Abstract
Objective
The Teaching, Raising, And Communicating with Kids (TRACK) program was a longitudinal pilot-trial intervention designed to assist mothers living with HIV (MLH) to disclose their serostatus to their young children (age 6 – 12 years).
Method
MLH and child dyads (N = 80 dyads) were recruited and randomized to intervention or control; the intervention group had three individual sessions and one follow-up phone call. The sessions focused on preparing MLH for disclosure through behavioral exercises utilizing Derlaga’s model of HIV-disclosure. Both MLH and their child were assessed across multiple time-points (baseline, 3-, 6-, and 9-months) regarding disclosure of HIV status, and specific outcome variables (i.e., relationship context, mother’s health, child’s mental health, and family outcomes).
Results
MLH in the intervention group were six times more likely to disclose their HIV status than those in the control group (O.R. 6.33, 95% C.I.: 1.64 – 24.45), with 33% disclosing in the intervention group compared to 7.3% in the control group. MLHs in the intervention group showed increases in disclosure self-efficacy across time, increased communication with their child, and improvement in emotional functioning. Children of MLHs in the intervention group exhibited reductions in depression and anxiety, and increases in happiness.
Conclusions
TRACK was found to be successful in helping MLH disclose their HIV status to their children, with positive outcomes noted for both MLH and their children.
Keywords: HIV, mothers, intervention, disclosure
An estimated 33 million people were living with HIV in 2007 (UNAIDS, 2008). Women account for half of all people living with HIV, and this percentage has remained stable for the past several years. Thus, women are one of the groups now at the forefront of HIV, and are most often the primary caregivers in families (Weiner, Battles, & Heilman, 1998). An HIV diagnosis impacts not only mothers as individuals, but also affects how they care for their families (Schmidt & Goggin, 2002).
Many mothers choose not to tell their young children about their HIV-positive status. However, not disclosing can negatively impact mothers’ physical and psychological functioning. For example, mothers living with HIV (MLHs) who had not disclosed reported sometimes skipping medications because they are afraid their children will observe them and suspect something is wrong, and were more likely to miss medical appointments (Mellins et al., 2002; Murphy, Steers, & Dello Stritto, 2001). Another study found disclosure related to improved well-being, particularly when the first-disclosure experience was positive, which may lessen fear of future disclosure (Chaudoir & Quinn, 2010).
Many MLH report that they choose not to disclose for fear of burdening their children (e.g., Palin et al., 2009). However, nondisclosure is no guarantee of positive child outcomes. One study found that adolescents who are not informed about their mothers’ HIV status can be left with feelings of resentment, and broken trust and anger because they were unable to address their parent’s illness openly, express their feelings, ask questions, and receive direct answers (Wood, Chase, & Aggleton, 2006). Among younger children whose mothers have chosen not to disclose, research indicates elevated levels of anxiety (Forsyth, Damour, Nagler, & Adnopoz, 1996; Murphy, Kaufman, & Swendeman, 1998), perhaps due to guilt they feel for a disordered family environment whose source they cannot identify. Children who found out their mothers’ serostatus report they knew something was wrong but felt unable to ask about the cause (Nagler, Adnopoz, & Forsyth, 1995). Women who had known their diagnoses longer were more likely to have children who were aware of their illness (Kirshenbaum & Nevid, 2002),
For MLH who do disclose to their young children, two findings have been fairly consistent: They are less likely to disclose to younger children and more likely to disclose to female children (e.g., Armistead, Tannenbaum, Forehand, Morse, & Morse, 2001; for a full review of factors affecting MLH disclosure, see Murphy, 2008). MLHs who have disclosed report significantly lower levels of depression than mothers who have not disclosed (Wiener et al., 1998), less use of concealment to manage HIV-related stigma, stronger social support (Letteney, 2006), and stronger family cohesion. However, disclosure may cause short-term stress among mothers and children. For example, parents reported their children reacted to their HIV disclosure with depression (39%), and anxiety (11%), although parents reported improved adjustment over time for the majority of children (Nostlinger, Bartoli, Gordillo, Roberfroid, & Colebunders, 2006). This is consistent with findings by Murphy, Roberts, and Hoffman (2006), where most children were upset immediately following disclosure, but the majority adjusted over time.
Whether maternal HIV disclosure may vary by race/ethnicity has been investigated in a number of studies. For example, Tompkins, Henker, Whalen, Axelrod, & Comer (1999) reported children of White and African American mothers were more likely to be aware of the mother's HIV status than were children of Latina women, but suggest this difference may be accounted for, at least in part, by the younger age of the Latino children. Corona et al. (2006) reported more English speaking compared to Spanish speaking parents disclosed their HIV status to their child; however, after controlling for factors including age of child and level of social isolation, language was no longer associated with disclosure. In a sample of predominantly African American and Latina HIV positive women, disclosers and non-disclosers were similar in most sociodemographic characteristics including race, marital status, religion and employment (Letteney & LaPorte, 2004). Other studies have not found ethnicity and/or acculturation to be related to serostatus disclosure (Lettney, 2006; Murphy et al., 2001; Rice, Comulada, Green, Arnold, & Rotheram-Borus, 2009).
The Parents And children Coping Together (PACT) study was designed to longitudinally assess MLHs and their well children age 6 -- 11 years of age. Throughout the course of the study (now in its 13th year), the UCLA research team has investigated maternal disclosure (Murphy, Marelich, & Hoffman, 2002; Murphy et al., 2001). Mothers who disclosed reported higher levels of social support in their lives than non-disclosing mothers. Children of disclosing mothers displayed lower levels of aggressiveness (by mothers report), and lower levels of negative self-esteem (by child report), compared to children of non-disclosing mothers. Across the course of the PACT study, a number of MLH disclosed to their children. An analysis of depression and anxiety scores for the children who were unaware of their mothers serostatus at baseline and who were disclosed to at any of the follow-up points was conducted (Murphy, 2008). Children showed significant improvement on the mental health variables at the assessment following disclosure (which gave them time to adjust potentially if they were immediately distressed by the disclosure). They had significantly fewer depression symptoms and showed a trend for lower anxiety.
To obtain more information about the process and content of maternal disclosure, the PACT research team conducted in-depth, qualitative interviews with mothers (N = 47) and children (N = 41). Overall, 51% of the children had no immediate reaction to their mothers HIV disclosure. The other 49% of the children expressed an emotional reaction. Anxiety was the most common reaction, with children expressing concern about their mother's health and how long she would live. Most of these reactions were short term, however, a few children (N = 7) displayed acting out behavior over time. Thus, most of the children adjusted, but a small percentage had maladaptive reactions that were sustained. The majority of the mothers who disclosed (77%) explicitly told their children not to tell other people (Murphy, Roberts, & Hoffman, 2002). The children understood this, as they were aware of the stigma associated with HIV/AIDS. Very few of the MLHs identified "safe people" with whom their child could talk. Children sworn to secrecy have been shown to demonstrate more externalizing problems and poorer social competence (Tompkins, 2007). Finally, the majority of PACT MLH had no regrets about disclosing (Murphy, Roberts, & Hoffman, 2003). However, many were sorry they had not planned for the event, but, rather, blurted out the news during an emotional time. Mothers deemed it crucial to have a plan for what to say when disclosing. They reported hoping for education to provide them with skills and information so that they would be better able to share appropriately with their children, indicating a need for assistance at this critical time.
