-to-face interviews took about 75 minutes (range 40–100) to complete. We gained a sense that many interviewees—especially those feeling isolated—enjoyed the chance to speak with us and did not find it burdensome. Interviews were conducted in pairs (interviewer and note-taker) with voice recorders if consent was given to do so. For safety, calls were made to the field research coordinator before entering the home, and upon leaving.
We aimed for a random sample (a “high bar” for marginalized groups), stratified and population-weighted by census tract, but, appropriately for a pilot, included some opportunistic sampling. Steps were: (1) set an initial target sample size (120 households); (2) stratify by each census tract in the study area, and population-weight the sample by strata; (3) undertake outreach to target streets and blocks using flyers and street-level conversations with locals to raise awareness and build trust; (4) contact selected participants by phone or in person by knocking on doors, make appointments for the interview, and explain the $20 food certificate compensation for participant’s time; (5) undertake the interview in the homes at the agreed time using one interviewer, one note-taker; and (6) contact participants who expressed interest during outreach at the local primary care clinic, and at popular meeting places. Training graduate student interviewers involved mock and pilot interviews. The target sample size was aspi-rational, and we revised it downwards after only 20 were gained in the first six months; it was not set based on confidence intervals for sample statistics. About 200 randomized addresses on the City’s Building Department records (sampling frame) were approached, with 10% no longer valid. For valid addresses where nobody was home (60/180), we re-approached three times after distributing flyers about the project on the street. Even when contacts were made (120), about 1 in 3 appointments were not kept after two more tries, giving a total yield of 80.
GPS coordinates of each household were gathered using a hand-held Garmin GPS60 (Garmin, Olathe, Kansas). We stored data in MS Access, analyzing them in SPSS 15.0 for Windows and MS Excel. The 80 surveys were completed in two and a half years (January 2005–June 2007), 70 random and 10 opportunistic, capturing 254 people. Access is difficult because: local people are wary of surveys (illegal immigrants are especially afraid of officialdom); they often work multiple jobs just to make ends meet so scheduling is hard; they move frequently; language barriers exist; and addresses randomly selected were quite often vacant. After low yields in the first six months (20), we employed opportunistic sampling for first contact at neighborhood locations like laundromats and cafés, as well as a few (4) from Family Health Center waiting area. Interviews were still undertaken in the privacy of homes.
2.2.1. Health Information
For the section on health information of respondents and their household members, we used a literature review to select 21 health conditions associated with different kinds of environmental stress. The conditions chosen reflected known local concerns and insights of partners during the design stage, and conditions commonly of interest in environmental health literature; the selection was judged comprehensive but not too burdensome to respondents. Disease burden was defined as the number of these 21 conditions each person self-identified/reported, and household burden as the average number of conditions per member.
2.2.2. Risk Perception Capture and Analysis
We used the psychometric methods of Mc-Daniels et al.(20) and Fischoff et al.(21) to capture and analyze data on risk/hazard perception. We chose 14 locally relevant hazards from the broad set of Slovic et al.(22) and five characteristics measured on a 5-point Likert scale. For each hazard, we asked: How much do you know about “X”? How new is X for this community? How easily can X be controlled? How serious are the effects of X? How likely are you to come into contact with X? Data on the five risk perception characterizations were gathered for the hazards from our 80 respondents. Factor analysis is used to reduce the number of risk characterizations to some underlying dimensions that would describe a sample population’s perception of risk in a more summarized manner. Principal component factor analysis in SPSS©15.0 (IBM, Chicago, IL) was used to extract factors to form the axes of a cognitive map summarizing respondents’ average perceptions. Two factors were extracted in the unrotated factor matrix and then a varimax rotation was used to produce a rotated matrix. This matrix was used to calculate the scores of Factor 1 and 2 for each of the 14 hazards.
2.2.3. Vulnerability Indices Versus Disease Burden
We used indicators based on primary and secondary data in Table II to construct two descriptive (not predictive) vulnerability indices at the household scale using a geographic information system (GIS). The primary data for the adaptability index (A) came from answers to selected questions on the questionnaire. Secondary data was used for the hazard index (H) in the form of location-specific information about proximity of the home to green space and potential sources of hazardous exposures.
Table II.
Vulnerability Indices’ Input Data
| Indicators for Hazard Index “H” | Indicators for Adaptability Index “A” |
|---|---|
|
|
Indicators for constructing two descriptive indices at the household scale used primary data for adaptability index (A) and secondary data for hazard index (H)
The choice of indicators was a judgment based in part on peer-reviewed literature, availability of primary and secondary data, and relevance of the indicators in the context of the study area. As described in Table II the values were standardized and normalized; this permitted summation using equal weights (final scale 0.0–1.0). Arc GIS (Environmental System Research Institute, Redlands, CA) was used to map household locations and calculate proximity to TRI sites, brownfield sites, waste disposal sites, Superfund sites, major roads, rail lines, and open spaces. Data for TRI sites, brownfield sites, and Superfund sites were taken from secondary sources. We mapped resulting indices at the block scale, and plotted household health burden against indices. Linear regressions were carried out in Excel.
3. RESULTS
3.1. Demographic
The 80 surveys—55 female respondents, 25 male—were completed in two and a half years. Respondents were of diverse self-identified ethnicities: white/Caucasian (18); other Hispanic (12); Puerto Rican (11); African American (5); Native American (4); W. European (3); African (3); Vietnamese (3); Dominican (1); Mexican (1); Central American (1); other (12); don’t know (1). The sample’s diversity reflects reasonably the census data presented in Table I. We gathered data on 254 people in the 80 homes: 132 females and 114 males (8 “missing”); mean age of females 29 years (SD 19, range 0.08–75) and of males 26 (SD 18, range 0.5–78). A third of households have incomes less than US$10,000/yr, another third $10,000–$30,000/yr, and fewer than 10% over $50,000/yr. Close to 75% of household members have less than $10,000/person/yr. Eighty percent of households rent, and spend on average 40% of their income on rent (SD 24%). Most households (94%) have all members able to read and write. About 22% of households have at least one member who does not speak English and 22% at least one who does not read it. About 75% of respondents have at least a high school diploma or GED; of these 20% of respondents graduated from a four-year college.
Thirty-nine percent are in school, 33% work, and 28% do neither. While 20% of respondents have lived in the neighborhood for only one year, the mean time is over nine years and one respondent had lived there 38 years. Most respondents (about 70%) had not moved in the past year; except for two individuals who had moved six times and three times, respectively, the rest had moved once or twice. The mean number of people in the households was about 3 with range 1–7.
3.2. Neighborhood Life
Questions about neighborhood life provide rich contextual insight with great variety in the attributes and concerns emphasized. Most residents find things to like about the neighborhood, citing such diverse attributes as convenience, safety, or peacefulness; few mention affordability or ethnic diversity as attractions; however, 25% said they moved into their homes because of affordability, while 16% said comfort. People’s perceptions of change during their residency are also divided between a plurality that said things remain the same, those who saw them as improving, and those who said they are getting worse. Some gave specific examples: a few said there is more crime and violence now; half as many said crime has gone down. In general people describe services as acceptable (“OK”) or better, and in many cases they have observed improvement. Sidewalks are perceived worst, then tap water. Despite common complaints about trash in streets, and persistent visible blight from trash, most rate trash pick-up and recycling “OK” or better. Over time, 31 said health services have improved, 29 said they are the same, and six said they have worsened. Forty said sidewalks have stayed the same, 21 said they have worsened. When asked what one thing would improve the neighborhood most: 33% said better trash pick-up and street cleaning; others mentioned more activities for youth, more police/better security, renovate abandoned houses, make more open spaces/beautify. Responding to a question about willingness to pay for a complete clean-up, roughly similar numbers (in decreasing order) said zero, $5/mo, $10/mo, and > $10/mo. Only 22% had participated in neighborhood clean-ups. Of the 50% who mentioned specific types of pollution, trash, oil/gas, construction materials, odors, water, or soil pollution were listed.
3.3. Stress and Risk Perception
Social stressors rank highest followed by physical stressors among the problems respondents worry about (Table III). Drugs and prostitution, and crime and violence were each placed in their top three worries by over 50% of the respondents; trash and dirty streets followed among major concerns Pollution and lack of green space are of moderate concern. Asked how they cope with the problem that worries them most: ignoring it and “don’t know” were the most common responses; calling the police, counseling their children, vigilance with their children, and limiting the time children go outside, and not going out at night were also mentioned. Asked about additional resources they would like to help deal with the problem, a third said more police, improved trash pick-up, more activities for youth, more involvement of neighbors, and more community organizations. Only 3% said more jobs.
Table III.
