Abstract
In this retrospective case series 80 patients divided in 40 matched pair groups with an arthroscopically proven ACL insufficiency were followed up for 15 years. One half was reconstructed using an autologous BTB patella graft, the other half was treated by a conservative physiotherapeutic based rehabilitation program. At follow-up the clinical scores (Lysholm, IKDC) showed no significant differences between subjects who had undergone ACL reconstruction and those who had not. Furthermore there was no detectable difference in the incidence of osteoarthritis between the cohorts. Patients having a negative pivot shift test showed significantly less signs of radiographic osteoarthritis and better functional assessment scores whether reconstructed or not. Based on these results and a review of the literature there is no clear evidence that ACL reconstruction reduces the rate of OA development or improves the long-term symptomatic outcome. Probably review of reconstruction by an anatomical approach will be more successful than operative techniques decades ago.
Introduction
Reconstruction of the ACL is a well-established procedure worldwide. It is estimated that more than 100,000 reconstructions are performed in the United States per year [1]. Even though the anterior cruciate reconstruction technique has provided high patient outcome success rates [2, 3], there are still patients complaining of persistent knee pain and instability [4]. Despite the fact that operative therapy is widely used there is still insufficient evidence to determine whether surgical or nonsurgical treatment is best for patients suffering from an anterior cruciate ligament injury [5]. Several treatment algorithms for the management of the anterior cruciate ligament injured knee have been proposed, none being superior to the other [6]. On the one hand well-designed investigations have documented potentially lower rates of subsequent meniscal and chondral injuries after surgical treatment, whereas on the other, the risk of secondary osteoarthritis (OA) remains high following operative reconstruction [7–10]. One of the main reasons for ligament reconstruction is to avoid a degenerative destruction of the joint cartilage. Even though degeneration of the joint increases over longer periods of time [11], investigations reporting the long-term results of ACL reconstructions are rare. Therefore the purpose of this retrospective study was to investigate the outcome of the ACL-injured patient treated by reconstruction with a patellar tendon autograft respectively undergoing a conservative physiotherapy-based rehabilitation program after a follow-up of 15 years. We postulated that patients willing to reduce their sportive activity and take part in a physiotherapy rehabilitation program have a similar long-term outcome as patients who have operative repair.
Patients and methods
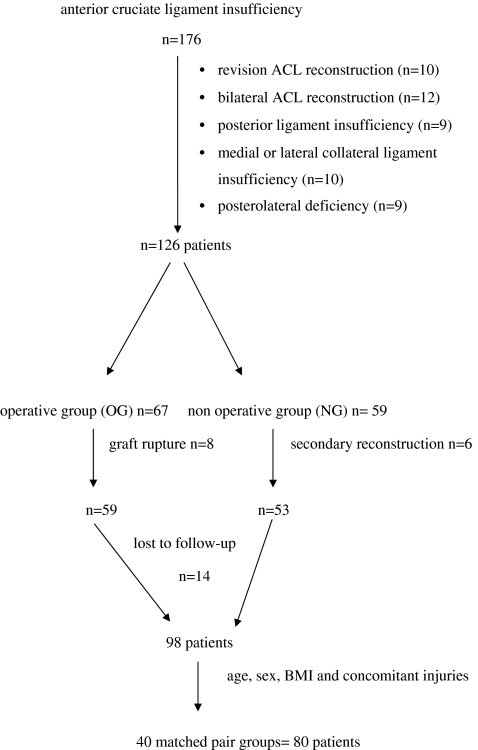
Between January 1990 and December 1992 a total of 176 patients who had an anterior cruciate ligament insufficiency were treated in our institution. Patients with bilateral ACL injury (n = 12), revision ACL reconstruction (n = 10) and other ligament pathologies associated with the ACL injury were excluded (Fig. 1). Therefore 126 patients were initially eligible to participate in the study.
Fig. 1.