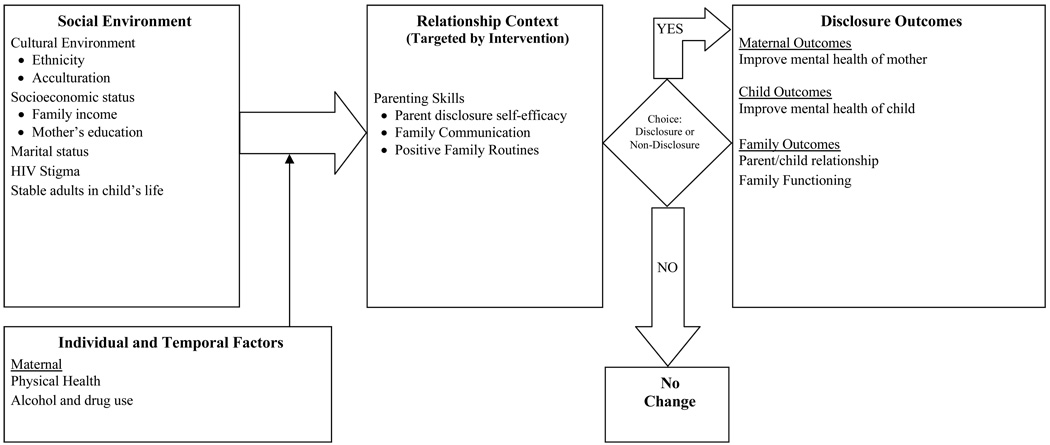
The Teaching, Raising And Communicating with Kids (TRACK) pilot intervention was developed based on the quantitative and qualitative disclosure studies conducted during Murphy's PACT study. Derlega et al.’s (2004) Model of HIV-Disclosure provided a conceptual framework for studying self-disclosure decisions and outcomes, which for TRACK was applied to the family context. The first factor in the model is the social environment in which the MLH and child live; the second factor focuses on individual, temporal, and relational contexts. These factors affect the endorsement of reasons for and against disclosure, which then leads to disclosure outcomes for both the mother and child. Consistent with family system theory (e.g., Alexander, Sexton, & Robbins, 2002), the intervention targets the relationship context, including intrafamilial communication and parenting skills, specifically as they apply to disclosure. By significantly improving parent skills and self-efficacy in these areas, the intervention was expected to increase steps toward disclosure and disclosure itself, as well as positively affect outcomes associated with disclosure (i.e., mother and child functioning). Thus, for all of the intervention MLHs, we anticipated improving relationship context variables (Figure 1, middle box) and the disclosure outcomes for those mothers who chose to disclose. This small pilot study focuses on the changes in the relationship context variables and the disclosure outcomes (Figure 1, last box) from the model. The specific aims of the intervention were to: (1) enhance family communication and parenting skills specific to disclosure; (2) increase readiness to disclose HIV serostatus, and increase disclosure itself (primary outcome); (3) improve MLH mental-health indicators over time (it was anticipated that MLH anxiety and depression scores might be poorer immediately following disclosure but that these would decrease over time); (4) improve child mental health indicators over time (it was anticipated that child depression, anxiety, and self-concept may actually be poorer around the time of disclosure, but would improve over time); and (5) improve the parent-child relationship and family functioning.
Figure 1.
Conceptual Diagram of Proposed Intervention Effects for Maternal HIV Disclosure (Based on Integrative Disclosure Theory; Derlega, Winstead, Greene, Serovich, & Elwood, 2004)
Method
Participants
MLH-child dyads (N = 80 dyads; 80 MLH and 80 children) were recruited through HIV/AIDS service organizations in Los Angeles County. Inclusion criteria were that the mother was diagnosed HIV+, spoke English or Spanish, had a well 6 – 12 year-old child living with her who was unaware of the mother’s serostatus, and the mother had no intention of disclosing to the child. Sixty percent of MLH who were screened were eligible for participation.
Enrolled mother/child pairs were interviewed at baseline and at 3, 6, and 9-month follow-ups. Approximately half (49%) of the mothers were randomly assigned to receive the 3-session intervention in addition to their standard care (e.g., medical care and case management); the remaining 51% served as the control condition and received standard care only.
Children’s mean age at baseline was 8.7 years (SD = 2.0), and mother’s mean age at baseline was 37.4 years (SD = 6.8). The racial/ethnic composition of the total enrolled sample, including both mothers and children, was 18% African-American/Black, 79% Latino/Hispanic, and 1% of mixed racial/ethnic background: 70% of the mothers were Spanish speaking only. Fifty-one percent of the MLH had less than 9 years of education, 36% had 9 – 12 years education, and 13% had some college or a college degree. Only 25% of the MLH were married. At the baseline interview, MLH reported having been diagnosed with HIV for an average of 10.6 years.
Given that participation typically lasted almost a year, attrition in the sample was expected; 85%, 81%, and 81% of the participants completed the 3-month, 6-month, and 9-month follow-ups, respectively. A small percent (2.5%) could not be located for any follow up interview. The reasons for attrition were as follows: illness or death of the mother, loss of custody of child, inability to locate, or participant refusal. No association was found between number of completed follow-up appointments and group assignment (intervention vs. control; χ2 [3] = 2.84, n.s.), mother’s age, F(3, 76) = 0.69 (n.s.), age of child, F(3,76) = 2.54 (n.s.), or mother’s educational level, F(3,76) = 2.09 (n.s.).
Procedures
All procedures were approved by UCLA’s Institutional Review Board. Recruitment sites displayed English and Spanish language flyers and brochures in waiting rooms, distributed these materials to potentially eligible mothers, and/or obtained verbal permission for UCLA interviewers to contact potential participants. MLH informed consent and the child’s assent were obtained prior to participation.
On most occasions, intervention and interview appointments were conducted in the mother’s home unless the mother chose a different location such as her treating clinic. Mother and child interviews were conducted in separate rooms to ensure confidentiality. Interviews were administered using a computer-assisted interviewing program on laptops. MLH interviews typically took 75 minutes, and child interviews typically took 60 minutes. Interviews were recorded for quality-assurance purposes. Spanish-speaking mothers were administered the interviews in Spanish by a trained bilingual interviewer. Prior to the child’s interview, the mothers were asked about their child’s language preference; all child interviews were conducted in English, as the mothers reported their children either preferred to conduct the interview in English, or were equally comfortable with English or Spanish. Interviewers were blind to group assignment. Interviewers never discussed the HIV diagnosis with the children; the project was presented as a study of parent-child communication. Immediately after each completed appointment, mothers were paid $45 for each interview and $45 for each intervention session, and children were allowed to select a toy or toys worth approximately $25 or a retail gift card worth $25. Intervention sessions were typically completed during school hours, unless another time was requested, and sessions were typically 50 to 75 minutes long.
All study documents, including the intervention manual, handouts and assessments, were professionally translated and back-translated by the Worldwide Translation Center (WTC) in San Diego, CA. The American Translators Association accredits WTC translators, and staff translates only into their native language. For quality assurance, a team of three handles all documents: a professional translator; an editor for accuracy of translation and grammar; and an additional editor for style. A blind back-translation is conducted by a separate translator at UCLA, using procedures described by Marin and Marin (1991).
Intervention
At the time a family was deemed eligible to participate in the study, MLH were randomly assigned to the intervention (n = 39) or control condition (n = 41). Intervention sessions took place within 1 – 3 weeks of the baseline appointment (M = 15 days) and were spaced approximately 1 week apart (M = 10 days). The vast majority (95%) of the mothers assigned to the intervention condition completed all 3 sessions.
A brief review of the intervention is provided here. Session 1 addressed children’s typical development (including at what age they are able to keep secrets, age-appropriate chores and self-care skills, and social development); pros and cons of disclosure; and improving family routines as a foundation for disclosure. Session 2 focused on improving mother-child communication, including a self-evaluation of the mother’s communication strengths and weaknesses; advice and quotes from other mothers on disclosure; quotes from children on their own reactions to disclosure, noting developmental age of each child reaction; and disclosure preparedness. Session 3 included behavioral practice for disclosure, during which the facilitator role-played the child; a self-evaluation of the disclosure role-play exercise; and information on issues to address after disclosure. This last session closed with a final discussion on disclosure readiness and positive reinforcement from the facilitator.
Measures
Disclosure
In the baseline assessment, the interviewer confirmed that mothers had not yet disclosed to the target child. MLH were then asked about their reasons for not disclosing and disclosure experiences with other children in the family, such as reactions to the disclosure. At baseline, mothers also completed a Disclosure Self-Efficacy scale, which was developed specifically for this study (described below). At each follow up, the mother was asked whether she had disclosed to the child that she is HIV-positive. If the mother had not disclosed, the above baseline information was collected again. If the mother had disclosed, information was collected on the disclosure, including the date of the disclosure, the child’s reactions to the disclosure and how the mother felt she handled the disclosure.
MLH feelings about they handled the disclosure and child response to disclosure
Information was collected on how MLH in the intervention group felt after they disclosed their HIV status to their child, with mother’s asked to rate six statements on a five-point scale (1 = Strong Agree; 5 = Strongly Disagree; or they could respond “don’t know”). Statements addressed: keeping an appropriate emotional tone during disclosure; feeling prepared to answer questions about HIV transmission; making a list with the child of “safe” people with whom the child could discuss the mother’s HIV status following disclosure; waiting to make the disclosure until the mother was in the right frame of mind; how well the mother handled the disclosure overall; and how the mother handled her child’s reaction to disclosure.
