Abstract
Background/objective
To describe the nature and distribution of activities during physical therapy (PT) delivered in inpatient spinal cord injury (SCI) rehabilitation and discuss predictors (patient and injury characteristics) of the amount of time spent in PT for specific treatment activities.
Methods
Six hundred patients from six inpatient SCI centers were enrolled in the SCIRehab study. Physical therapists documented details, including time spent, of treatment provided during 37 306 PT sessions that occurred during inpatient SCI rehabilitation. Ordinary least squares regression models associated patient and injury characteristics with time spent in specific PT activities.
Results
SCIRehab patients received a mean total of 55.3 hours of PT over the course of their rehabilitation stay. Significant differences among four neurologic groups were seen in the amount of time spent on most activities, including the most common PT activities of strengthening exercises, stretching, transfer training, wheelchair mobility training, and gait training. Most PT work (77%) was provided in individual therapy sessions; the remaining 23% was done in group settings. Patient and injury characteristics explained only some of the variations seen in time spent on wheelchair mobility, transfer and bed mobility training, and range of motion/stretching.
Conclusion
Analysis yielded both expected and unexpected trends in SCI rehabilitation. Significant variation was seen in time spent on PT activities within and among injury groups. Providing therapeutic strengthening treatments consumed the greatest proportion of PT time. About one-quarter of all PT services were provided in group settings. Details about services provided, including time spent, will serve as a starting point in detailing the optimal treatment delivery for maximal outcomes.
Keywords: Spinal cord injuries, Rehabilitation, Health services research, Physical therapy, Paraplegia, Tetraplegia
Introduction
Physical therapy (PT) is a key component of the rehabilitation process following spinal cord injury (SCI), and includes a variety of interventions that address multiple domains in the International Classification of Functioning, Disability and Health (ICF) adopted by World Health Organization (WHO).1 These domains include body function and structure, activity limitation, and participation. When applying these concepts in the context of rehabilitation following SCI, body function and structure refer to impairments in sensation or motor function, range of motion (ROM) limitations, musculoskeletal pain, etc. Activity limitation refers to deficits in daily tasks such as rolling in bed or propelling a wheelchair. Participation refers to activities that contribute to social and leisure skill roles, such as homemaker, sports participant, or college student.
The SCI rehabilitation process typically includes multiple phases that take place over a period of weeks, months, or years. For many patients with SCI, the foundation of this process is laid during inpatient rehabilitation where primary goals include maximizing independence with basic skills (bed mobility, wheelchair management, and transfers), progression to ambulation if appropriate, caregiver training, provision of equipment, and education (on topics such as pressure relief, medical complications, etc.). A number of investigations have examined the impact of the timing, intensity, or duration of inpatient rehabilitation programs on rehabilitation outcomes, and have associated participation in inpatient rehabilitation for SCI with functional gains.2–7
While these studies help build evidence for the importance of specialized inpatient rehabilitation programs for SCI, they are limited in that they provide few details about the specific interventions provided within the rehabilitation package. As a result, such studies provide little guidance on the interventions that rehabilitation clinicians should select for a given patient and how these interventions should be delivered to maximize positive outcomes. In recent years, efforts have been made by van Langeveld et al.8,9 and others10 to develop systems for classifying SCI rehabilitation interventions, so that the specific components of rehabilitation programs can be described and studied in detail. A better understanding of the nature of interventions delivered in inpatient rehabilitation is critical to assessing how specific interventions relate to rehabilitation outcomes.
The ongoing SCIRehab project aims at filling the gaps in knowledge about the nature and impact of specific interventions provided in inpatient rehabilitation for traumatic SCI. This 5-year, multi-center investigation is recording and analyzing the details of the SCI inpatient rehabilitation process for approximately 1400 patients and will relate them to first-year post-injury outcomes. The study design and implementation of its practice-based evidence (PBE) methods have been described previously.11,12 In general, the process of PBE involves describing and defining the content and timing of treatments/services provided in the clinical setting in order to determine which of those treatments/services are associated with the best outcomes. PBE studies also consider the health status of the patient when evaluating relationships between treatments/services and outcomes, since patients' health status may well impact the clinicians' choice of interventions and patients' response to those interventions.
The first phase of the SCIRehab project involved the creation of a taxonomy of rehabilitation interventions.10,13–18 Representatives from each of the six study centers participated in a consensus-driven process that used a multi-faceted approach to include all potential elements of the rehabilitation process. The PT taxonomy includes 20 PT activities that are conducted in individual and/or group therapy sessions.10 It is embedded in an electronic documentation system that also captures information about the amount of time patients spend in classes led by physical therapists (PTs) and in clinics facilitated by PT (e.g. seating and positioning, spasticity, wound/skincare) – as well as the time PTs spend participating in interdisciplinary conferences to discuss patients' goals and progress.
Data collection was ongoing at the time of this writing, and analyses related to outcomes will take place in later phases of the study. The current paper describes the nature and distribution of activities in which patients participated during PT sessions and discusses predictors (patient, injury, and clinician characteristics) of the amount of time spent in PT, and specifically in different treatment activities.