Top Three Problems Respondents Worry About
| Ranking |
|||
|---|---|---|---|
| Problem | 1st | 2nd | 3rd |
| High worry | |||
| Drugs and prostitution | 34 (43%) | 8 (11%) | – |
| Crime/violence/gangs | 15 (19%) | 11 (15%) | 11 (21%) |
| Dumping of trash/dirty streets | 8 | 7 | 1 |
| Traffic/roads/cars | 5 | – | – |
| Noise | 4 | 3 | 3 |
| Theft and loss of property | 3 | – | – |
| School service | 2 | – | – |
| Drinking water | 2 | – | – |
| Drugs/smoking/alcohol | 2 | 8 | 5 |
| Moderate worry | |||
| Safety/security | – | 7 | – |
| Bad neighbors | – | 5 | – |
| Pollution | – | 3 | 6 |
| Lack of law enforcement | – | 3 | – |
| Lack of open space | – | 2 | 3 |
| Low worry | |||
| Vandalism | – | 2 | – |
| Snow in winter | – | 1 | 1 |
| Homelessness | – | 1 | – |
| People just hanging around | – | – | 3 |
| Discrimination | – | – | −3 |
| Poor health service | – | – | 2 |
| Animals | – | – | 2 |
| Don’t know/no problem | 5 | 10 | 12 |
| Total (n) | 80 | 71 | 52 |
Numbers are frequencies of responses (1st, 2nd, or 3rd). The problems fall into three groups: high worry; moderate; low.
A similar picture emerged from other questions. The reported top sources of stress at home included financial problems, dealing with children/family, health concerns, and insecurity issues (Table IV). Pollution was only mentioned by 3%.When asked to rank a predetermined set of 21 hazards/stressors, the ones mentioned of most concern (in decreasing order) were drugs in the community, handguns, crime, and violence (Table V). Only a few said lead in drinking water or trash, and one respondent said terrorism. Asked about their next biggest concern, respondents chose violence, drugs, crime, handguns, and people losing jobs.
Table IV.
Top Source of Stress Perceived by Respondents at Home
| Top Source | Count | % |
|---|---|---|
| Financial problem | 13 | 18.6 |
| Children/family | 10 | 14.3 |
| Health | 6 | 8.6 |
| Insecurity | 6 | 8.6 |
| Dealing with people | 3 | 4.3 |
| Household work | 3 | 4.3 |
| Work pressure | 3 | 4.3 |
| Pollution | 2 | 2.9 |
| Loud noise | 2 | 2.9 |
| Loneliness | 2 | 2.9 |
| Lack of time | 1 | 1.4 |
| Dealing with tenants/landlord | 1 | 1.4 |
| Unemployment | 1 | 1.4 |
| Boyfriend/girlfriend | 1 | 1.4 |
| Having no children | 1 | 1.4 |
| Lack of privacy | 1 | 1.4 |
| No stress/don’t know | 14 | 20.0 |
| Total | 70 | 100.0 |
Table V.
Hazard/Stressor Ranking: Psychosocial Stressors Dominate
| Hazard of Most Concern | Count | % | Hazard of Next Concern | Count | % |
|---|---|---|---|---|---|
| Drugs in the community | 24 | 30.4 | Violence in the community | 16 | 20.3 |
| Handguns in the community | 18 | 22.8 | Drugs in the community | 15 | 19.0 |
| Crime in the community | 10 | 12.7 | Crime in the community | 13 | 16.5 |
| Violence in the community | 7 | 8.9 | Handguns in the community | 11 | 13.9 |
| Lead in your drinking water | 5 | 6.3 | People losing their jobs | 4 | 5.1 |
| Trash/illegal dumping | 3 | 3.8 | Motor vehicle accidents in the community | 3 | 3.8 |
| People losing their jobs | 3 | 3.8 | Health effects of alcohol | 3 | 3.8 |
| Noise level in the community | 2 | 2.5 | Trash/illegal dumping | 2 | 2.5 |
| Police relations | 2 | 2.5 | Terrorism | 2 | 2.5 |
| Health effects of cigarette smoke | 2 | 2.5 | Health effects of cigarette smoke | 2 | 2.5 |
| Side effects of prescription drugs | 2 | 2.5 | Lead in soil, dust, and paint | 2 | 2.5 |
| Terrorism | 1 | 1.3 | Noise level in the community | 1 | 1.3 |
| Total (n) | 79 | 100.0 | Nutrition | 1 | 1.3 |
| Police relations | 1 | 1.3 | |||
| Chemicals in house cleaning products | 1 | 1.3 | |||
| Health effects of pesticides | 1 | 1.3 | |||
| Lead in your drinking water | 1 | 1.3 | |||
| Total (n) | 79 | 100.0 |
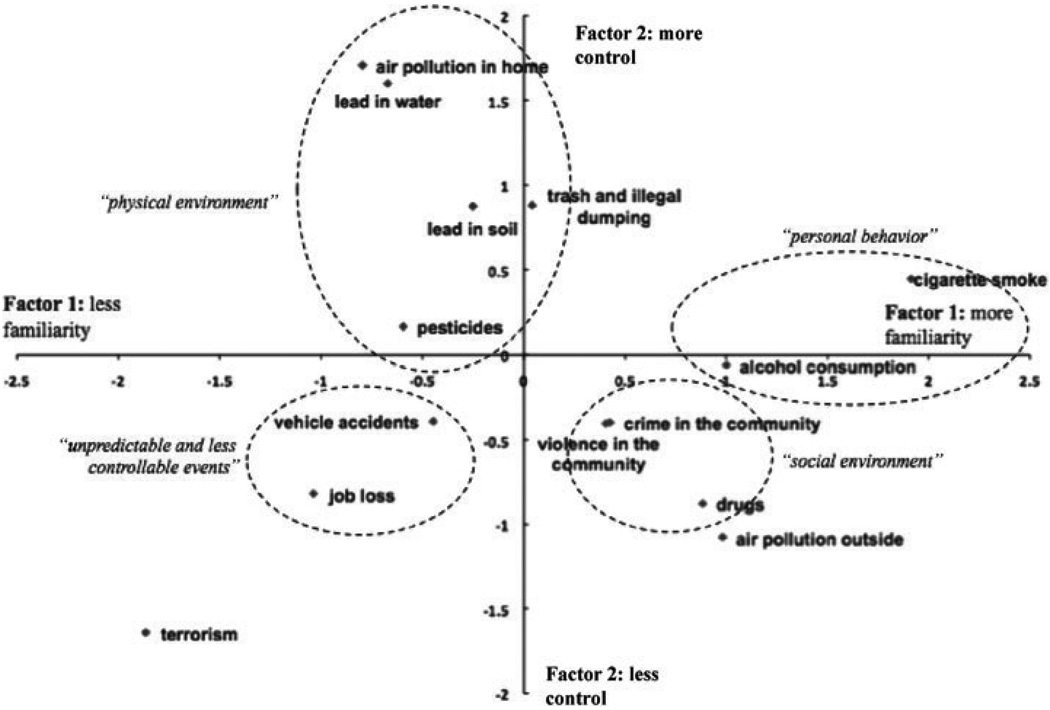
The cognitive map of risk perception comprises two factors representing level of “familiarity” and level of “control” as shown in Fig. 3. Factor 1 correlated highly with levels of knowledge (0.825), newness (0.942), seriousness (0.844), and contact (0.769), thus, “familiarity” was the term used to describe this factor. Factor 2 only correlated with control (0.989), so was simply labeled “control”. Over 60% of the variance in all 5 characteristics was explained by the two extracted factors. The dominant psychosocial stressors—crime in the community, violence in the community, and drugs—are located in the high familiarity/low control quadrant, indicative of high exposure and low coping capacity. Notably, lead in soil and lead in water, pesticides, and air pollution at home have low familiarity but high control while air pollution outside has high familiarity but low control. Surprisingly, vehicle accidents and job loss are in the low familiarity/low control quadrant (the survey was done before the 2008 economic recession), and terrorism is rated very low familiarity despite the September 11, 2001 attacks.
Fig. 3.
Cognitive map summarizing risk perceptions. Two-factor representation of factor scores for each of 14 hazards. Dashed circles show identified clustering of risks.
3.4. Visual Survey
In a subjective visual survey of interior and exterior household conditions by interviewers most indicators showed “OK” or “good” conditions. The highest “poor” indicator proportions were 16% for poor backyards, 13% poor exterior walls, and 10% poor overall cleanliness.
3.5. Time-Activity and Mobility
The question on time-activity was open-ended; asked to mention three places respondents spend most time in the neighborhood (outside home, work, or school), shopping for groceries was mentioned most, by 22% of respondents, next most frequent mentions were the park, restaurants or bars, and friends’ or relatives’ homes. The gym/exercise/play was only mentioned four times, church three times. These are places where stress relief can occur, are available to local residents, yet underutilized. Turning to mobility: 30% of households do not own a functioning car, 38% have one, 25% two, and 7% more than two. To shop and run errands, 74% use a car, 9% a taxi, 9% the bus, and 6% walk. Slightly more than half report spending money each week on buses or taxis in amounts ranging from $1–40 per week. On average those captured by the survey spend 80% of their time per year indoors.