MLH in the intervention group were also asked questions regarding their child’s response to the disclosure. One item asked MLH who disclosed how they felt their child responded to the disclosure on a scale of 1 to 5, with 5 indicating a very positive reaction by the child, and 1 being the “worst response you could have imagined.” MLH also were asked a series of questions as to how the child responded to the disclosure (“yes,” “no,” or “don’t know”), including: crying, being angry, frightened, surprised, the child had already guessed the mother was ill; and the child was glad the mother disclosed to them.
Relationship Context Measures (Targeted by Intervention): Family Communication and Parenting Skills
Disclosure self-efficacy
To assess the mother’s level of confidence in her ability to disclose her HIV status to her child, a nine-item Disclosure Self-efficacy scale was developed for this study. The mother rated how confident she was that she could: decide whether the child is developmentally ready to learn of her HIV status; come up with a plan for how to disclose; come up with an age-appropriate way to explain what HIV is; set a time and date to disclose; disclose to the child; stay calm during disclosure; deal with the child’s emotional response to disclosure; talk to the child about HIV facts; and answer personal questions on HIV. A visual analogue scale, as described in Kalichman et al. (2005), was used to guide respondents in selecting their confidence ratings. Cronbach’s alpha for the scale was 0.90.
Family routines
A subset of 11 questions from The Family Routines Questionnaire (Jensen, James, Boyce, & Hartnett, 1983) was administered to mothers (e.g., “In our family, children go to bed at the same time each night”; “In our family, the whole family eats dinner together”). Higher scores equal more frequent involvement in each family routine. Cronbach’s alpha in this sample was .70.
Parent-child communication
Mothers completed the 10-item parent-adolescent communication scale (Miller, Forehand, & Kotchick, 1999). Higher scores indicate better communication. Items included, “You sometimes don’t listen to [Child],” and, “It is easy for [Child] to discuss all his/her true feelings with you.” Cronbach’s alpha for the current sample was .69.
Coping with child emotions
The Parenting Stress Index (Abidin, 1990) was developed for early identification of stressful parent-child systems and assesses how difficult the mother perceives it is to get her child to do something or stop doing something; and how frequently she is bothered by things the child does. Mothers were asked how strongly they agree or disagree with statements such as, “My child turned out to be more of a problem than I had expected” or “My child makes more demands on me than most children.” Cronbach’s alpha in this sample is 0.89.
Maternal Outcomes
Maternal mental health functioning
The Rand Mental Health Inventory assesses general mental health functioning in the past month (Veit & Ware, 1983). The measure can be scored as three specific subscales of distress (anxiety, depression, and loss of emotional control), and two subscales of well-being, positive affect and emotional ties, and a single item of general satisfaction with life, which assessed how happy, satisfied, or pleased the respondent had been with her personal life, on a 6-point scale ranging from extremely happy to very dissatisfied. We included the depression, anxiety and satisfaction measures. Higher scores indicate higher levels of distress/well-being. For the current sample, Cronbach’s alpha for depression was .81, and for anxiety .86.
Maternal Well-being
The Medical Outcome Study Short Form 36 (MOS SF-36) was administered to the mothers. The three-item subscale addressing role limitations due to emotional problems (i.e., “role-emotional” subscale) was used in this analysis. It assesses the extent to which emotional problems interfere with doing work or other regular daily activities. Cronbach’s alpha for this scale was .86. Higher scores indicate better functioning. The MOS SF-36 has been found to be psychometrically sound and responsive to clinical change over time (Ware, Gandek, and the IQOLA Project Group, 1994).
Child Outcomes
Depression
The Children's Depression Inventory (CDI; Kovacs, 1985; Kovacs & Beck, 1977) was administered to both the mothers and children. The CDI is a widely used, reliable self-report measure of childhood distress and depressive symptomatology (Curry & Craighead, 1993). All subscales were administered to the children (i.e., negative mood, interpersonal problems, ineffectiveness, anhedonia, and negative self-esteem); for this sample, total internal consistency was .82.
Self-concept
The Piers-Harris Children’s Self-Concept Scale was administered to the children. The Piers-Harris scale is a widely used, psychometrically sound self-concept measure designed for children and adolescents (Hughes, 1984; Piers, 1993). The six subscales used in this analysis were the intellectual and school status scale; the popularity scale; the physical appearance and attributes scale; the behavioral adjustment scale; the freedom from anxiety scale; and the happiness and satisfaction scale. Cronbach’s alphas in this sample for each subscale ranged from .60 to .64.
Family Outcomes
Parent-child attachment
The Parent subscale from the Inventory of Parent and Peer Attachment (Armsden & Greenberg, 1987) was used to assess mother-child attachment. The scale was administered to the child (e.g., “I feel my mother does a good job as my mother”; “I wish I had a different mother”). Three subscales (trust, communication, alienation), as well as a global score are calculated; Cronbach’s alphas were .72, .66, .72, and .85, respectively. Higher scores indicate a more secure attachment.
Family cohesion
The family cohesion subscale from the Family Functioning Scale (Bloom & Naar, 1994) was used in this analysis. On five items, MLH rated the degree to which specific family characteristics were ‘like’ her family (e.g., “there is a feeling of togetherness in our family”). Higher scores indicate more family cohesion. Cronbach’s alpha in this sample was .71.
Analyses
A randomized pretest-posttest 2-group design with repeated assessments was implemented. A power analysis was conducted prior to participant recruitment, with a minimum target sample size of 40 per group deemed appropriate for medium to large effects with 80% power. The initial analyses address group (intervention vs. control) descriptives and disclosure. Next, evaluation of change in these outcomes was conducted utilizing simple main effects analysis within repeated measures ANOVA (Jaccard, 1998; Winer, 1971), with paired within-group comparisons to evaluate change over time (Maxwell, 1980). Effect size calculations are also included for these comparisons, using r (Cohen, 1992). To retain cases with missing data across time, analyses were conducted using a mixed-model approach for repeated measures through SAS Proc Mixed (V9.1.3; see Wolfinger & Chang, 1995) with a Kenward-Roger degrees of freedom adjustment per recommendations by Brown and Prescott (2006).
Results
Disclosure
Overall, 16 MLH (20%; 16 of 80) disclosed their HIV status to their child; 13 in the intervention group (33.3%; 13 of 39) and 3 in the control condition (7.3%; 3 of 41). Those in the intervention group were six times more likely to disclose their HIV/AIDS status to their child than those in the control condition (Mantel-Haenszel O.R. 6.33; 95% C.I.: 1.64 – 24.45; r = .33 [a medium effect]). All intervention group disclosures took place after the intervention, primarily near the 3-month follow-up, with 3 mothers disclosing near the 9-month assessment. Of the MLH who disclosed from the control group, the disclosures took place near the 9-month assessment.
Focusing only on the 16 children who were disclosed to across both the intervention and control groups, their average age at baseline assessment was 9.81 years (SD = 1.47), ranging from 7 to 12 years. A goodness of fit χ2 (N = 16) indicated older children were not disclosed to at a greater rate than younger children (χ2 = 6.5, df = 5, p = .26). Gender composition was 10 males and 6 females (binomial test p = .45 indicating no gender preference in disclosure).
Of the MLH who disclosed, 11 were Latina and 5 were African American (binomial test p = .21 indicating no race/ethnicity preference in disclosure), with no association noted between race/ethnicity and whether MLH were in the intervention or control group (Fisher's Exact test p = 1.00). Time since diagnosis for MLH at baseline had no association with disclosure (r = −0.15. n.s.). In looking at the intervention and control groups separately, the gender composition of those disclosed to in the intervention group included seven males and six females, while all three of those disclosed to in the control group were male.
Children in our study who had been disclosed to were compared to children to whom disclosure had not occurred (N = 80): children made aware of their mothers’ serostatus did not differ on gender composition (χ2 = .46, df = 1, p = .50) or race/ethnicity (Cramer’s V = .22, p = .14). After taking group membership into account, an ANCOVA showed no significant difference between disclosure status (disclosed/not disclosed) and baseline age of the child, F(1, 77) = 1.18, p = .28.