Methods
The first paper in this SCIRehab series19 describes the project's study design, including use of PBE research methodology,11,12,20–23 study details such as inclusion criteria, data sources, and the analysis plan. Briefly, the SCIRehab team included representatives of all rehabilitation clinical disciplines, including PT, from six inpatient rehabilitation facilities: Craig Hospital, Englewood, CO; Shepherd Center, Atlanta, GA; Rehabilitation Institute of Chicago, Chicago, IL; Carolinas Rehabilitation, Charlotte, NC; Mount Sinai Medical Center, New York, NY; and National Rehabilitation Hospital, Washington, DC. Institutional Review Board (IRB) approval was obtained at each center and patients who were 12 years of age or older, provided informed consent (independently or via a parent or guardian), and were admitted to the facility's SCI unit for initial rehabilitation following traumatic SCI were enrolled.
Patient/injury and clinician data
The International Standards of Neurological Classification of SCI (ISNCSCI),24 which describe the motor level and completeness of injury, were used to place patients into four injury groups based on ISNCSCI examination. Patients with American Spinal Injury Association Impairment Scale (AIS) grade D were grouped together regardless of injury level. Patients with AIS classifications of A, B, and C were grouped together and separated by motor level to determine the remaining three categories: patients with high tetraplegia (C1–C4), those with low tetraplegia (C5–C8), and patients with paraplegia (T1 and below). These injury categories were selected because they were each large enough for analysis and created groupings thought to have relatively homogenous functional ability within groups and clear differences between the groups. The Comprehensive Severity Index (CSI®) was used to score the severity of each of a patient's complications and comorbidities at the time of rehabilitation admission and over time during rehabilitation. In the CSI system, higher scores are given for greater deviations from a ‘normal’ health state, such that higher CSI scores may be interpreted as greater levels of morbidity or medical complexity.25–29 The FIM® was used to describe a patient's independence with specific motor and cognitive abilities at rehabilitation admission and discharge.30,31 Trained data abstractors collected patient and injury data from patient medical records. PTs who documented treatment completed a clinician profile that included their years of SCI rehabilitation experience at the start of the project.
PT Treatment data collection
PTs who provided care to patients enrolled in the project recorded details about each PT session they provided using a handheld personal digital assistant (PDA) (Hewlett Packard PDA hx2490b, Palo Alto, CA) that contained a modular custom software application. The point-of-care documentation system (PointSync Pro version 2.0, MobileDataforce, Boise, ID, USA) on the devices included the PT taxonomy.10 Activities included in the taxonomy are contained in Table 1 and are based partly on concepts presented in the ICF taxonomy. The ICF model does not make those distinctions – it just differentiates body structures/functions, activity (limitations), and participation (restrictions). The ICF taxonomy does make distinctions related to those in Table 1. The mobility grouping consists primarily of interventions that address activity limitations, while interventions in the preparatory grouping address impairments in body function or structure. Other interventions that do not align fully with ICF categories are listed in the ‘other care activities’ group.
Table 1.
Physical therapy activities – individual and group therapy combined: percent of patients receiving each type of activity, mean number of minutes per week (SD), and total hours (SD)*
| Full SCIRehab Sample (n = 600) | 1–C4 AIS A, B, C (n = 132) | C5–C8 AIS A, B, C (n = 151) | Para AIS A, B, C (n = 223) | AIS D (n = 94) | |
|---|---|---|---|---|---|
| Any physical therapy activities | |||||
| % of patients | 100 | 100 | 100 | 100 | 100 |
| Minutes per week† | 442.3 (127.2) | 393.0 (118.1) | 434.1 (101.9) | 463.1 (140.0) | 475.6 (123.8) |
| Total hours | 55.3 (35.1) | 65.1 (34.4) | 66.0 (36.4) | 49.2 (32.6) | 38.8 (29.7) |
| Group 1: mobility training | |||||
| Bed Mobility | |||||
| % of patients | 87 | 79 | 94 | 95 | 66 |
| Minutes per week† | 18.5 (17.9) | 9.2 (11.3) | 26.8 (20.0) | 22.7 (17.8) | 8.5 (10.3) |
| Total hours† | 2.3 (2.4) | 1.5 (1.7) | 3.8 (3.2) | 2.3 (2.0) | 0.8 (1.2) |
| Gait | |||||
| % of patients | 36 | 23 | 23 | 27 | 96 |
