Abstract
There has been renewed interest for metal-on-metal hip resurfacing due to improved design and manufacturing of implants, better materials, and enhanced implant fixation. In contrast to conventional total hip replacements, only a few clinical hip resurfacing trials using radiostereometry (RSA) have been reported, and solely for the Birmingham hip resurfacing arthroplasty. The purpose of this RSA trial was to describe the migration pattern of a new hip resurfacing system (ReCap) within the first two years after primary surgery. Twenty-six patients underwent total hip replacement. The patients were followed-up for up to 24 months and were evaluated with the use of radiostereometric measurements. The prosthesis showed mean translations and rotation close to zero. Maximum translation was seen along the transverse axis in the medial direction (0.13 mm). No statistically significant translation or rotation was seen at two-years follow-up, (t-test, p <0.05, translation or rotation).
Introduction
Total hip replacement (THR) has proven to be one of the most successful operations in terms of pain relief, patient mobility, and improvement in quality of life, and more than 7,000 hip prostheses are implanted every year in Denmark [1]. However, because of high activity level and life expatiation in younger patients, a conventional THR does not offer an optimal solution due to the risk of premature aseptic loosening leading to multiple revisions.
There has been renewed interest for metal-on-metal hip resurfacing following improved design and manufacturing of implants, better materials, and enhanced implant fixation [2]. It has been proposed that the resurfacing hip prostheses have a lower dislocation rate due to oversized femoral heads [3], better reproduction of anatomical hip biomemechanics, and easier revision surgery on the femoral side due to preservation of the femoral canal [4]. Clinical studies have demonstrated good short- and long-term results [5–7], although femoral neck fracture has been recognised to cause early failures [8, 9]. Despite a documented low wear rate, longevity and long-term effects of metal wear debris are currently unknown [10].
Until now, only very limited clinical results of the ReCap prosthesis have been reported. Gagala et al. [11] described good short-term results with no significant complications in a group of 25 patients. In contrast to conventional THRs, only few clinical hip resurfacing trials using radiostereometry (RSA) have been reported, and these solely for the Birmingham hip resurfacing arthroplasty [12–14].
The purpose of this RSA trial was to describe the migration pattern of a new hip resurfacing system called ReCap (Biomet, Warsaw, Indiana, USA) within the first two years following primary surgery. Since the acetabular component is much like the conventional hip prosthesis, the focus in this paper is on the femoral component, which may show different migration patterns from the conventional THRs in view of its different design. Karrholm et al. [15] have shown that the extent of early implant migration may predict implant loosening; therefore, the endpoint in our study was implant migration two years after hip surgery.
Materials and methods
The design and conduct of the clinical trial were approved by the local ethics committee before patients were included and it was performed in accordance with the Helsinki Declaration II. Informed patient consent in writing was required. Additional permission was granted by the local ethics committee to perform ten double RSA examinations.
The trial was registered before September 13, 2005 in an openly available database in accordance with the directions of the Committee of Medical Journal Editors (ICMJE).
Twenty-six patients (15 men, 11 women; median age 58 years, range 51–63) underwent total hip replacement.
Patients were included if they (1) had primary osteoarthritis, (2) had sufficient bone density to allow implantation of a ReCap prosthesis, (3) had no regular intake of non-steroid anti-inflammatory drugs (NSAID), and (4) were under 65 years old.
The prosthesis evaluated in this study was the ReCap hip resurfacing system (Biomet, Warsaw, Indiana, USA), which consists of a cobalt chrome cemented femoral resurfacing head and an uncemented titanium non-hydroxyapatite-coated closed-pore porous-coated acetabular component with a cobalt chrome core (Fig. 1). The Birmingham hip resurfacing arthroplasty and the ReCap prosthesis have many similarities; however, in two aspects they differ significantly. The ReCap prosthesis has an entirely spherical geometry at the non-articulation femoral side, in contrast to the Birmingham hip resurfacing arthroplasty which has a chamfer design. Beaule et al. [16] have shown, that geometry of the femoral component affects the cement mantle thickness influencing the seating of the implant. Furthermore, the recap prosthesis is made of “as cast” cobalt chrome. As-cast materials were determined to have greater abrasive wear resistance when compared to single or multiple heat treated materials [17].
Fig. 1.
