Abstract
The aim of this study was to evaluate the clinical and radiological outcome of the treatment of osteonecrosis of the femoral head by implantation of an osteonecrosis intervention rod. In this retrospective study the follow-up of 19 patients with 23 osteonecrotic femoral heads treated with implantation of an osteonecrosis intervention implant was assessed. From 19 patients with 23 necrotic femoral heads, there were 13 cases in which a total hip replacement was necessary. This implies a survival rate of 44% after implantation of an osteonecrosis intervention rod after a mean follow-up of 1.45 years. The outcome after core decompression combined with the insertion of a tantalum osteonecrosis intervention implant did not show superior results compared to core decompression alone. This is in contrast to existing studies. In addition, this study showed that in cases of total hip replacement, no problems appeared during explantation of the tantalum rod.
Introduction
Osteonecrosis of the femoral head (ONFH) is a locally destructive and complex disorder. If left untreated it usually leads to a destruction of the hip joint. The typical age of appearance is between the third and fifth decade. Thus, ONFH has high socioeconomic relevance. About 10% of all total hip replacements (THR) are implanted due to advanced ONFH.
The effectiveness of conservative treatment of ONFH is poor; although, Zhao et al. showed that the lesion size in ONFH often decreases slightly over time [18]. Thus, in most cases an operative approach is necessary. However, no uniform recommendation for treatment exists. The primary goal is to preserve the femoral head. This is only possible for the early stages of ONFH, i.e. ARCO I and II (association research circulation osseous). For ARCO I and II neither collapse of the femoral head nor any crescent line is visible.
For ONFH within the reversible stage, core decompression (CD) of the necrotic area represents an established and commonly used technique. This therapeutical principle was developed by Ficat and Arlet in 1962 during diagnostic “functional exploration of bone” [4]. In the reversible stages CD is supposed to reduce the intraosseous pressure and bring about reperfusion. CD can be modified by additional interventions such as implantation of bone-marrow cells, growth factors or fibular grafting [6, 8, 9]. Recently, the treatment of ONFH using bone impaction grafting through a femoral neck window showed encouraging results [17], while cement injection is not recommended for the treatment of ONFH [5]. These additional approaches are believed to be associated with an increased donor-site morbidity [16]. Furthermore, the transtrochanteric rotational osteotomy, which is often used in Asian patients with good long-term results, is not recommended for young Caucasians [11].
However, isolated CD is results in a lack of structural support and has varying outcomes. CD combined with the insertion of an osteonecrosis intervention implant is supposed to be an alternative. This implant consists of a porous and cellular structure and a stiffness similar to bone [1, 13]. By giving structural support, it is supposed to offer an alternative to bone grafts. Thus, on the one hand this combined technique provides the effects of CD with reduction of the increased intraosseous pressure and on the other hand gives structural support. This technique is minimally invasive and has no donor-site morbidity [16].
Therefore, this study evaluated the clinical and radiological outcome by MRI of the insertion of the osteonecrosis intervention implant. The survival rate of ONFH treated by CD combined with the implantation of osteonecrosis intervention rods should be determined. This is the first study assessing the radiological follow-up by MRI after the treatment of CD and simultaneous implantation of the osteonecrosis intervention implant.
Patients and methods
Inclusion criteria
This study assessed the follow-up of 19 patients with 23 ONFH treated by implantation of an osteonecrosis intervention implant (Trabecular Metal, Zimmer, Allendale, New Jersey, USA). The study was approved by the local ethics committee. Detailed biomechanical characteristics of this implant have been described previously [1, 2, 15]. The operations were performed between December 2003 and March 2007. All surgical procedures were conducted according to the operating instructions. The diagnosis “ONFH” was set by radiological and clinical evidence. Exclusion criteria were the complete destruction of the hip joint (ARCO III and IV) and an age above 65 years.