| Minutes per week† | 29.8 (57.7) | 13.7 (32.0) | 14.8 (36.8) | 14.6 (40.5) | 112.6 (75.4) |
| Total hours† | 2.6 (5.5) | 2.2 (5.5) | 1.9 (5.7) | 1.3 (3.6) | 7.5 (6.1) |
| Transfers | |||||
| % of patients | 98 | 100 | 99 | 100 | 90 |
| Minutes per week† | 55.7 (34.2) | 37.4 (19.9) | 52.1 (25.8) | 78.7 (35.3) | 32.3 (24.5) |
| Total hours† | 6.7 (4.7) | 6.3 (4.5) | 7.4 (4.2) | 8.0 (4.6) | 3.0 (3.6) |
| Wheelchair mobility – manual | |||||
| % of patients | 85 | 71 | 90 | 96 | 68 |
| Minutes per week† | 36.6 (45.7) | 8.9 (18.5) | 26.5 (27.5) | 69.5 (53.7) | 13.4 (21.7) |
| Total hours† | 4.2 (6.0) | 1.4 (2.8) | 4.1 (5.2) | 7.3 (7.4) | 1.2 (2.2) |
| Wheelchair mobility – power | |||||
| % of patients | 47 | 88 | 73 | 16 | 21 |
| Minutes per week† | 12.9 (24.9) | 33.3 (37.5) | 16.2 (22.8) | 2.3 (7.4) | 3.6 (9.8) |
| Total hours† | 1.5 (2.8) | 4.0 (3.9) | 2.0 (2.5) | 0.3 (0.8) | 0.5 (1.3) |
| Group 2: preparatory interventions | |||||
| Airway/respiratory management | |||||
| % of patients | 16 | 34 | 21 | 5 | 6 |
| Minutes per week† | 1.3 (5.3) | 2.9 (7.4) | 1.9 (7.1) | 0.3 (1.9) | 0.3 (1.7) |
| Total hours† | 0.2 (0.9) | 0.5 (1.3) | 0.3 (1.1) | 0.1 (0.4) | <0.0 (0.2) |
| Aquatic exercises | |||||
| % of patients | 21 | 24 | 21 | 19 | 19 |
| Minutes per week | 4.8 (12.3) | 5.5 (12.5) | 4.2 (11.1) | 4.5 (11.9) | 5.9 (14.8) |
| Total hours | 0.9 (2.3) | 1.2 (2.8) | 0.9 (2.4) | 0.7 (1.7) | 0.8 (2.3) |
| Complementary approaches | |||||
| % of patients | 3 | 4 | 6 | 1 | 0 |
| Minutes per week | 0.1 (0.7) | 0.1 (0.9) | 0.2 (1.0) | 0.1 (0.5) | <0.0 (<0.0) |
| Total hours† | 0.2 (0.1) | 0.3 (0.2) | <0.0 (0.2) | <0.0 (0.1) | <0.0 (<0.0) |
| Musculoskeletal treatment modalities | |||||
| % of patients | 68 | 80 | 78 | 60 | 52 |
| Minutes per week† | 13 (18.4) | 20.0 (21.5) | 16.5 (21.3) | 8.0 (13.0) | 9.0 (14.8) |
| Total hours† | 1.9 (3.8) | 3.5 (4.4) | 2.6 (5.1) | 1.0 (2.2) | 1.0 (2.5) |
| Pre-gait | |||||
| % of patients | 33 | 25 | 28 | 28 | 62 |
| Minutes per week* | 5.1 (12.0) | 2.9 (7.1) | 4.4 (12.7) | 4.4 (11.4) | 11.1 (15.7) |
| Total hours | 0.56 (1.4) | 0.5 (1.3) | 0.6 (2.0) | 0.4 (0.8) | 1.1 (1.8) |
| Skin management | |||||
| % of patients | 49 | 64 | 59 | 46 | 19 |
| Minutes per week† | 3.5 (8.0) | 3.6 (5.4) | 4.5 (6.7) | 4.0 (10.9) | 0.8 (2.0) |
| Total hours† | 0.5 (1.1) | 0.7 (1.1) | 0.7 (1.5) | 0.4 (1.0) | 0.1 (0.2) |
| Balance exercises | |||||
| % of patients | 84 | 68 | 90 | 87 | 86 |
| Minutes per week† | 18.9 (20.2) | 12.2 (17.5) | 18.8 (16.5) | 19.4 (16.6) | 27.2 (31.1) |
| Total hours† | 2.2 (2.4) | 1.9 (2.5) | 2.9 (3.1) | 2.1 (2.0) | 1.8 (1.6) |
| Endurance exercises | |||||
| % of patients | 61 | 60 | 59 | 57 | 76 |
| Minutes per week | 14.7 (23.0) | 13.6 (22.7) | 17.8 (27.9) | 12.0 (18.3) | 17.2 (23.7) |
| Total hours† | 2.4 (4.8) | 2.9 (5.3) | 3.7 (6.6) | 1.6 (3.0) | 1.6 (3.4) |
| Range of motion/stretching | |||||
| % of patients | 96 | 99 | 100 | 98 | 77 |
| Minutes per week† | 54.5 (35.4) | 77.9 (36.4) | 60.0 (31.9) | 50.2 (29.1) | 22.4 (25.1) |
| Total hours† | 7.6 (7.5) | 13.4 (1.0) | 8.8 (6.1) | 5.6 (5.0) | 2.4 (3.9) |
| Strengthening exercises | |||||
| % of patients | 99 | 98 | 99 | 100 | 99 |
| Minutes per week† | 85.1 (63.6) | 63.6 (52.9) | 80.2 (52.8) | 83.4 (66.1) | 126.9 (68.6) |
| Total hours† | 10.5 (10.1) | 10.4 (11.4) | 12.6 (10.6) | 9.0 (8.9) | 10.6 (9.8) |
| Upright work | |||||
| % of patients | 72 | 82 | 81 | 73 | 37 |
| Minutes per week† | 14.1 (15.1) | 16.5 (15.5) | 17.6 (16.4) | 14.2 (14.2) | 5.3 (10.6) |
| Total hours† | 1.9 (2.4) | 2.6 (2.7) | 2.7 (2.8) | 1.5 (1.8) | 0.6 (1.4) |
| Wound care | |||||
| % of patients | 5 | 5 | 8 | 4 | 3 |
| Minutes per week | 1.4 (11.3) | 1.8 (17.5) | 1.6 (7.8) | 1.4 (10.6) | 0.9 (5.5) |
| Total hours | 0.2 (1.1) | 0.2 (1.4) | 0.3 (1.5) | 0.1 (0.8) | 0.1 (0.6) |
| Group 3: other care activities | |||||
| Assessment | |||||
| % of patients | 86 | 89 | 86 | 81 | 94 |
| Minutes per week† | 17.8 (17.2) | 14.3 (12.3) | 14.9 (12.6) | 15.3 (14.4) | 33.1 (25.7) |
| Total hours† | 1.9 (1.8) | 2.2 (1.9) | 2.2 (2.0) | 1.5 (1.5) | 2.1 (1.6) |
| Classes led by PT | |||||
| % of patients | 23 | 30 | 25 | 18 | 21 |
| Minutes per week | 3.8 (9.3) | 4.2 (9.0) | 3.3 (7.2) | 4.2 (11.2) | 3.3 (7.8) |
| Total hours† | 0.4 (1.1) | 0.8 (1.7) | 0.5 (1.0) | 0.3 (0.7) | 0.2 (0.6) |
| Clinics led by PT | |||||
| % of patients | 4 | 8 | 3 | 4 | 0 |
| Minutes per week | 0.6 (3.3) | 0.7 (2.6) | 0.5 (2.8) | 0.8 (4.4) | 0.0 (0.0) |
| Total hours | 0.1 (0.6) | 0.2 (0.7) | 0.1 (0.6) | 0.1 (0.6) | 0.0 (0.0) |
| Education | |||||
| % of patients | 79 | 85 | 86 | 80 | 6 |