ReCap hip resurfacing system. Note the tantalum markers attached to the femoral stem
Two senior surgeons (FMM) at Silkeborg Regions Hospital, Denmark and (TP) at Aarhus University Hospital, Denmark, undertook all operations during a period of two years. An extended posterolateral approach with the patient in a lateral decubitus was used in all cases. Stable fixation of the acetabular component was achieved with a line-to-line reaming, whereas low viscosity cement (implex P bone cement with Tobramycin; Stryker, Hopkinton, USA) was applied to the femoral component to obtain fixation to the femoral host bone.
Radiostereometric analysis
Intraoperatively, four 1.0-mm tantalum markers were inserted in the greater trochanter and four tantalum markers were inserted in the lesser trochanter forming a reference rigid body (Fig. 2). The femoral components had 1.0-mm tantalum markers at the distal tips, and an additional two placed on pegs at the distal half of the rod provided by the manufacturer. To facilitate optimal visualisation of all three prosthesis markers on both stereoradiographs a slot was made in the femoral neck along the canal made for the rod.
Fig. 2.

Implant positioning
Two stationary radiographic tubes were positioned so the X-ray beams crossed at an angle of approximately 40 degrees. The exposure was set to 150 kV and 3mAs.
Model-based RSA (MbRSA) version 3.2, marker mode (Medis Specials®, Leiden, The Netherlands) was used to calculate the implant migration [18–20].
Radiostereometric examinations were done within the first week after surgery and at three months, 12 months, and 24 months after surgery.
Ten patients underwent double examinations to assess the precision of the RSA system. Between the two investigations, the equipment was removed from the location and repositioned before the second session.
Statistics
We performed probability plots to test for normality. A paired t test was used for the statistical analysis, where p < 0.05 (two tailed) was considered statistically significant. The coefficient of repeatability (CR) was calculated as 1.96 times the standard deviation of the difference (d) between the two measurements as a precision measure of the system as described by Valstar et al. [21].
Based on an estimated clinically significant difference of 0.6 mm and a standard deviation of 0.7 mm between groups [22], a pre study sample size calculation required 22 patients in each group to achieve 80% power at a 0.05 significance level. Due to the risk of patient drop-out, 26 patients were included.
Statistical analysis was performed with STATA 8 (Stata Corporation, Texas, USA) software package.
Results
One patient was excluded from the RSA because of too few visual tantalum markers on the femoral implant. One patient was revised after ten months following a fracture of the femoral neck. This patient had a lateral translation of more than 0.7 mm (the highest value in the whole dataset) after three months. One patient did not attend radiographic follow-up.
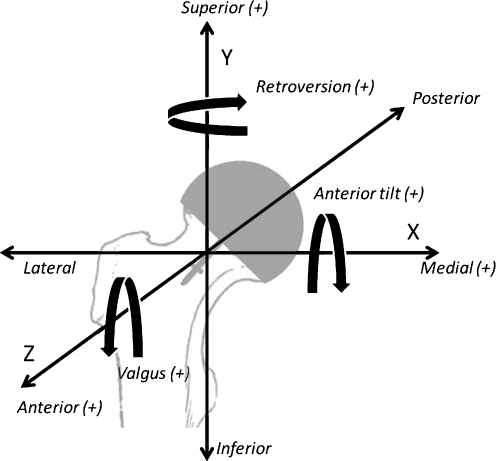
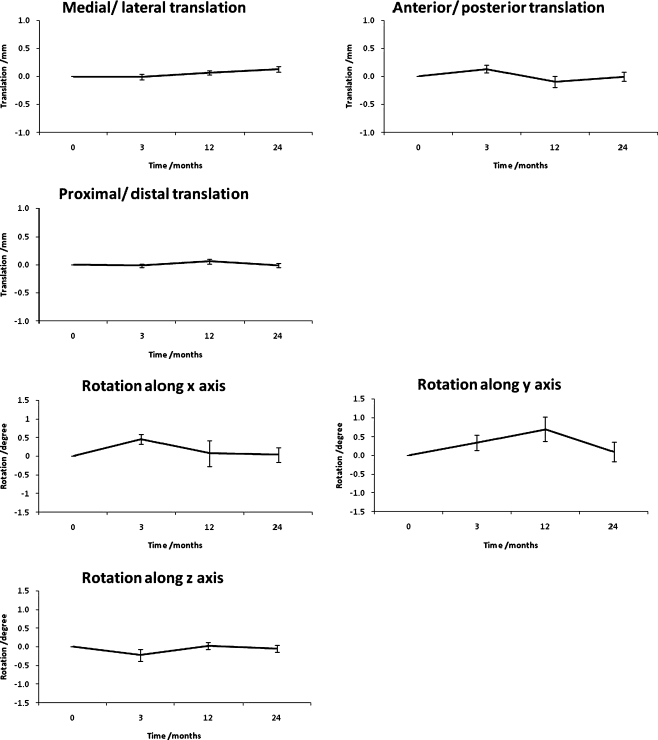
Double examinations of ten patients revealed a precision of 0.09-mm translation and rotation of 0.23° along the transverse axis, 0.15 mm and 0.59° along the longitudinal axis, and 0.13 mm and 0.38° along the sagittal axis. Average condition number for the inserted markers was calculated as 70. The calculated migrations in terms of mean translation and rotation were small. Maximum translation was seen along the transverse axis in the medial direction (0.13 mm); see Fig. 3 for explanation of the directions of translation and rotation. No statistically significant translation or rotation was seen between three months and two years (for translation between 0.07 and 0.79, p > 0.07; with regard to rotation between 0.08 and 0.46, p > 0.08; see Table 1). The migration pattern over time for the ReCap hip prosthesis is displayed in Fig. 4.