Flowchart of patient selection
The decision for operative ACL reconstruction or conservative therapy was based on clinical and personal patient related factors. All patients were intensively informed on both treatment strategies. Operative management was chosen if the patient participated in sports at a professional level (n = 14), took part in sport activities including pivoting, cutting or sidestepping and were not willing to decrease the activity level (n = 29) or an explicit wish to have a primary ACL reconstruction (n = 24).
Therefore the ACL reconstructed group (ACL group) comprised 67 patients, while the non reconstructed group (non ACL group) consisted of 59 individuals. During the follow-up period graft rupture occurred in eight (12%) of the 67 patients in the reconstructed group. A secondary reconstruction for persistent instability was performed in six patients in the non reconstructed group (10%).
Despite extensive searches 12 patients could not be located, two died for unrelated reasons, leaving 98 patients as potential individuals. Out of this cohort 40 matched pair groups were built according to age, gender, BMI and concomitant injuries (Table 1).
Table 1.
Patient details
| Variable | ACL group (n = 40) | Non ACL group (n = 40) | Significance |
|---|---|---|---|
| Age (y) | 26.0 ± 6.3 (18-39) | 24.0 ± 6.5 (17–38) | n.s. |
| BMI | 23.3 ± 2.7 (19.5–29.1) | 22.8 ± 2,1 (19.0–30.2) | n.s. |
| Gender | 28 male | 28 male | n.s. |
| 12 female | 12 female | ||
| Interval between injury and beginning of treatment (months) | 7.3 ± 3.2 (2–29) | 5.8 ± 2.9 (0–24) | n.s. |
| Follow-up period (y) | 15.4 ± 0.76 (14–16) | 15.2 ± 0.69 (14–16) | n.s. |
| Meniscal injury (partial menisectomy) | 9 | 10 | n.s. |
| Activity causing injury | |||
| Skiing | 8 | 12 | p < 0.001 |
| Soccer | 11 | 11 | |
| Judo | 11 | 0 | |
| Other sports | 3 | 8 | |
| ADL | 7 | 9 | |
n.s. not significant
Values given as n or mean ± standard deviation (range)
Treatment algorithm
In all patients (ACL and non ACL group) a diagnostic arthroscopy and verification of a complete ACL tear was performed and the torn ACL was debrided. Meniscal status and the pattern of meniscal injury were recorded. Partial meniscectomy was performed in nine patients in the reconstructed group (23%), while ten patients underwent partial meniscectomy in the non reconstructed group (25%).
Operative ACL reconstruction (ACL group)
The central third of the patella (10 mm in width) was harvested through a single longitudinal incision. The graft was removed with a rectangular bone plug (20–25 mm in length). The tendon portion of the graft was freed from fat, and the bone blocks were trimmed to fit a 10-mm-diameter bone tunnel. An arthroscopic-assisted reconstruction was used. The torn ACL was debrided and the anatomical tibial and femoral footprints were identified and left intact. The tibial tunnel was drilled using a 55° drillguide under arthroscopic view through the posterior part of the middle of the tibial ACL footprint. To create the femoral tunnel a 5-mm offset guide system was placed transtibially at the posterior margin of the intercondylar notch. The patellar tendon autograft was passed through the tibial tunnel using an Ethibond pull through suture. Bone blocks were positioned in the tunnel and the autograft was placed with its cortical edge oriented posteriorly within the femoral tunnel. The femoral side was secured with a metal interference screw placed anteriorly to minimize graft tissue injury. After femoral fixation the affected knee was cycled several times to assess graft fixation and isometry, and final fixation was achieved by using a metal interference screw alongside the tibial bone block with the knee in 30° flexion applying manual tension to the sutures on the tibial bone plug. Postoperatively the patients were immobilised in a full extension plaster cast for the first 14 days. Range of motion of the knee and isometric muscle exercises were then started and gradually progressed on the basis of closed kinetic chain callisthenics. Knee flexion of more than 90° and full weight bearing was allowed two months postoperatively. Indoor cycling and swimming were permitted after eight weeks, running after and 16 weeks. High-demand pivoting sports activities were allowed after nine months.
