Abstract
We postulated that the lowest instrumented vertebra (LIV) can be determined based on the apical vertebra. Seventy-two Lenke type 1 patients (average age: 13.6 years) receiving posterior spinal fusion were randomised into two groups. In group A, the apical vertebra was used to determine the LIV and in group B the neutral vertebra was used. All patients had Cobb angles <90° and average follow-up was over three years. Posteroanterior and lateral standing radiographs were used to assess flexibility, Cobb angle and distance from the C7 line to the central sacral vertical line. Both methods produced statistically significant changes in Cobb angle, sagittal T5–T12 and plumb line deviation, and there were no significant differences between the two methods. More cases of imbalance occurred in group B (five) than group A (two). We conclude that the apical vertebra can be used to determine the LIV in patients with Lenke type 1 adolescent idiopathic scoliosis.
Introduction
The aims of surgical treatment for adolescent idiopathic scoliosis (AIS) are to correct the deformity in the coronal plane, to restore balance in the sagittal plane, to derotate the spinal column and to fuse as few spinal segments as possible. Loss of balance after surgery leads to complications [1, 3, 6], and the most important factor causing loss of balance is selection of the wrong segments for fusion, especially selecting the wrong lowest instrumented vertebra (LIV) [7, 12]. Different evaluation standards, however, lead to variability in the choice of fusion segments.
At present, most surgeons believe that a coronal Cobb angle of more than 40 or 45° is a clear indication for surgical treatment of scoliosis, but the best method for choosing the most appropriate LIV in a posterior fusion for Lenke type 1 scoliosis is still debated [4]. Newer systems are able to correct for rotation as well as curvature and allow a shorter fusion length [2, 4, 10]. Lenke considered that fusion was required for Lenke type 1 curves in AIS, but did not clearly define the segments to be fused [5, 6]. A method commonly used to determine fusion length with newer instrumentation that uses the end vertebra and the neutral vertebra was devised by Suk et al. [11]. However, the selection of these two vertebrae is not very precise, as study has shown that observers agree on the exact vertebral level of each of these two parameters only 50% of the time [8], probably because the method used to select the vertebrae is somewhat indirect.
Another parameter determined during the treatment of AIS is the apical vertebra, i.e. the vertebra in the major curve that is parallel to the vertical axis and whose distance from the plumb line shows the horizontal extent of the curve [9]. The apical vertebra can be determined more accurately than the end or neutral vertebrae. We postulated that the apical vertebra can substitute for the neutral vertebrae in determining the LIV in patients with AIS undergoing spinal fusion. Thus, the aim of this prospective case-matched study was to compare the outcomes of using the neutral vertebra versus the apical vertebra to determine the LIV in patients with AIS undergoing posterior spinal fusion.
Patients and methods
In total, 72 patients with AIS and Lenke type 1 curves were recruited into this prospective case-matched study. The study was approved by Institutional Review Board of our hospital and informed consent was obtained for all patients. The average patient age was 13.6 years (range: 11.2–16.3 years) and the average follow-up time was more than three years (range: 2.1–4.6 years). All patients had Cobb angles <90° and leg lengths were equal in all patients.
The patients were divided into two groups, an apical vertebra method group (group A) and a neutral vertebra method group (group B), with 36 patients in each group; thus, the groups were matched 1:1 with respect to method of LIV determination. No matching was performed with respect to patient age, Risser sign, scoliosis in the coronal plane or kyphosis angle in the sagittal plane. All radiographs were assessed by two surgeons having the same clinical experience in AIS surgery and the same standards for reading the radiographs. Determination of the apical vertebra, end vertebra, etc. was made by agreement of the two surgeons. Thus, the evaluation standard in this study was uniform and the identification of the stable and neutral vertebrae by the two surgeons was similar to that in clinical practice. The neutral vertebra is the most cephalad vertebra inferior to the apex of the distal structural curve, the pedicles of which are symmetrically situated (neutral rotation) within the vertebral body. The apical vertebra is the most cephalad vertebra below the end vertebra of the distal structural curve, which is most closely bisected by the central sacral vertical line (CSVL).
