Abstract
The purpose of this study was to evaluate the effect of eccentric humeral components with different degrees of posterior offset on range of glenohumeral motion in reverse shoulder arthroplasty. Uncemented PROMOS® reverse shoulder prostheses were implanted in eight human cadaveric shoulder specimens. Passive range of motion was evaluated with a robot-assisted shoulder simulator. Three movements were tested: abduction, anterior elevation and external rotation. Each specimen was tested with a customary reverse humeral component and two eccentric components with 3 and 6 mm of posterior offset respectively. Mean abduction was 81° (standard deviation [SD] 12) for the customary reverse components, 81° (SD 13) for the 3 mm eccentric and 82° (SD 15) for 6-mm eccentric implants. Mean anterior elevation was 68° (SD 13) in the regular group and 66° (SD 14) and 63° (SD 14) for 3- and 6-mm eccentric groups. With all configurations, 90° of external rotation were achieved without requiring more than 2 N·m of applied rotational moment. Although there was no statistically significant difference between the conventional and the eccentric implants, anterior elevation was decreased by almost 20° in three of eight shoulders with the posterior offset configurations. This was due to a conflict between the proximal humerus and the anterior aspect of the acromion or the coracoid. Although eccentric humeral components can be useful in reverse shoulder arthroplasty to avoid anterior cortical defects in individuals with pronounced humeral head posterior offset, a potential conflict between proximal humerus and scapula may have an unfavourable effect on range of anterior elevation. However, this observation is only true for the uncemented PROMOS® reverse prosthesis. Other reverse shoulder designs with posterior offset components are yet to be tested.
Introduction
Reverse shoulder arthroplasty is an established procedure in patients with shoulder pathologies that cannot be managed with standard arthroplasty, such as rotator cuff tear arthropathy with pseudoparalysis, certain revision arthroplasties or even cases of musculoskeletal tumours around the shoulder joint [9]. Since the original design of a reverse shoulder arthroplasty was presented by Prof. Paul Grammont in 1985, several modifications have led to the current designs. Surgical technique has also evolved; problems such as scapular notching have been identified and addressed by modifications of the technique [11]. With modern modular reverse shoulder systems, the prostheses can be adjusted to accommodate individual glenohumeral anatomy for parameters such as medial offset, inclination in the coronal plane, and retroversion in the axial plane. Posterior offset in the axial plane is addressed by only very few current reverse shoulder systems, although several cadaveric studies have demonstrated a great interindividual variability of humeral head posterior offset relative to the humeral shaft axis, ranging between −0.8° and 10° [2, 4, 12]. While the importance of posterior offset in reverse shoulder arthroplasty is largely unclear, it is known that in humeral heads with pronounced posterior offset, implantation of a reverse humeral component can result in osseous defects of the humeral head anterior cortex. This is due to the position of the prosthetic stem which is predetermined by the humeral medullary canal. This is particularly true for uncemented designs such as the uncemented PROMOS® reverse shoulder. To a certain degree, posterior offset can be managed by increasing retroversion of the reverse humeral component to avoid cortical defects [2]. Anterior cortical defects can compromise the subscapularis repair at the end of the procedure. Insufficiency of the subscapularis has been shown to result in a weakness with internal rotation on the one hand, while on the other hand there is evidence that an irreparable subscapularis tendon in reverse shoulder arthroplasty is associated with an increased risk of postoperative dislocation [3, 10]. Eccentric humeral components with different degrees of posterior offset relative to the prosthetic stem allow for individual adjustment of posterior offset in order to avoid damage to the anterior cortex. The effect of posterior offset components on range of motion is unclear. The aim of this experimental cadaver study was to evaluate the effects of eccentric humeral components on glenohumeral range of motion in reverse shoulder arthroplasty. The hypothesis to be tested was that eccentric humeral components do not have adverse effects on passive range of motion of the arthroplasty.