Conservative treatment (non ACL group)
Immediately after arthroscopy the non reconstructed patients were referred in a neuromuscular based rehabilitation program supervised by a physical therapist. The aim was to regain joint mobility and knee stability. The PT started with closed kinetic chain exercises. As the subjective patients' stability improved, the activity level was increased. All non reconstructed patients were instructed to avoid high demand pivot shift activities such as downhill skiing, soccer and comparable sports.
Clinical assessment at follow-up
The final examination was performed by two independent and blinded observers (D.Z., G.B.). Both knees of the patient were covered with a stockinette to blind the operated side and the incisions. The side-to-side anterior laxity was measured using the KT-1000 knee arthrometer (MEDmetric Corporation, San Diego, CA, USA) with the knee at 20° and 60° flexion. An anterior displacement force of 134 N was applied for the tibia of both the injured and the normal uninjured leg. The differences were noted in millimeters. For overall evaluation the International Knee Documentation Committee (IKDC), Lysholm and Tegner activity scores were used.
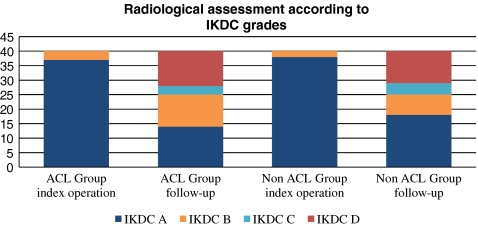
Radiological assessment
In both groups standard unilateral weight-bearing radiographic examinations in the anteroposterior view with the knee in 30° flexion and in lateral view were classified according to the IKDC guidelines as follows: A, normal; B, minimal changes and barely detectable joint space narrowing; C, moderate changes and joint space narrowing of up to 50%; and D, severe changes and more than 50% joint space narrowing. This grading has been shown to be reliable and reproducible with longitudinal data [12]. The radiographs were obtained twice, immediately after the index procedure and again at follow-up. According to a requirement of the local ethical committee, weight bearing radiographs of the contralateral limb could not be performed.
Statistics
All data were tested for normal distribution by means of the Kolmogorov-Smirnov test. Homogeneity of the variances was ascertained by Levene's F-test. A paired T-test and Fishers exact test were used to test the differences between the individual average values for significance. Correlation of the metric variables was tested with the aid of Pearson's correlation coefficient. We used the Wilcoxon signed-rank test to compare paired continuous variables. All tests were carried out in two directions and a p-value <0.05 was regarded as significant. Each of the box-and-whisker plots shows the first and third quartiles as the ends of the box, maximum and minimum as whiskers, and the median as a vertical line inside the box. Outliers are marked as individual separate values. The statistical evaluation was performed using SPSS 17.0 for Windows (SPSS Inc., Chicago, IL, USA)
This study was approved by the appropriate ethics committee (University of Heidelberg, Germany) and has therefore been performed in accordance with the ethical standards laid down in the 1975 Declaration of Helsinki. All persons gave their informed consent prior to their inclusion in the study.
Results
Demographic data
Both study cohorts comprised 80 patients, with an average age of 25.8 years (range 17–39 years) at the index operation. As shown in Table 1, no statistical differences were noted preoperatively between the two groups with regard to the age, BMI, gender, time from injury to operation, meniscal injuries treated by partial menisectomy nor time of follow-up.
Clinical examinations (pivot-shift, KT-1000, range of motion)
At 15-year follow-up there was no significant differences in the side-to-side anterior laxity measurement with the KT-1000 between both groups (20° flexion for the ACL group was 1.98 mm and for the non ACL group it was 2.12 mm, T-test p = 0.389; 60° flexion for the ACL group was 2.09 mm and for the non ACL group it was 2.23 mm, T-test p = 0.732). Despite a trend towards a better reconstruction of the rotation stability for the ACL group, as evaluated by the pivot shift, a significant correlation could not be noted (Fisher exact test p = 0.662). Of twenty patients reconstructed in the non ACL group 17 had a normal pivot shift and 23 (20 in ACL group) had a grade I rotation instability (Table 2).
Table 2.