| Minutes per week | 12.2 (15.9) | 13.3 (15.4) | 12.2 (11.2) | 12.8 (15.5) | 9.5 (22.4) |
| Total hours† | 1.6 (2.0) | 2.2 (2.3) | 1.9 (2.1) | 1.4 (1.7) | 0.8 (1.9) |
| Equipment evaluation and provision | |||||
| % of patients | 84 | 90 | 89 | 87 | 61 |
| Minutes per week† | 18.1 (16.9) | 19.9 (14.9) | 19.3 (15.5) | 21.1 (19.1) | 6.7 (10.2) |
| Total hours† | 2.4 (2.7) | 3.3 (2.8) | 2.9 (2.7) | 2.3 (2.7) | 0.7 (1.4) |
| Interdisciplinary conferences | |||||
| % of patients | 100 | 100 | 100 | 100 | 100 |
| Minutes per week† | 20.1 (15.7) | 17.4 (8.7) | 20.0 (14.9) | 19.4 (14.9) | 25.6 (23.2) |
| Total hours† | 2.5 (2.2) | 3.2 (2.3) | 3.0 (2.3) | 2.1 (2.0) | 1.9 (1.9) |
*Hours and minutes per week are calculated as averages over all 600 patients, not just based on those who did receive one or more sessions of a particular activity.
†Statistically significant differences in mean minutes per week or total minutes among groups.
PTs documented the date/time of each session, the number of minutes spent on intervention activities performed in the session, activity-specific details, patient and family participation, and factors that limited or impacted session activities. Interventions provided for less than 5 minutes were not documented. Each clinician was trained and tested quarterly on use of the documentation system. The project's site coordinators compared session entries with clinical documentation of treatment provided (chart notes, schedules, and/or billing records) on a regular basis to assess data collection completeness and take steps to obtain documentation of sessions not contained in the database.
Data analysis
Analyses reported here are for patients enrolled in the SCIRehab project's first year of enrollment and focus on time spent in specific PT activities overall and by patient injury grouping. The total amount of time spent in PT was first calculated by summing the amount of time recorded for each PT activity during the patient's rehabilitation stay. Total time, however, has a linear relationship with time spent in rehabilitation (length of stay), which varied from 2 to 259 (mean 55) days; therefore, minutes of treatment per week were calculated and examined as the primary measure of therapy intensity. Contingency tables/chi-square tests and analysis of variance were used to test differences across injury groups for categorical and continuous variables, respectively. (A P value less than 0.05 was considered statistically significant.)
Ordinary least squares stepwise regression models were used to identify patient and injury characteristics associated with time spent on common PT activities, where the standard for ‘common’ was that more than 70% of patients had the activity at least once. The strength of a regression model is determined by the R2 value, which indicates that amount of variation explained by the significant independent variables. Type II semi-partial correlation coefficients allow for comparison of the unique contribution of each predictor variable after controlling for all other variables in the model.32,33 Parameter estimates indicate the direction and strength of the association between each statistically significant independent variable (predictor) with the dependent variable (outcome). The predictors used were gender, marital status, racial/ethnic group, traumatic SCI etiology, body mass index (BMI), English-speaking status, third-party payer, pre-injury occupational status, severity of illness (CSI) score, age, FIM score, experience level of the clinician, and injury grouping. Only if the predictors jointly explained more than 20% of the variance in the number of minutes per week for a PT activity are model details shown.
Results
The SCIRehab project enrolled 600 patients during its first year. Details of patient demographic and injury characteristics are presented for the sample as a whole and for each of the injury groups separately in Table 1 of the first article in this series19. The average age of subjects was 37 years (standard deviation (SD) = 17). The sample was 65% white (22% black), 81% male, 38% married, 82% had a BMI of <30, and 65% were employed at the time of injury. Vehicular accidents were the most common cause of injury (49%), falls accounted for 23%, etiology of sports for 12%, violent etiologies for 11%, and the remaining 5% were classified as other. The mean rehabilitation length of stay was 55 days (range 2–259 days, SD 37, median 43). The mean total FIM score at admission was 53 (motor score of 24 and cognitive score of 29), and a mean of 32 days had elapsed from the time of injury to the time of rehabilitation admission.