Fig. 3.
Directions of translation & rotation
Table 1.
Translation and rotation at three, 12 and 24 months. Values presented as mean and standard deviation (SD)
| Measured parameter | Three months | 12 months | 24 months |
|---|---|---|---|
| Translation, mm | |||
| Media–lateral (X) | -0.006 (0.243) | 0.076 (0.175) | 0.131 (0.243) |
| Proximal–distal (Y) | -0.014 (0.16) | 0.065 (0.196) | -0.009 (0.175) |
| Anterior–posterior (Z) | 0.133 (0.32) | -0.121 (0.524) | -0.028 (0.402) |
| Rotation, degrees | |||
| Transverse axis (X) | 0.449 (0.674) | -0.093 (1.692) | -0.089 (0.965) |
| Longitudinal axis (Y) | 0.345 (1.049) | 0.497 (1.599) | -0.077 (1.314) |
| Sagittal axis (Z) | -0.225 (0.791) | 0.008 (0.442) | -0.077 (0.456) |
Fig. 4.
Migration pattern for the ReCap hip prosthesis
Discussion
The results of this study demonstrate an excellent fixation of the ReCap hip resurfacing system at two-years follow-up. We detected no significant translation or rotation of the femoral component. However, it is important to note that the reported results of the implant migration may be underestimated, since the threshold values of the measuring system are tested to be higher. No specific translation pattern was observed during the observation and no signs of prosthesis migration to 'level off' could be seen at any given time. Furthermore, it is important to remember that even with promising short-term migration results of the ReCap prosthesis, the results of radiostereometric analysis are implant specific and it is not possible to predict whether early results will last another 10–15 years. However, the migration analysis in our study is based on markers attached to the tip of the distal part of the prosthesis. Therefore an indirect measurement of the migration of the centre of the resurfacing prosthesis is given and this may lead to a biased result. Nevertheless, in comparison, our migration results are similar to the RSA studies of the Birmingham hip resurfacing arthroplasty showing an implant translation of 20 and 22 implants respectively at two-years follow-up with values between −0.02 and 0.15 mm in the anterior–posterior direction, 0.04 and 0.05 mm in the distal direction, and −0.008 and −0.04 mm in the medial–lateral direction [12–14].
No consensus has been achieved on how to report or display the migration results. Recent publications advocate expressing the translation as the mean scalar product of the vector since the mean translation is less informative [23]. RSA guidelines by Valstar et al. [21] advise avoidance of absolute migration values since they are not always normally distributed. However, all RSA studies evaluating hip resurfacing prostheses report absolute values. The study by Glyn-Jones et al. [14] depicts the translation over time with absolute values and SEMs, whereas Itayem et al. [13] shows individual graphs for each implant. Furthermore, an alternative migration axis has been introduced to elucidate specific translation issues with regard to hip resurfacing prostheses [13]. Taking the above-mentioned into account, we decided to report our results in the same manner as the previously published RSA studies relating to resurfacing prostheses to facilitate a direct comparison.
