Abstract
Thirteen matched pairs of cadaveric femurs were placed into two groups. In each group, a transverse fracture was created at a point 70% distal between the lesser trochanter and the adductor tubercle. One femur out of each matched pair was then stabilised with an interlocking intramedullary nail (nail only group) and the other femur was stabilised with plate augmentation after interlocking intramedullary nailing (plate augmentation group). The bending load to promote 5-mm displacement showed statistically significant differences between the plate augmentation group (mean 843.36 ± 409.13 N) and the nail only group (mean 315.02 ± 219.80 N) (p = 0.001). Torsional torque at the angle of 15 degrees showed statistically significant differences between the two groups; a mean of 2.09 ± 0.53 N·m for the plate augmentation group and a mean of 0.63 ± 0.46 N·m for the nail only group (p = 0.0001). We found a 2.6-fold increase in bending stiffness and a 3.3-fold increase in torsional stiffness in plate augmentation leaving a nail in situ compared to interlocking nailing only in the distal third fracture of femur.
Introduction
Interlocking intramedullary nailing has become widely accepted as the treatment of choice for femoral shaft fractures since the description by Kuntscher [9]. The intramedullary nail reduces the gross motion of fracture fragment but does not abolish it completely. Fracture healing can be achieved by the formation of peripheral callus since acceptable motion is present at the fracture site. Complications such as shortening, angulation, and rotation, especially in complex fractures, can be minimised with interlocking screws, which may be inserted transversely and/or obliquely through the nail proximal and distal to the fracture site [6, 14]. However, as the interlocking intramedullary nails are not canal-filling in the distal shaft or comminuted fractures of the femur, the ability to resist rotational and bending force is limited. Furthermore, according to one experiment, the fracture site did not show much resistance to rotational movement within 10–15 degrees when interlocking nails were inserted, suggesting that absolute fixation power at the fracture site by interlocking intramedullary nails was limited. Too much motion in complex fractures resulted in unpredictable mechanical stability and nonunion [12]. This small subset of cases may require more stability than that is afforded by interlocking intramedullary nailing [5].
Plate augmentation leaving the nail in situ can provide additional stability for the fracture when there is continuous excess motion at the fracture site after interlocking intramedullary nailing. The retained nail acts as a useful load-sharing device, neutralising shear forces at the fracture site and maintaining alignment of the fracture [12]. Choi et al. [2] reported successful bony union with plate augmentation leaving the nail in situ for unstable femoral nonunion. Many surgeons ask about the mechanical role of plate augmentation after interlocking intramedullary nailing whenever authors present the clinical results at meetings.
The object of this study was to examine the differences in mechanical rigidity between plate augmentation leaving the nail in situ and interlocking nail using a cadaveric fracture model of the femur.
Materials and methods
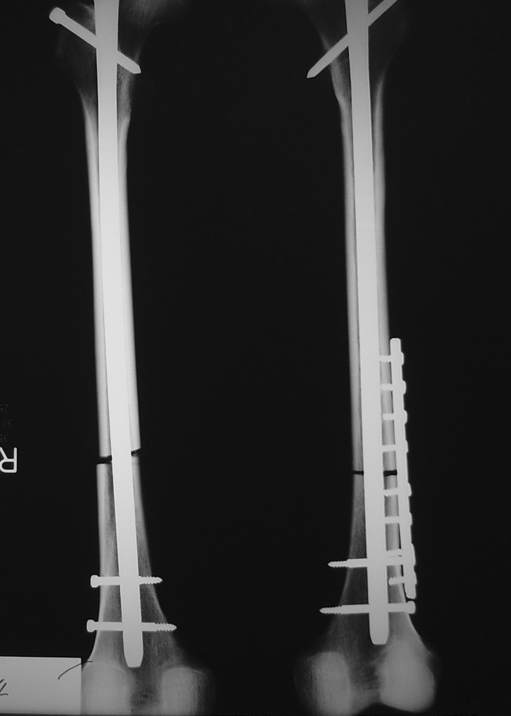
Thirteen embalmed human femora were obtained from the anatomical lab at the College of Medicine, Chonnam National University. None of the limbs had any radiological abnormality. The mean age of cadavers at the time of death was 51 years (range 34–87). There were 12 males and one female. The bone density was determined at the proximal trochanter using dual energy X-ray absorptionometry (QDR-2000, Hologic). After the femur length and intramedullary canal size were confirmed on radiographs, a transverse fracture was created using an electric saw at a point 70% of the distance from the lesser trochanter towards the adductor tubercle. After reducing the fracture, a Grosse-Kempf intramedullary nail was inserted after reaming, according to the manufacturer’s recommendations [8], with guiding devices. Reaming was performed 2 mm larger than the intramedullary canal with its size confirmed radiographically, and intramedullary nailing was performed. One interlocking screw was fixed at the proximal portion and two screws at the distal portion (nail only group). Likewise, the other femur of each matched pair achieved fixation with plate augmentation after interlocking intramedullary nailing. The same size and length intramedullary nails were applied to each pair of matching femurs. A compression plate with eight holes was applied at the lateral side of the femur and unicortical screw fixation was performed with four screws in the proximal portion and four screws in the distal portion (plate augmentation group). The matched pair femora were randomised into two groups. After the implantation, radiographic examination was done to evaluate the fracture gap and nail distribution (Fig. 1).