Feelings about Disclosures and Child Response
Six items addressed how MLH felt after they disclosed their HIV status to their child. Focusing on those who disclosed from the intervention group only, 12 of the 13 MLH provided responses for each of the items (one responded “don’t know” to all the items). For the statements, “I kept an appropriate emotional tone during the disclosure,” and “I felt prepared to answer any questions about HIV transmission during the disclosure,” 84.6% (11 of 13) either strongly agreed or agreed; 84.6% (11 of 13) strongly agreed or agreed with the statement “I felt I handled the disclosure well.” Of the intervention MLH who disclosed, 69.2% (9 of 13) either strongly agreed or agreed with the statement “I waited to disclose until I was in the right frame of mind,” and 69.2% (9 of 13) strongly agreed or agreed with the statement “I felt I handled my child’s reaction to the disclosure well.” For the statement “My child and I together made a list of ‘safe’ people to whom s/he could talk to about my HIV status,” 46.2% (6 of 13) of the MLH either strongly agreed or agreed.
For the item addressing how MLH felt their child responded to the disclosure, 69.2% (9 of 13) noted the child reacted very positively, with another 15.4 % (2 of 13) noting a positive response (none of the mother’s noted the disclosure resulted in the “worst response” imagined). None of the children were described as crying or being angry after disclosure (0 of 13). Over 23% (3 of 13) of the children were reported being “frightened” after the disclosure, and 46.2% (6 of 13) of the children were described as being “surprised.” Over 23% (3 of 13) of the children had already guessed something was wrong with the mother. Overall, 61.5% of the MLH responded “yes” when asked if their child was glad they had disclosed; 30.8% responded they didn’t know; and one mother said “no.”
The three women in the control group who disclosed their serostatus to their child were also assessed using these measures. One mother felt she handled most aspects of the disclosure well, but the child seemed to have already guessed the mother had a health problem. Another mother felt she handled the disclosure well, but the child was reported by the mother as responding poorly to the disclosure.
Additional Intervention Outcomes
A series of simple main effects analyses were used to evaluate change within each group across time, with the grouping variable treated as a moderator (Jaccard, 1998). The repeated measures ANOVA results reported in Table 1 show only the group main effect and simple main effects since these effects comprise the full decomposed ANOVA model. Paired t-tests on the mean estimates across time within each group are then used to assess change across the different time points (Maxwell, 1980). Note that prior to these analyses, groups were compared at baseline for pre-existing differences using independent samples t-tests; no group differences at baseline were noted at the p < .01 level.
Table 1.
Simple main effects Repeated Measures ANOVA Results: Relationship Context, Mother's Mental Health, Child Mental Health, and Family Outcome Variables by Group (Control, Intervention) across time
| Main Effects | Simple Main Effects of Time within Group | |||||
|---|---|---|---|---|---|---|
| Group Main Effect | Control | Intervention | ||||
| F | (df1, df2) | F | (df1, df2) | F | (df1, df2) | |
| Relationship Context (Targeted by Intervention) | ||||||
| Disclosure Self-Efficacy | 4.47* | (1, 78.6) | 1.45 | (3, 57.5) | 4.74** | (3, 55.5) |
| Parent/Child Communication | 2.46 | (1, 73.9) | 0.35 | (3, 65.7) | 0.97 | (3, 62.3) |
| Family Routines | 0.3 | (1, 75.7) | 0.95 | (3, 64.2) | 0.55 | (3, 60.1) |
| Mother’s Mental Health Outcomes | ||||||
| RAND Mental Health Inventory(MHI) | ||||||
| Anxiety | 0 | (1, 78.6) | 0.85 | (3, 66.3) | 1.01 | (3, 62.7) |
| Depression | 0.98 | (1, 78.8) | 0.21 | (3, 69.3) | 0.9 | (3, 65.6) |
| Satisfaction Item | 0.12 | (1, 74.4) | 3.95* | (3, 68.6) | 1.52 | (3, 65.1) |
| Medical Outcome Study Short Form 36 (MOS SF-36) | ||||||
| Role-Emotional | 0.63 | (1, 75.8) | 0.28 | (3, 68.6) | 3.65* | (3, 65.2) |
| Child Outcomes | ||||||
| Child Depression Inventory (CDI) | ||||||
| Total | 0.72 | (1, 74.5) | 3.69* | (3, 64.8) | 10.83*** | (3, 62.5) |
| Negative Self-Esteem | 1.26 | (1, 80.5) | 1.07 | (3, 73.5) | 2.69+ | (3, 71.1) |
| Anhedonia | 0.37 | (3, 73.3) | 2.33+ | (3, 66) | 9.12*** | (3, 63.6) |
| Interpersonal Problems | 0 | (1, 79) | 0.15 | (3, 69) | 6.94*** | (3, 66.8) |
| Ineffectiveness | 1.24 | (1, 71.3) | 0.32 | (3, 60.7) | 3.27* | (3, 58.6) |
| Negative Mood | 0.77 | (1, 75.2) | 5.22** | (3, 66.7) | 4.26** | (3, 64.6) |
| Piers-Harris | ||||||
| Freedom from Anxiety | 1.31 | (1, 76.2) | 1.52 | (3, 67.3) | 3.29* | (3, 64.2) |
| Happiness | 0.86 | (1, 78.7) | 0.45 | (3, 64.4) | 5.32** | (3, 62.4) |
| Family Outcomes | ||||||
| Inventory of Parent and Peer Attachment | ||||||
| Trust | 0.51 | (1, 77.2) | 0.68 | (3, 65.6) | 0.22 | (3, 63.1) |
| Communication | 1.68 | (1, 70.3) | 2.29+ | (3, 66) | 3.47* | (3, 63.2) |
| Alienation | 0.41 | (1, 75.9) | 0.54 | (3, 66.7) | 1.33 | (3, 63.5) |
| Total | 1.11 | (1, 75.8) | 1.25 | (3, 65.9) | 1.69 | (3, 63) |
| Family Cohesion | 1.03 | (1, 79) | 0.32 | (3, 70.1) | 1.97 | (3, 66.7) |
p < .10.
p < .05.
p < .01.
p < .001.
Relationship Context (Targeted by Intervention)
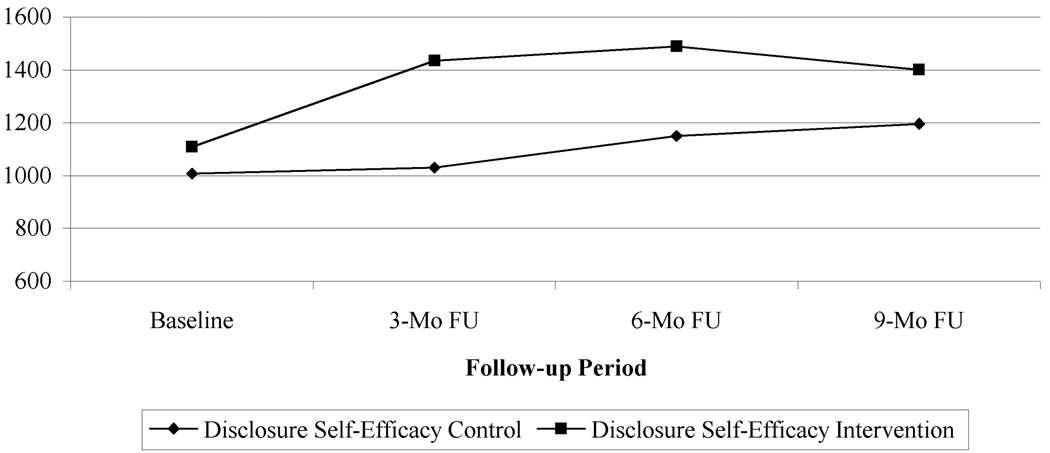
Disclosure self-efficacy
An overall group effect was noted (see Table 1), with a higher mean estimate for disclosure self-efficacy in the intervention group compared to the control (control M = 1096.97 vs. intervention M = 1357.93). Significant simple main effects were noted for the intervention group (see Figure 2), but not the control group. Follow-up tests (paired t-tests) in the intervention group showed significant increases with medium or better effects from baseline (M = 1108.51) to 3-month FU (M = 1434.08; t[70.1]= 3.12, p = .002, r = .35), to 6-month FU (M = 1487.76; t[66.8]= 3.58, p < .001, r = .40), and to 9-month FU (M = 1401.35; t[66.5]= 2.66, p = .009, r = .31), but not between later time-points.