It has been stated that proper preparation of the femoral head and cautious implantation of the resurfacing prosthesis is crucial to minimise the risk of femoral neck fractures [24]. As previously stated, a single implant showed a lateral translation of more than 0.7 mm and distal translation of 0.45 mm within the first three months after surgery, eventually leading to a fracture of the femoral neck at ten months postoperatively. The femoral stem-shaft angle (SSA) of this patient was measured as 128 degrees on the postoperative radiographs. A relationship between SSA and stress forces within the femoral bone during walking has indicated that SSA <130 degrees gives an increased risk of adverse outcome [25]. Whether the fracture was caused by a reduced SSA or was due to an excessive migration leading to a mal-orientated femoral component giving rise to a femoral neck fracture remains unclear. However, a study using the Ein Bild Roentgen Analyse on the Birmingham hip resurfacing arthroplasty demonstrated that prosthesis migration is a good predictor of implant failure even before onset of clinical symptoms or radiological evidence of failure [26].
In conclusion, the ReCap hip prosthesis shows encouraging results comparable to other resurfacing prostheses with low migration and rotation values; however, the insertion of all resurfacing prostheses requires meticulous surgical technique and specialised instrumentation and even small deviations from the optimal position may lead to short-term failures of the prosthesis.
Acknowledgments
We would like to thank Flemming Møller Larsen, MD, and Thomas Prynø, MD for performing the hip surgery.
References
- 1.Lucht U, Johnsen Paaske S (2004) Danish Hip Arthroplasty Registry. Annual report 2004. http://www.dhr.dk/Ny%20mappe/Dhr-rapport2004%20engelsk.pdf. Accessed 09 February 2010
- 2.Grigoris P, Roberts P, Panousis K, Jin Z. Hip resurfacing arthroplasty: the evolution of contemporary designs. Proc Inst Mech Eng [H] 2006;220:95–105. doi: 10.1243/095441105X69042. [DOI] [PubMed] [Google Scholar]
- 3.Scifert CF, Brown TD, Pedersen DR, Callaghan JJ. A finite element analysis of factors influencing total hip dislocation. Clin Orthop Relat Res. 1998;355:152–162. doi: 10.1097/00003086-199810000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Shimmin A, Beaule PE, Campbell P. Metal-on-metal hip resurfacing arthroplasty. J Bone Joint Surg Am. 2008;90:637–654. doi: 10.2106/JBJS.G.01012. [DOI] [PubMed] [Google Scholar]
- 5.Amstutz HC, Duff MJ. Eleven years of experience with metal-on-metal hybrid hip resurfacing: a review of 1000 conserve plus. J Arthroplasty. 2008;23:36–43. doi: 10.1016/j.arth.2008.04.017. [DOI] [PubMed] [Google Scholar]
- 6.Amstutz HC, Beaule PE, Dorey FJ, Duff MJ, Campbell PA, Gruen TA. Metal-on-metal hybrid surface arthroplasty: two to six-year follow-up study. J Bone Jt Surg Am. 2004;86-A:28–39. [PubMed] [Google Scholar]
- 7.Heilpern GN, Shah NN, Fordyce MJ. Birmingham hip resurfacing arthroplasty: a series of 110 consecutive hips with a minimum five-year clinical and radiological follow-up. J Bone Joint Surg Br. 2008;90:1137–1142. doi: 10.1302/0301-620X.90B9.20524. [DOI] [PubMed] [Google Scholar]
- 8.Davis ET, Olsen M, Zdero R, Waddell JP, Schemitsch EH. Femoral neck fracture following hip resurfacing: the effect of alignment of the femoral component. J Bone Joint Surg Br. 2008;90:1522–1527. doi: 10.1302/0301-620X.90B11.20068. [DOI] [PubMed] [Google Scholar]
- 9.Whittingham-Jones P, Charnley G, Francis J, Annapureddy S. Internal fixation after subtrochanteric femoral fracture after hip resurfacing arthroplasty. J Arthroplasty. 2008 doi: 10.1016/j.arth.2008.10.015. [DOI] [PubMed] [Google Scholar]
- 10.Mabilleau G, Kwon YM, Pandit H, Murray DW, Sabokbar A. Metal-on-metal hip resurfacing arthroplasty: a review of periprosthetic biological reactions. Acta Orthop. 2008;79:734–747. doi: 10.1080/17453670810016795. [DOI] [PubMed] [Google Scholar]