Methods
Robot-assisted shoulder simulator
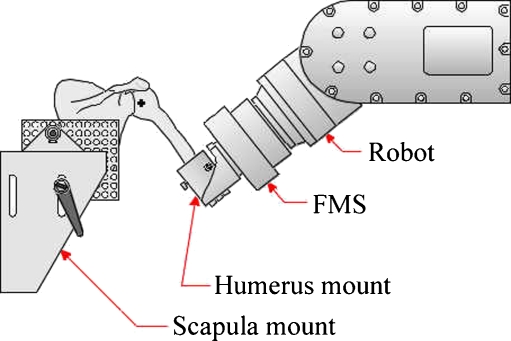
The tests were performed using a robot-assisted shoulder simulator that consisted of an industrial robot (KUKA GmbH, Augsburg, Germany) with a six-component force moment sensor (IpeA GmbH, Berlin, Germany) and a scapula mount. In this setup, the scapula was fixed to the scapula mounting tower and the humerus was attached to the force moment sensor (FMS) of the robot with a humerus mount so the humerus could be moved by the robot in order to simulate glenohumeral motion, and joint loading could be monitored (Fig. 1). The sensor-guided robot allowed for repeatable movements with a precision of 0.1 mm, measurement of joint loading with a resolution of 3.0 N of force and 0.15 N·m of torque. The motion and loading applied to the joint could be programmed in one of two coordinate systems: a global coordinate system fixed in space, or a humeral coordinate system moving with the specimen.
Fig. 1.
Robot-assisted shoulder simulator setup. FMS force moment sensor
Specimen preparation and mounting
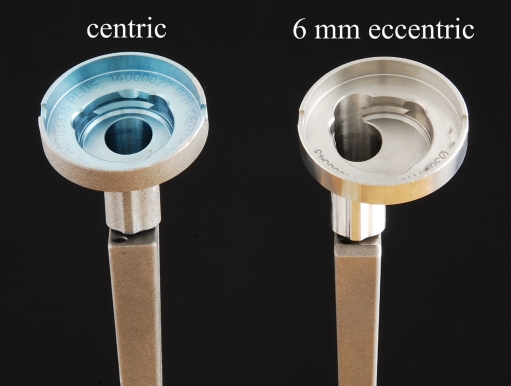
Eight macroscopically and radiologically normal, embalmed cadaveric human shoulder specimens were obtained from this University's Institute of Anatomy. The shoulders were embalmed in Thiel's solution [13]. Each humerus was transected approximately 20 cm distal to the tip of the greater tuberosity and all soft tissue attachments were removed from the distal 10 cm of the bone. The humeri were potted in brass cylinders (diameter 38 mm, height 50 mm) with a cold curing resin (Ureol FC 53, Vantico GmbH, Wehr, Germany) while the humeral shaft axis was aligned with the cylinder using an intramedullary alignment jig. Then, modular reverse shoulder prostheses (Promos®, Smith & Nephew Orthopaedics AG, Switzerland) were implanted through a standard deltopectoral approach according to the surgical procedure recommended by the manufacturer. In shoulders with an intact rotator cuff, the tendon of supraspinatus was resected in order to better reflect the clinical situation of reverse shoulder arthroplasty and to prevent soft tissues from blocking abduction. An uncemented prosthetic stem was implanted first, the size of which was determined by the size of the last reamer used. After adjusting retroversion with an alignment jig, a reamer guide was placed over the stem and the humeral metaphysis was prepared to accommodate the reverse humeral component. The reverse component was then coupled with the stem using a coupling device and finally secured with a screw. On the side of the glenoid, uncemented glenoid baseplates with a central peg and locking screws were implanted. A standard size glenoid baseplate and a 36-mm glenosphere were used in all shoulders. There was a choice of 3-, 6- and 9-mm articular inlays, the size of which was chosen depending on soft tissue tension as estimated by the surgeon. Each shoulder was tested with a customary centric humeral component and two eccentric humeral components with 3 mm and 6 mm of posterior offset, respectively (Fig. 2).
Fig. 2.