Surgical technique
The operation was conducted in supine position with the affected hip prepared and draped freely. Fluoroscopy was used to detect the centre of the necrotic lesion and the point immediately superior to the lesser trochanter. After skin incision the subcutaneous soft tissue, the fascia lata and the vastus lateralis muscle were split in the direction of the fibres. A guide pin was inserted so that the tip was positioned about 5 mm from the endosteal surface of the femoral head. With the guide pin in correct position cannulated reamers were used to progressively ream the core to 10 mm under fluoroscopy. After measuring and tapping, the implant was threaded into the final position. Finally, the incision was closed in layers. Patients remained in hospital for at least three days for care of the wound and initial physiotherapy. Patients were allowed to increase weight-bearing gradually as tolerated.
Clinical follow-up
For the review, the following parameters were documented: age at surgery, date of surgery, gender, side of affected hip, preoperative Harris hip score (HHS), postoperative HHS, length of the implant, subsequent THR including date of replacement and kind of arthroplasty, time to THR and associated risk factors.
Radiological assessment
The radiological assessment included the preoperative and follow-up MRIs. The MRIs were compared in order to analyse the outcome of this treatment. The stage of the osteonecrosis was classified according to ARCO. Although it is reported that in the presence of a metal implant MRIs tend to loose accuracy and precision, the MRIs in this study provided good images and information.
Statistical analysis
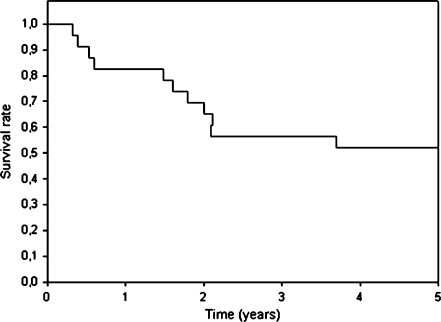
In order to illustrate the failure of this treatment, the Kaplan-Meier survival curve was used. Furthermore, the survival rate after this treatment was determined. In addition, the time until hip arthroplasty after implantation of the implant was evaluated.
Results
No patient was lost to follow-up. Evaluations of 19 patients (14 men and five women) with 23 ONFH were completed with regard to clinical and radiological outcome after CD combined with implantation of an osteonecrosis intervention rod. In four patients bilateral treatment was necessary.
Survival rate
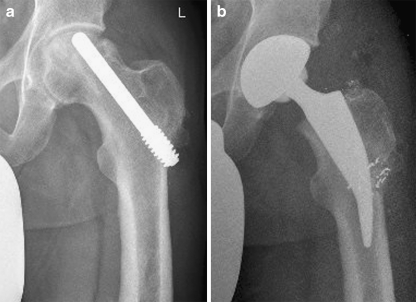
From 19 patients with 23 ONFH, THR was necessary in 13 cases (eleven patients; Fig. 1a, b). This implies a survival rate of 44% after implantation of an osteonecrosis intervention rod. The indication for arthroplasty was persistence of pain or destruction of the joint (two hips in two women, eleven hips in nine men). The time until conversion to THR averaged 529 days (1.45 years) (range 120–1,348 days) (Table 1; Figs. 1a, b and 2). From the 11 patients who required a THR, four patients had a previous femoral neck fracture and three patients (four hips) had chronic disease. Two patients (three hips) had an acute myeloid leukaemia with bone marrow transplantation and prolonged cortisone medication before surgery, while another patient had a Hodgkin's lymphoma treated by chemotherapy.
Fig. 1.
a, b Follow-up of a patient with osteonecrosis of the femoral head (ONFH) after insertion of the tantalum implant with later conversion to total hip replacement
Table 1.