3.6. Health Information
3.6.1. Insurance
Most respondents had health care coverage (it is mandatory in Massachusetts since 2006) and believed that they had reasonable access to health care services. When asked about health care coverage for themselves, 95% said they have it, only 5% do not. Regarding other household members, out of 64 respondents, 83% said all members have coverage, 13% said some, 4% don’t know. Sixty-one percent have a government plan (Medicare, Medicaid, or MassHealth), 20% receive coverage from their employer, 9% through someone else’s employer, 4% have a private plan, 3% have military/VA coverage, and 3% another type. Asked who they speak to most about health concerns, one-half said doctors, one-third said family members, and a few said friends/co-workers, social worker/counselor, “other,” or “don’t know.” On ease of obtaining health care, 14% said very easy, 46% easy, 19% neutral, 9% difficult, and 12% very difficult.
3.6.2. Disease Profile and Burden
Table VI shows the ranking and prevalence of responses to a list of 21 health problems. Allergies rank top, followed by back pain, smoking, asthma, depression, high BP, sleep disorder, and chronic pain. Heart disease ranked 17th overall at 5%; while only three cases of cancer were captured. Many people reported suffering from multiple problems; notably they tend to be of very low income. Table VII shows the reported pattern for the top 10 burdened females and males, and income poverty. Eighteen of the 20 cases have annual income ≤ $10,000/person/yr. The females’ age range is 30–75 years, with a burden range 9–13 health problems/female. There are several women with co-occurring back problems, chronic pain, allergies, asthma, chronic bronchitis, pneumonia, depression, and insomnia. All 10 women report suffering from depression. Among the top-10 males, age range is 3–56, burden range 4–12 problems/male. In males, there is no discernable pattern of co-occurrence of illness.
Table VI.
Ranking and Prevalence of Health Problems
| Health problem | Count (n = 254) | % |
|---|---|---|
| 1. Allergies | 72 | 28.0 |
| 2. Back pain | 58 | 22.6 |
| 3. Smoking habit | 49 | 19.1 |
| 4. Asthma | 42 | 16.3 |
| 5. Depression | 33 | 12.8 |
| 6. High blood pressure | 33 | 12.8 |
| 7. Insomnia or sleep disorder | 31 | 12.1 |
| 8. Chronic pain | 26 | 10.1 |
| 9. Behavioral or emotional disorders | 19 | 7.4 |
| 10. Diabetes | 19 | 7.4 |
| 11. Skin disorders | 18 | 7.0 |
| 12. Pneumonia | 17 | 6.6 |
| 13. Chronic bronchitis | 15 | 5.8 |
| 14. Miscarriages | 15 | – |
| 15. Anemia | 12 | 4.7 |
| 16. Ulcer | 12 | 4.7 |
| 17. Heart disease | 12 | 4.7 |
| 18. Gastro-intestinal infection | 8 | 3.1 |
| 19. Elevated lead/lead poisoning | 8 | 3.1 |
| 20. Cancer | 3 | 1.2 |
| 21. Tuberculosis | 0 | 0.0 |
Table VII.
Disease Profile of Top-10 Burdened Females and Males: Shows Co-Morbidity Patterns and Income Poverty: 18 of the 20 Cases Have Annual Income ≤ $10,000/person/yr.
| Gender | Number in home | No. disease/ person | Age (yrs) | Annual income/person ($’000/yr) |
Time in area (yrs) | % lifetime in area | Ethnicitya | Back problems | Chronic pain | Allergies | Asthma | Chronic bronchitis | TB | Pneumonia | Behavioral or emotional disorder |
Depression | Insomnia or sleep disorder |
Anemia | Diabetes | GI infection/persist. diarrhea |
Ulcer | Cancer | Heart disease | High BP | Skin disorder | Smoking habit | Miscarriage | Elevated lead levels or lead poisoning |
Avg. disease burden per person per home |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F | 2 | 13 | 59 | 5.0 | 10.0 | 16.9 | C | • | • | • | • | • | • | • | • | • | • | • | • | • | 6.50 | ||||||||
| F | 1 | 12 | 53 | 10.0 | 11.0 | 20.8 | C | • | • | • | • | • | • | • | • | • | • | • | • | 12.00 | |||||||||
| F | 1 | 12 | 75 | 10.0 | 13.0 | 17.3 | C | • | • | • | • | • | • | • | • | • | • | • | • | 12.00 | |||||||||
| F | 1 | 11 | 55 | 15.0 | 10.0 | 18.2 | C | • | • | • | • | • | • | • | • | • | • | • | 11.00 | ||||||||||
| F | 4 | 11 | 33 | 10.0 | 0.5 | 1.5 | W | • | • | • | • | • | • | • | • | • | • | • | 3.75 | ||||||||||
| F | 4 | 10 | 66 | 6.3 | 8.0 | 12.1 | C | • | • | • | • | • | • | • | • | • | • | 3.00 | |||||||||||
| F | 1 | 10 | 55 | 10.0 | 24.5 | 44.5 | C | • | • | • | • | • | • | • | • | • | • | 10.00 | |||||||||||
| F | 2 | 9 | 41 | 5.0 | 1.0 | 2.4 | W | • | • | • | • | • | • | • | • | • | 6.50 | ||||||||||||
| F | 1 | 9 | 30 | 10.0 | 8.0 | 26.7 | C | • | • | • | • | • | • | • | • | • | 9.00 | ||||||||||||
| F | 1 | 9 | 46 | 10.0 | 0.8 | 1.6 | W | • | • | • | • | • | • | • | • | • | 9.00 | ||||||||||||
| M | 1 | 12 | 56 | 10.0 | 13.0 | 23.2 | C | • | • | • | • | • | • | • | • | • | • | • | • | n/a | 12.00 | ||||||||
| M | 2 | 9 | 40 | 5.0 | 0.2 | 0.4 | W | • | • | • | • | • | • | • | • | • | 8.50 | ||||||||||||
| M | 3 | 7 | 20 | 5.0 | 5.0 | 25.0 | C | • | • | • | • | • | • | • | 3.67 | ||||||||||||||
| M | 4 | 7 | 38 | 10.0 | 0.3 | 0.7 | C | • | • | • | • | • | • | • | 3.25 | ||||||||||||||
| M | 1 | 6 | 50 | 10.0 | 8.0 | 16.0 | W | • | • | • | • | • | • | 6.00 | |||||||||||||||
| M | 6 | 4 | 3 | 2.5 | 3.0 | 100 | ? | • | • | • | • | 2.33 | |||||||||||||||||
| M | 5 | 4 | 19 | 2.0 | 0.7 | 3.5 | W | • | • | • | • | 1.60 | |||||||||||||||||
| M | 3 | 4 | 42 | 8.3 | 1.2 | 2.8 | W | • | • | • | • | 2.33 | |||||||||||||||||
| M | 1 | 4 | 47 | 60.0 | 3.0 | 6.4 | W | • | • | • | • | 4.00 | |||||||||||||||||
| M | 4 | 4 | 53 | 10.0 | 5.0 | 9.4 | C | • | • | • | • | 2.25 |
W = white/Caucasian person; C = person of color; n/a = not applicable.
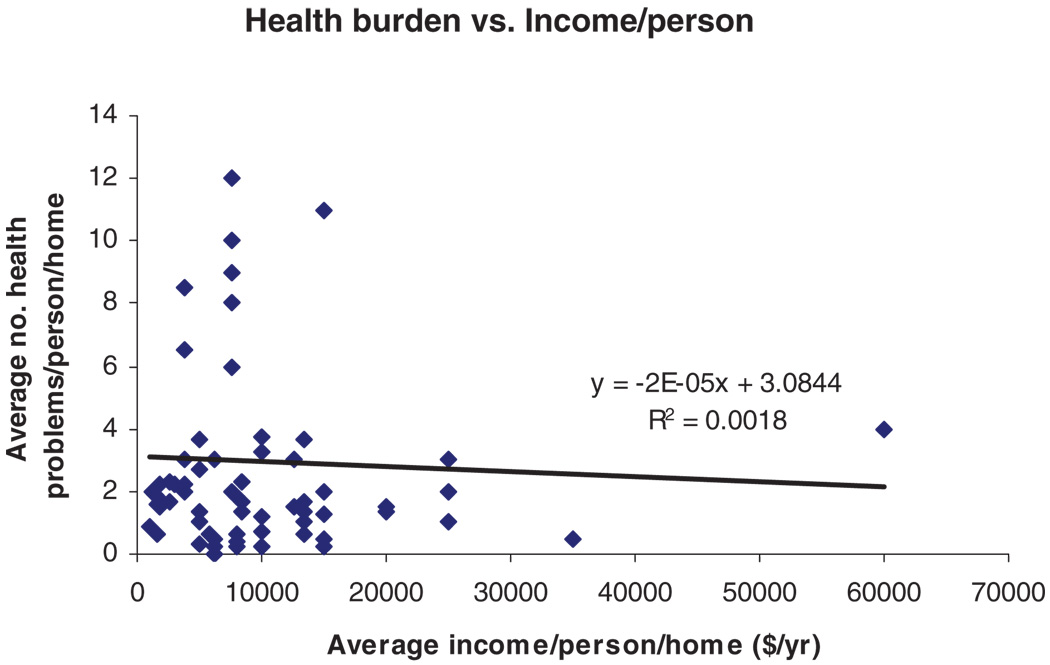
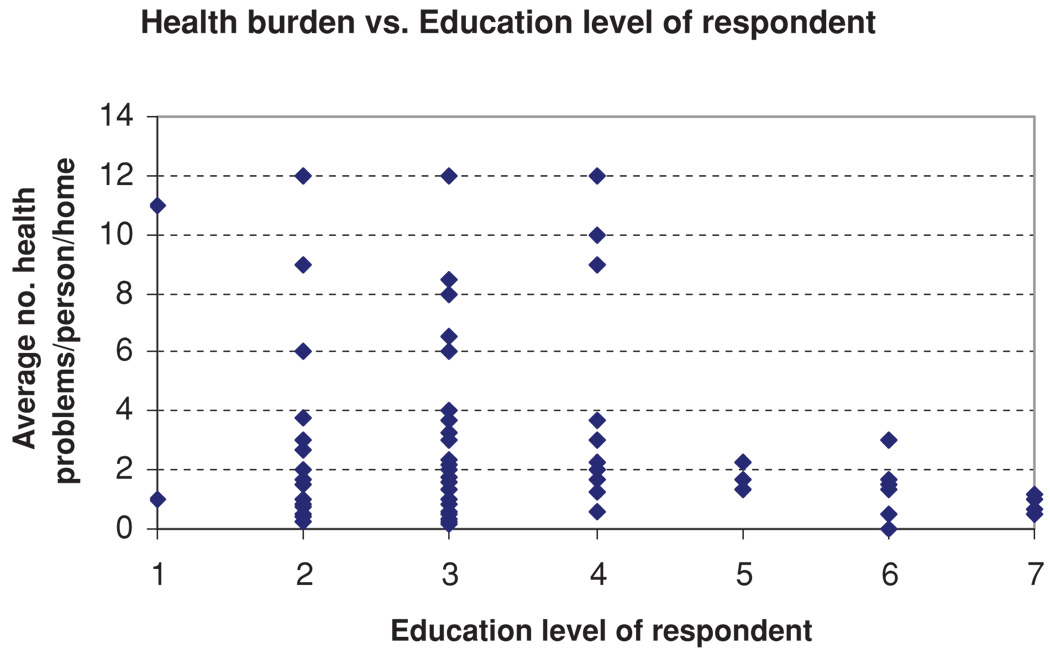
Except for the highly burdened group there was no overall correlation between health burden per person and average income per person, by household (Fig. 4). On average those households with respondents who have a two-year degree or higher have much less health burden, and in the 12 most burdened households, education level of the respondent is high school/GED or less (Fig. 5).