Reverse humeral components coupled with uncemented stems. The centric component is a customary reverse humeral component (PROMOS, Smith & Nephew Orthopaedics AG, Switzerland). The 6-mm eccentric is an eccentric reverse humeral component with 6-mm posterior offset
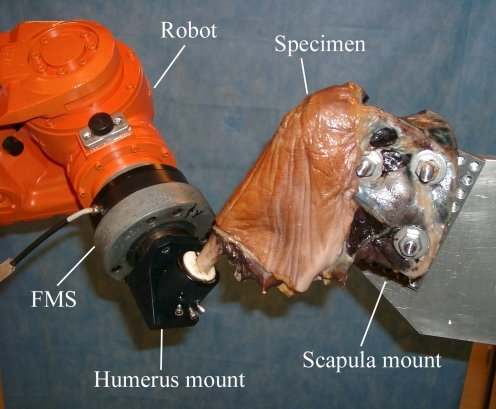
All humeral components were positioned in 10° of retroversion regardless of the individual humeral head retroversion. This was done to eliminate possible effects of retroversion, in order to exclusively observe the effects of posterior offset on passive ROM. The initial arthroplasty was always performed using the conventional centric reverse component. For the subsequent implantations of the experimental eccentric components, the reverse component was uncoupled with an uncoupling device. Then, an eccentric reamer guide was attached to the stem with 3-mm or 6-mm posterior offset, respectively. After alignment of the reamer guide in 10° of retroversion, the humeral metaphysis was reamed again to accommodate the eccentric component which was then implanted. During all manipulations, the humeral stem was left in situ. The subscapularis tendon was not repaired at the end of the procedures, because leaving the joint open during the experiments allowed continuous observation of the articulation of the reverse arthroplasty in order to exclude subluxation. Correct articulation was defined as full contact of the humeral metaphyseal component with the glenosphere. The shoulder specimens were mounted on steel plates with three threaded steel rods passing through the scapula according to a standardised protocol [8, 14]. The scapulae were orientated on the plates with a 10° forward tilt to approximate to the physiological orientation on the chest wall [5]. Then the specimens were mounted on the testing tower with the vertical axis of the scapula parallel to the testing tower. The exact position of the scapulae on the mounting tower was marked for each specimen allowing the different tests to be reproducible [6, 8, 14]. The plane of the scapula was defined visually as the vertical plane passing through both the superior and inferior angles of the scapula and the middle of the glenoid surface. The humerus was attached to the robot by fitting the brass cylinder into a mount on the force moment sensor (FMS) (Fig. 3). Neutral rotation of the arm was determined by palpating the intertubercular groove and aligning it midway between the coracoid process and the lateral margin of the acromion. The neutral rotation for each individual specimen was then marked on the humeral shaft and the brass cylinder, so the starting position was reproducible for subsequent simulations. For each specimen, an individual coordinate system was generated by determining the geometric centre (GC) of the reverse arthroplasty, which was defined as the point that moved the least during passive motions. To determine the GC, the humerus was moved by the robot from 20° to 60° of abduction in the scapular plane and from 20° of flexion to 20° of extension. During these movements, a 20-N medially-directed force was applied by the robot in order to ensure articulation of the reverse arthroplasty during the movement. The force of 20 N was chosen because it provided sufficient stability of the articulation and did not damage tissues of the specimen, as shown in a previous study [8]. The GC was then computed from the resulting motion data using a non-linear least squares minimisation algorithm [6, 14]. The global coordinate system, which is fixed in space, was defined so that the anterior direction was normal to the previously described plane of the scapula, the superior direction was the vertical direction in the plane of the scapula, and the lateral direction was the direction orthogonal to the anterior and superior directions. Finally, the humeral coordinate system, located at the GC of the reverse arthroplasty, was defined such that it was co-directional with the global coordinate system with the specimen hanging under its own weight in the previously defined position of neutral rotation. This defined the reference position relative to which all movements were simulated.
Fig. 3.