Conversion to total hip replacement (THR) after treatment of osteonecrosis of the femoral head (ONFH) by insertion of a tantalum osteonecrosis intervention implant
| Initials | Gender | Age at surgery (years) | Hip side | Length of osteonecrosis intervention rod (mm) | Preoperative ARCO stage | Postoperative ARCO stage | Kind of arthroplasty | Time to arthroplasty (days) | Comorbidity | Complication / particularities |
|---|---|---|---|---|---|---|---|---|---|---|
| B.B. | Female | 41 | Right | 85 | II | III | Long stem hip arthroplasty | 655 | Traumatic fracture of the femoral neck treated with osteosynthesis 18 months before | |
| R.B. | Male | 51 | Right | 95 | II | III | Long stem hip arthroplasty | 773 | ||
| U.G. | Male | 48 | Left | 100 | II | III | Long stem hip arthroplasty | 120 | Acute myeloid leukaemia with bone marrow transplantation and long term cortisone medication | |
| U.G. | Male | 48 | Right | 115 | II | III | Long stem hip arthroplasty | 1348 | Acute myeloid leukaemia with bone marrow transplantation and long term cortisone medication | |
| M.G. | Male | 19 | Left | 95 | II | III | Short stem hip arthroplasty | 542 | Acute myeloid leukaemia with bone marrow transplantation and long term cortisone medication | |
| W.K. | Male | 45 | Right | 95 | II | III | Short stem hip arthroplasty | 142 | ||
| A.K. | Male | 22 | Right | 100 | II | III | Short stem hip arthroplasty | 731 | ||
| J.K. | Male | 47 | Left | 90 | II | II | Hip resurfacing | 197 | Traumatic fracture of the femoral neck | |
| V.P. | Male | 42 | Left | 105 | II | III | Short stem hip arthroplasty | 646 | Additional implantation of spongious bone and augmentation of BMP 7 | |
| D.S. | Male | 40 | Right | 105 | I | III | Short stem hip arthroplasty | 157 | ||
| D.S. | Male | 40 | Left | 105 | II | III | Short stem hip arthroplasty | 220 | M. Hodgkin treated with chemotherapy | |
| F.S. | Male | 16 | Left | 85 | II | III | Short stem hip arthroplasty | 764 | Traumatic fracture of the femoral neck treated with osteosynthesis | Postoperative weakness of dorsiflexion of the feet (external hospital) |
| A.W. | Female | 63 | Left | 100 | II | III | Long stem hip arthroplasty | 587 | Traumatic acetabular fracture | |
| Mean value | 40 | 529 | ||||||||
Fig. 2.
Kaplan-Meier survivorship curve with conversion to total hip replacement
Radiographic assessment
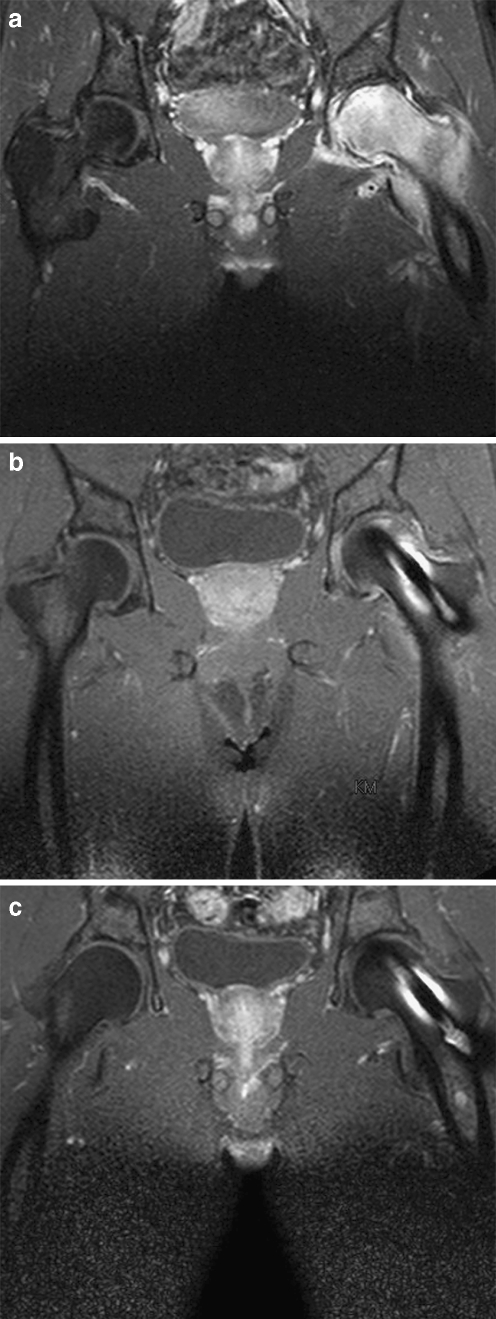
Within the survivor group radiographic progression occurred in one patient (10%) after implantation of an osteonecrosis intervention rod. A regression occurred in one patient (10%). In case of a complete regression from ARCO II with tendency to ARCO III was visible (Fig. 3a–c). The majority of osteonecrosis in the patients who did not need a THR remained almost unchanged (80%). The mean time between surgery and the last MRI evaluation for the survivor group was 618 days (Table 2).