Stability at Follow-up after 15 years
| Variable | ACL group (n = 40) | Non ACL group (n = 40) |
|---|---|---|
| KT 1000 side to side difference at 134 N at 20° flexion | ||
| <−1 mm | 0 | 0 |
| −1 to 3 mm | 14 | 12 |
| 3–5 mm | 25 | 15 |
| >5 mm | 1 | 3 |
| KT 1000 side to side difference at 134 N at 60° flexion | ||
| <−1 mm | 0 | 0 |
| −1 to 3 mm | 12 | 12 |
| 3–5 mm | 24 | 13 |
| >5 mm | 3 | 5 |
| Pivot shift sign | ||
| 0 | 20 | 17 |
| 1+ | 20 | 23 |
| 2+ | 0 | 0 |
| 3+ | 0 | 0 |
At follow-up 24 patients (11 ACL group, 13 non ACL group) showed an extension deficit between 3° and 5°. While eight individuals in the non ACL group had a flexion deficit of more than 6°, 17 reconstructed patients had a reduced flexion, which was significant (p < 0.05).
Overall evaluation (IKDC, Lysholm score, Tegner activity score)
We found no significant differences for the IKDC subjective (ACL group 69.9 ± 17.0; non ACL group 75.9 ± 13.1; p = 0.069) and the Lysholm score (ACL group 68.0 ± 19.8; non ACL group 75.5 ± 15.9; p = 0.066) at final follow-up between the two methods. Also, no differences were seen between both groups concerning the IKDC overall score. None of the patients were ranked as normal. Forty percent of the patients reconstructed with an autograft and 42.5% of the non reconstructed individuals were ranked as “nearly normal”, while 60% (ACL) and 57.5 % (non ACL), respectively, were “abnormal” or “severely abnormal”.
While there was no correlation between the functional clinical scores (IKDC and Lysholm score) and the anteriorposterior translation measured by the KT 1000 arthrometer, we found a significant relationship between the pivot shift and the clinical assessment scores. Patients having a negative pivot shift demonstrated significantly better results in the IKDC subjective and Lysholm score than patients having a rotational instability in the pivot shift test (p <0.001).
The evaluation of the Tegner activity score showed a significant decrease (p = 0.036) from 7.6 points ± 1.5 (range 6–10) preoperatively to 4.7 points ± 1.8 (range 3–7) postoperatively in the ACL group, and 7.1 points ± 1.4 (range 6–9) preoperatively versus 5.1 points ± 1.9 (range 3–6) postoperatively in the non ACL group. Even though the reduction was significant for both methods, no difference was seen between the groups.
Further surgical interventions
There was a significantly higher rate (Fisher exact test, p = 0.028) of subsequent meniscal surgery in the non ACL group compared to the ACL group. After a mean of 65 months (range 15–110), 16 individuals of the non-reconstructed cohort (40%) and four patients initially reconstructed (mean 71 months, range 21–80) underwent a secondary partial menisectomy (10%).
Radiological examination
According to the IKDC guidelines there was a significant aggravation (Wilcoxon test p < 0.001) in the radiographic grading in both groups. As shown in Table 3 25 knees in the ACL group (62.5%) and 22 patients in the non ACL group (55%) altered the radiological OA grade during follow-up time. To assess the relative contributions of age, BMI, gender, functional outcome, time from injury to index operation, initial or secondary meniscal surgery, KT-1000 and pivot shift a statistical analysis was performed. While no correlation was found for age, BMI, gender, time from injury to initial surgery, primary and subsequent meniscal surgery, functional outcome or the KT-1000 arthrometer, there was a significant relationship between a positive pivot shift at follow-up and the radiographic grading of OA (p < 0.001).
Table 3.
Radiological assessment according to IKDC grades
Discussion
In this retrospective case series 80 patients divided in to 40 matched pair groups with arthroscopically proven ACL insufficiency were followed for 15 years. One half was reconstructed by an autologous BTB patella graft, the other half was treated by a conservative physiotherapy-based rehabilitation program.