- 11.Gagala J, Mazurkiewicz T. First experiences with total hip resurfacing arthroplasty. Chir Narzadow Ruchu Ortop Pol. 2007;72:311–317. [PubMed] [Google Scholar]
- 12.Itayem R, Arndt A, McMinn DJ, Daniel J, Lundberg A. A five-year radiostereometric follow-up of the Birmingham hip resurfacing arthroplasty. J Bone Joint Surg Br. 2007;89:1140–1143. doi: 10.1302/0301-620X.89B9.18367. [DOI] [PubMed] [Google Scholar]
- 13.Itayem R, Arndt A, Nistor L, McMinn D, Lundberg A. Stability of the Birmingham hip resurfacing arthroplasty at two years. A radiostereophotogrammetric analysis study. J Bone Joint Surg Br. 2005;87:158–162. doi: 10.1302/0301-620X.87B2.15394. [DOI] [PubMed] [Google Scholar]
- 14.Glyn-Jones S, Gill HS, McLardy-Smith P, Murray DW. Roentgen stereophotogrammetric analysis of the Birmingham hip resurfacing arthroplasty. A two-year study. J Bone Joint Surg Br. 2004;86:172–176. doi: 10.1302/0301-620X.86B2.14371. [DOI] [PubMed] [Google Scholar]
- 15.Karrholm J. Roentgen stereophotogrammetry. Review of orthopedic applications. Acta Orthop Scand. 1989;60:491–503. doi: 10.3109/17453678909149328. [DOI] [PubMed] [Google Scholar]
- 16.Beaule PE, Matar WY, Poitras P, Smit K, May O (2009) 2008 otto aufranc award: Component design and technique affect cement penetration in hip resurfacing. Clin Orthop Relat Res 467:84–93. doi:10.1007/s11999-008-0541-8 [DOI] [PMC free article] [PubMed]
- 17.Cawley J, Metcalf JEP, Jonesa AH, Band TJ, Skupien DS. A tribological study of cobalt chromium molybdenum alloys used in metal-on-metal resurfacing hip arthroplasty. Wear. 2003;255:999–1006. doi: 10.1016/S0043-1648(03)00046-2. [DOI] [Google Scholar]
- 18.Beumer A, Valstar ER, Garling EH, Niesing R, Ginai AZ, Ranstam J, Swierstra BA. Effects of ligament sectioning on the kinematics of the distal tibiofibular syndesmosis: a radiostereometric study of 10 cadaveric specimens based on presumed trauma mechanisms with suggestions for treatment. Acta Orthop. 2006;77:531–540. doi: 10.1080/17453670610012557. [DOI] [PubMed] [Google Scholar]
- 19.Krijnen MR, Valstar ER, Smit TH, Wuisman PI. Does bioresorbable cage material influence segment stability in spinal interbody fusion? Clin Orthop Relat Res. 2006;448:33–38. doi: 10.1097/01.blo.0000224015.42669.cc. [DOI] [PubMed] [Google Scholar]
- 20.Nelissen RG, Doets HC, Valstar ER. Early migration of the tibial component of the Buechel–Pappas total ankle prosthesis. Clin Orthop Relat Res. 2006;448:146–151. doi: 10.1097/01.blo.0000224013.57916.24. [DOI] [PubMed] [Google Scholar]
- 21.Valstar ER, Gill R, Ryd L, Flivik G, Borlin N, Karrholm J. Guidelines for standardization of radiostereometry (RSA) of implants 1. Acta Orthop. 2005;76:563–572. doi: 10.1080/17453670510041574. [DOI] [PubMed] [Google Scholar]
- 22.Ryd L (1992) Roentgen stereophotogrammetric analysis of prosthetic fixation in the hip and knee joint. Clin Orthop 276:56–65 [PubMed]
- 23.Derbyshire B, Prescott RJ, Porter ML. Notes on the use and interpretation of radiostereometric analysis. Acta Orthop. 2009;80:124–130. doi: 10.1080/17453670902807474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Amstutz HC, Campbell PA, Duff MJ. Fracture of the neck of the femur after surface arthroplasty of the hip 7. J Bone Joint Surg Am. 2004;86-A:1874–1877. doi: 10.2106/00004623-200409000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Beaule PE, Lee JL, Duff MJ, Amstutz HC, Ebramzadeh E. Orientation of the femoral component in surface arthroplasty of the hip. A biomechanical and clinical analysis 1. J Bone Joint Surg Am. 2004;86-A:2015–2021. doi: 10.2106/00004623-200409000-00021. [DOI] [PubMed] [Google Scholar]
- 26.Beaule PE, Krismer M, Mayrhofer P, Wanner S, Duff M, Mattesich M, Stoeckl B, Amstutz HC, Biedermann R. EBRA-FCA for measurement of migration of the femoral component in surface arthroplasty of the hip 1. J Bone Joint Surg Br. 2005;87:741–744. doi: 10.1302/0301-620X.87B5.15377. [DOI] [PubMed] [Google Scholar]