Robot-assisted shoulder simulator performing abduction with left shoulder specimen. FMS force moment sensor
Measurement of glenohumeral range of motion
Three movements were tested: abduction in the plane of the scapula, anterior elevation with 30° of internal rotation of the humerus and external rotation starting from 60° of abduction in the scapular plane. Elevation was performed in 30° of internal rotation in order to reproduce a physiological movement such as drinking or combing hair. The starting point of the abduction and elevation motions was the position of the arm hanging under its own weight. The end point of each motion was detection of a resistive moment of 2 N·m by the FMS, at which the robot was programmed to abort any motion. This was done to obtain objective measurements of the motions. The 2-N·m moment had been applied in previous studies as this has been shown to be safe and not cause ligamentous or osseous damage [6]. External rotation was started with the arm in a position of 60° of abduction in the scapular plane and was performed up to a maximum of 90° in all specimens, although a much greater range of passive external rotation would have been possible for most but not all shoulders. The reason for this was the fact that external rotation greater than 90° is not likely to be achieved by a patient with a reverse shoulder replacement and therefore was considered clinically irrelevant. During all movements, the articulation of the reverse arthroplasty was visualised to exclude subluxation. Each specimen was first tested with the conventional centric humeral component in all three directions. Subsequently, the 3- and 6-mm eccentric components were implanted and tested using the same procedure.
Computing the motion data
The data obtained from the FMS during each movement was computed using the Mathematica®5.1 Software (Wolfram Research Inc., Champaign, IL) which allows visualisation of the motion data in a 2D diagram as well as a 3D graphic. Start and end points of each movement could be read from the 2D diagrams.
Statistical methods
Statistical analysis was performed with SPSS version 13.0 (SPSS Inc., Chicago, IL, USA). Normal distribution was confirmed using the one-sample Kolmogorov-Smirnov test. Mean values as well as standard deviations were computed for each movement. The paired samples t-test was used to compare the results of the centric with the 3-mm eccentric, the 3- with the 6-mm eccentric and the centric with 6-mm eccentric configurations of the specimens. Significance was defined as P < 0.05.
Results
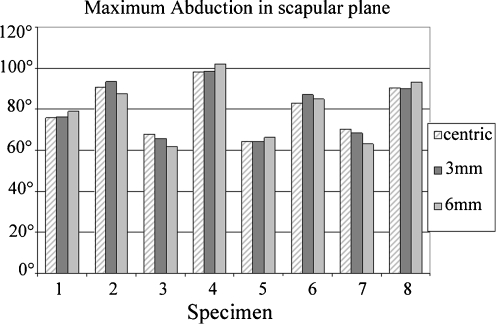
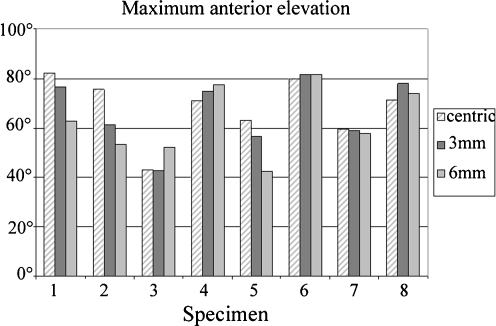
Shoulder specimens with centric humeral components were found to achieve a mean abduction of 81° (range 68–91°, standard deviation [SD] 12). With the 3-mm eccentric humeral components, mean abduction was also 81° (range 65–99°, SD 13), and it was 82° (range 62°-102°, SD 15) with 6-mm eccentric components (Fig. 4). Comparison between the groups did not reveal statistically significant differences with P = 0.93 for centric versus 3-mm eccentric, P = 0.33 for 3-mm versus 6-mm eccentric, and P = 0.45 for centric versus 6-mm eccentric. Mean anterior elevation was 68° (range 43–82°, SD 13) in the centric group, 66° (range 43–82°, SD 14) in the 3-mm eccentric and 63° (range 43–82°, SD 14) in the 6-mm eccentric group. Again, the data were compared using the paired samples t-test and no statistically significant differences were observed with P = 0.46 for centric versus 3-mm eccentric, P = 0.25 for 3-mm versus 6-mm eccentric, and P = 0.27 for centric versus 6-mm eccentric. In three individual shoulders, anterior elevation was decreased with the 3- and 6-mm posterior offset configurations (Fig. 5). In specimen 1, anterior elevation was decreased by 19° with 6-mm posterior offset; in specimen 2, the decrease was 22° and in specimen 5 it was 21°. All tested specimens achieved 90° of passive external rotation.