The PTs who contributed to data collection documented treatment using all 20 PT activities provided during 37 306 PT sessions. In addition, PTs recorded time patients spent in classes or clinics that were facilitated by PTs and time that PTs spent in interdisciplinary conferences discussing patient goals and progress. Table 1 presents time spent in these activities for individual and group therapy combined expressed as total hours over the full rehabilitation stay and as an average number of minutes per week, for the full sample and for the four injury groups separately. Also shown is the percentage of patients who received each activity. Mean hours and minutes per week are based on all patients, not just those receiving each treatment. Significant differences among the four injury groups were seen in the amount of time spent on most activities, including the most commonly delivered PT activities: ROM/stretching, strengthening exercises, transfer training, manual wheelchair mobility training, and gait training.
Most PT (77%) was provided in individual therapy sessions; the remaining 23% was delivered in groups. Table 2 depicts the same information included in Table 1 for time spent in individual therapy only. For patients with AIS ABC level of impairment, the three most frequent activities (transfers, ROM, and strengthening) in individual therapy sessions were the same regardless of motor level of injury, although there was significant variation in time spent among injury groups in terms of the rank order of these activities. The three most common individual therapy activities for patients with high tetraplegia were ROM/stretching (23% of total mean minutes per week), strengthening, and transfers (11% each). Most individual therapy time for patients with low tetraplegia (C5–C8) was spent on ROM/stretching, transfers, and strengthening (16, 14, and 12%, respectively). For patients with paraplegia, the most common individual PT activities were transfers (22%), ROM/stretching (12%), and strengthening (11%). The most prominent activities differed for patients with AIS D: gait training (15%), strengthening (11%), and balance exercises (9%).
Table 2.
Physical therapy activities – individual therapy only: percent of patients receiving each type of activity, mean number of minutes per week (SD), and total hours (SD)*
| Full SCIRehab Sample (n = 600) | C1–C4 AIS A, B, C (n = 132) | C5–C8 AIS A, B, C (n = 151) | Para AIS A, B, C (n = 223) | AIS D (n = 94) | |
|---|---|---|---|---|---|
| Physical therapy activities | |||||
| % of patients | 100 | 100 | 100 | 100 | 100 |
| Minutes per week | 341.2 (82.4) | 332.4 (84.2) | 355 (79.7) | 339.8 (74.5) | 336.1 (98.9) |
| Total hours | 42.3 (25.0) | 54.7 (26.5) | 52.4 (25.2) | 34.7 (18.9) | 26.8 (19.9) |
| Group 1: mobility training | |||||
| Bed mobility | |||||
| % of patients | 86 | 79 | 94 | 94 | 65 |
| Minutes per week* | 18 (17.6) | 9.1 (11.2) | 26.4 (20.0) | 21.7 (17.4) | 8.2 (10.3) |
| Total hours† | 2.2 (2.4) | 1.5 (1.7) | 3.8 (3.2) | 2.2 (1.9) | 0.8 (1.2) |
| Gait | |||||
| % of patients | 36 | 23 | 23 | 26 | 96 |
| Minutes per week† | 21.2 (39.8) | 10.6 (25.3) | 11.5 (29.2) | 10.3 (24.3) | 77.7 (52.0) |
| Total hours† | 1.8 (3.6) | 1.7 (4.1) | 1.3 (3.0) | 0.9 (2.3) | 5.2 (3.9) |
| Transfers | |||||
| % of patients | 98 | 100 | 99 | 100 | 89 |
| Minutes per week† | 52.8 (33.2) | 36.1 (19.0) | 50.5 (25.5) | 74.2 (35.2) | 29.4 (23.0) |
| Total hours† | 6.3 (4.3) | 6.1 (4.2) | 7.2 (4.0) | 7.4 (4.2) | 2.7 (3.1) |
| Wheelchair mobility – manual | |||||
| % of patients | 84 | 70 | 90 | 96 | 67 |
| Minutes per week† | 19.3 (22.3) | 4.9 (5.2) | 17.5 (18.0) | 33.7 (26.1) | 7.8 (9.2) |
| Total hours† | 1.9 (1.9) | 0.8 (0.9) | 2.3 (2.0) | 2.9 (1.9) | 0.6 (0.8) |
| Wheelchair mobility – power | |||||
| % of patients | 44 | 88 | 70 | 11 | 20 |
| Minutes per week† | 8.7 (17.6) | 24.3 (26.2) | 10.4 (15.7) | 1.0 (5.3) | 2.1 (5.3) |