Figure 2.
Least Squares Mean Plot of Disclosure Self-Efficacy by Group across Time
Overall, results indicate that the intervention group had higher levels of disclosure self-efficacy, showing increases from baseline and sustaining through the 9-month FU period.
Parent-Child communication
No significant effects were noted.
Family routines
No significant effects were noted.
Maternal Outcomes
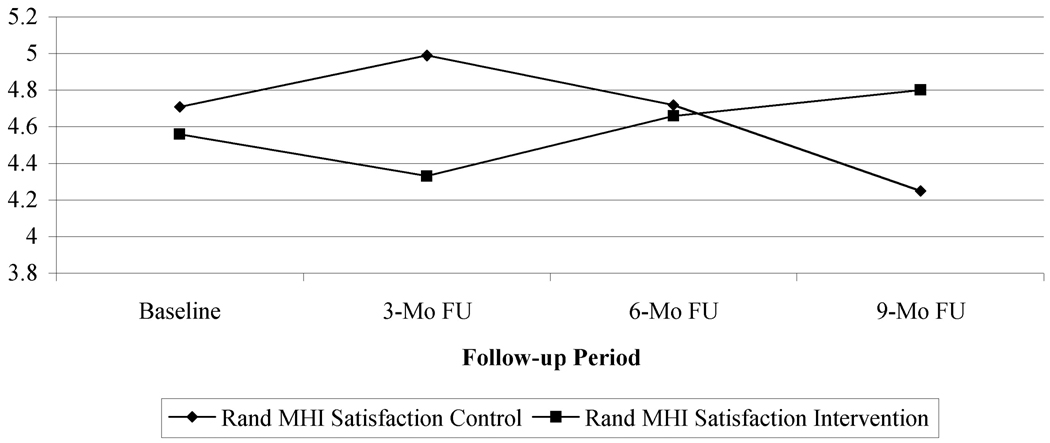
RAND Mental Health Inventory
Only the RAND Satisfaction item revealed significant mean differences for the simple main effects, and in the control group only (see Table 1). Follow-up paired tests within the control group show a significant decline in satisfaction with small to medium effects from baseline (M = 4.71) to 9-month FU (M = 4.25; t[73.1] = −2.07, p = .04, r = .24), and from 3-month FU (M = 4.99) to 9-month FU (t[70.3] = −3.42, p = .001, r = .38). Although no significant simple main effect was noted for the intervention group (p = .21), an increase in satisfaction was noted from 3-month FU (M = 4.33) to 9-month FU (M = 4.80; t[68.6] = 2.16, p = .03, r = .25). As seen in Figure 3, satisfaction rises initially for the control group, then diminishes, while in the intervention group, satisfaction at first declines then shows a steady rise. Note that within the intervention group only, we also assessed this quadratic trend by disclosure status, with similar quadratic trends (a decline then steady rise in satisfaction) noted regardless of disclosure status.
Figure 3.
Least Squares Mean Plot of Rand Mental Health Inventory (MHI) Satisfaction Item by Group across Time
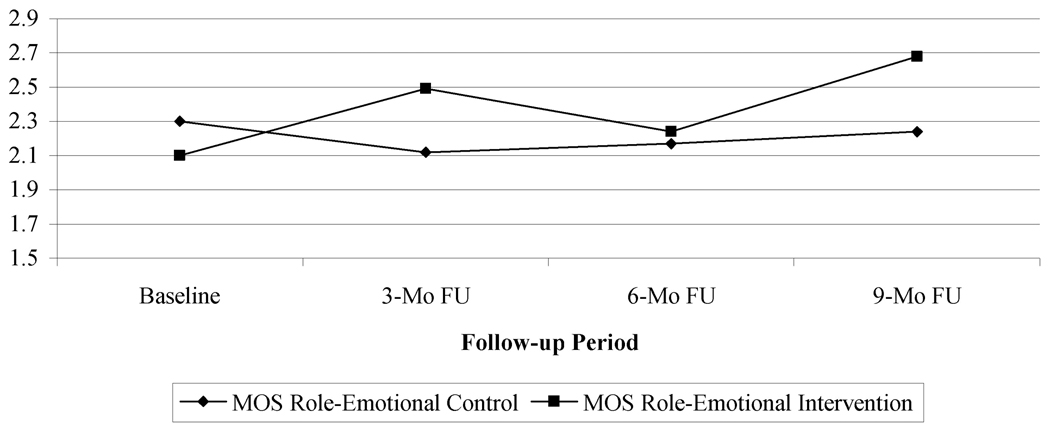
Medical Outcome Study Short Form 36 (MOS SF-36)
Only the emotional functioning subscale showed significant simple main effects, and for the intervention group only. Paired tests on the intervention group over time show an increase in emotional functioning with medium effects from baseline (M = 2.10) to 9-month FU (M = 2.68; t[73] = 3.03, p = .003, r = .33; see Figure 4). As a further evaluation, we assessed linear trends by disclosure status within the intervention group only – regardless of disclosure status, similar trend increases in emotional functioning were noted.
Figure 4.
Least Squares Mean Plot of Medical Outcome Study Short Form 36 (MOS SF-36) Role-Emotional Scale by Group across Time
Child Outcomes
Child Depression Inventory
Simple main effects showed significant declines across all measures for the intervention group, and some declines as well for the control group (see Table 2 for all measure mean estimates). For CDI Total, follow-up pairwise comparisons for the control group show declines with medium effects from baseline to 6-month FU (t[73.2] = −2.74, p = .007, r = .31), from baseline to 9-month FU (t[76.3] = −2.40, p = .01, r = .27), and from 3-month FU to 6-month FU (t[54.2] = −2.65, p = .01, r = .34). For the intervention group on CDI Total, declines are noted with large effects from baseline to 3-month FU (t[74.2] = −5.20, p < .001, r = .52), to 6-month FU (t[79.3] = −4.91, p <.001, r = .48), and to 9-month FU (t[69.8] = −5.19, p < .001, r = .53), but no latter time point differences were noted. Thus, similar declines were noted across both the control and intervention groups for this measure.
Table 2.