Fig. 3.
Follow-up of a patient with osteonecrosis of the femoral head (ONFH) and an additional bone marrow oedema and complete regression after insertion of a tantalum implant. a Preoperative (stage ARCO II with tendency to ARCO III). b Four months postoperative. c 18 months postoperative
Table 2.
Survivor group after treatment of the femoral head necrosis using a tantalum osteonecrosis intervention rod
| Initials | Gender | Age at surgery (years) | Hip side | Preoperative HHS | Postoperative HHS | Time to HHS (days) | Length of osteonecrosis intervention rod (mm) | Preoperative ARCO stage | Postoperative ARCO stage | Time to MRI (days) | Comorbidity | Complication / particularities |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| H.A. | Male | 35 | Left | 56 | 74 | 185 | 90 | II | III | 257 | ||
| J.B. | Male | 50 | Right | 41 | 91 | 759 | 95 | II | II | 746 | Postoperative subtrochanteric femoral fracture treated with a plate | |
| J.B. | Male | 50 | Left | 41 | 95 | 759 | 100 | II | II | 746 | ||
| W. E. | Male | 49 | Left | 18 | 95 | 511 | 95 | II | 0 | 547 | Osteogenesis imperfecta | |
| D.G. | Male | 42 | Left | 32 | 49 | 519 | 105 | II | II | 1099 | ||
| M.J. | Female | 61 | Left | 41 | 71 | 200 | 85 | II | II | 121 | Patient with persistence of pain; in case of further persistence indication for arthroplasty | |
| C.K. | Female | 50 | Right | 34 | 76 | 196 | 85 | II | II | 921 | ||
| H.L. | Male | 63 | Left | 33 | 59 | 947 | 95 | II | II | 1380 | ||
| M.S. | Female | 41 | Right | 46 | 46 | 345 | 90 | II | II | 181 | ||
| M.S. | Female | 41 | Left | 46 | 46 | 345 | 85 | II | II | 181 | ||
| Mean value | 48 | 39 | 70 | 477 | 618 | |||||||
Harris hip score
The mean HHS within the survivor group after insertion of an osteonecrosis intervention rod increased postoperatively during follow-up from 39 (range 18–56) to 70 (range 46–95). The mean time of assessment of the postoperative HHS was 477 days (1.31 years) (Table 2).
Complications
One postoperative subtrochanteric fracture due to a trauma occurred, and was stabilised with an osteosynthesis plate. Another patient developed a postoperative weakness of dorsiflexion of the foot after THR in another hospital. Apart from these, no infection, thrombosis, embolism or fracture occurred.