| Total hours† | 1.1 (2.1) | 3.0 (3.0) | 1.3 (1.8) | 0.1 (0.6) | 0.3 (0.9) |
| Group 2: preparatory interventions | |||||
| Airway/respiratory management | |||||
| % of patients | 15 | 34 | 21 | 5 | 5 |
| Minutes per week† | 1.1 (4.6) | 2.8 (7.2) | 1.5 (5.6) | <0.0 (1.6) | 0.1 (0.9) |
| Total hours† | 0.2 (0.8) | 0.5 (1.2) | 0.2 (0.8) | <0.0 (0.4) | <0.0 (0.1) |
| Aquatic exercises | |||||
| % of patients | 20 | 24 | 20 | 18 | 19 |
| Minutes per week | 4.7 (12.1) | 5.4 (12.5) | 4.1 (11.1) | 4.3 (11.7) | 5.5 (14.2) |
| Total hours | 0.8 (2.3) | 1.2 (2.8) | 0.1 (2.4) | 0.6 (1.7) | 0.8 (2.2) |
| Balance exercises | |||||
| % of patients | 82 | 67 | 90 | 85 | 86 |
| Minutes per week† | 15.6 (18.6) | 10.2 (14.3) | 17.0 (15.6) | 14.6 (14.0) | 23.5 (30.9) |
| Total hours† | 1.8 (2.2) | 1.6 (2.1) | 2.7 (3.1) | 1.5 (1.5) | 1.4 (1.3) |
| Complementary approaches | |||||
| % of patients | 2 | 2 | 6 | 1 | 0 |
| Minutes per week | 0.1 (0.6) | 0.1 (0.6) | 0.2 (1.0) | <0.0 (0.4) | — |
| Total hours† | <0.0 (0.1) | <0.0 (0.1) | <0.0 (0.2) | <0.0 (0.1) | — |
| Endurance exercises | |||||
| % of patients | 48 | 50 | 48 | 40 | 62 |
| Minutes per week | 7.5 (13.3) | 9.2 (16.2) | 7.3 (12.1) | 6.4 (12.8) | 8.5 (12.0) |
| Total hours† | 1.2 (2.8) | 2.0 (3.9) | 1.4 (2.8) | 0.8 (2.1) | 0.8 (2.0) |
| Musculoskeletal treatment modalities | |||||
| % of patients | 67 | 80 | 78 | 58 | 51 |
| Minutes per week† | 12.7 (18.3) | 19.9 (21.4) | 16.4 (21.1) | 7.9 (12.9) | 8.4 (14.7) |
| Total hours† | 1.9 (3.8) | 3.5 (4.4) | 2.6 (5.1) | 1.0 (2.2) | 0.9 (2.5) |
| Pre-gait | |||||
| % of patients | 30 | 23 | 26 | 25 | 59 |
| Minutes per week† | 4.1 (9.9) | 2.4 (6.3) | 3.3 (9.7) | 3.5 (10.2) | 8.9 (12.0) |
| Total hours† | 0.4 (1.0) | 0.4 (1.0) | 0.4 (1.2) | 0.3 (0.7) | 0.8 (1.2) |
| Range of motion/stretching | |||||
| % of patients | 95 | 99 | 100 | 98 | 73 |
| Minutes per week† | 49.2 (34.6) | 75.1 (37.0) | 57.4 (31.5) | 40.8 (25.3) | 19.4 (23.0) |
| Total hours† | 6.9 (7.2) | 12.9 (9.8) | 8.4 (5.8) | 4.3 (4.0) | 2.0 (3.3) |
| Skin management | |||||
| % of patients | 46 | 63 | 56 | 41 | 19 |
| Minutes per week† | 3.3 (7.9) | 3.5 (5.3) | 4.2 (6.6) | 3.6 (10.8) | 0.8 (2.0) |
| Total hours† | 0.5 (1.1) | 0.6 (1.1) | 0.7 (1.5) | 0.4 (0.9) | 0.1 (0.2) |
| Strengthening exercises | |||||
| % of patients | 98 | 98 | 99 | 98 | 97 |
| Minutes per week† | 41.5 (31.6) | 37.1 (28.5) | 43.2 (28.5) | 36.3 (30.9) | 57.2 (36.9) |
| Total hours† | 4.9 (4.3) | 5.6 (4.4) | 6.5 (5.3) | 3.6 (3.3) | 4.4 (3.6) |
| Upright work | |||||
| % of patients | 71 | 82 | 81 | 71 | 37 |
| Minutes per week† | 13.1 (14.3) | 15.7 (15.1) | 16.3 (15.1) | 12.7 (13.4) | 4.8 (9.8) |
| Total hours† | 1.8 (2.2) | 2.4 (2.4) | 2.5 (2.6) | 1.4 (1.8) | 0.6 (1.3) |
| Wound care | |||||
| % of patients | 5 | 5 | 8 | 4 | 3 |
| Minutes per week | 1.4 (11.3) | 1.8 (17.5) | 1.6 (7.8) | 1.4 (10.6) | 0.9 (5.5) |
| Total hours | 0.2 (1.1) | 0.2 (1.4) | 0.3 (1.5) | 0.1 (0.8) | 0.1 (0.6) |
| Group 3: other care activities | |||||
| Assessment | |||||
| % of patients | 86 | 88 | 86 | 81 | 94 |
| Minutes per week† | 17.6 (17.1) | 14.1 (12.1) | 14.8 (12.6) | 15.1 (14.2) | 33.1 (25.7) |
| Total hours† | 1.9 (1.7) | 2.2 (1.9) | 2.2 (2.0) | 1.5 (1.5) | 2.1 (1.6) |
| Education | |||||
| % of patients | 76 | 83 | 82 | 77 | 52 |
| Minutes per week | 10.8 (14.9) | 12.3 (14.7) | 11.4 (11.0) | 10.9 (13.8) | 7.7 (21.6) |
| Total hours† | 1.4 (1.9) | 2.0 (2.2) | 1.8 (2.1) | 1.2 (1.5) | 0.6 (1.6) |
| Equipment evaluation, education, and provision | |||||
| % of patients | 84 | 90 | 89 | 87 | 60 |
| Minutes per week† | 17.9 (16.7) | 19.7 (14.8) | 19.1 (15.5) | 20.7 (18.8) | 6.6 (9.9) |
| Total hours† | 2.4 (2.7) | 3.2 (2.8) | 2.9 (2.7) | 2.3 (2.6) | 0.7 (1.3) |
*Hours and minutes per week are averages calculated over all 600 patients, not just based on those who did receive one or more sessions of a particular activity.