Fig. 1.
Fractures were created that were at 70% the length of the femur, measured from the lesser trochanter to the adductor tubercle. A femur of each matched pair was fixed with interlocking intramedullary nail and the contralateral femur was fixed with plate augmentation after interlocking intramedullary nail
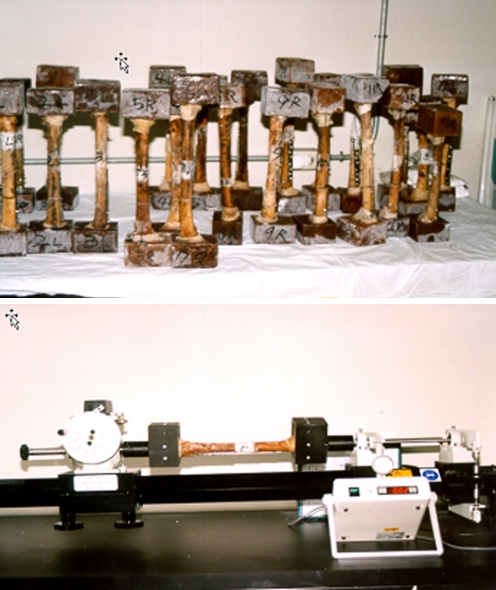
First, the four-point bending test was performed using the Instron machine (model 1331; Instron, Canton, MA, USA). Bending moment was applied to the fracture site from the posteromedial to the anterolateral direction, and the value of load for maximum displacement of 5 mm was recorded in a computer (Fig. 2). During the experiment, we tried to establish the same conditions for both groups, such as the direction and location of load. The tests were carried out within the elastic range of the construction.
Fig. 2.
Four-point bending test performed until the fracture bent to 5-mm displacement
Second, a mounting jig was designed to secure both ends of the femur for a subsequent torsional test. After connecting the jig to the SM1 Torsion Testing Machine (TecQuipment, LTD), the value of load given for displacement of 15 degrees of the fracture site or the failure of the screws in the augmentation plate was recorded (Fig. 3).
Fig. 3.
A mounting jig was designed to keep the two holding fixtures for a subsequent torsional test (above). Each femur was rotated until an angle of 15 degrees or failure of the fixation (below)
The data were expressed as mean ± standard deviation. We determined the difference in the gap of the fracture, nail distribution ratio and bone mineral density between both groups using the t-test. Data retrieved from the four-point bending tests and torsional tests were analysed with the t-test. Finally, we analysed the correlation between bone mineral density and results from bending and torsional tests. Statistical analyses were performed using SPSS software (version 12.0; SPSS Inc., Chicago, IL).
Results
According to the radiographic examination, the average fracture gap was 4.3 ± 1.2 mm in the nail only group and 4.2 ± 1.2 mm in the plate augmentation group (Table 1). The average nail distribution ratio in the distal fragment was 74.9 ± 7.2% in the nail only group and 73.5 ± 7.0% in the plate augmentation group. The average bone density at the trochanter of the femur was 0.87 ± 0.11 g/cm2 in the nail only group and 0.86 ± 0.10 g/cm2 in the plate augmentation group. Thus, no significant differences were present in the fracture gap (p = 0.93), nail distribution ratio in the distal fragment (p = 0.60), and bone density (p = 0.72) between the two groups.