Fig. 4.
Health burden vs. average income per person by household. Shows no overall correlation (n = 80), though seven of the eight most burdened homes do have an income <$10,000/person/yr.
Fig. 5.
Health burden versus educational level of respondent by household. Levels: (1) no school or kindergarten; (2) less than high school; (3) high school or GED; (4) some college; (5) 2-year degree; (6) 4-year degree; (7) grad school.
Based on their reported heights and weights, about 40% of respondents have BMI 30 or above (obese). All households report engaging in less than seven hours of active or heavy exercise per person per week, with a mean 3.1 hours/wk (SD 2.0).
3.6.3. Health Disparities
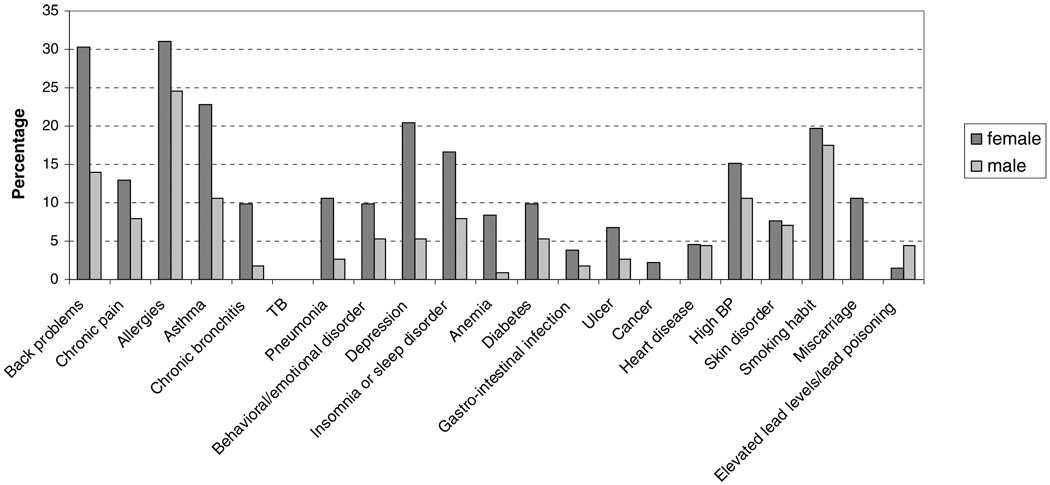
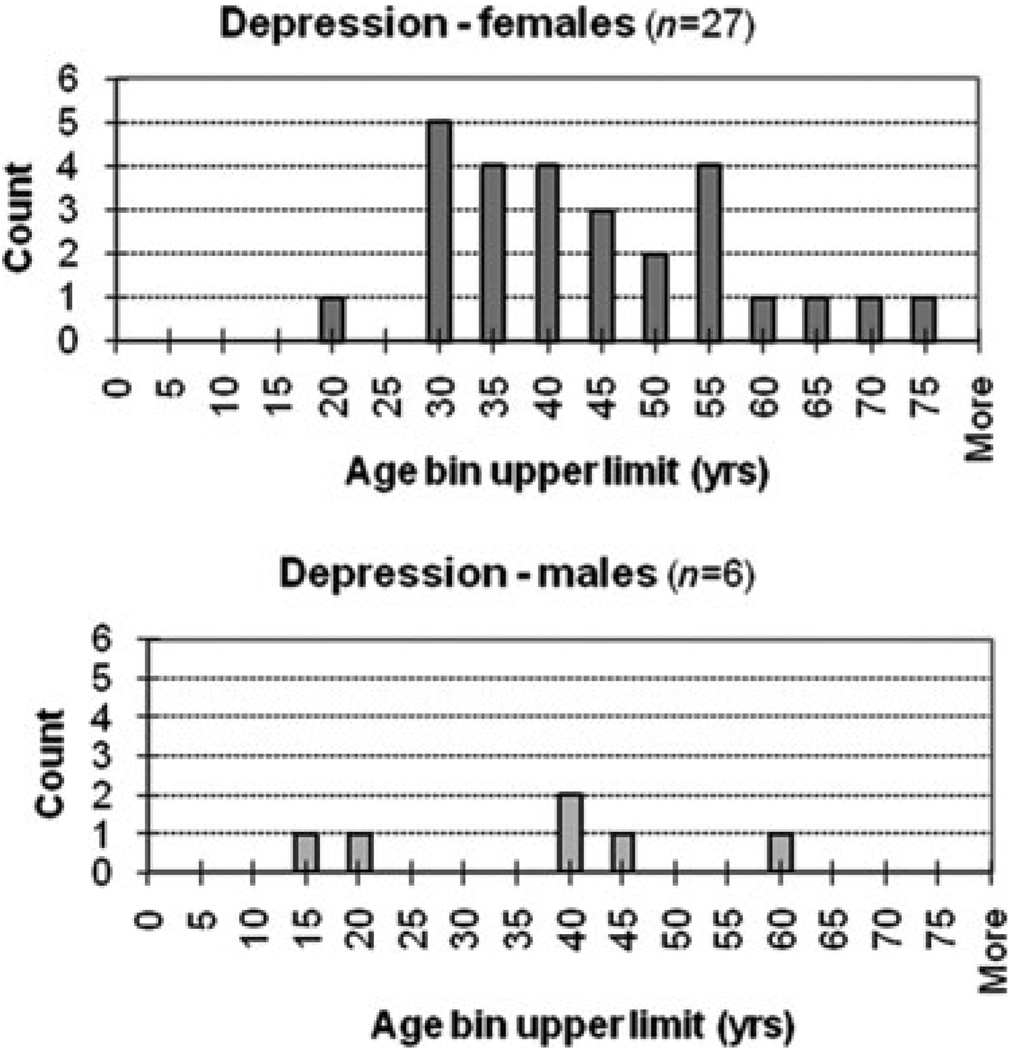
Gender disparities are significant in the reported number of diseases per person: females (M = 2.545, SE = 0.2713, Var = 9.715, n = 132) have almost twice the disease burden of males (M = 1.351, SE = 0.2713, Var = 3.628, n = 114, t(221) = −3.67, p < 0.01). On average, there was no significant difference in age between females and males, or time in the neighborhood. Fig. 6 shows that this disparity runs the full spectrum of diseases captured. Ethnicity also appears to matter, at least for females. On average, white females (M = 4.348, SE = 0.699, Var = 11.23, n = 23) have 2.0 times the disease burden of females of color (M = 2.220, SE = 0.303, Var = 9.183, n = 100, t(31) = 2.79, p < 0.01). No significant difference was found, on average, between the burden of white males versus males of color. Histograms for the 21 self-reported diseases were captured by gender and age. Gender disparities are prominent in diseases associated with psychosocial stress like depression (Fig. 7).