Surgical procedure for THR
The THR after implantation of an osteonecrosis intervention rod resulted in no complications. For the THR the femoral head was removed with an oscillating saw which was able to cut through the implant. The remaining part of the implant could be removed without major bone loss. Thus, conversion of the osteonecrosis intervention rod to a THR was easy to perform. In five cases a long stem hip arthroplasty, in seven cases a short stem arthroplasty and in one case in another hospital a hip resurfacing was carried out (Table 1). Eight of these conversions to THR were performed in our department (four long stem and four short stem hip arthroplasties).
Discussion
This study evaluated the clinical and radiological outcome of the implantation of an osteonecrosis intervention implant in 19 patients with 23 ONFH. For radiological assessment MRI was conducted during follow-up. This treatment has a survival rate of 44%. Conversion to THR occurred after a mean time of 529 days (1.45 years). The majority of the survivors revealed an almost unchanged radiological appearance (80%). In the patients not requiring THR the clinical symptoms improved according to the HHS by this treatment.
Left untreated the ONFH usually progresses within a few years and in a high percentage of cases leads to destruction of the hip joint, so that a THR becomes necessary. The variation of treatment is wide and no definite algorithm exists. In early stages several conservative treatments have been described: non-weight bearing, magnetic field therapy, shock wave therapy, hyperbaric oxygenation and pharmacotherapeutical treatments. However, by now none of these conservative approaches showed encouraging long-term results.
CD has been proven to be appropriate for small to medium-sized, centrally located defects before collapse of the head. It is supposed to reduce the oedema-related intraosseous pressure in order to relieve pain. Furthermore, it is suggested that CD induces reperfusion, possibly associated with revascularisation and bone regeneration of the necrotic area. In 1985, Ficat et al. published good long-term results after core depression [4]. They evaluated 133 patients with ONFH without destruction of the femoral head 9.5 years after core depression. Radiological failure occurred in Ficat stage I in 13.4% and in stage II in 33.3%. Further studies indicated varying results. In 1986, Camp et al. described a clinical and radiological failure in 60% of cases 18 months after core depression. Unfortunately, they did not differentiate between preoperative stages of osteonecrosis [3]. Another large study confirmed that the outcome depends on the stage of ONFH. While patients of Ficat stage I showed no radiological failure three years after CD, in 42% and 56% of patients of Ficat II and Ficat III, respectively, a radiological failure occurred [14]. A meta-analysis of 24 studies conducted by Mont et al. [7] included 1,206 hip joints treated with CD. In 84% of the patients of Ficat stage I and 65% of Ficat stage II good results were revealed after this treatment.
In order to improve the treatment of ONFH, alternative techniques have been described. The development of an osteonecrosis intervention implant was supposed to improve the treatment of precollapse ONFH. Possible benefits were thought to include the advantages of the CD: reduction of the intraosseous pressure and reperfusion with the possibility of regeneration. Additional advantages were supposed to be the structural support, the low donor-site morbidity and the minimally invasive procedure [16]. Due to the additional structural support, early postoperative load-bearing would be possible. Our study revealed no fracture after implantation of the tantalum implant except for one subtrochanteric fracture after significant trauma. However, this study did not confirm the mainly encouraging results presented previously. Veilette et al. reported the outcome of treatment of ONFH with the tantalum implant and postoperative non-weight bearing for six weeks [16]. The survival rates of 60 hips with ONFH were 92% after 12 months, 82% after 24 months and 68% after 48 months. The majority of patients had osteonecrosis of stage II according to Steinberg, meaning that there was no destruction of the femoral head. In the absence of chronic systemic disease the survival rate at 48 months was 92%. They concluded that implantation of this tantalum rod represents an encouraging treatment, especially in patients without chronic systemic disease. Shuler et al. presented a survival rate of 86% after 39 months after insertion of the tantalum implant and six weeks protected weight bearing [12], while Tsao et al. described a survival rate of 85% at 12 months, 79% at 24 months and 73% at 48 months [15]. In the multicentre study of Tsao et al., information about the postoperative procedure is not included. Nadeau et al. reported a survival rate of 78% after 12 months and an overall success rate of 45% [10]. The patients were instructed to be non-weight bearing for three weeks, to partial weight bear for an additional three weeks and then to bear weight as tolerated. A possible reason for the worse results reported by Nadeau et al. is the inclusion of patients with subchondral collapse with and without flattening.