Table 1.
Summary of the data
| Patient number | Age (years) | Gender | Site | BMD | Gap size (mm) | Nail distribution (%) | 15° torsional test (N·m) | 5-mm bending test (N) |
|---|---|---|---|---|---|---|---|---|
| 1 | 44 | M | Nail | 0.86 | 3 | 67.16 | 0.32 | 376.1 |
| Plate | 0.873 | 6 | 65.41 | 2.12 | 1044.2 | |||
| 2 | 40 | M | Nail | 0.952 | 4 | 65.87 | 0.36 | 386.8 |
| Plate | 0.935 | 4.5 | 66.67 | 1.61 | 420.8 | |||
| 3 | 47 | M | Nail | 1.001 | 3 | 82.71 | 1.19 | 515.9 |
| Plate | 0.983 | 3.5 | 76.39 | 2.43 | 1809.9 | |||
| 4 | 87 | M | Nail | 0.983 | 4 | 78 | 1.18 | 209 |
| Plate | 0.842 | 3 | 73.08 | 2.81 | 726.2 | |||
| 5 | 59 | M | Nail | 0.833 | 4 | 76.47 | 0.26 | 161.5 |
| Plate | 0.849 | 3 | 74.4 | 0.85 | 700.6 | |||
| 6 | 53 | M | Nail | 0.895 | 6 | 67.67 | 1.31 | 119.5 |
| Plate | 0.905 | 5.5 | 65.56 | 2.45 | 1412.2 | |||
| 7 | 43 | M | Nail | 0.567 | 4 | 88.08 | 0.14 | 30.1 |
| Plate | 0.553 | 3.5 | 84.62 | 1.51 | 434.1 | |||
| 8 | 34 | M | Nail | 0.99 | 3.5 | 64.71 | 1.04 | 865.2 |
| Plate | 0.94 | 3.5 | 63.85 | 1.89 | 871.7 | |||
| 9 | 42 | M | Nail | 0.827 | 6 | 71.94 | 0.31 | 448.7 |
| Plate | 0.857 | 3 | 70.8 | 2.3 | 497.4 | |||
| 10 | 44 | M | Nail | 0.96 | 6 | 76.92 | 0.1 | 126.1 |
| Plate | 0.945 | 6 | 76.47 | 2.5 | 783.7 | |||
| 11 | 59 | M | Nail | 0.83 | 3 | 73.57 | 0.13 | 295.7 |
| Plate | 0.884 | 3 | 72.39 | 2.23 | 1049.6 | |||
| 12 | 56 | M | Nail | 0.914 | 6 | 78.83 | 0.92 | 373.3 |
| Plate | 0.866 | 6 | 81.82 | 2.65 | 445.6 | |||
| 13 | 53 | F | Nail | 0.784 | 3.5 | 82.76 | 0.99 | 187.4 |
| Plate | 0.757 | 5 | 84.04 | 1.89 | 767.8 | |||
| Mean ± standard deviation (SD) | Nail | 0.87 ± 0.11 | 4.3 ± 1.2 | 74.9 ± 7.2 | 0.634 ± 0.46 | 315.02 ± 219.80 | ||
| Plate | 0.86 ± 0.10 | 4.2 ± 1.2 | 73.5 ± 7.0 | 2.095 ± 0.53 | 843.37 ± 409.14 | |||
BMD bone mineral density, M male, F female, Nail IM nail only group, plate plate augmentation group
The mechanical tests showed statistically significant differences in bending stiffness with the displacement of 5 mm (p = 0.001). The average bending stiffness was 843.36 ± 409.13 N in the plate augmentation group and 315.02 ± 219.80 N in the nail only group (Fig. 4). The plate augmentation group showed 2.6-fold bending stiffness compared with the nail only group. However, there was no correlation between bone mineral density and bending stiffness from the plate augmentation group (p = 0.067, r = 0.522) and the nail only group (p = 0.108, r = 0.467).
Fig. 4.