Preoperatively, posteroanterior and lateral standing radiographs were used to assess curvatures and left and right lateral bending radiographs were used to assess flexibility. Radiographs in the standing position were taken at the last follow-up to assess deformity correction and spinal balance. The Cobb angle of the scoliosis was measured and the diagnostic criteria for loss of balance in the coronal plane was defined as a distance from the C7 vertical line to the CSVL >2 cm. Disc wedging was not evaluated in this study.
In group A, the LIV was selected based on the vertebral level of the apical vertebra as follows: T11 was selected if the apical vertebra was the vertebral body of the T6–T6/7 intervertebral space (2 cases); T12 was selected if the apical vertebra was the vertebral body of T7 or T8 (15 cases); L1 was selected if the apical vertebra was the T8/9 intervertebral space or the vertebral body of T10.
In group B, the LIV was selected using the method of Suk et al. [11]. The neutral vertebra was selected as the LIV when the neutral vertebra was identical to the end vertebra or one level distal; the vertebra one level above the neutral vertebra was selected as the LIV when the neutral vertebra was two or more levels distal to the end vertebra.
All patients underwent posterior fixation and fusion in the period from 2003 to 2006. None of the patients had anterior release nor was thoracoplasty performed. Hybrid hook/screw instrumentation was used for 21 cases and pedicle screw fixation for 51 cases. One or two screws were inserted for every two vertebrae, or screws were placed for each vertebra in the correction side. The superior vertebra of the apical vertebra was the upper level of instrumentation. Bone grafting using either autologous (harvested from the iliac crest) or homologous (femoral epiphysis harvested from our Bone Bank) was carried out at the same time as placement of the internal fixation instruments. During surgery, spinal cord integrity was monitored in all patients using somatosensory evoked potential. The instrumentation used included Cotrel-Dubousset-Hopf (CDH), Moss Miami (DePuy Spine, Inc., Raynham, MA, USA) and Isola (DePuy Spine, Inc., Raynham, MA, USA).
Statistical analysis
To determine any baseline differences, groups were compared using independent two-sample t tests. The Mann-Whitney U test was performed to determine the baseline group difference in the Risser sign. Paired t tests in both groups were employed to analyse the results of differences in outcome parameters (Cobb angle, sagittal T5–T12, plumb line deviation from the CSVL) between before and after surgery. Independent two-sample t tests were used to detect pre- and postoperative differences in outcome measurements. Continuous data were presented as mean ± standard deviation and categorical data as number and percentage. Statistical analyses were performed using SPSS 15.0 statistics software (SPSS Inc., Chicago, IL, USA). All statistical assessments were two-sided and P < 0.05 was considered to indicate statistical significance.
Results