Fig. 4.
Maximum abduction in the scapular plane with centric, 3- and 6-mm eccentric humeral components (abduction in scapular plane, in angular degrees)
Fig. 5.
Maximum anterior elevation with centric, 3- and 6-mm eccentric humeral components (anterior elevation in angular degrees)
Discussion
In this study, we evaluated the effect of eccentric humeral components with different degrees of posterior offset on glenohumeral motion in uncemented PROMOS® reverse shoulder arthroplasties. We were unable to show a statistically significant effect of humeral component posterior offset on range of motion. This may be due to the relatively high standard deviations in range of motion of the individual shoulders, as well as the relatively limited number of specimens tested. From our results, eccentric implants with 3- and 6-mm of posterior offset did not show a significant effect on abduction and external rotation. However, anterior elevation was decreased by almost 20 degrees in three of eight shoulders with increasing posterior offset (Fig. 5). Although not statistically significant, we postulate a clinical relevance to these findings. At what degree a decrease in range of anterior elevation would clinically affect a patient can only be estimated. Anterior elevation, or flexion, is necessary for a multitude of daily activities, such as drinking and combing or washing hair. Kasten et al. tested active-angle-reproduction (AAR) in patients before and after shoulder arthroplasty and found a mean AAR of 5.5° preoperatively and 7.6° postoperatively for 60° of flexion [7]. Based on the findings of the study by Kasten et al. we assumed the observed decrease in flexion in our study to be clinically significant. To further investigate the observed decrease in anterior elevation, we looked at the mechanism that limited passive ROM in these specimens and found that in all cases abutment of the humerus on the anterior aspect of the acromion or the coracoid occurred at the end point of anterior elevation. The decrease in anterior elevation in three shoulders may be due to a ventral shift of humeral structures caused by the posterior offset reverse components. Since the reverse shoulder prosthesis is a semi-constrained design, modifications to the humeral component leave the centre of rotation unchanged, but alter the position of humeral head structures relative to it and lead to conflicts with scapular structures that limit anterior motion. But this is only one possible explanation for the observed effects. Due to the multitude of interindividual differences in humeral and scapular anatomy it is very difficult to predict the effect of a single prosthetic component on function and outcome of the arthroplasty. The overall poor results for passive ROM in the specimens tested can be explained by the setup of the shoulder simulator. Since the scapulae were fixed on steel plates and mounted on the testing tower, scapulothoracic motion was eliminated. Clinical studies have shown that glenohumeral motion contributes on average two thirds to the entire thoracohumeral ROM in reverse shoulder arthroplasty [1]. Since scapulothoracic motion was eliminated, the measured movements represent the passive ROM of the prosthetic articulation, not physiological ROM of a patient.
From our results, posterior offset humeral components for the uncemented PROMOS® reverse shoulder arthroplasty do not appear to affect range of motion with regard to abduction and external rotation. Anterior elevation was decreased in three of eight specimens with posterior offset configurations. Although this decrease did not reach statistical significance, we observed a potential conflict between proximal humeral and scapular structures with the use of posterior offset components that may have clinical implications. However, since only one prosthetic design was tested in our study, we cannot generalise our observations. Other reverse shoulder designs with posterior offset humeral components are yet to be tested.
Acknowledgements
This study was funded by Smith & Nephew Orthopaedics AG, Switzerland. The authors thank Evgenij Bobrowitsch for his contribution regarding the robot-assisted shoulder simulator.
Conflict of interest This group has received funding and support for this work from Smith & Nephew Orthopaedics AG, Switzerland of less than $10,000. Furthermore, the senior author (Joern Steinbeck), has received royalties from Smith & Nephew Orthopaedics AG, Switzerland in excess of $10,000.
