Abstract
Treatment of reverse oblique trochanteric femoral fractures is still challenging. We present the results of our proximal nailing surgery performed for reverse obliquity intertrochanteric fractures using two lag screws and evaluated the quality of the reduction, operative time, complications and functional status of the patients. Fifteen patients with AO/OTA 31 A-A3 fractures were treated by proximal femoral nailing in our trauma centre. The mean Harris hip score was 74.66 (range 65–96) and the mean Barthel activity score was 15.71 (range 12–20). The mean duration of surgery was 48 minutes and the average consolidation time was 8.6 weeks. No intraoperative complications or postoperative technical failures and no stress shielding as evidenced by the lack of cortical hypertrophy at the level of the tip of the implant were detected. Intramedullary nailing with proximal femoral nails may be a good option in the treatment of reverse obliquity intertrochanteric fractures.
Introduction
The incidence of fractures in the proximal femoral area has risen with the increasing numbers of elderly persons with osteoporosis and traffic accidents in young adults.
Fractures about the trochanteric area are classified according to the Orthopaedic Trauma Association classification system as AO/OTA 31-A, which delineates them as extracapsular fractures of the hip. These fractures are subdivided into groups A1, A2 and A3. A1 fractures are simple, two part fractures, whereas A2 fractures have multiple fragments. A3 fractures include reverse oblique and transverse fracture patterns.
There are two main types of implant available for the treatment of these fractures, namely, extramedullary and intramedullary implants [1–3]. Although the most widely used extramedullary implant is the dynamic hip screw, which consists of a sliding neck screw connected to a plate in the lateral femoral cortex, most authors have reported that this device is not suitable for AO/OTA 31-A3 reverse oblique or transverse fractures due to high incidence of fixation failures. Thus, the treatment of these unstable trochanteric femoral fractures is still challenging, and clinical reports regarding intramedullary hip nailing for reverse obliquity intertrochanteric fractures are few in number [3–10].
In our study, we present the results of our proximal nailing surgery performed for reverse obliquity intertrochanteric fractures using two lag screws, and include evaluation of the quality of the reduction, operative time, complications and functional status of the patients.
Materials and methods
From 2006 to 2008, 15 patients with AO/OTA 31 A-A3 fractures were treated by proximal femoral nailing in our trauma centre. Our unit is familiar with the use of proximal femoral nailing for the treatment of all trochanteric fractures.
The PROFIN (TST SAN, Istanbul, Turkey) is a cannulated straight tube made of titanium alloy, with a proximal curvature of 6 degrees and a distal slotted design, intended to decrease the risk of intraoperative and postoperative fractures of the shaft by a significant reduction in bone stress. The proximal part of the nail is 16 mm in diameter and has two oblique lag screws with diameters of 8.5 mm. The neck shaft angle of the nail is 135 degrees, and it has two distal holes that allow either dynamic or static fixation. The transverse locking screw at the distal end of the PFN has a diameter of 4.5 mm. All operations were performed within 4.45 days of injury and closed reduction was achieved in 13 cases. We classified the quality of reduction as anatomical (<5 degrees of varus, valgus, anteversion or retroversion), acceptable (5–10 degrees) or poor (>10 degrees) [11]. The fracture was determined to have healed when the fracture was filled with callus and the patient did not feel any pain at the fracture site [12]. Postoperatively, the patients were allowed to bear as much weight as they could tolerate. During a mean of 12.36 months (range 12–22), the results, as well as the intraoperative and postoperative complications, were noted. All patients were evaluated by regular physical and radiographic examinations. Clinical and functional outcomes were assessed according to Harris hip score and Barthel activity score, respectively. The mean age of our patients was 62 years (range 21–93) and nine (60%) of them were men. Ten fractures were right-sided and five were left. Of the 15 fractures, six were 31-A3-1, five were 31-A3-2 and four were 31-A3-3. The mean duration of surgery was 48 minutes. Thirteen patients were operated upon on a fracture table in supine position and two patients on a radiolucent table in lateral decubitus position. We used two screws distally in three patients and one screw in 12 patients. Cut-out, Z-effect or reversed Z-effect of the lag screws were scored as technical failures.