Demographic and preoperative data of the two groups of patients are presented in Table 1. Due to the matching process, the apical, end and neutral vertebrae were similar in the two groups. Both groups included Lenke type A, B and C curvatures (data not shown). There were no significant differences between the two groups in age, Risser sign, duration of follow-up, preoperative side-bending values, Cobb angle, sagittal T5–T12, T10–L2 Cobb angle, LIV tilt or plumb line deviation from the CSVL (all P > 0.05).
Table 1.
Patient demographic and preoperative data
| Group A (n = 36) | Group B (n = 36) | P value | |
|---|---|---|---|
| Apical vertebra | |||
| T6–T6/7 | 2 (5.6%) | 2 (5.6%) | Matched design |
| T7–T8 | 15 (41.7%) | 15 (41.7%) | |
| T8/9–T10 | 19 (52.7%) | 19 (52.7%) | |
| Neutral vertebra | |||
| L1–L3 | 24 (66.7%) | 24 (66.7%) | Matched design |
| T10–T12 | 12 (33.3%) | 12 (33.3%) | |
| Age (years)a | 13.56 ± 1.17 | 13.70 ± 1.34 | 0.648 |
| Risser signb | |||
| 0 | 3 (8.3%) | 2 (5.6%) | 0.967 |
| 1 | 1 (2.8%) | 1 (2.8%) | |
| 2 | 6 (16.7%) | 8 (22.2%) | |
| 3 | 12 (33.3%) | 11 (30.6%) | |
| 4 | 13 (36.1%) | 12 (33.3%) | |
| 5 | 1 (2.8%) | 2 (5.6%) | |
| Duration of follow-up (years)a | 3.03 ± 0.75 | 2.99 ± 0.54 | 0.831 |
| Preoperative data | |||
| Side-bindinga | 17.11 ± 8.27 | 19.36 ± 7.91 | 0.242 |
| Cobb angle (°)a | 52.47 ± 10.83 | 52.97 ± 9.85 | 0.828 |
| Sagittal T5 T12 (°)a | 20.53 ± 4.83 | 21.42 ± 4.63 | 0.428 |
| T10 L2 Cobb (°)a | 9.25 ± 4.87 | 8.19 ± 5.41 | 0.387 |
| LIV tilt (cm)a | 20.69 ± 5.67 | 21.17 ± 5.75 | 0.718 |
| Plumb line deviation from the CSVL (cm)a | 1.40 ± 0.82 | 1.29 ± 0.70 | 0.529 |
P values are based on aindependent two-sample t test and bMann-Whitney U test
Data are displayed as mean ± standard deviation or number (percentage)
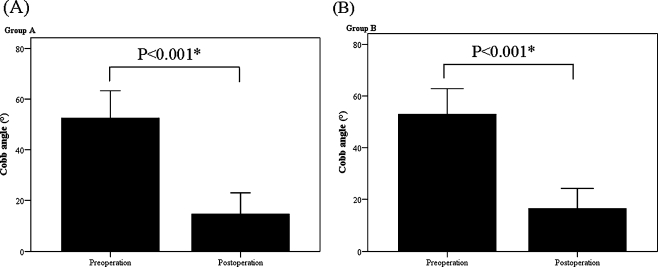
Outcome measurements of the two groups are shown in Table 2. The Cobb angle was significantly (P < 0.001) decreased after surgery in both group A (preoperative 52.47 ± 10.83°; postoperative 14.78 ± 8.19°; Fig. 1a) and group B (preoperative 52.97 ± 9.85°; postoperative 16.41 ± 7.78°; Fig. 1b). However, there was no significant difference between the two groups in the amount of decrease, nor was there a significant difference between the two groups in the related parameter, thoracic correction rate (group A 72.86 ± 10.51%; group B 70.09 ± 9.20%; P = 0.238).
Table 2.
Outcome measurement data
| Group A (n = 36) | Group B (n = 36) | P value | |
|---|---|---|---|
| Mean change between before and after operation | |||
| Cobb angle (°) | −37.69 ± 6.62 | −36.56 ± 4.87 | 0.408 |
| Sagittal T5–T12 (°) | 2.89 ± 5.44 | 1.19 ± 2.95 | 0.106 |
| T10–L2 Cobb (°) | −0.72 ± 4.20 | 0.14 ± 4.59 | 0.409 |
| LIV tilt (cm) | −15.72 ± 5.20 | −15.22 ± 5.36 | 0.689 |
| Plumb line deviation from the CSVL (cm) | −0.89 ± 0.97 | −0.57 ± 1.03 | 0.179 |
| Thoracic curve correction (%) | 72.86 ± 10.51 | 70.09 ± 9.20 | 0.238 |
| Thoracic curve flexibility (%) | 68.36 ± 10.02 | 64.38 ± 8.92 | 0.080 |
P values are based on independent two-sample t test
Fig. 1.