Least Squares Means and Standard Errors for Relationship Context, Mother's Mental Health, Child Mental Health, and Family Outcome Variables by Group (Control, Intervention) across time
| Control Group – M (SE) | Intervention Group – M (SE) | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 3-month | 6-month | 9-month | Baseline | 3-month | 6-month | 9-month | |
| Relationship Context (Targeted by Intervention) | ||||||||
| Disclosure Self-Efficacy | 1008.39 (89.21) | 1031.69 (104.19) | 1150.59 (111.32) | 1197.23 (113.16) | 1108.51 (91.46) | 1434.08 (111.00) | 1487.76 (117.54) | 1401.35 (114.37) |
| Parent/Child Communication | 28.88 (0.62) | 29.22 (0.52) | 28.99 (0.56) | 28.64 (0.53) | 30.38 (0.64) | 29.45 (0.54) | 30.08 (0.59) | 29.51 (0.53) |
| Family Cohesion | 16.34 (0.48) | 16.40 (0.44) | 16.40 (0.44) | 16.76 (0.45) | 16.64 (0.50) | 16.75 (0.46) | 16.94 (0.46) | 17.67 (0.45) |
| Mother’s Mental Health Outcomes | ||||||||
| RAND Mental Health Inventory (MHI) | ||||||||
| Anxiety | 21.59 (1.32) | 20.01 (1.33) | 21.76 (1.44) | 21.36 (1.33) | 22.10 (1.36) | 20.67 (1.38) | 20.45 (1.50) | 21.05 (1.34) |
| Depression | 9.27 (0.61) | 8.95 (0.50) | 9.20 (0.66) | 9.35 (0.57) | 9.03 (0.63) | 8.35 (0.52) | 8.07 (0.68) | 8.71 (0.57) |
| Satisfaction Item | 4.71 (0.19) | 4.99 (0.22) | 4.72 (0.20) | 4.25 (0.22) | 4.56 (0.19) | 4.33 (0.23) | 4.66 (0.21) | 4.80 (0.22) |
| Medical Outcome Study Short Form 36 (MOS SF-36) | ||||||||
| Role-Emotional | 2.30 (0.18) | 2.12 (0.18) | 2.17 (0.21) | 2.24 (0.19) | 2.10 (0.19) | 2.49 (0.19) | 2.24 (0.22) | 2.68 (0.19) |
| Child Outcomes | ||||||||
| Child Depression Inventory (CDI) | ||||||||
| Total | 7.39 (1.00) | 6.52 (0.91) | 4.87 (0.89) | 4.84 (0.95) | 10.62 (1.03) | 5.78 (0.94) | 5.77 (0.96) | 5.20 (0.92) |
| Negative Self-Esteem | 0.78 (0.23) | 0.65 (0.17) | 0.43 (0.17) | 0.51 (0.20) | 1.23 (0.24) | 0.67 (0.17) | 0.82 (0.19) | 0.54 (0.19) |
| Anhedonia | 3.22 (0.44) | 2.83 (0.44) | 2.34 (0.48) | 2.04 (0.42) | 4.56 (0.45) | 2.48 (0.46) | 2.44 (0.52) | 2.16 (0.40) |
| Interpersonal Problems | 0.76 (0.23) | 0.67 (0.18) | 0.78 (0.16) | 0.78 (0.19) | 1.46 (0.23) | 0.51 (0.18) | 0.49 (0.18) | 0.58 (0.18) |
| Ineffectiveness | 1.17 (0.29) | 1.12 (0.25) | 0.91 (0.22) | 0.94 (0.24) | 1.97 (0.30) | 1.27 (0.26) | 1.06 (0.25) | 1.06 (0.23) |
| Negative Mood | 1.78 (0.30) | 1.35 (0.23) | 0.65 (0.17) | 0.83 (0.24) | 2.05 (0.31) | 1.20 (0.23) | 0.96 (0.18) | 1.23 (0.23) |
| Piers-Harris | ||||||||
| Freedom from Anxiety | 10.71 (0.38) | 10.64 (0.40) | 10.76 (0.44) | 11.53 (0.47) | 9.49 (0.39) | 10.67 (0.42) | 10.69 (0.48) | 10.56 (0.46) |
| Happiness | 7.37 (0.20) | 7.35 (0.17) | 7.47 (0.15) | 7.27 (0.18) | 6.67 (0.21) | 7.33 (0.17) | 7.35 (0.17) | 7.44 (0.17) |
| Family Outcomes | ||||||||
| Inventory of Parent and Peer Attachment | ||||||||
| Trust | 42.12 (0.90) | 41.47 (1.06) | 43.02 (0.91) | 42.28 (1.21) | 42.69 (0.92) | 42.66 (1.09) | 43.48 (1.00) | 43.14 (1.14) |
| Communication | 34.00 (0.99) | 33.07 (1.06) | 35.42 (0.96) | 34.45 (1.27) | 34.54 (1.01) | 34.87 (1.09) | 37.42 (1.04) | 36.36 (1.22) |
| Alienation | 22.46 (0.81) | 23.24 (0.75) | 22.94 (0.89) | 23.93 (1.09) | 22.79 (0.83) | 23.60 (0.78) | 23.54 (0.98) | 24.99 (1.02) |
| Total | 98.59 (2.22) | 97.93 (2.40) | 101.12 (2.32) | 100.22 (3.08) | 100.30 (2.28) | 101.44 (2.47) | 104.34 (2.48) | 104.55 (2.98) |
| Family Routines | 32.17 (0.93) | 31.55 (0.95) | 33.13 (1.20) | 31.96 (1.19) | 32.44 (0.95) | 32.42 (0.99) | 33.68 (1.25) | 33.07 (1.20) |
For CDI interpersonal problems, pairwise comparisons were made within the intervention group, with a significant decline noted with medium to large effects from baseline to 3-month FU (t[78.4] = −4.14, p < .001, r = .42), to 6-month FU (t[76.3] = −4.23, p < .001, r = .44), and to 9-month FU (t[73.7] = −3.50, p < .001, r = .38; see Table 2 for mean values). However, the latter timepoints were not found to differ (e.g., 3-month FU to 6-month FU). For CDI negative self-esteem within the intervention group, declines are noted with medium effects from baseline to 3-month FU (t[80.5] = −2.39, p = .01, r = .26), and to 9-month FU (t[75.8] = −2.70, p = .008, r = .30). However, the latter timepoints were not found to differ (e.g., 3-month FU to 6-month FU). For CDI anhedonia within the intervention group, a significant decline is noted with large effects from baseline to 3-month FU (t[72.4] = −4.32, p <.001, r = .45), to 6-month FU (t[76.9] = −4.35, p < .001, r = .44), and to 9-month FU (t[70] = −4.80, p <.001, r = .50). However, the latter timepoints were not found to differ. For CDI ineffectiveness within the intervention group, declines are noted with medium effects from baseline to 3-month FU (t[69.4] = −2.87, p = .005, r = .33), to 6-month FU (t[74.5] = −2.58, p = .01, r = .29), and to 9-month FU (t[69.6] = −2.98, p = .004, r = .34), but no latter timepoint differences were noted.
Finally, for CDI negative mood, significant declines were noted in both the control and intervention groups. Follow-up pairwise comparisons for the control group show declines with medium effects from baseline to 6-month FU (t[74.7] = −3.81, p < .001, r = .40), from baseline to 9-month FU (t[74.5] = −2.91, p = .004, r = .32), and from 3-month FU to 6-month FU (t[63.3] = −2.83, p = .006, r = .34). For the intervention group, declines are noted with medium effects from baseline to 3-month FU (t[74.9] = −2.84, p < .001, r = .31), baseline to 6-month FU (t[80.1] = −3.48, p <.001, r = .36), and baseline to 9-month FU (t[68.7] = −2.54, p = .01, r = .29), but no latter time point differences were noted.
Overall, and primarily in the intervention group, declines in depression were noted from baseline to the latter follow-up time-points, with a leveling of the effect after the 3-month FU. We also assessed linear trends by disclosure status within the intervention group only for the CDI scales. Similar trend declines in the CDI measures were noted regardless of disclosure status.
Piers-Harris Anxiety and Happiness
Simple main effects were found for the intervention group for both measures. Pairwise tests within the intervention group reveal significant increases in freedom from anxiety with medium effects from baseline (M = 9.49) to 3-month FU (M = 10.67; t[73.4] = 2.83, p = .005, r = .31), baseline to 6-month FU (M = 10.69; t[76.4] = 2.78, p = .006, r = .30), and baseline to 9-month FU (M = 10.56; t[67.3] = 2.20, p = .03, r = .26). Pairwise tests for the happiness scale also reveal significant increases with medium effects in happiness from baseline (M = 6.67) to 3-month FU (M = 7.33; t[75.6] = 3.16, p = .002, r = .34), baseline to 6-month FU (M = 7.35; t[75.1] = 3.11, p = .002, r = .34), and baseline to 9-month FU (M = 7.44; t[71.1] = 3.67, p < .001, r = .40).
Thus, for those in the intervention group, happiness increased and a greater freedom from anxiety was noted from baseline to 3-month FU, and maintained through subsequent assessments. We also assessed linear trends by disclosure status within the intervention group only for these measures. Regardless of disclosure status, similar trend increases for the Piers-Harris measures were noted.
Family Outcomes
Inventory of Parent and Child Attachment
The communication subscale was noted to have a significant simple main effect finding for the intervention group only at the .05 or better level (see Table 1). Pairwise tests showed a significant increase in parent-child communication with medium effects from baseline (M = 34.54) to 6-month FU (M = 37.42; t[73] = 2.98, p = .003, r = .33), and an increase from 3-month FU (M = 34.87) to 9-month FU (M = 36.36; t[65.8] = 2.53, p = .01, r = .30), suggesting a graduated increase in parent-child communication for the intervention group. None of the other parent/child attachment measures evidenced significant findings.
We also assessed linear trends by disclosure status within the intervention group only for parent-child communication. Whether MLH had disclosed their HIV status, similar trend increases in communication were noted.
Family cohesion
No significant simple main effects were noted, although in the intervention group a pairwise difference is evident between baseline (M = 16.64) and 9-month FU (M = 17.67), showing a significant increase with almost a medium effect in family cohesion, t(73.3) = 2.22, p = .02, r = .25. Linear trends by disclosure status were also evaluated within the intervention group only, with similar trend increases in cohesion noted regardless of disclosure status.