Plate augmentation after interlocking intramedullary nailing was significantly stiffer than the interlocking intramedullary nail alone in bending test (p = 0.001)
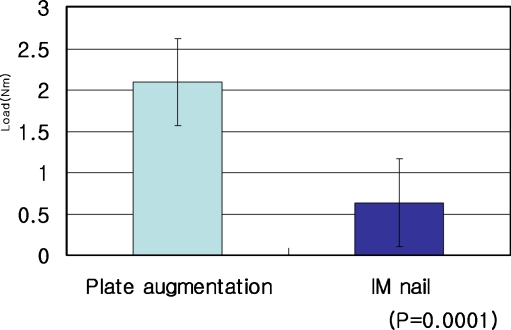
Torsional stiffness showed statistically significant differences with displacement of 15 degrees (p = 0.0001). The mean torsional stiffness was 2.09 ± 0.53 N·m in the plate augmentation group and 0.63 ± 0.46 N·m in the nail only group (Fig. 5). The plate augmentation group showed 3.3-fold torsional stiffness compared with the nail only group. The torsional stiffness of the plate augmentation group (p = 0.409, r = 0.250) and the nail only group ( p = 0.094, r = 0.484) revealed no correlation with bone mineral density.
Fig. 5.
The torsional stiffness showed that the plate augmentation group was 3.3-fold stiffer than the nail only group (p = 0.0001)
Discussion
Many endeavours and considerable amounts of money have been expended in research to treat nonunion developed after interlocking intramedullary nailing for femoral shaft fractures, but these efforts must be shifted to find out the causes of nonunion and to prevent it [4, 7, 13, 17, 18]. Reamed exchange nailing was widely accepted as the treatment of choice for the nonunion of femoral shaft fracture, but a significant number of patients who had undergone reamed exchange nailing required additional procedures to achieve union of the fractures [3, 16]. Choi et al. [2] reported successful bony union with plate augmentation leaving the nail in situ for unstable femoral nonunion. Ueng et al. [15] and Nadkarni et al. [11] achieved successful bony union with plate augmentation in the presence of intramedullary nailing for femoral nonunion. However, it could be argued that plate fixation might be an unnecessarily redundant fixation for nonunion after interlocking intramedullary nailing. We, therefore, carried out this study to discover whether the plate augmentation leaving the nail in situ had better mechanical stiffness than the interlocking nail only in the distal third fracture of femur.
The rigidity of intramedullary nailing is not enough to maintain stability for the fracture site of the femur when a rotational force is applied to the fracture site. But resistance for rotational force can be increased significantly with the use of interlocking screws. According to the experiment by Kyle et al. [10], the rotational resistance could be increased up to four times using interlocking screws, and Bankston et al. [1] reported it could be increased as much as ten times. However, even if rotational resistance could be increased by using interlocking screws, the rotational stiffness of an interlocking nail is only 3% of the normal femur according to the experiment by Johnson et al. [6]. Thus, compared with 55–70% of bending stiffness in the normal femur, an interlocking intramedullary nail would be relatively vulnerable to rotational deformity. Furthermore, according to these experiments, the fracture site did not have much resistance to rotational moment between 10–15 degrees when an interlocking intramedullary nail was inserted into the femur. This suggests that the absolute fixative power at the fracture site by an interlocking intramedullary nail would be limited, especially in rotation.
Tarr and Wiss [14] reported that although plates were strong under torsional force, they were weak under bending forces due to stress concentration through the screw hole. However, intramedullary nails were strong against axial compressive forces and bending forces but were weak against torsional force. In internal fixation for fractures, when dynamic loading such as weight bearing exceeds the stability of the internal fixation, bone resorption will occur in the fracture by micromotion between the bone and the internal fixation implant instead of fracture healing, so that this fracture would require additional protection from the stress.
In our study, plate augmentation after interlocking intramedullary nailing was significantly stiffer than the interlocking intramedullary nail only in the 5-mm bending test (p = 0.001). The torsional stiffness showed that the plate augmentation group was 3.3 times stiffer than the interlocking nail only group (p = 0.0001). Plate augmentation leaving the nail in situ provides additional stability for the fracture when there is excess motion at the fracture site after interlocking intramedullary nailing for femoral shaft fracture. The retained nail acts as a useful load-sharing device, neutralising the shear forces on the fracture site and maintaining alignment of the fracture. Although this study is limited by it use of a cadaveric fracture model of the femur, these results suggest that plate augmentation leaving the nail in situ can be an effective solution in cases of unstable femoral nonunion after interlocking intramedullary nailing.