Comparison of Cobb angles before and after surgery. a Group A. b Group B
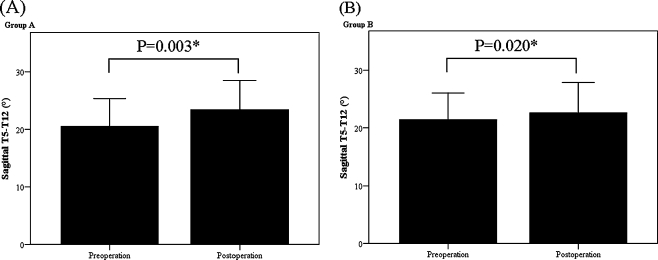
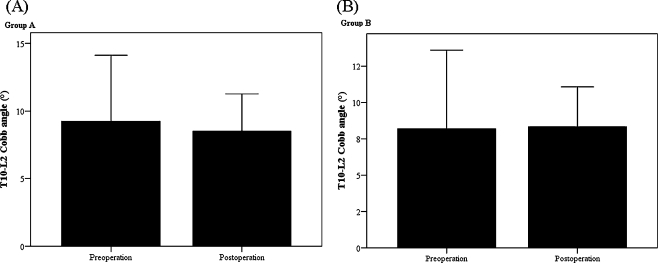
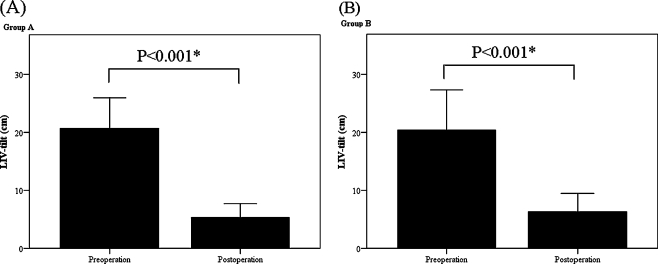
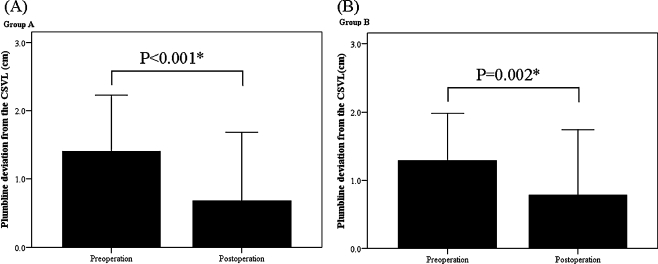
Sagittal T5–T12 increased significantly after surgery in both group A (preoperative 20.53 ± 4.83°; postoperative 23.42 ± 5.08°; P = 0.003; Fig. 2a) and group B (preoperative 21.42 ± 4.63°; postoperative 22.61 ± 5.27°; P = 0.020; Fig. 2b). However, there was no significant change in the T10–L2 Cobb angle between before and after surgery in either group A (P = 0.309; Fig. 3a) or group B (P = 0.857; Fig. 3b). LIV tilt decreased significantly after surgery in both group A (preoperative 20.69 ± 5.27 cm; postoperative 8.53 ± 2.74 cm; P < 0.001; Fig. 4a) and group B (preoperative 21.17 ± 5.75 cm; postoperative 5.94 ± 2.27 cm; P < 0.001; Fig. 4b). Plumb line deviation from the CSVL also decreased significantly after surgery in group A (preoperative 1.40 ± 0.82 cm; postoperative 0.51 ± 0.79 cm; P < 0.001; Fig. 5a) and group B (preoperative 1.29 ± 0.70 cm; postoperative 0.72 ± 0.89 cm; P = 0.002; Fig. 5b). No significant difference was seen between the two groups in the mean increase in sagittal T5–T11, the mean decrease in LIV tilt or the mean decrease in plumb line deviation. However, two patients (5.6%) in group A and five patients (13.9%) in group B had more than 2 cm of plumb line deviation from the CSVL.
Fig. 2.
Comparison of sagittal T5–T12 before and after surgery. a Group A. b Group B
Fig. 3.
Comparison of T10–L2 Cobb angle before and after surgery. a Group A. b Group B
Fig. 4.
Comparison of LIV tilt before and after surgery. a Group A. b Group B
Fig. 5.
Comparison of plumb line deviation from the CSVL before and after surgery. a Group A. b Group B
For the two cases in group A in which the apical vertebra was at T6–T6/7, T11 was selected as the LIV and the average correction rate was 62% and no imbalance was found. For the 15 cases in which the apical vertebra was at T7–T8, T12 was selected as the LIV and the average correction rate was 71%, but imbalance occurred in one case. For the 19 cases in which the apical vertebra was at T8/9–T10, L1 was selected as the LIV and the average correction rate was 75% and imbalance occurred in one case.
For the two cases in group B in which the apical vertebra was at T6–T6/7, T11 was selected as the LIV and the average correction rate was 70% and no imbalance was found. For 15 patients in group B in which the apical vertebra was at T7–T8, T11 was selected as the LIV for one patient, T12 for nine patients, L1 for two patients and L2 for three patients. The average correction rate for these 15 patients was 72% and imbalance occurred in two cases. For the 19 patients in which the apical vertebra was T8/9–T10, T12 was selected as the LIV for one patient, L1 for 16 patients and L2 for one patient. The average correction rate in these 19 patients was 73% and imbalance occurred in three cases (Table 3).
Table 3.