†Statistically significant differences in mean minutes per week or hours among groups.
Activities used in group therapy varied among injury categories; however, strengthening was the most common group therapy activity for patients in each of the injury categories (38–50%). For patients with C1–C4 ABC injuries, the two most common activities following strengthening were power wheelchair mobility and endurance (15 and 7%, respectively). For patients with C5–C8 ABC injuries, the second and third most common activities were endurance training (13%) and manual wheelchair mobility (11%). Patients with Para ABC injuries also worked on manual wheelchair mobility (29%) and ROM/stretching (8%). Finally, those patients with AIS D injuries worked on gait training (25%) and endurance (6%) in group sessions.
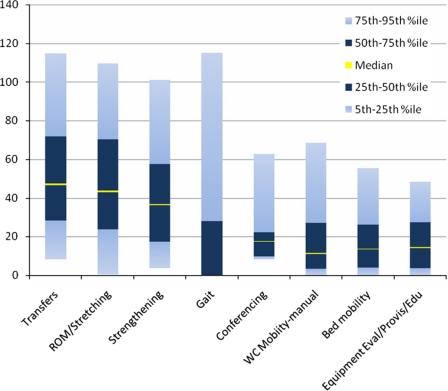
Fig. 1 depicts the substantial variation in mean minutes per week spent within the eight activities that consumed the most time during individual PT sessions. For transfer work, the interquartile range (IQR) was 28–72 (median 47); it was 24–70 (median 44) for ROM/stretching exercises, and for strengthening/endurance exercises the IQR was 17–58 (median 37) minutes per week. The IQR for gait training was 0–28 (more than 25% of patients received no gait training); however, for patients with AIS D, who received most of the gait training work, the IQR was 35–115 (median 70) minutes per week.
Figure 1.
Variation in time spent (minutes per week) on PT activities during individual therapy sessions (includes only the eight activities that were used the most often).
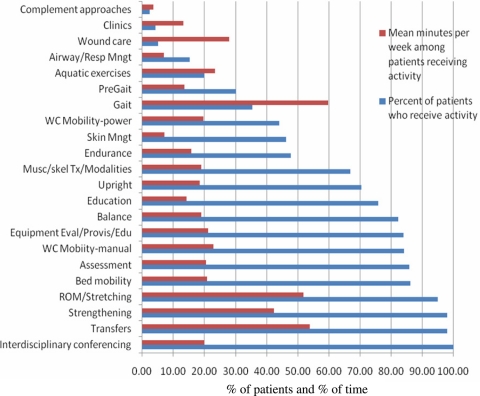
Fig. 2 displays the percentage of patients who received each PT activity during individual therapy sessions and the mean number of minutes per week spent on each activity, for these patients only. PTs participated in interdisciplinary conferences for all patients (100%), which consumed approximately 20 minutes per week. Almost all patients received strengthening exercises and transfer training; a mean of 42 minutes per week was spent on strengthening and 54 minutes per week on transfer training. In contrast, only 36% of patients received gait training but, for these patients, a mean of 60 minutes per week was devoted to gait work.
Figure 2.
Physical therapy activities in individual sessions: percent of patients receiving each and mean minutes per week for those receiving each.
Some of the variation seen in time spent (minutes per week) on PT activities can be attributed to patient and injury characteristics, as shown in Table 3. Only regression models for PT activities where R2 values were greater than 0.2 (and, thus, explain at least 20% of the variation) are presented. The parameter estimate indicates the strength and direction (how much (more or less) time was spent (in minutes per week)) of the association between each independent variable with the dependent variable. The semi-partial R2 value signifies the unique percent contribution that the independent variable adds to the total R2 for the model after controlling for all other variables in the model. For manual wheelchair mobility, the regression model explained 41% of the variation in time spent (R2 = 0.41). The parameter estimate for injury group: Para ABC (independent variable) was 46.86, which indicated that patients in this group received an average of nearly 47 minutes per week more of wheelchair mobility training than patients in the other injury groups and the semi-partial R2 indicated that this was the largest explanatory variable (it contributed 15% to the total R2). Older age, more days from injury to rehabilitation admission, race – black, and sports-related injury were associated with less time spent on wheelchair mobility training (negative parameter estimates).
Table 3.