The results of our study differ from the mainly encouraging outcome described by Veillette et al., Tsao et al. and Shuler et al. [12, 15, 16]. A possible reason may be the variation of postoperative load bearing. The suggested advantage of this treatment of an earlier load bearing may have a negative influence on the outcome of the treatment. Further studies analysing the outcome of implanted osteonecrosis intervention rod would be helpful.
In contrast to previous studies, in our study an additional radiological follow-up by MRI was conducted. In a few cases a liquid layer surrounded the tantalum implant. This raises the question of the extent of the supposed osteointegration.
In summary, the results of our study revealed an outcome that was worse than that described previously in the literature. Furthermore, this surgical procedure is associated with a longer operation time compared to simple CD. In addition, the cost for the tantalum implant is relatively high, which has to be considered when choosing the surgical procedure. Another disadvantage of the tantalum rod is that it is a foreign body that, in case of a deep infection, may have to be removed. This would be associated with a high risk of fracture. A possible advantage of the treatment is the earlier postoperative load-bearing without increased risk of femoral neck fracture, allowing the patients to resume their daily routine sooner. However, CD via multiple small drill holes would also allow similar postoperative load-bearing and seems to result in similar or even better clinical outcome without the prolonged implantation of an expensive tantalum implant. Nevertheless, in this study it was found that in cases of joint destruction, removal of the tantalum rod and the simultaneous THR presents no particular surgical problems. It was possible to implant either a cementless short stem or a cementless distal interlocking femoral stem hip arthroplasty.
A disadvantage of this study is the relatively small number of patients, including different aetiologies of the ONFH. However, in view of the poor survival rate of the treatment detected in this study, contrary to the existing literature, CD using multiple small drill holes would seem preferable.
In conclusion, treatment of the early stage of ONFH with CD combined with the implantation of an osteonecrosis intervention rod seems to be no better and no worse than simple CD. Furthermore, the procedure is associated with increased costs and a prolonged operation time. Thus, this study does not recommend the insertion of the tantalum implant for the early stages of ONFH.
References
- 1.Bobyn JD, Poggie RA, Krygier JJ, Lewallen DG, Hanssen AD, Lewis RJ, Unger AS, O’Keefe TJ, Christie MJ, Nasser S, Wood JE, Stulberg SD, Tanzer M. Clinical validation of a structural porous tantalum biomaterial for adult reconstruction. J Bone Joint Surg Am. 2004;86-A(Suppl 2):123–129. doi: 10.2106/00004623-200412002-00017. [DOI] [PubMed] [Google Scholar]
- 2.Bobyn JD, Stackpool GJ, Hacking SA, Tanzer M, Krygier JJ. Characteristics of bone ingrowth and interface mechanics of a new porous tantalum biomaterial. J Bone Joint Surg Br. 1999;81:907–914. doi: 10.1302/0301-620X.81B5.9283. [DOI] [PubMed] [Google Scholar]
- 3.Camp JF, Colwell CW., Jr Core decompression of the femoral head for osteonecrosis. J Bone Joint Surg Am. 1986;68:1313–1319. [PubMed] [Google Scholar]