Comparisons of the vertebral fusion range
| LIV/AV | T6–T6/7 (n = 2) | T7–T8 (n = 15) | T8/9–T10 (n = 19) |
|---|---|---|---|
| Group A | |||
| T11 | 2 | - | - |
| T12 | - | 15 | - |
| L1 | - | - | 19 |
| Group B | |||
| T11 | 2 | 1 | - |
| T12 | - | 9 | 2 |
| L1 | - | 2 | 16 |
| L2 | - | 3 | 1 |
In the control group, there were two patients with shoulder height asymmetry. No pseudarthrosis was found in the two groups.
Discussion
The results of this study show that it is feasible to use the apical vertebra as the basis for LIV selection in Lenke type 1 AIS. T11 was selected as the LIV when the apical vertebra was T6–T6/7, T12 was selected as the LIV when the apical vertebra was T7–T8 and L1 was selected as the LIV when the apical vertebra was T8/9–T10. The patients were followed up for 2–4.6 years, and in group A (apical vertebra used to select LIV) imbalance occurred in two of the 36 patients. In group B, imbalance occurred in five of the 36 patients.
In group A, imbalance occurred in one patient in the T7–T8 group and one in the T8/9–T10 group. However, the imbalance seemed to have no relationship to the positions of the neutral vertebra and the end vertebra in that both cases were Lenke type 1C, that is, the apex of the lumbar curve was completely off the midline. In group B (neutral vertebra used), imbalance occurred in two patients in the group whose apical vertebra was T7–T8; both of the patients were also Lenke type 1C. In patients in group B whose apical vertebra was T8/9–T10, imbalance occurred in three patients, one that was Lenke type 1A, one that was Lenke type 1B and one that was Lenke type 1C. There were no differences in the scoliosis correction rate between the two groups, but the retention of motion segments in group A was greater than that in group B. In addition, the postoperative correction rate did not depend on the instrumentation chosen as different instrumentations achieved similar correction rates.
These results suggest that when the Cobb angle does not exceed 90°, as in the two patient groups studied, the LIV can be selected quantitatively based on the apical vertebra. That is, the same apical vertebrae will result in the same LIV. Moreover, the lowest LIV selected in group A was L1, but L2 was selected for four cases in group B, which suggests that the retention of motion segments in group A was superior to that in group B. As more motion segments in the lumbar spine are preserved, more self-correction of scoliosis occurs, and there is less likelihood of imbalance and possible pain and back problems in later life.
Suk et al. [11] analysed 42 cases of King type III patients using the neutral vertebra as the criteria for assessment of the thoracic fusion range. They reported that when the neutral vertebra and end vertebra were the same vertebra or differed by one vertebral level, and the neutral vertebra was selected as the LIV, good results were achieved in all 14 patients who met these criteria. When the neutral vertebra was two or more levels below the end vertebra, and the spine was fused to the vertebra one level above the neutral vertebra, good results were achieved in all of the nine patients thus treated. However, when the spine was fused to two or more levels above the neutral vertebra, imbalance occurred in 14 of 19 patients. In comparing our results with those of Suk et al. [11], we found that 80% of the LIV selection results were identical. At the same time, our results are similar to those of Lenke et al. [6] that imbalance is more likely to occur in type C scoliosis. In the two groups, most of the cases with imbalance were type C scoliosis. This warrants further study, even if the compensatory flexibility of the lumbar scoliosis is good.
Compared to posterior spinal fusion, anterior spinal fusion (ASF) for the treatment of AIS is associated with shorter fusion segments and thus less loss of mobility of the lumbar spine. In a study of ASF for the treatment of AIS, Liu et al. [7] showed that preservation of mobile segments and selection of the LIV was associated with trunk balance. The authors concluded that fusion that was too short can lead to disc wedging distal to the LIV and result in trunk imbalance.
In this study, we choose to use side-bending radiographs instead of fulcrum bending. Because the average age of our patients was approximately 13 years, flexibility was good. In assessment of spinal flexibility, the error of side-bending radiographs is less than that of fulcrum bending radiographs; possibly because patients may feel discomfort during fulcrum bending radiographs, which results in muscle tension and a complete evaluation of the spinal flexibility becomes impossible. In addition, differences in the location of the fulcrum placed at the apex of the scoliosis may induce error. These errors are avoided with side-bending radiographs; hence we used side-bending radiographs for evaluating spinal flexibility.