Fig. 6.
Gender distribution of health problems by percentage (132 females, 114 males). [From Ref. 5, by permission of Elsevier, Inc.]
Fig. 7.
Histograms of depression.
The gender of the respondent did not appear to influence the gender disparity in reported disease burden for members of the household. Considering proxies for exposures, on average, there was no significant difference in either age or time in the neighborhood between people of color and whites and no significant correlation between reported health problems and time in neighborhood. Asthma rates did not differ significantly between people of color and whites. We found no significant difference in household income per person/home or education level of respondents between people of color and whites. Interestingly, social group membership differences were significant: 92% of respondents of color belong to neighborhood groups compared to only 72% of white respondents (p < 0.05). When asked: “Do you feel safe and secure in your home?” 80% of both whites and people of color responded “yes.”
3.7. Vulnerability Index
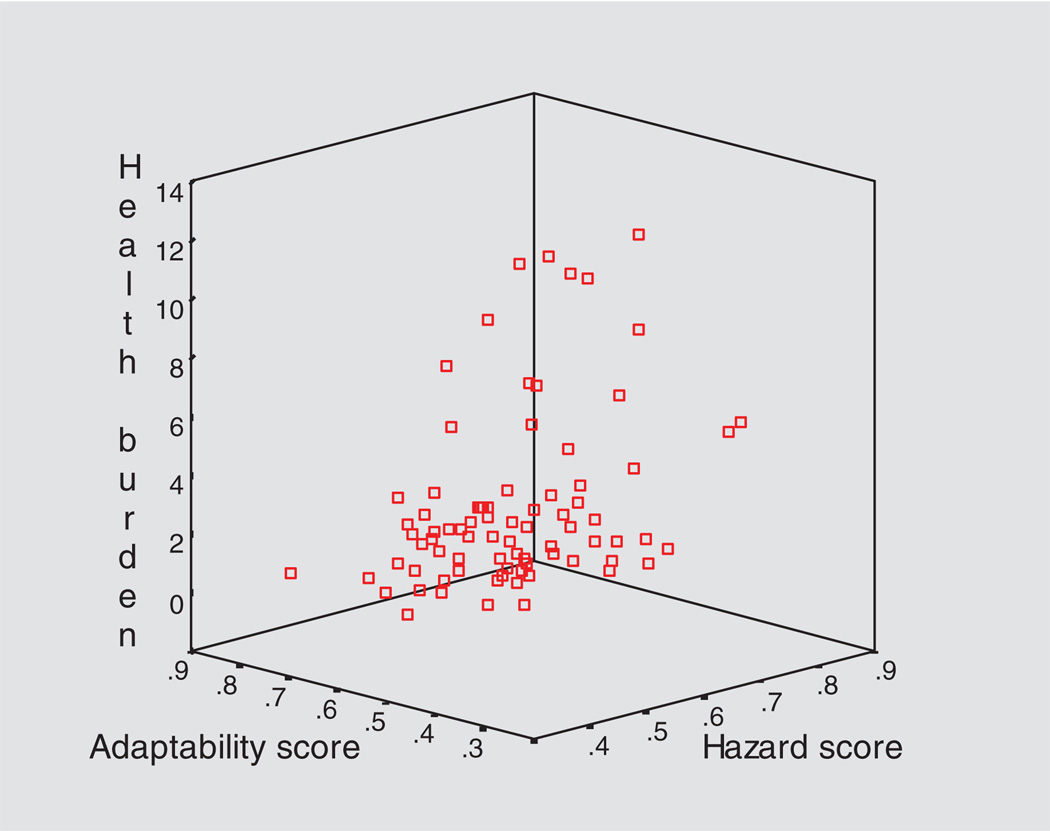
A GIS-based vulnerability index that summarizes information about proximity to hazards and proximity to resources for coping can serve useful purposes in planning and development contexts. We showed that a GIS-based vulnerability index at the household scale is practical and useful in terms of its ability to incorporate primary and secondary data, its ability to show a measure of relative vulnerability on the scale at which it is experienced (individual/household rather than block, block-group, or town as in other studies), and its stimulation of a creative dialogue about how best to model vulnerability. The 3-D plot of household disease burden against two independent indices, hazard index and adaptation index (Fig. 8), reveals a weak association worthy of further exploration.
Fig. 8.
Household health burden versus vulnerability. Shows health burden (HB) as a function of standardized adaptation index (A) and hazard (H) index scores (0.0–1.0, 1.0 being maximum hazard score, or max. adaptability) for 80 randomly sampled households. HB is the average number of self-reported problems per household member, from a set of 21 problems (Table VI). The plot shows logical but weak associations worthy of further research (linear regression: HB = −11.46A + 1.42H + 8.62; r2 = 0.161, SE = 2.865).
4. DISCUSSION
4.1. Stress and Health
Risk assessments often ignore psychosocial conditions and response capacities;(23) these dimensions are more often captured by vulnerability approaches; our data set strongly supports their inclusion. Gee and Payne-Sturges(24) suggest psychosocial stress may be the “missing” vulnerability factor that links social conditions with environmental hazards. Our perception data strongly suggest psychosocial stressors dominate the stress regime of Main South/Piedmont; chronic stress-related health data are consistent with such a regime. A growing literature recognizes the importance of contextual determinants of health and health disparities, reviewed by Hillemeier et al.(25) How socio-environmental factors impact disease etiology has become a priority topic, calling for the development of new concepts and assessment tools that capture contextual determinants of health.(26–31) Williams is a pioneer of research on the social determinants of health.(32,33)
Public reporting of “chronic disease” in the United States tends to use mortality rates from diseases like heart disease and cancer; our chronic, cumulative stress-related morbidity data (Fig. 6; Table VII) reveal an important health picture society rarely sees. The most important general finding from our survey was to document the diversity, and often multiplicity, of reported health problems. Problems of highest prevalence—allergies, back pain, smoking, asthma, depression, high BP, sleep disorder, and chronic pain—are associated with chronic stressors, a weakened immune system, and pollution.(24,34–36) While reports of heart disease ranked 17th of 21 problems at 5%, the burdens of chronic stress-related illness we captured represent a major risk factor for heart-disease mortality.(37)
One limitation of our survey was that self-reported health data were not clinically verified. While self-reported/self-identified data have a legitimate place in any health exposition, in moving beyond our pilot, some clinical validation even for a small sample of respondents would be informative; it could be carried out by a primary-care partner.
U.S. Center for Disease Control and Prevention (CDC) data provide an opportunity for some comparison with national data (Table VIII); reported asthma rates stand out as much higher than the national rates. Obesity rates are slightly higher than the most recent national data, though the difference is within sampling error.
Table VIII.
Comparison of Study’s Disease Rates with National Data
Regarding health insurance coverage, the 2008 Massachusetts survey showed only 2.6% of the population without coverage, but the uninsured rate among Hispanic residents was 7.2%, and among households with incomes less than 300% federal poverty level it was 5%.(40) Our data are consistent with state findings.
4.2. Health Disparities
Gender disparities appear vividly in Table VII, co-morbidities of the top-10 burdened females and males; all 10 of the women report suffering from depression and several suffer from co-occurring back problems, chronic pain, allergies, asthma, chronic bronchitis, pneumonia, and insomnia. Unlike the females, there is no discernable pattern of health burdens in the males. Population health disparities are generally viewed to be a function of gradients in: environmental exposures; health care access, utilization, or quality; health status; or health outcomes.(30–42) On average, females report twice the chronic disease burden as males. This may be explained by: (i) reluctance of males to report illness (though this was not perceived); (ii) an increased sensitivity of females to multiple stressors (especially psychosocial ones); and/or (iii) a higher female stress burden given their multiple roles as primary caregivers, home-makers, wives, mothers, and co-income generators. Our results are consistent with epidemiological evidence that women tend to have higher morbidity (yet longer life-spans) on average than men in many societies.(43,44) Understanding why women are more burdened than men requires attention to their lifestyles and needs.(45,46) In ongoing research we are using the survey data to look more closely at the stressors and adaptive capacities of these highly burdened individuals, and compare them to those less burdened.
Frequent attention has been given to racial/ethnic disparities, often showing people of color to be more burdened than whites.(47) In Boston, Brugge et al.(48) found disparities in diagnosed asthma rates between black/African Americans born in the United States (33%) versus those born outside (11%). Our data allowed us to compare self-reported asthma rates of whites and people of color: 21% versus 15%, respectively, but the difference was not significant.
The second goal of “Healthy People 2010,” to eliminate health disparities, includes differences that occur by gender, race or ethnicity, education or income, disability, geographic location, or sexual orientation.(4) “Compelling evidence indicates that race and ethnicity correlate with persistent, and often increasing, health disparities among U.S. populations .… These disparities are believed to be the results of the complex interaction among genetic variations, environmental factors, and specific health behaviors.”(47) Interestingly, our data show white residents in the same external environment report 1.6 times the burden of people of color. As in Krieger et al.(46) this result suggests we should look very carefully at how the same contextual determinants of health as well as the structural drivers of poverty are experienced and mitigated by different racial/ethnic groups, and by females and males. “Structural drivers” is the same idea as “root causes” (a term much used in the global health arena), but is more precise in conveying the notion of a system structure that needs to be understood, has inertia, but could be changed in potentially transformative ways.