Although it is claimed that surgical treatment is better to restore overall knee function [13], the clinical results in our investigation were comparable for both treatment options. The applied self-reported assessment scores showed no significant differences between subjects who had undergone ACL reconstruction and those who had not. This finding was in line with the results published by the Cochrane group in 2005 [5]. This systematic review could not demonstrate any evidence from randomised trials to determine whether surgery or conservative management was best for ACL injury. Also they could not quote any evidence to inform current practice. In contrast to their report and other previously published investigations the mean Lysholm score was lower in both of our treatment cohorts. While Salmon et al. [11] showed good to excellent Lysholm knee scores in 80% of their patients, with a mean score of 89 points after 13 years of follow-up undergoing endoscopic ACL reconstruction, the present Lysholm mean was 68 points for our ACL reconstructed patients. Also our non reconstructed patients scored less than in comparable investigations. Kostogiannis et al. [14] reported good functional scores in their conservatively-treated patients at the 15 year follow-up. As a large number of studies have reported on clinical assessment after ACL insufficiency but only few extend beyond ten years of follow-up [13], we can just speculate on a potential influence of time as there is certain evidence of a significant deterioration of the clinical scores over time [11, 12]. Interestingly, the self-reported activity level graded according to Tegner had a mean of 4 for ACL and 5 for non-ACL and was therefore higher than in comparable studies [11, 12]. This could possibly indicate that the high proportion of fair results may be an expression of non acceptance of a lower activity level rather than evidence of a truly impaired knee function.
Another important finding of the present investigation was the influence of rotational stability on the incidence of osteoarthritis and the functional subjective outcome. Patients having a negative pivot shift test showed significantly less signs of radiographic osteoarthritis and better functional assessment scores independent of reconstruction. This is in line with the results published by Jonsson et al. [15] who suggested a positive pivot shift test as predictor of later osteoarthritis based on the results of a long-term radiographic evaluation. Also Kocher et al. reported a significant relationship between the pivot shift test grades and patient satisfaction, whereas anterior posterior laxity did not have influence on patient subjective assessment two years postoperatively [16]. In view of these observations it seems to be clear that one of the main targets of any outcome evaluation of ACL treatment should be the precise documentation of transverse plane rotatory stability. But as there is a variety of possible tools for measuring the rotational stability in the lab, the manual pivot shift test still remains the only validated parameter in the daily clinical routine. Even if there is an attempt of an objective quantitative measurement by several technical devices [17–20], objective quantitative assessment of the pivot shift phenomenon is currently lacking and the evaluation greatly depends on the examiner’s subjective experience and impression [21, 22]. Therefore, accurate assessment of the pivot shift is essential to obtain an exact clinical assessment of ACL-deficient or reconstructed knee.
Furthermore, there was no detectable difference in the incidence of osteoarthritis between the cohorts. This finding was in line with the literature as there are no published data supporting a preventive effect of reconstructive ACL surgery against osteoarthritis. On the contrary, a study by Daniel et al. showed a trend towards a greater prevalence of osteoarthritis in surgically-treated than in non-surgically treated patients [7]. Also Kessler et al. reported on a significantly higher rate of osteoarthritis in patients 11 years following an operative treatment of ACL insufficiency [23]. In contrast to our investigation they excluded patients with meniscal injuries or chondral lesions, which rarely occur [24]. Although there are several publications [13, 25] showing a negative influence of meniscal resection on the incidence of osteoarthritis, this was not seen in our cohort. Even though there was a significantly higher rate of subsequent meniscal surgery in the non ACL group (40%) compared to the ACL group (10%), no correlation between the index operation and the amount of radiographic joint degeneration at follow-up was observed. There may be several reasons for this. One could be that in both treatment groups the percentage of degenerative changes was high and therefore statistical differences due to the restricted numbers of patients was probably too low. Another might be that the surgical treatment of subsequent meniscal injuries occurred after a mean of 65 months and the follow-up period until the present study was performed might be too short to develop significant radiographic aggravation of OA.