In summary, the apical vertebra can be used for LIV selection in patients with Lenke type 1 AIS. Compared to LIV selection using the neutral vertebra, results using the apical vertebra offer higher reliability and repeatability and more motion segments are retained. T11 is selected as the LIV when the apical vertebra is T6–6/7, T12 when the apical vertebra is T7–T8 and L1 when the apical vertebra is located at T8/9–T10. The scoliosis curvature of the patients included in this study was <90°; thus, further observational studies including more patients with greater scoliosis and low spinal flexibility are warranted.
Acknowledgments
Conflicts of interest None.
Footnotes
Fenghua Tao and Zhicai Shi contributed equally to this work.
Contributor Information
Fenghua Tao, Phone: +86-015-921455843, FAX: +86-021-81873398, Email: fenghuatao@yahoo.cn.
Ming Li, Email: limingch@21cn.com.
References
- 1.Behensky H, Giesinger K, Ogon M, et al. Multisurgeon assessment of coronal pattern classification systems for adolescent idiopathic scoliosis: reliability and error analysis. Spine. 2002;27:762–767. doi: 10.1097/00007632-200204010-00015. [DOI] [PubMed] [Google Scholar]
- 2.Bridwell KH, McAllister JW, Betz RR, et al. Coronal decompensation produced by Cotrel-Dubousset “derotation” maneuver for idiopathic right thoracic scoliosis. Spine. 1991;16:769–777. doi: 10.1097/00007632-199107000-00015. [DOI] [PubMed] [Google Scholar]
- 3.King HA, Moe JH, Bradford DS, et al. The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg Am. 1983;65:1302–1313. [PubMed] [Google Scholar]
- 4.Knapp DR, Jr, Price CT, Jones ET, et al. Choosing fusion levels in progressive thoracic idiopathic scoliosis. Spine. 1992;17:1159–1165. doi: 10.1097/00007632-199210000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Lenke LG, Betz RR, Haher T, et al. Multisurgeon assessment of surgical decision-making in adolescent idiopathic scoliosis: curve classification, operative approach, and fusion levels. Spine. 2001;26:2347–2353. doi: 10.1097/00007632-200111010-00011. [DOI] [PubMed] [Google Scholar]
- 6.Lenke LG, Betz RR, Harms J, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am. 2001;83-A:1169–1181. [PubMed] [Google Scholar]
- 7.Liu Y, Li M, Zhu XD, et al. Retrospective analysis of anterior correction and fusion for adolescent idiopathic thoracolumbar/lumbar scoliosis: the relationship between preserving mobile segments and trunk balance. Int Orthop. 2009;33:191–196. doi: 10.1007/s00264-007-0489-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Potter BK, Rosner MK, Lehman RA, Jr, et al. Reliability of end, neutral, and stable vertebrae identification in adolescent idiopathic scoliosis. Spine. 2005;30:1658–1663. doi: 10.1097/01.brs.0000170290.05381.9a. [DOI] [PubMed] [Google Scholar]
- 9.Puno RM, An KC, Puno RL, Jacob A, Chung SS. Treatment recommendations for idiopathic scoliosis: an assessment of the Lenke classification. Spine. 2003;28(18):2102. doi: 10.1097/01.BRS.0000088480.08179.35. [DOI] [PubMed] [Google Scholar]
- 10.Richards BS, Birch JG, Herring JA, et al. Frontal plane and sagittal plane balance following Cotrel-Dubousset instrumentation for idiopathic scoliosis. Spine. 1989;14:733–737. doi: 10.1097/00007632-198907000-00015. [DOI] [PubMed] [Google Scholar]
- 11.Suk SI, Lee SM, Chung ER, et al. Determination of distal fusion level with segmental pedicle screw fixation in single thoracic idiopathic scoliosis. Spine. 2003;28:484–491. doi: 10.1097/00007632-200303010-00014. [DOI] [PubMed] [Google Scholar]
- 12.Thompson JP, Transfeldt EE, Bradford DS, et al. Decompensation after Cotrel-Dubousset instrumentation of idiopathic scoliosis. Spine. 1990;15:927–931. doi: 10.1097/00007632-199009000-00017. [DOI] [PubMed] [Google Scholar]