Assuming exposure to the same stress level on average, the ethnic disparity could be explained by: (i) underreporting by respondents of color less willing to share health information with strangers (though not perceived by our multiethnic interviewers), (ii) overreporting by whites; (iii) differential sociocultural construction/perception of health/disease between whites and people of color (medical anthropology perspective), and/or (iv) greater social adaptation among people of color who belong to neighborhood groups. The same level of stress may elicit higher responses among whites because of higher social isolation; isolation provides positive feedback to other psychosocial stressors. Racial explanations of health disparity have been criticized for being imprecise and biologically meaningless.(49,50) Our approach is compatible with more nuanced, contextual deciphering of disparities, although in our pilot we do not provide any definitive answers.
Working with secondary data across Massachusetts and Rhode Island, Krieger et al.(46) found that among white, black, and Latino women and men, indicators of poverty at the census tract scale were the best predictors of spatial health disparities and gradients. Study scale is fundamental: we worked at a household scale to capture data undetectable at the census tract scale. Relevant scales to consider are those at which suspected causes operate, and effects manifest, and they differ, are multiple and overlapping. But results are highly context- and method-specific: working with data from the national population health survey of Canada, Wu and Schimmele(51) found no association between socioeconomic or behavioral differences and racial/ethnic health disparities.
4.3. Risk Perception
Risk perception studies have tended to survey relatively educated groups, like students,(22) or people with time to fill out and return surveys in the mail.(21,52) In Lai and Tao,(52) for instance, 42% had a higher education level and all had previously participated in risk perception surveys. Our target population is very different, and their results are shown in the context of other information about life and health in such places. Arguably, without this wider context, risk perception data have less power to understand complex vulnerability or inform action to reduce it.
4.4. Vulnerability Index
Our pilot effort showed that a household-scale index of locational vulnerability can be practical to construct and to assign values; it may be useful in exploring determinants of health, although more work is needed to refine the index. Unlike other work on indices,(53–55) the project used primary data from a survey as well as the secondary data normally used.
4.5. Practicality and Usefulness
How can these pilot findings be used by stakeholders? For residents and resident groups, they are already being used to create an information resource, and a political resource to advocate for changes in practice, and policy. For health-care providers they can help by matching responses to local needs, and for public agencies at local, state, and federal levels, they can be used to inform strategic responses and resource allocation. For scientists, our results contribute knowledge, and help develop methods. To improve access to the full range of our findings, we are developing a project website with text, maps, tables, and figures (see Neighborhood-STRENGTH.org). We see the potential for positive change in our neighborhoods, and that this process must begin with dialogue among stakeholders about the most pressing problems and alternative ways to solve them, one that is informed and stimulated by our findings and those of others. Making sure that results are accessible and communicated to the diverse stakeholder community is a priority and the joint responsibility of research partners. Developing and maintaining this information resource and stimulating ongoing dialogue and participatory planning requires a long-term commitment to CBPR work.
Partnerships among stakeholders—residents-at-risk, scientists, community groups, and public agencies—can enable such data collection and interpretation, and strengthen their influence on local policies, practices, and behaviors. But such partnerships are challenging too and must be carefully crafted. In the pilot, our challenges centered on persistent tensions between research goals of the university and action goals of community partners. The survey work became contentious because the university wanted to gather data while one community partner felt problems were known and action was overdue. Unfortunately, tensions between research and action goals grew. In hindsight, we consider funding the formation of local community-university “connectors” who represent the target population essential for the full potential of CBPR approaches to be realized. In essence, the challenge for community-based science is to build authentic, empowering partnerships among scientists, residents-at-risk, and community groups.(56,57) They must both reflect community concerns (ours did) and literally “wear the face of the community” (ours did not). Success also depends on clear achievable goals, sufficient funding, favorable political climate, and positive media attention.(58)
Despite difficulties, we are having sustained impact. Findings inform our new “National Children’s Study—Worcester County” partnership with University of Massachusetts Medical School, county residents, local agencies, hospitals, and Massachusetts Department of Public Health. The partners continue to participate in the Worcester Lead Action Collaborative, a multistakeholder group our project helped start in 2005 to target the priority of childhood lead poisoning prevention. The Collaborative received a large grant from the U.S. Department of Housing and Urban Development in 2007 for strategic lead abatement that targets vulnerable residents.
4.6. Limitations
The main limitation was the size of the household sample (n = 80), which limits the degree to which we can claim it is representative and results can be generalized. That said, the characteristics of the sample do seem to be illustrative of conditions and the sociodemographic data reasonably representative of local people, according to discussions among the partners and others who know the city well. Low yield was in part a function of the very marginalization we sought to understand, but also of limited community organizing capacity among project partners. Learning from the pilot, new funding has been found to build this capacity, now considered a priority.
4.7. Implications and Future Developments
What are the implications of our pilot findings for environmental health science, research practice, and policy? They do not fit easily into a context of environmental regulation that focuses on particular chemical exposures that produce individual lifetime excess cancer risks of 10−4–10−6. In that context there is a useful and energetic dialogue emerging about shifting burdens of “proof” away from vulnerable people to prove polluters do cause health risks, and towards polluters to prove they do not and about differing levels of “proof” and weights/qualities of evidence that are appropriate for different situations.(59) Nevertheless, given the multiple-stressor reality of built environments and our pilot psychosocial findings and those of others, we argue such a focus is likely still too narrow; interactions among stressors can still be ignored, as can be the implications of multiple burdens. From our perspective participatory work must pay more attention to the most vulnerable, marginalized populations, not just those who are accessible, and build the capacity to engage with them. In ongoing and future research we are focusing attention on those who are most vulnerable within marginalized populations, especially children, women, and those who are isolated. It is important to better understand the nature of intragroup and intergroup differences in perceptions, stressors, adaptations, and health burdens. The work reported herein is directly informing our collaborative research for the “National Children’s Study–Worcester County,”(60) part of a 21-year nationwide study of how environmental and socio-demographic variations are associated with variations in the health and development of children, and the health of mothers.(61) Holistic CBPR approaches are, however, resource intensive, difficult, and without due care become more burdensome than conventional assessment. How we develop new participatory data-gathering methodologies to reveal the nature of environmental health vulnerability and its systemic, structural drivers—the “root causes”—will remain a priority. We need efficient methods that rank problems, a form of environmental health triaging; dominant stressors, outcomes, and drivers become the focus of strategic science and policy, keeping resource and data needs reasonable.
5. CONCLUSIONS
Globally, stressful built environments are the fastest-growing human habitat, and marginalized people within these environments are particularly vulnerable. This powerful trend calls for the development of efficient integrative, participatory vulnerability assessment approaches that identify sources and drivers of dominant stressors, and strategic planning to address them. The creation, implementation, and interpretation of the vulnerability questionnaire described above should be considered as one of several pieces of an action-oriented research effort. Valuable lessons we learned from some of the difficulties in our pilot implementation include: community-based participatory research (CBPR) approaches should actively engage with marginalized populations; there is a need for representatives as funded partners to act as researcher-community “connectors” who can help build dialogue and trust; for momentum and early impact, community-university partnerships should convene a critical mass of ready-to-go activities that blend action-oriented research (like the work herein) with action that is research-informed (like health outreach) and meets local needs.
The revealed complexity of the stressor/outcome system and the diversity in population concerns and vulnerabilities necessitate holistic approaches both in assessment and in devising appropriate policies. Environmental and other health impacts must be considered against a backdrop that includes a diverse range of social and physical stressors, a multiplicity of existing health burdens, and diversity in coping capabilities. Any focus on concerns about single risk agents or diseases that neglects such background is likely to miss the mark. The richer context of life, stress, and health revealed informs, and is informed by, risk perception results.
Multifaceted community-based research approaches are demanding in resources, especially time, but critical information can be gained in no other way; developing appropriate efficiencies that respect complexity but limit resource demands is a vital area for development. Once seed capacity has been built at community and institutional levels, and benefits demonstrated, cost effectiveness can improve. Above all, by tackling drivers of disease and preventing chronic, cumulative burdens, we have a greater chance of: (a) stemming the burgeoning direct and indirect societal costs threatening to overwhelm our neighbors and our institutions, and (b) dismantling systemic vulnerability and securing healthier places for people to live and flourish.
ACKNOWLEDGMENTS
We thank the residents of Main South/Piedmont for their hospitality. Work was supported by National Institutes of Health/National Institute of Environmental Health Science (NIH/NIEHS) Program “Environmental Justice—Partnerships for Communication” Grant IR25ES013210. Support for student work was also provided by the Albert Schweitzer Fellowship Program, Worcester Chapter.
APPENDIX: VULNERABILITY QUESTIONNAIRE DESIGN
Shows types and sequence of questions
I. Demographic Data
Family ID code, interviewer’s initials, note-taker’s initials, data, start time, respondent male or female
What do you like about living in this neighborhood? How have things changed in the area since you have lived here? How many times have you moved in the last year?