References
- 1.Bergmann JHM, Leeuw M, Janssen TWJ, Veeger DHEJ, Willems WJ. Contribution of the reverse endoprosthesis to glenohumeral kinematics. Clin Orthop Rel Res. 2008;466:594–598. doi: 10.1007/s11999-007-0091-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boileau P, Walch G. The three dimensional geometry of the proximal humerus. J Bone Joint Surg Br. 1997;79-B:857–865. doi: 10.1302/0301-620X.79B5.7579. [DOI] [PubMed] [Google Scholar]
- 3.Edwards TB, Williams MD, Labriola JE, Elkousy HA, Gartsman GM, O’Connor DP. Subscapularis insufficiency and the risk of shoulder dislocation after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2009 doi: 10.1016/j.jse.2008.12.013. [DOI] [PubMed] [Google Scholar]
- 4.Hertel R, Knothe U, Ballmer FT. Geometry of the proximal humerus and implications for prosthetic design. J Shoulder Elbow Surg. 2002;11(4):331–338. doi: 10.1067/mse.2002.124429. [DOI] [PubMed] [Google Scholar]
- 5.Hurschler C, Wulker N, Mendila M. The effect of negative intraarticular pressure and rotator cuff force on glenohumeral translation during simulated active elevation. Clin Biomech. 2000;15:306–314. doi: 10.1016/S0268-0033(99)00088-1. [DOI] [PubMed] [Google Scholar]
- 6.Hurschler C, Wulker N, Windhagen H, Plumhoff P, Hellmers N. Medially based anterior capsular shift of the glenohumeral joint. Passive range of motion and posterior capsular strain. Am J Sports Med. 2001;29(3):346–353. doi: 10.1177/03635465010290031601. [DOI] [PubMed] [Google Scholar]
- 7.Kasten P, Maier M, Rettig O, Raiss P, Wolf S, Loew M. Proprioception in total, heim- and reverse shoulder arthroplasty in 3D motion analyses: a prospective study. Int Orthop (SICOT) 2009;33:1641–1647. doi: 10.1007/s00264-008-0666-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marquardt B, Hurschler C, Schneppendahl J, Witt K, Potzl W, Steinbeck J. Quantitative assessment of glenohumeral translation after anterior shoulder dislocation and subsequent arthroscopic Bankart repair. Am J Sports Med. 2006;34(11):1756–1762. doi: 10.1177/0363546506289702. [DOI] [PubMed] [Google Scholar]
- 9.Matsen FA, Boileau P, Walch G, Gerber C, Bicknell RT. The reverse total shoulder arthroplasty. J Bone Joint Surg Am. 2007;89:660–667. doi: 10.2106/00004623-200703000-00027. [DOI] [PubMed] [Google Scholar]
- 10.Miller BS, Joseph TA, Noonan TJ, Horan MP, Hawkins RJ. Rupture of the subscapularis tendon after shoulder arthroplasty: diagnosis, treatment and outcome. J Shoulder Elbow Surg. 2005;14(5):492–496. doi: 10.1016/j.jse.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 11.Nyffeler RW, Werner CM, Gerber C. Biomechanical relevance of glenoid component positioning in the reverse Delta III total shoulder prosthesis. J Shoulder Elbow Surg. 2005;14(5):524–528. doi: 10.1016/j.jse.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 12.Roberts SN, Foley APJ, Swallow HM, Wallace WA, Coughlan DP. The geometry of the humeral head and the design of prostheses. J Bone Joint Surg Br. 1991;73-B:647–650. doi: 10.1302/0301-620X.73B4.2071652. [DOI] [PubMed] [Google Scholar]
- 13.Thiel W. The preservation of the whole corpse with natural color. Ann Anat. 1992;174(3):185–195. [PubMed] [Google Scholar]
- 14.Wulker N, Schmotzer H, Thren K, Korell M. Translation of the glenohumeral joint with simulated active elevation. Clin Orthop Rel Res. 1994;309:193–200. [PubMed] [Google Scholar]