Mainly due to its retrospective design this study has several limitations. The main focus of our investigation was to evaluate the long-term outcome. Therefore, we are unable to provide any clinical or radiological data for the short- or midterm results of our patients. So it is unclear if one of our cohorts is superior to the other in the chronological sequence of clinical or radiological parameters. Furthermore inexact documentation of parameters may lead to a certain bias. Despite this fact we believe that due to strict study and inclusion criteria and a high follow-up rate this potential error could be negligible.
Based on our results and a review of the literature there is no clear evidence that ACL reconstruction reduces the rate of OA development or improves the long-term symptom outcome [5, 13]. As degeneration of the joint increases over longer periods of time [11], there is a need for well designed investigations reporting on long-term results of ACL reconstructions. Probably review of reconstruction by an anatomical approach will be more successful than operative techniques decades ago.
References
- 1.Griffin LY, Agel J, Albohm MJ, et al. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8(3):141–150. doi: 10.5435/00124635-200005000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Aglietti P, Giron F, Buzzi R, Biddau F, Sasso F. Anterior cruciate ligament reconstruction: bone-patellar tendon-bone compared with double semitendinosus and gracilis tendon grafts. A prospective, randomized clinical trial. J Bone Joint Surg Am. 2004;86-A(10):2143–2155. [PubMed] [Google Scholar]
- 3.Freedman KB, D'Amato MJ, Nedeff DD, Kaz A, Bach BR., Jr Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003;31(1):2–11. doi: 10.1177/03635465030310011501. [DOI] [PubMed] [Google Scholar]
- 4.Buoncristiani AM, Tjoumakaris FP, Starman JS, Ferretti M, Fu FH. Anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2006;22(9):1000–1006. doi: 10.1016/j.arthro.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 5.Linko E, Harilainen A, Malmivaara A, Seitsalo S (2005) Surgical versus conservative interventions for anterior cruciate ligament ruptures in adults. Cochrane Database Syst Rev 18(2):CD001356 [DOI] [PubMed]
- 6.Fithian DC, Paxton EW, Stone ML, Luetzow WF, Csintalan RP, Phelan D, Daniel DM. Prospective trial of a treatment algorithm for the management of the anterior cruciate ligament-injured knee. Am J Sports Med. 2005;33(3):335–346. doi: 10.1177/0363546504269590. [DOI] [PubMed] [Google Scholar]
- 7.Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient a prospective outcome study. Am J Sports Med. 1994;22(5):632–644. doi: 10.1177/036354659402200511. [DOI] [PubMed] [Google Scholar]
- 8.Asano H, Muneta T, Ikeda H, Yagishita K, Kurihara Y, Sekiya I. Arthroscopic evaluation of the articular cartilage after anterior cruciate ligament reconstruction: a short-term prospective study of 105 patients. Arthroscopy. 2004;20(5):474–481. doi: 10.1016/j.arthro.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 9.Fink C, Hoser C, Hackl W, Navarro RA, Benedetto KP. (2001) Long-term outcome of operative or nonoperative treatment of anterior cruciate ligament rupture—is sports activity a determining variable? Int J Sports Med. 2001;22(4):304–309. doi: 10.1055/s-2001-13823. [DOI] [PubMed] [Google Scholar]
- 10.Myklebust G, Holm I, Maehlum S, Engebretsen L, Bahr R. Clinical, functional, and radiologic outcome in team handball players 6 to 11 years after anterior cruciate ligament injury: a follow-up study. Am J Sports Med. 2005;31(6):981–989. doi: 10.1177/03635465030310063901. [DOI] [PubMed] [Google Scholar]