Why did you move into this apartment or house? How many people live in your house?
Household members: age, gender, relationship to respondent, how long they have lived in the area.
How would you describe your ethnicity/ancestry? What language do you speak most often at home?
II. Local Knowledge, Concerns, and Resources
Currently are you part of any neighborhood groups or clubs? Which ones? What do you get out of belonging to these groups? Would you be interested in getting involved with a neighborhood group to improve the neighborhood? What type?
What problem in the neighborhood worries you most? How do you deal with it? What additional resources would you like to see to help you deal with it? What is the one thing you think would make the most difference in the neighborhood? Have you noticed sources of pollution? What types, and where? [map]
Are you concerned about any particular lots or abandoned buildings? Where are they? [map]
Do you feel safe and secure living in your home? What makes you feel safe or unsafe?
Public services: Please rate the quality of the following public services, and tell us how the quality has changed since you have lived here: sidewalks, fire service, health service, drinking water, library services, activities for youth, trash pick-up, recycling, bus service, policing.
How much would you be willing to pay per month to make sure your streets were trash-free? Have you participated in a street clean-up in the past year? What would encourage you?
III. Time-Activity Patterns
How many functioning cars does the household have? What two main ways do members travel to shop and run errands? How much do you think the household spends on taxis, buses, trains per week? Outside of the home or workplace, what three places do you spend most time in the neighborhood?
Using same household member sequence as before, list their hours on a bus/day, hours outside/day in summer, hours outside/day winter.
IV. Health Information
What would you say is your biggest health concern for you or your family? Why is this a concern? Where do you go for help? (Repeat for 2nd and 3rd concerns)
Please tell me if you or any of the people who live in your household suffer from the following conditions now, or have suffered from them in the past.” [Table VI].
Has anyone suffered from any injuries in the past year? What type? Which illnesses or injuries do you think are the result of your current or previous job? To your knowledge is your home de-leaded? Have your children been tested for lead by a doctor?
Do you have any kind of health coverage? What kind? How do you pay for prescriptions? Do other members have coverage? Who do you speak with most about your health concerns? When was the last time you visited a doctor, nurse or other health professional? Which of the three types of health care facilities in Worcester do you use? How easy is it for you and your household to get health care?
V. Risk and Stress Perception
What are your three biggest sources of stress at home? What are your three biggest sources of stress at work? What are your two biggest sources of stress in the neighborhood?
We asked about 14 hazards: lead in drinking water; lead in soil/dust; air pollution indoors, air pollution outdoors; trash and illegal dumping; cigarette smoke; alcohol; motor vehicle accidents in the area; violence in the area; crime in the area; job loss in the area; pesticides; drugs in the area; terrorism. For each we asked: How much do you know about “X”? How new is X for your community? How easily can X be controlled? How serious are the effects of X? How likely are you to come into contact with X? [psychometric on a Likert 1–5 scale]
Please circle the three things you are most concerned about on this list of 21 things (14 above plus: chemicals in cleaning products; side-effects of prescription drugs; police relations; nutrition; noise in the area; handguns in the community; other).
VI. Existing Capacity and Resources
Income and Education
Please indicate your income level after taxes. Do you pay rent? How much? Is everyone over 10 years old able to read and write? Where do you find information about what’s going on in the community? Where do you find information about health care and health problems? Who knows how to use the Internet? Do you have a computer at home? Is there anyone who does not speak English? Is there anyone who does not write English? What is the highest grade or year of schooling you have completed?
Exercise
How many hours a week do you spend in active or heavy exercise? What do you do? Where? (repeat for other members). Does anything prevent you from participating in physical exercise? What? What is your height and weight?
Closing
What would you like to see us do with this study? Would you like us to test your home for pollution? Would you like to stay involved, be notified of community meetings, or chances to get involved in neighborhood issues?
REFERENCES
- 1.UNPF (United Nations Population Fund) [Accessed on 05/2008];State of World Population: Unleashing the potential of urban growth. 2007 http://www.unfpa.org/swp/2007/presskit/pdf/sowp2007_eng.pdf.
- 2.NIH. Conference Proceedings: Built Environment—Healthy Communities, Healthy Homes, Healthy People: Multilevel, Interdisciplinary Research Approaches, 15–16 July 2002 in Research Triangle Park, NC. Co-sponsored by the NIEHS and the NIH Office of Behavioral and Social Sciences Research and Office of Rare Diseases. [Google Scholar]
- 3.Krieger J, Higgins DL. Housing and health: Time again for public health action. American Journal of Public Health. 2002;92(5):758–768. doi: 10.2105/ajph.92.5.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.USHHS (U.S. Department of Health and Human Services) Healthy People 2010. Washington, DC: U.S. Government Printing Office; With Understanding and Improving Health and Objectives for Improving Health. 2 vols. (2nd ed.) 2000 November; 2000.
- 5.Downs TJ, Ross L, Patton S, Rulnick S, Sinha D, et al. Complexities of holistic community-based participatory research for a low-income, multi-ethnic population exposed to multiple built-environment stressors in Worcester, Massachusetts. Environmental Research. 2009;109:1028–1040. doi: 10.1016/j.envres.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Census 2000. [Accessed on 04/2008];US Census 2000. Available at: http://www.census.gov/main/www/cen2000.html.
- 7.RKG Associates. Massachusetts: City of Worcester; 2002. Housing Market Study. 9/4/02. Unpublished report. [Google Scholar]
- 8.Worcester City. [Accessed 05/08];Crime rates for 1999–2000. 2003 http://www.ci.worcester.ma.us/cau/ncs/ncs.htm.
- 9.Minkler M, Wallerstein N. Community Based Participatory Research for Health. San Francisco: Jossey-Bass; 2003. [Google Scholar]
- 10.Fawcett S, Paine-Andrews A, Francisco VT, Schultz JA, Richter KP, Lewis RK, Williams EL, Harris KJ, Berkley JY, Fisher JL, Lopez CM. Using empowerment theory in collaborative partnership for community health and development. American Journal of Community Psychology. 1995;23(5):677–697. doi: 10.1007/BF02506987. [DOI] [PubMed] [Google Scholar]
- 11.Israel BA, Schultz AJ, Parker EA, Becket AB. Review of community based research: Assessing partnership approaches to improve public health. Ann Review of Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 12.Lebel J. Health: An Ecosystem Approach. Ottawa, Canada: International Development Research Center; 2003. [Google Scholar]
- 13.Downs TJ. A systematic, integrated approach for crafting poverty reduction and sustainable development projects. Natural Resources Forum. 2007;31:35–50. [Google Scholar]
- 14.Ahmad QK, et al. Summary for policy makers. In: McCarthy JJ, Canziani OF, Leary NA, Dokken DJ, White KS, editors. Climate Change 2001: Impacts, Adaptation and Vulnerability. Contribution of the Working Group II to the Third Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, UK: 2001. [Google Scholar]
- 15.NEJAC/EPA. Report developed from the National Environmental Justice Advisory Council Meeting of April 13–16, 2004. Washington, DC: USEPA; Ensuring Risk Reduction in Communities with Multiple Stressors: Environmental Justice and Cumulative Risks/Impacts. [Google Scholar]
- 16.Forster R, editor. Workshop documentation. GTZ. 1996. [Accessed 02/2010]. ZOPP marries PRA: Participatory learning and action—A challenge for our services and institutions. Available online at: http://www.gtz.de/de/dokumente/en-SVMP-forster-1996.pdf. [Google Scholar]
- 17.MIT. [Accessed 02/2010];Interactive Community Planning: ZOPP: Goal Oriented Project Planning. Available at: http://web.mit.edu/urbanupgrading/upgrading/issues-tools/tools/ZOPP.html.