Results
There were acceptable reductions in two (13.33%) patients and anatomical reductions in 13 (%86.67) patients. The mean Harris hip score was 74.66 (range 65–96) and the mean Barthel activity score was 15.71 (range 12–20). Nine patients had excellent results, four had good results and two had poor results according to Harris hip score; two had low range, two patients had a median range and 11 patients had a high range of mobility according to the Barthel activity score. The mean duration of surgery was 48 minutes. The fractures healed in all patients; the average consolidation time was 8.6 weeks (range 7–13). No intraoperative complications or postoperative technical failures and no stress shielding as evidenced by the lack of cortical hypertrophy at the level of the tip of the implant were detected.
The initial and follow-up radiographs of a sample case are presented in Figs. 1, 2, 3.
Fig. 1.
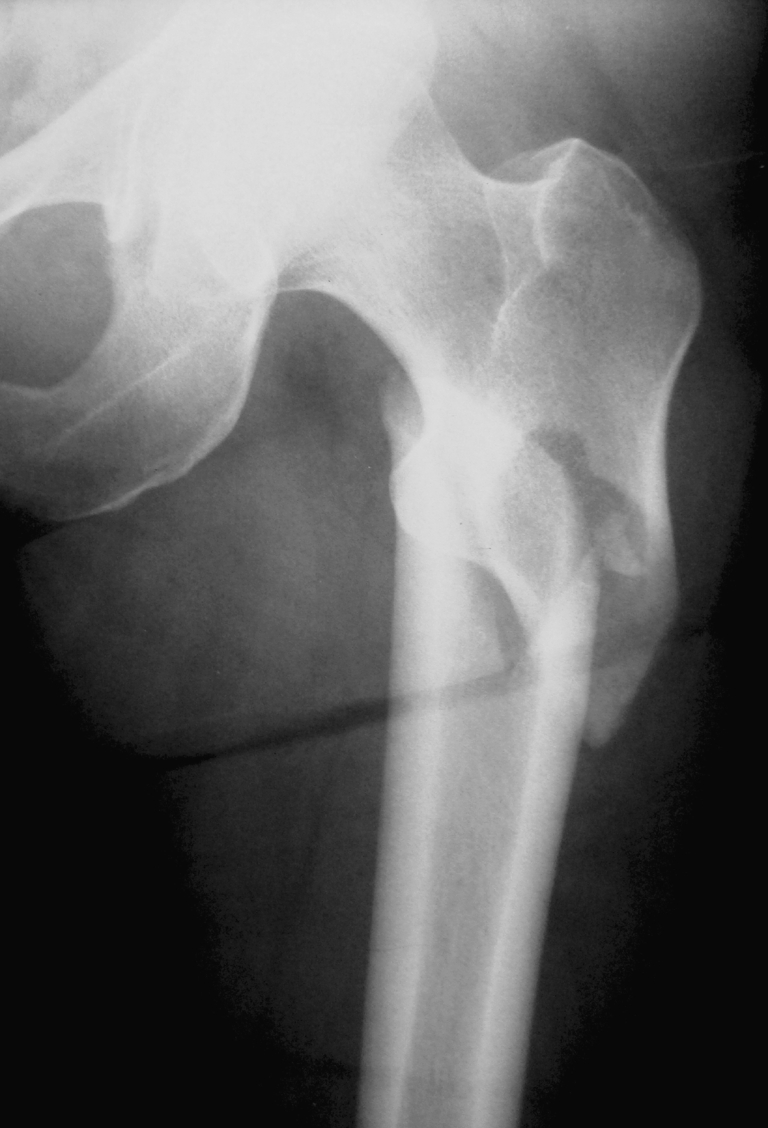
Preoperative anterior-posterior proximal femur X-ray of the sample case
Fig. 2.

Early postoperative anterior-posterior proximal femur X-ray of the sample case
Fig. 3.
Anterior-posterior (a) and lateral (b) X-rays of the proximal femur at the postoperative ninth week
Discussion
Trochanteric fractures are one of the most important causes of mortality and morbidity, especially in the elderly population. Early surgical stabilisation of the fractures is important to reduce complications associated with long-term immobilisation and to decrease mortality risk [1, 2, 6, 11, 13, 14].