- 4.Ficat RP. Idiopathic bone necrosis of the femoral head. Early diagnosis and treatment. J Bone Joint Surg Br. 1985;67:3–9. doi: 10.1302/0301-620X.67B1.3155745. [DOI] [PubMed] [Google Scholar]
- 5.Gangji V, Rooze M, De MV, Hauzeur JP. Inefficacy of the cementation of femoral head collapse in glucocorticoid-induced osteonecrosis. Int Orthop. 2009;33:639–642. doi: 10.1007/s00264-008-0518-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hungerford MW, Mont MA. Potential uses of cytokines and growth factors in treatment of osteonecrosis. Orthopade. 2000;29:442–448. doi: 10.1007/s001320050465. [DOI] [PubMed] [Google Scholar]
- 7.Mont MA, Carbone JJ, Fairbank AC (1996) Core decompression versus nonoperative management for osteonecrosis of the hip. Clin Orthop Relat Res 169–178 [DOI] [PubMed]
- 8.Mont MA, Jones LC, Seyler TM, Marulanda GA, Saleh KJ, Delanois RE. New treatment approaches for osteonecrosis of the femoral head: an overview. Instr Course Lect. 2007;56:197–212. [PubMed] [Google Scholar]
- 9.Mont MA, Marulanda GA, Seyler TM, Plate JF, Delanois RE. Core decompression and nonvascularized bone grafting for the treatment of early stage osteonecrosis of the femoral head. Instr Course Lect. 2007;56:213–220. [PubMed] [Google Scholar]
- 10.Nadeau M, Seguin C, Theodoropoulos JS, Harvey EJ. Short term clinical outcome of a porous tantalum implant for the treatment of advanced osteonecrosis of the femoral head. Mcgill J Med. 2007;10:4–10. [PMC free article] [PubMed] [Google Scholar]
- 11.Rijnen WH, Gardeniers JW, Westrek BL, Buma P, Schreurs BW. Sugioka’s osteotomy for femoral-head necrosis in young Caucasians. Int Orthop. 2005;29:140–144. doi: 10.1007/s00264-005-0639-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shuler MS, Rooks MD, Roberson JR. Porous tantalum implant in early osteonecrosis of the hip: preliminary report on operative, survival, and outcomes results. J Arthroplasty. 2007;22:26–31. doi: 10.1016/j.arth.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 13.Tanzer M, Karabasz D, Krygier JJ, Cohen R, Bobyn JD. The Otto Aufranc Award: bone augmentation around and within porous implants by local bisphosphonate elution. Clin Orthop Relat Res. 2005;441:30–39. doi: 10.1097/01.blo.0000194728.62996.2d. [DOI] [PubMed] [Google Scholar]
- 14.Tooke SM, Nugent PJ, Bassett LW, Nottingham P, Mirra J, Jinnah R (1988) Results of core decompression for femoral head osteonecrosis. Clin Orthop Relat Res 99–104 [PubMed]
- 15.Tsao AK, Roberson JR, Christie MJ, Dore DD, Heck DA, Robertson DD, Poggie RA. Biomechanical and clinical evaluations of a porous tantalum implant for the treatment of early-stage osteonecrosis. J Bone Joint Surg Am. 2005;87(Suppl 2):22–27. doi: 10.2106/JBJS.E.00490. [DOI] [PubMed] [Google Scholar]
- 16.Veillette CJ, Mehdian H, Schemitsch EH, McKee MD. Survivorship analysis and radiographic outcome following tantalum rod insertion for osteonecrosis of the femoral head. J Bone Joint Surg Am. 2006;88(Suppl 3):48–55. doi: 10.2106/JBJS.F.00538. [DOI] [PubMed] [Google Scholar]
- 17.Wang BL, Sun W, Shi ZC, Zhang NF, Yue DB, Guo WS, Shi SH, Li ZR. Treatment of nontraumatic osteonecrosis of the femoral head using bone impaction grafting through a femoral neck window. Int Orthop. 2009 doi: 10.1007/s00264-009-0822-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhao FC, Li ZR, Zhang NF, Wang BL, Sun W, Cheng LM, Liu ZH. Lesion size changes in osteonecrosis of the femoral head: a long-term prospective study using MRI. Int Orthop. 2009 doi: 10.1007/s00264-009-0829-7. [DOI] [PMC free article] [PubMed] [Google Scholar]