Discussion
The TRACK pilot study results indicate the intervention shows preliminary success in its primary aim: to increase disclosures to young children by the MLH. The intervention group mothers were significantly more likely to disclose, and the majority did it right after the intervention ended. Previous research indicates that MLH who do decide to disclose are more likely to disclose to older children, and female children. However, there were no age or gender differences in disclosure in this pilot study, perhaps because the intervention preparedness was more compelling than these typical tendencies.
The majority of the MLH who disclosed felt that they had managed well the main stumbling blocks to disclosure, all of which are targeted within intervention sessions. For example, the vast majority of disclosing MLHs reported they kept an appropriate emotional tone during the disclosure process and were ready to answer the typical questions that children ask during disclosure. A slight majority worked with the child to prepare a list of “safe people” with whom the child could talk. Thus, the intervention appeared to be effective in preparing at least a portion of the intervention MLH not only to disclose, but to make the disclosure in an effective manner.
The main intermediate variable upon which the intervention seemed to have an effect was disclosure self-efficacy. There were significant effects for communication, measured within the context of the parent-child relationship. Most importantly, the intervention increased self-efficacy to disclose, and this maintained across the entire study.
The hypotheses included that disclosure would increase MLH’s anxiety and depression, and increase child anxiety and depression in the short term (i.e., immediately following disclosure), with a return to normal functioning over time. However, given the research group’s concerns about increasing emotional distress in this vulnerable sample, extensive effort was undertaken during session development to decrease this possibility by: (1) ensuring MLH were aware of typical responses to disclosure based on a child’s developmental level, so that MLH were prepared for their child’s emotional reactions, as well as the typical questions asked by children when MLH disclose; and (2) teaching the MLH that their own emotional tone during the disclosure would have a big impact on the child’s reaction.
In this pilot study, the intervention group MLH’s emotional functioning and satisfaction improved significantly following the intervention. Similarly, and validating these results, the child mental health indicators among the children of intervention mothers showed significant positive change: by their own report levels on the anhedonia, negative self-esteem, interpersonal problems, and ineffectiveness subscales were reduced. Moreover, children of MLH in the intervention group also reported significant decreases in anxiety and depression scores, while the control group did not evidence such change. This finding was confirmed on a second measure (i.e., the Beck Youth Inventory anxiety and depression subscales; data not shown here). Finally, the Piers-Harris happiness and satisfaction subscale, as well as the freedom from anxiety subscale, improved among the intervention group. All of these findings indicate that overall, children of MLH in the intervention group improved on mental health indicators, while change in the control group was not evident. Thus, the disclosure appears not to have been traumatic for children. This is consistent with previous research that indicates that children unaware of their mother’s health status are often aware that something is wrong (e.g., they may notice their mothers taking medication, or physical symptoms, or hospitalizations) and that this awareness may cause tension and anxiety.
In terms of family outcomes, the intervention also demonstrates some effects. When the TRACK intervention was developed, it was unclear whether a brief intervention (only three sessions, focused primarily on disclosure) would have sufficient strength to influence broader family outcomes such as the parent-child relationship and family functioning, and whether a small pilot trial would evidence such influences if they did occur. Among the children of the intervention group mothers, communication increased significantly according to the parent attachment measure. In addition, family cohesion improved among the intervention group.
It should be noted that MLH satisfaction and emotional functioning improved in the intervention group, regardless of disclosure status. Similarly, the children of intervention group MLH showed better scores for anxiety, depression, and happiness regardless of whether they were the child of an MLH who had disclosed or not. Thus, it appears that the intervention skills the MLH learned in the intervention influenced these mental health indicators; the skills (e.g., parent-child communication) proved beneficial for these families even if the MLH did not reach the point of disclosure.
Three women from the control group disclosed their serostatus to their children. It was anticipated when the study was developed that within a 9-month longitudinal study of MLH who have not disclosed their status, a limited number of disclosures were likely to take place in the control group, for developmentally appropriate reasons or as unplanned disclosure (e.g., a mother discloses when she is angry or upset at the child). For the current study, disclosure rates were much higher in the intervention group than the control group, with the disclosures from intervention MLH overall being reported as a positive experience for both the MLH and their child. While there were too few disclosures among the control group to conduct specific comparative analysis, it appears that among control group MLH who disclosed, disclosure resulted in less positive reactions.
There are several limitations to this study, the first of which is the generalizability of our findings to other populations. Our sample was limited to recruitment from the greater Los Angeles area. Potentially important variables such as access to HIV services and stigma differ by geographic locale, and may differentially affect the outcomes of the disclosure intervention. A second limitation is the representativeness of our sample. Although HIV is disproportionately represented among women of color, our sample consists totally of women of color, so the only comparison that could be made was between Latina and African-American mothers, and no ethnic differences were found for disclosure rates. This finding is consistent with previous research in which ethnicity and/or acculturation have not been found to be related to disclosure (e.g., Lettney, 2006; Letteney & LaPorte. 2004; Rice et al., 2009). Inclusion criteria for this study required that the mother had not yet disclosed her status to her child. It is quite possible that our sample is representative of Los Angeles area HIV+ mothers who have not yet disclosed. One study of maternal HIV provides evidence supporting this; Tompkins et al. (1999), in their Los Angeles area sample, found that the children of European and African American mothers were more likely to be aware of their mother’s HIV status than children of Latina mothers. Another limitation is that a p < .05 significance level was used for pair-wise comparisons. Although this may lead to inflated Type I error, the use of simple effects tests as an initial test prior to these comparisons acts to limit such inflation. Regardless, pair-wise findings reported here close to the p < .05 cutoff should be interpreted cautiously. Finally, the full theoretical model (Derlega et al., 2004) could not be tested in this small pilot trial due to a lack of power. As noted in the Introduction to the paper, this small pilot study only focuses on the changes in the relationship context variables and the disclosure outcomes from the model. The relationship context, including intrafamilial communication and parenting skills, was of particular interest since these factors could potentially be influenced by a behavioral intervention. A full-scale trial of the intervention is needed to test the full model.