Reverse obliquity intertrochanteric fractures are unstable with unique anatomical and mechanical characteristics. Weight on the fractured limb generates a shearing movement at the fracture side and results in telescoping of the implant, especially in sliding hip screw fixation. These fractures therefore pose a great challenge to both patients and orthopaedic surgeons. Although the intramedullary fixation has a biomechanical advantage of shorter lever arm compared to extramedullary implants, clinical reports of intramedullary nailing for reverse obliquity and unstable fractures are very limited in number [15, 16].
Min et al. [7] reported migration of femoral neck screw and hip pin in four of 21 cases in their PFN group and three of them required revision surgery. Hernandez et al. reported nail displacement in three of their 47 patients treated for reverse oblique intertrochanteric femur fractures with the gamma nail. In addition, high failure rates were found in treating fractures with the reverse oblique intertrochanteric pattern using the 95° screw plate.
We found that using two proximal lag screws could provide better rotational control of the femoral head fragment and decrease the cut-out of the femoral head by prevention of head fragment toggling. Anatomical reduction is also extremely important; especially varus malalignment should be avoided to prevent implant failure.
In this kind of fracture we have not used cerclage wire fixation of the fragments to preserve blood supply to bone and avoid damage the periosteum, which is the integral part for bone healing.
It may also be important to place the inferior lag screw as close as possible to the inferior femoral neck cortex on AP view and both screws as close as possible to the central part of the femoral head to create a stable fixation and to prevent varus collapse of the femoral head [17].
Recently, we have started to use only distal dynamic stabilisation of the proximal femoral nail to prevent breakage of femur at the screw insertion side, which may act as a stress riser.
Limitations of our study are lack of control group and relatively small patient population, but these are uncommon fractures accounting for 5–23% of all trochanteric fractures even in the centralised trauma centres.
In conclusion, intramedullary nailing with proximal femoral nails consisting of two proximal lag screws may be a good option in the treatment of reverse obliquity intertrochanteric fractures if attention is given to ensure correct technique during nail insertion. First, the fracture has to be reduced before passing the intramedullary nail. The correct entry point for the nail, that is, the tip of the greater trochanter on the anteroposterior and in line with the femoral neck on the lateral view, should be achieved and distraction should be avoided during insertion of the nail. Any excessive anterior bow of the femoral shaft should be determined preoperatively by obtaining a lateral view of the femur to avoid penetration the anterior femoral cortex, especially when using a straight nail without a slotted distal end [18, 19]. In case of severe osteoporosis that interferes with proximal screw fixation, screws augmented with cement may be used to increase stability [20].
Despite correct technical application, complications such as varus angulation of the proximal fragment and medialisation of the distal fragment during nail insertion, which may necessitate open reduction, may occur. Excessive loading of the femur may also occur due to distraction between the proximal and distal fragments that may cause stress fracture of the nail. This can be prevented with dynamic stabilisation or distal stabilisation of the nail after releasing the traction.
Acknowledgments
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.Domingo L, Cecillia D, Herrera A, et al. Trochanteric fractures treated with a proximal femoral nail. Int Orthop. 2001;25:298–301. doi: 10.1007/s002640100275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haldar SC. The Gamma nail for pertrochanteric fractures. J Bone Joint Surg. 1992;74-B:340–344. doi: 10.1302/0301-620X.74B3.1587873. [DOI] [PubMed] [Google Scholar]