- 11.Salmon LJ, Russell VJ, Refshauge K, Kader D, Connolly C, Linklater J, Pinczewski LA. Long-term outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft: minimum 13-year review. Am J Sports Med. 2006;34(5):721–732. doi: 10.1177/0363546505282626. [DOI] [PubMed] [Google Scholar]
- 12.LaValley MP, McAlindon TE, Chaisson CE, Levy D, Felson DT. The validity of different definitions of radiographic worsening for longitudinal studies of knee osteoarthritis. J Clin Epidemiol. 2001;54(1):30–39. doi: 10.1016/S0895-4356(00)00273-0. [DOI] [PubMed] [Google Scholar]
- 13.Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007;35(10):1756–1769. doi: 10.1177/0363546507307396. [DOI] [PubMed] [Google Scholar]
- 14.Kostogiannis I, Ageberg E, Neuman P, Dahlberg L, Fridén T, Roos H. Activity level and subjective knee function 15 years after anterior cruciate ligament injury: a prospective, longitudinal study of nonreconstructed patients. Am J Sports Med. 2007;35(7):1135–1143. doi: 10.1177/0363546507299238. [DOI] [PubMed] [Google Scholar]
- 15.Jonsson H, Riklund-Ahlstrom K, Lind J. Positive pivot shift after ACL reconstruction predicts later osteoarthrosis: 63 patients followed 5–9 years after surgery. Acta Orthop Scand. 2004;75(5):594–599. doi: 10.1080/00016470410001484. [DOI] [PubMed] [Google Scholar]
- 16.Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ. Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32(3):629–634. doi: 10.1177/0363546503261722. [DOI] [PubMed] [Google Scholar]
- 17.Kubo S, Muratsu H, Yoshiya S, Mizuno K, Kurosaka M. Reliability and usefulness of a new in vivo measurement system of the pivot shift. Clin Orthop Relat Res. 2007;454:54–58. doi: 10.1097/BLO.0b013e31802b4a38. [DOI] [PubMed] [Google Scholar]
- 18.Monaco E, Labianca L, Conteduca F, Carli A, Ferretti A. Double bundle or single bundle plus extraarticular tenodesis in ACL reconstruction? A CAOS study. Knee Surg Sports Traumatol Arthrosc. 2007;15(10):1168–1174. doi: 10.1007/s00167-007-0368-y. [DOI] [PubMed] [Google Scholar]
- 19.Ristanis S, Stergiou N, Patras K, Vasiliadis HS, Giakas G, Georgoulis AD. Excessive tibial rotation during high-demand activities is not restored by anterior cruciate ligament reconstruction. Arthroscopy. 2005;21(11):1323–1329. doi: 10.1016/j.arthro.2005.08.032. [DOI] [PubMed] [Google Scholar]
- 20.Ristanis S, Giakas G, Papageorgiou CD, Moraiti T, Stergiou N, Georgoulis AD. The effects of anterior cruciate ligament reconstruction on tibial rotation during pivoting after descending stairs. Knee Surg Sports Traumatol Arthrosc. 2003;11(6):360–365. doi: 10.1007/s00167-003-0428-x. [DOI] [PubMed] [Google Scholar]
- 21.Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1(3–4):226–234. doi: 10.1007/BF01560215. [DOI] [PubMed] [Google Scholar]
- 22.Jakob RP, Staubli HU, Deland JT. Grading the pivot shift. Objective tests with implications for treatment. J Bone Joint Surg Br. 1987;69-Br(2):294–299. doi: 10.1302/0301-620X.69B2.3818763. [DOI] [PubMed] [Google Scholar]
- 23.Kessler MA, Behrend H, Henz S, Stutz G, Rukavina A, Kuster MS. Function, osteoarthritis and activity after ACL-rupture: 11 years follow-up results of conservative versus reconstructive treatment. Knee Surg Sports Traumatol Arthrosc. 2008;16(5):442–448. doi: 10.1007/s00167-008-0498-x. [DOI] [PubMed] [Google Scholar]
- 24.Finsterbush A, Frankl U, Matan Y, Mann G. Secondary damage to the knee after isolated injury of the anterior cruciate ligament. Am J Sports Med. 1990;18(5):475–479. doi: 10.1177/036354659001800505. [DOI] [PubMed] [Google Scholar]
- 25.Joseph C, Pathak SS, Aravinda M, Rajan M. Is ACL reconstruction only for athletes? A study of the incidence of meniscal and cartilage injuries in an ACL-deficient athlete and non-athlete population: an Indian experience. Int Orthop. 2008;32(1):57–61. doi: 10.1007/s00264-006-0273-x. [DOI] [PMC free article] [PubMed] [Google Scholar]