Acknowledgments
This research was supported by Grant 5R01MH077493 from the National Institute of Mental Health to the first author.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ccp
References
- Abidin RR. Parenting Stress Index Manual. Charlottesville, VA: Pediatric Psychology Press; 1990. [Google Scholar]
- Alexander JF, Sexton TL, Robbins MS. The developmental status of family therapy in family psychology intervention science. In: Liddle HA, Santisteban DA, Levant RF, Bray JH, editors. Family psychology. Science-based interventions. Washington, DC: American Psychological Association; 2002. pp. 17–40. [Google Scholar]
- Armistead L, Tannenbaum L, Forehand R, Morse E, Morse P. Disclosing HIV status: Are mothers telling their children? Journal of Pediatric Psychology. 2001;26:11–20. doi: 10.1093/jpepsy/26.1.11. [DOI] [PubMed] [Google Scholar]
- Armsden GC, Greenberg MT. The Inventory of Parent and Peer Attachment: Individual differences and the relationship to psychological well-being in adolescence. Journal of Youth and Adolescence. 1987;16:427–454. doi: 10.1007/BF02202939. [DOI] [PubMed] [Google Scholar]
- Bloom BL, Naar S. Self-report measures of family functioning: Extensions of a factorial analysis. Family Process. 1994;33:203–216. doi: 10.1111/j.1545-5300.1994.00203.x. [DOI] [PubMed] [Google Scholar]
- Brown H, Prescott R. Applied MIXED models in medicine. 2nd ed. New York, NY: Wiley; 2006. [Google Scholar]
- Cohen J. A power primer. Psychological Bulletin. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Chaudoir SR, Quinn DM. Revealing concealable stigmatized identities: The impact of disclosure motivations and positive first-disclosure experiences on fear of disclosure and well-being. Journal of Social Issues. 2010;66:570–584. doi: 10.1111/j.1540-4560.2010.01663.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corona R, Beckett MK, Cowgill BO, Elliott MN, Murphy DA, Zhou AJ, Schuster MA. Do children know their parent’s HIV-Status? Parental reports of child knowledge in a nationally representative sample. Ambulatory Pediatrics. 2006;6:138–144. doi: 10.1016/j.ambp.2006.02.005. [DOI] [PubMed] [Google Scholar]
- Curry JF, Craighead WE. Depression. In: Ollendick TH, Hersen M, editors. Handbook of child and adolescent assessment. Boston: Allyn and Bacon; 1993. pp. 251–268. [Google Scholar]
- Derlega VJ, Winstead BA, Greene K, Serovich J, Elwood WN. Reasons for HIV disclosure/nondisclosure in close relationships: Testing a model of HIV-disclosure decision making. Journal of Social & Clinical Psychology. 2004;23:747–767. [Google Scholar]
- Forsyth BW, Damour L, Nagler S, Adnopoz J. The psychological effects of parental human immunodeficiency virus infection on uninfected children. Archives of Pediatrics and Adolescent Medicine. 1996;150:1015–1020. doi: 10.1001/archpedi.1996.02170350017002. [DOI] [PubMed] [Google Scholar]
- Hughes HM. Measures of self-concept and self-esteem for children ages 3 – 12 years: A review and recommendations. Clinical Psychology Review. 1984;4:657–692. [Google Scholar]
- Jaccard J. Interaction effects in factorial analysis of variance. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- Jensen EW, James SA, Boyce WT, Hartnett SA. The Family Routines Inventory: Development and validation. Social Science & Medicine. 1983;17:201–211. doi: 10.1016/0277-9536(83)90117-x. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Cain D, Fuhrel A, Eaton L, Di Fonzo K, Ertl T. Assessing medication adherence self-efficacy among low-literacy patients: Development of a pictographic visual analogue scale. Health Education Research. 2005;20:24–35. doi: 10.1093/her/cyg106. [DOI] [PubMed] [Google Scholar]
- Kirshenbaum SB, Nevid JS. The specificity of maternal disclosure of HIV/AIDS in relation to children’s adjustment. AIDS Education & Prevention. 2002;14:1–16. doi: 10.1521/aeap.14.1.1.24331. [DOI] [PubMed] [Google Scholar]
- Kovacs M. The Interview Schedule for Children. Psychopharmacology Bulletin. 1985;21:991–994. [PubMed] [Google Scholar]
- Kovacs M, Beck AT. An empirical clinical approach toward a definition of childhood depression. In: Schulterbrandt JG, Raskin A, editors. Depression in childhood: Diagnosis, treatment, and conceptual models. New York: Raven Press; 1977. pp. 1–25. [Google Scholar]
- Letteney S. Mothers disclosure of maternal HIV status to children: Key psychosocial correlates. Journal of HIV/AIDS & Social Services. 2006;5:67–84. [Google Scholar]
- Letteney S, LaPorte HH. Deconstructing stigma: Perceptions of HIV-seropositive mothers and their disclosure to children. Social Work in Health Care. 2004;38:105–123. doi: 10.1300/J010v38n03_06. [DOI] [PubMed] [Google Scholar]
- Maxwell SE. Pairwise multiple comparisons in repeated measures designs. Journal of Educational Statistics. 1980;5:269–287. [Google Scholar]
- Mellins CA, Brackis-Cott E, Dolezal C, Richards A, Nicholas SW, Abrams EJ. Patterns of status disclosure to perinatally HIV-infected children and subsequent mental health outcomes. Clinical Child Psychology & Psychiatry. 2002;7:101–114. [Google Scholar]
- Miller KS, Forehand R, Kotchick BA. Adolescent sexual behavior in two ethnic minority samples: The role of family variables. Journal of Marriage and the Family. 1999;61:85–98. [Google Scholar]
- Murphy DA. HIV-positive mothers’ disclosure of their serostatus to their young children: A review. Clinical Child Psychology and Psychiatry. 2008;13:105–122. doi: 10.1177/1359104507087464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy DA, Kaufman A, Swendeman D. Mothers with AIDS who have young children: Preliminary findings. Paper presented at the sixth annual NIMH Research Conference on the Role of Families in Preventing and Adapting to HIV/AIDS; 1998, July; Washington, DC. [Google Scholar]
- Murphy DA, Marelich WD, Hoffman D. A longitudinal study of the impact on young children of maternal HIV serostatus disclosure. Clinical Child Psychology and Psychiatry. 2002;7:55–70. [Google Scholar]
- Murphy DA, Roberts KJ, Hoffman D. Stigma and ostracism associated with HIV/AIDS: Children carrying the secret of their mothers’ HIV+ serostatus. Journal of Child and Family Studies. 2002;11:191–202. [Google Scholar]
- Murphy DA, Roberts KJ, Hoffman D. Regrets and advice from mothers who have disclosed their HIV+ serostatus to their young children. Journal of Child and Family Studies. 2003;12:307–318. [Google Scholar]
- Murphy DA, Roberts KJ, Hoffman D. Young children’s reactions to mothers’ disclosure of maternal HIV+ sersostatus. Journal of Child and Family Studies. 2006;15:39–56. [Google Scholar]
- Murphy DA, Steers WN, Dello Stritto ME. Maternal disclosure of mother’s HIV serostatus to their young children. Journal of Family Psychology. 2001;15:441–450. doi: 10.1037//0893-3200.15.3.441. [DOI] [PubMed] [Google Scholar]
- Nagler S, Adnopoz J, Forsyth W. Uncertainty, stigma, and secrecy: Psychological aspects of AIDS for children and adolescents. In: Geballe S, Gruendel J, Andemann W, editors. Forgotten children of the AIDS epidemic. New Haven, CT: Yale University; 1995. pp. 71–82. [Google Scholar]
- Nostlinger C, Bartoli G, Gordillo V, Roberfroid D, Colebunders R. Children and adolescents living with HIV positive parents: Emotional and behavioural problems. Vulnerable Children and Youth Studies. 2006;1:29–43. [Google Scholar]
- Palin FL, Armistead L, Clayton A, Ketchen B, Lindner G, Kokot-Louw P, Pauw A. Disclosure of maternal HIV-infection in South Africa: Description and relationship to child functioning. AIDS and Behavior. 2009;13:1241–1252. doi: 10.1007/s10461-008-9447-4. [DOI] [PubMed] [Google Scholar]
- Piers EV. Piers-Harris Children’s Self-Concept Scale: Revised Manual 1984. Los Angeles: Western Psychological Services; 1993. [Google Scholar]
- Rice E, Comulada S, Green S, Arnold EM, Rotheram-Borus MJ. Differential disclosure across social network ties among women living with HIV. AIDS and Behavior. 2009;13:1253–1261. doi: 10.1007/s10461-009-9554-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt CK, Goggin K. Disclosure Patterns among HIV+ Women. American Clinical Laboratory. 2002;21:40–43. [PubMed] [Google Scholar]
- Tompkins TL. Parentification and maternal HIV infection: Beneficial role or pathological burden? Journal of Child and Family Studies. 2007;16:108–118. [Google Scholar]
- Tompkins TL, Henker B, Whalen CK, Axelrod J, Comer LK. Motherhood in the context of HIV infection: Reading between the numbers. Cultural Diversity & Ethnic Minority Psychology. 1999;5:197–208. [Google Scholar]
- UNAIDS: The Joint United Nations Program on HIV/AIDS. Report on the global AIDS epidemic 2008. Geneva, Switzerland: Author; 2008. Aug, [Google Scholar]
- Veit C, Ware J. The structure of psychological distress and well-being in general populations. Journal of Consulting and Clinical Psychology. 1983;51:730–742. doi: 10.1037//0022-006x.51.5.730. [DOI] [PubMed] [Google Scholar]
- Ware JE, Gandek B the IQOLA Project Group. The SF-36 Health Survey: Development and use in mental health research and the IQOLA Project. International Journal of Mental Health. 1994;23:49–73. [Google Scholar]
- Weiner LS, Battles HB, Heilman NE. Factors associated with parents’ decision to disclose their HIV diagnosis to their children. Child Welfare. 1998;77:115–135. [PubMed] [Google Scholar]
- Winer BJ. Statistical principles in experimental design. 2nd ed. New York, NY: McGraw-Hill; 1971. [Google Scholar]
- Wood K, Chase E, Aggleton P. ‘Telling the truth is the best thing’: Teenage orphans’ experiences of parental AIDS-related illness and bereavement in Zimbabwe. Social Science & Medicine. 2006;63:1923–1933. doi: 10.1016/j.socscimed.2006.04.027. [DOI] [PubMed] [Google Scholar]
- Wolfinger RD, Chang M. Comparing the SAS GLM and MIXED procedures for repeated measures. Cary, NC: SAS Institute Inc.; 1998. [Google Scholar]