- 3.Leung KS, So WS, Shen WY, et al. Gamma nails and dynamic hip screws for pertrochanteric fractures. J Bone Joint Surg. 1992;74-B:345–351. doi: 10.1302/0301-620X.74B3.1587874. [DOI] [PubMed] [Google Scholar]
- 4.Banan H, Al-Sabti A, Jimulia T, et al. The treatment of unstable extracapsuler hip fractures with AO/ASIF proximal femoral nail (PFN)—our first 60 cases. Injury. 2002;33:401–405. doi: 10.1016/S0020-1383(02)00054-2. [DOI] [PubMed] [Google Scholar]
- 5.Boldin C, Seibert FJ, Frankhauser F, et al. The proximal femoral nail (PFN)—a minimal invasive treatment of unstable proximal femoral fractures: a prospective study of 55 patients with a follow-up of 15 months. Acta Orthop Scand. 2003;74:53–58. doi: 10.1080/00016470310013662. [DOI] [PubMed] [Google Scholar]
- 6.Kregor PJ, Obremsky WT, Kreder HI, et al. Evidence-based orthopaedic trauma working group. Unstable pertrochanteric femoral fractures. J Orthop Trauma. 2005;19:63–66. doi: 10.1097/00005131-200501000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Min WK, Kim SY, Kim TK, et al. Proximal femoral nail for the treatment of reverse obliquity intertrochanteric fractures compared with gamma nail. J Trauma. 2007;63:1054–1060. doi: 10.1097/01.ta.0000240455.06842.a0. [DOI] [PubMed] [Google Scholar]
- 8.Park SY, Yang KH, Yoo JH, et al. The treatment of reverse obliquity intertrochanteric fractures with the intramedullary hip nail. J Trauma. 2008;65:852–857. doi: 10.1097/TA.0b013e31802b9559. [DOI] [PubMed] [Google Scholar]
- 9.Sadowski C, Lübbeke A, Saudan M, et al. Treatment of reverse oblique and transverse intertrochanteric fractures with use of an intramedullary nail or a 95 degrees screw-plate: a prospective, randomized study. J Bone Joint Surg. 2002;84-A:372–381. [PubMed] [Google Scholar]
- 10.Werner W, Llajter G, Schmiedhuber G. Intra-und Komplikationen bei der Stabilisienung von Per- und Subtrochantaren Femur Fracturen Mittels PFN. Unfallchirurg. 2002;105:881–885. doi: 10.1007/s00113-002-0416-5. [DOI] [PubMed] [Google Scholar]
- 11.Ozkan K, Unay K, Demirçay C, et al. Distal unlocked proximal femoral intramedullary nailing for intertrochanteric femur fractures. Int Orthop. 2009;33:1397–1400. doi: 10.1007/s00264-008-0673-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mc Kibbin B. The biology of fracture healing in long bones. J Bone Joint Surg. 1978;60-B:150–162. doi: 10.1302/0301-620X.60B2.350882. [DOI] [PubMed] [Google Scholar]
- 13.Simmermacher RK, Boch AM, Werken V, et al. The AO/ASIF proximal femoral nail (PFN): new device for treatment of unstable proximal femoral fractures. Injury. 1999;30:327–332. doi: 10.1016/S0020-1383(99)00091-1. [DOI] [PubMed] [Google Scholar]
- 14.Tyllianakis M, Panagopoulos A, Papadopoulos A, et al. Treatment of extracapsuler hip fractures with the proximal femoral nail (PFN): long term results in 45 patients. Acta Orthop Belg. 2004;70:444–454. [PubMed] [Google Scholar]
- 15.Utrilla AL, Reig JS, Muñoz FM, Tufanisco CB. Trochanteric gamma nail and compression hip screw for trochanteric fractures: a randomized, prospective, comparative study in 210 elderly patients with a new design of the gamma nail. J Orthop Trauma. 2005;19:229–233. doi: 10.1097/01.bot.0000151819.95075.ad. [DOI] [PubMed] [Google Scholar]
- 16.Palm H, Jacobsen S, Sonne-Holm S, Gebuhr P, Hip Fracture Study Group Integrity of the lateral femoral wall in intertrochanteric hip fractures: an important predictor of a reoperation. J Bone Joint Surg Am. 2007;89:470–475. doi: 10.2106/JBJS.F.00679. [DOI] [PubMed] [Google Scholar]
- 17.Lin J. Encouraging results of treating femoral trochanteric with specially designed double-screw nails. J Trauma. 2007;63:866–874. doi: 10.1097/TA.0b013e3180342087. [DOI] [PubMed] [Google Scholar]
- 18.Haidukewych GJ. Intertrochanteric fractures: ten tips to improve results. J Bone Joint Surg Am. 2009;91:712–719. [PubMed] [Google Scholar]
- 19.Kaplan K, Miyamoto R, Levine BR, et al. Surgical management of hip fractures: an evidence-based review of the literature. II: intertrochanteric fractures. J Am Acad Orthop Surg. 2008;16:665–673. doi: 10.5435/00124635-200811000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Alexa O, Cozma T. Compression hip screw fixation with bone cement in trochanteric fractures. Rev Med Chir Soc Med Nat Iasi. 2004;108:416–419. [PubMed] [Google Scholar]