- 18.Ross L, Downs TJ, Tejani A, Dezan R, Lowe K. Trust, preparation, transparency, and reflection: Negotiating roles in youth-adult partnerships for social and environmental justice. In: Linds W, Goulet L, Samme A, editors. Emancipatory Practices: Adult/Youth Engagement for Social and Environmental Justice. Rotterdam, Netherlands: Sense Publishers; [Accepted 09/2009/slated 04/2010]. [Google Scholar]
- 19.Ross L, Farley J. Unpublished Report. Worcester, MA: IDCE, Clark University; 2003. Preliminary Participatory Action Research (PAR) Findings for Piedmont & Main South. [Google Scholar]
- 20.McDaniels T, Axelrod LJ, Slovic P. Perceived ecological risks of global change. Global Environmental Change. 1995;6:159–171. [Google Scholar]
- 21.Fischoff B, Slovic P, Lichtenstein S, Read S, Combs B. How safe is safe enough? A psychometric study of attitudes towards technological risks and benefits. In: Slovic P, editor. The Perception of Risk. Sterling, VA: Earthscan Publications; 2000. [Google Scholar]
- 22.Slovic P, Fischoff B, Lichtenstein S. Facts and fears: Understanding perceived risks—Extended study of risk perception. In: Slovic P, editor. The Perception of Risk. Sterling, VA: Earth-scan Publications; 2000. [Google Scholar]
- 23.deFur PL, Evans GW, Cohen Hubal EA, Kyle AD, Morello-Frosch RA, Williams DR. Vulnerability as a function of individual and group resources in cumulative risk assessment. Environ Health Perspect. 2007;115(5):817–824. doi: 10.1289/ehp.9332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gee GC, Payne-Sturges DC. Environmental health disparities: A framework integrating psychosocial and environmental concepts. Environmental Health Perspectives. 2004;112(17):1645–1653. doi: 10.1289/ehp.7074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hillemeier MM, Lynch J, Harper S, Casper M. Measuring contextual characteristics for community health. Health Serv Res. 2003;38(6-part 2):1645–1718. doi: 10.1111/j.1475-6773.2003.00198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pickett KE, Pearl M. Multilevel analyses of neighbour-hood socioeconomic context and health outcomes: A critical review. Journal of Epidemiology and Community Health. 2001;55(2):111–122. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Macintyre S, Ellaway A, Cummins S. Place effects on health: How can we conceptualise, operationalise and measure Them? Social Science and Medicine. 2002;55(1):125–139. doi: 10.1016/s0277-9536(01)00214-3. [DOI] [PubMed] [Google Scholar]
- 28.Kaplan GA, Lynch JW. Whither studies on the socioeconomic foundations of population health? American Journal of Public Health. 1997;87(9):1409–1411. doi: 10.2105/ajph.87.9.1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yen IH, Syme SL. The social environment and health: A discussion of the epidemiologic literature.”. Annals Review of Public Health. 1999;20:287–308. doi: 10.1146/annurev.publhealth.20.1.287. [DOI] [PubMed] [Google Scholar]
- 30.Marmot M, Wilkinson RG, editors. Social Determinants of Health. 2nd Edn. Oxford, UK: Oxford University Press; 2006. [Google Scholar]
- 31.WHO. Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health. [Accessed 02/2010];Geneva: WHO; Commission on Social Determinants of Health—Final Report. Marmot M. (Chair) 2008 doi: 10.1016/S0140-6736(08)61690-6. Available at: http://www.who.int/social_determinants/thecommission/finalreport/en/index.html. [DOI] [PubMed]
- 32.Williams DR, Sternthal M, Wright RJ. Social determinants: Taking the social context of asthma seriously. Pediatrics. 2009;123 Suppl 3:S174–S184. doi: 10.1542/peds.2008-2233H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Williams DR, Costa MV, Odunlami AO, Mohammed SA. Moving upstream: How interventions that address the social determinants of health can improve health and reduce disparities. Journal of Public Health Managment Practices. 2008;14 Suppl:S8–S17. doi: 10.1097/01.PHH.0000338382.36695.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McEwen BS. Protective and damaging effects of stress mediators. New England Journal of Medicine. 1998;338:171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 35.Steptoe A, Feldman PA. Neighborhood problems as sources of chronic stress: Development of a measure of neighborhood problems and associations with socioeconomic status and health. Annals of Behavioral Medicine. 2001;23:177–185. doi: 10.1207/S15324796ABM2303_5. [DOI] [PubMed] [Google Scholar]
- 36.Morenoff JD. Neighborhood mechanisms and the spatial dynamics of birth weight. American Journal of Sociology. 2003;108:976–1017. doi: 10.1086/374405. [DOI] [PubMed] [Google Scholar]
- 37.CDC. [Accessed 05/2008];Centers for Disease Control and Prevention. National Center for Health Statistics. Data and Statistics. http://www.cdc.gov/datastatistics/, Accessed 12/2008. http://www.cdc.gov/nchs/fastats/deaths.htm.
- 38.NHIS (National Health Interview Survey) [Accessed 0815//09];Asthma and chronic obstructive pulmonary disease: US, 1999–2007. 2008 Available at: http://205.207.175.93/HDI/TableViewer/summary.aspx.
- 39.Ogden CL, Carroll MD, McDowell MA, Flegal KM. NCHS data brief no 1. Hyattsville, MD: National Center for Health Statistics; 2007. Obesity among adults in the United States–no change since 2003–2004. [PubMed] [Google Scholar]
- 40.Massachusetts Division of Health Care Finance and Policy and the Urban Institute. [Accessed 02/2010];Health Insurance Coverage in Massachusetts: Estimates from the 2008 Massachusetts Health Insurance Survey. 2008 December; Presentation available at: http://www.mass.gov.
- 41.Gibbons MC. A historical overview of health disparities and the potential of eHealth solutions. Medical Internet Research. 2005;7(5):e50. doi: 10.2196/jmir.7.5.e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Carter-Pokras O, Baquet C. What is a “health disparity”? Public Health Report. 2002;117(5):426–434. doi: 10.1093/phr/117.5.426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Inhorn M, Whittle KL. Feminism meets the new epidemiologies: Toward an appraisal of antifeminist biases in epidemiological research on women's health. Social Science and Medicine. 2001;53:553–567. doi: 10.1016/s0277-9536(00)00360-9. [DOI] [PubMed] [Google Scholar]
- 44.Krieger N, Fee E. Man-made medicine and women’s health: The biopolitics of sex/gender and race/ethnicity. In: Fee, Krieger, editors. Women’s Health, Politics and Power: Essays on Sex/Gender, Medicine, and Public Health. New York: Baywood Publishing Company; 1994. [Google Scholar]
- 45.McGrath BB, Puzan E. Gender disparities in health: Attending to the particulars. Nursing Clinics of North America. 2004;39(1):37–51. doi: 10.1016/j.cnur.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 46.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: A comparison of area-based socioeconomic measures–the Public Health Disparities Geocoding Project. American Journal of Public Health. 2003;93(10):1655–1671. doi: 10.2105/ajph.93.10.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.CDC/OMHD (Center for Disease Control and Prevention/Office of Minority Health and Health Disparities) [Accessed 05/2008];Eliminating racial and ethnic health disparities: Disease burden and risk factors. 2008 http://www.cdc.gov/omhd/AMH/dbrf.htm.
- 48.Brugge D, et al. Community-level data suggest that asthma prevalence varies between U.S. and foreign-born black sub-populations. Journal of Asthma. 2008;45(9):785. doi: 10.1080/02770900802179957. [DOI] [PubMed] [Google Scholar]
- 49.Anderson NB, Nickerson KJ. Genes, race, and psychology in the genome era: An introduction. American Journal of Psychology. 2005;60(1):5–8. doi: 10.1037/0003-066X.60.1.5. [DOI] [PubMed] [Google Scholar]
- 50.Smedley A, Smedley BD. Race as biology is fiction, racism as a social problem is real: Anthropological and historical perspectives on the social construction of race. American Journal of Psychology. 2005;60(1):16–26. doi: 10.1037/0003-066X.60.1.16. [DOI] [PubMed] [Google Scholar]
- 51.Wu Z, Schimmele CM. Racial/ethnic variation in functional and self-reported health. American Journal of Public Health, 2005. 2005;95(4):710–716. doi: 10.2105/AJPH.2003.027110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lai JC, Tao J. Perception of environmental hazards in Hong Kong Chinese. Risk Analysis. 2003;23:669–683. doi: 10.1111/1539-6924.00346. [DOI] [PubMed] [Google Scholar]
- 53.Faber DR, Krieg EJ. Unequal Exposure to Ecological Hazards: Environmental Injustice in the Commonwealth of Massachusetts. [released January 9, 2001];A report by the philanthropy and environmental justice research project Northeastern University. doi: 10.1289/ehp.02110s2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cutter SL, Boruff BJ, Shirley LW. Social vulnerability to environmental hazards. Social Science Quarterly. 2003;84(2):242. [Google Scholar]
- 55.Ewart C, Suchday S. Discovering how urban poverty and violence affect health: Development and validation of a neighborhood stress index. Health Psychology. 2002;21(3):254–262. doi: 10.1037//0278-6133.21.3.254. [DOI] [PubMed] [Google Scholar]
- 56.Agyeman J. Where justice and sustainability meet: Alternatives for community and environment. Environment. 2005;47(6):10–14. [Google Scholar]
- 57.Chao K, Long S. Youth participation in research: Weighing the benefits and challenges of partnerships. Race, Poverty and the Environment. 2004/2005 Winter [Google Scholar]
- 58.Petersen D, Minkler M, Breckwith Vasquez V, Corage Baden A. Community-based participatory research as a tool for policy change: A case study of the Southern California Environmental Justice Collaborative. Review of Policy Research. 2006;23(2) [Google Scholar]
- 59.NIEHS EJ/CBPR. Discussion break-out session. Annual Grantee Meeting for Environmental Justice/Community Based Participatory Research; Boston, MA. 2007. Oct, [Google Scholar]
- 60.Downs TJ, Ogneva-Himmelberger Y, Aupont O, Wang Y, Raj A, Zimmerman P, et al. Vulnerability-based spatial sampling stratification for the National Children’s Study-Worcester County, Massachusetts: Capturing environmental and socio-demographic variability. Environmental Health Perspectives. 2010;18(9):1318–1325. doi: 10.1289/ehp.0901315. DOI information: 10.1289/ehp.0901315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.NCS. [Accessed March 2009];2009 Website: http://www.nationalchildrensstudy.gov/