References
- 1.Bankston AB, Keating DA, Simon FD. The biomechanical evaluation of intramedullary nails in distal femoral shaft fractures. Clin Orthop. 1992;276:277–282. [PubMed] [Google Scholar]
- 2.Choi YS, Kim KS. Plate augmentation leaving the nail in situ and bone grafting for nonunion of femoral shaft fractures. Int Orthop. 2005;29(5):287–290. doi: 10.1007/s00264-005-0668-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cole JD (1996) The vascular response of bone to internal fixation. In: Browner BD (ed) The science and practice of intramedullary nailing, 2nd edn. Willians and Wilkins, pp 43–69
- 4.Finkemeier CG, Chapman MW. Treatment of femoral diaphyseal nonunions. Clin Orthop. 2002;398:223–234. doi: 10.1097/00003086-200205000-00031. [DOI] [PubMed] [Google Scholar]
- 5.Hak DJ, Lee SS, Goulet JA. Success of exchange reamed intramedullary nailing for femoral shaft nonunion or delayed union. J Orthop Trauma. 2000;14:178–182. doi: 10.1097/00005131-200003000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Johnson KD, Tencer AF, Blementhal S. Biomechanical performance of locked intramedullary nailing system in comminuted femoral shaft fractures. Clin Orthop. 1986;206:151–1616. [PubMed] [Google Scholar]
- 7.Kan WS, Zheng Q, Wang JW, Huang H, Chen PYH, XIe M, Li P. Treatment of the ununited lower limb fracture with reamed intramedullary interlocking nail. Zhonghua Wai Ke Za Zhi. 2006;44(20):1417–1419. [PubMed] [Google Scholar]
- 8.Kempf I, Grosse A, Beak GF. Closed locked Intramedullary nailing. Its application to comminuted fractures of the femur. J Bone Joint Surg [Am] 1985;67:709–720. [PubMed] [Google Scholar]
- 9.Kuntscher G. Intramedullary surgical technique and its place in orthopaedic surgery. J Bone Joint Surg [Am] 1965;47:809–818. [PubMed] [Google Scholar]
- 10.Kyle RF, Shcaffhausen JM, Bechtold JE. Biomechanical characteristics of interlocking femoral nails in the treatment of complex femoral fractures. Clin Orthop. 1991;267:169–173. [PubMed] [Google Scholar]
- 11.Nadkarni B, Srivastav S, Mittal V, Agarwal S. Use of locking compression plates for long bone nonunions without removing existing intramedullary nail: review of literature and our experience. J Trauma. 2008;65(2):482–486. doi: 10.1097/TA.0b013e31817c9905. [DOI] [PubMed] [Google Scholar]
- 12.Pihlajamaki HK, Salminen ST, Bostman OM. The treatment of nonunions following intramedullary nailing of femoral shaft fractures. J Orthop Trauma. 2002;16(6):394–402. doi: 10.1097/00005131-200207000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Steinberg EL, Keynan O, Sternheim A, Drexler M, Luger E. Treatment of diaphyseal nonunion of the femur and tibia using an expandable nailing system. Injury. 2009;40(3):309–314. doi: 10.1016/j.injury.2008.07.029. [DOI] [PubMed] [Google Scholar]
- 14.Tarr RR, Wiss DA. The mechanics and biology of intramedullary fracture fixation. Clin Orthop. 1986;212:10–17. [PubMed] [Google Scholar]
- 15.Ueng SWN, Chao EK, Lee SS, Shih CH. Augmentative plate fixation for the management of femoral nonunion after intramedullary nailing. J Trauma. 1995;43:640–644. doi: 10.1097/00005373-199710000-00013. [DOI] [PubMed] [Google Scholar]
- 16.Weresh MJ, Hakanson R, Stover M, Sims SH, Kellam JK, Bosse MJ. Failure of exchange reamed intramedullary nails for ununited femoral shaft fractures. J Orthop Trauma. 2000;14:335–338. doi: 10.1097/00005131-200006000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Wu CC. The effect of dynamization on slowing the healing of femur shaft fractures after interlocking nailing. J Trauma. 1997;43(2):263–267. doi: 10.1097/00005373-199708000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Zhang X, Zhong B, Sui S, Yu X, Jiang Y. Treatment of distal femoral nonunion and delayed union by using a retrograde intramedullary interlocking nail. Chin J Traumatol. 2001;4(3):180–184. [PubMed] [Google Scholar]