Patient and injury characteristics associated with time (minutes per week) spent in physical therapy activities*,†
| Wheelchair mobility – manual |
Transfers |
Bed mobility |
ROM/stretching |
Assessment |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total R2 | 0.41 |
0.36 |
0.25 |
0.26 |
0.23 |
|||||
| Independent variables | Parameter estimate | Type II semi-partial R2 | Parameter estimate | Type II semi-partial R2 | Parameter estimate | Type II semi-partial R2 | Parameter estimate | Type II semi-partial R2 | Parameter estimate | Type II semi-partial R2 |
| Injury group: Para ABC | 46.86 | 0.15 | 48.89 | 0.31 | −6.11 | 0.02 | ||||
| Injury group: C1–C4 ABC | −17.21 | 0.12 | 17.84 | 0.03 | ||||||
| Injury group: C5–C8 ABC | 13.20 | 0.01 | 16.38 | 0.03 | ||||||
| Injury group: AIS D | −16.27 | 0.10 | −28.25 | 0.08 | 13.12 | 0.05 | ||||
| Admission FIM motor score | 0.50 | 0.12 | −0.49 | 0.02 | −0.24 | 0.02 | −0.41 | 0.02 | 0.38 | 0.04 |
| Admission FIM cognitive score | −0.27 | 0.01 | 0.25 | 0.01 | ||||||
| Severity of illness score (CSI) | −0.13 | 0.01 | ||||||||
| Age at injury | −0.55 | 0.04 | ||||||||
| Traumatic etiology – vehicular | 7.66 | 0.01 | ||||||||
| Traumatic etiology – sports | −11.40 | 0.01 | ||||||||
| Payer – Medicaid | −8.85 | 0.01 | −4.49 | 0.01 | ||||||
| Clinician experience | 0.96 | 0.01 | −0.40 | 0.01 | 0.41 | 0.01 | ||||
| Race – black | −10.22 | 0.01 | 4.44 | 0.01 | ||||||
| Race – other‡ | −5.73 | 0.01 | ||||||||
| Days from injury to rehab admission | −0.15 | 0.01 | 0.13 | 0.01 | ||||||
| Ventilator use at rehab admit | −8.03 | 0.01 | ||||||||
| Injury work related | −8.05 | 0.01 | ||||||||
| Employment status at injury – other§ | 15.17 | 0.01 | 5.78 | 0.01 | ||||||
*The activities listed in Table 1 are included here only if total R2 > 0.20 and if more than 70% of the patients received the treatment activity.
†Independent variables allowed into models: age at injury, male, married, race – white, race – black, race – Hispanic, race – other, admission FIM motor score, admission FIM cognitive score, severity of illness score (CSI), injury group – C1–C4 ABC, injury group – C5–C8 ABC, injury group – Para ABC, injury group – AIS D, clinician experience, traumatic etiology – vehicular, traumatic etiology – violence, traumatic etiology – falls, traumatic etiology – sports, traumatic etiology – medical/surgical complication, traumatic etiology – other, work-related injury, number of days from trauma to rehabilitation admission, BMI >40, BMI 30–40, BMI <30, language – English, language – no English, language – English sufficient for understanding, payer – Medicare, payer – worker compensation, payer – private, payer – Medicaid, employment status at the time of injury – employed, employment status at the time of injury – student, employment status at time of injury – retired, employment status at time of injury – unemployed, employment status at time of injury – other, ventilator use at rehabilitation admission.
‡Race – other subcategory includes Native American, Asian/Pacific Islander, and unknown.
§Employment status at injury ‘other’ category includes retired, unemployed, homemaker, on-job training, sheltered workshop, and unknown.
The regression model for transfer training also was quite robust; the R2 value was 0.36, which means that 36% of the variation in time spent (minutes per week) was explained by the patient and injury characteristics examined here. Injury group: Para ABC again was the strongest predictor (type II semi-partial R2 = 0.31); the parameter estimate was 48.89, which means that patients in this injury group spent approximately 49 more minutes per week practicing transfers than patients in the other injury groups.
Discussion
Activity selection within impairment groups
Statistically significant differences in time spent on PT activities were seen among injury groups and the pattern of interventions delivered shows a focus on impairment-oriented interventions for patients with higher levels of injury. PTs focused primarily on ROM/stretching and strengthening when working with patients with high tetraplegia (C1–C4). Patients need optimal ROM to build strength, which, in turn, can translate to advancement of functional tasks. This pattern of intervention delivery suggests that impairment-oriented interventions are being used to address underlying deficits and lay a foundation for training of functional skills. Furthermore, the pattern of delivery of interventions among groups fits well with traditional functional expectations for these groups. When working with individuals with high tetraplegia, for example, PTs focus on impairment-related activities, as well as education and family/caregiver training, rather than functional training since functional independence is not a likely goal. Independent performance of transfers is often a key therapy goal for patients with paraplegia; significantly more time was spent in transfer training with this subgroup of patients compared to the tetraplegia and AIS D groups. Patients classified as AIS D often have sufficient remaining function to make ambulation a realistic inpatient rehabilitation goal; patients in the AIS D group spent the majority of their PT time working on gait in addition to strengthening activities. The patterns of intervention delivery observed in the current study suggest that interventions are being matched to the functional deficits and needs of patients with SCI.
In the two tetraplegia groups nearly 23% of patients worked on gait. While gait training with patients with motor complete cervical injuries (AIS A or B), even with body weight support systems, is not a common PT practice, PTs may use body weight support to facilitate gait training with patients with incomplete injuries (AIS C)34 and this may explain the proportion of time spent on gait training in the tetraplegia groups. Patients with AIS C often have emerging lower extremity function, and literature suggests that ambulation is a realistic possibility for many of these patients.35 Patients with AIS C comprised approximately 30% of the high tetraplegia (C1–C4) group (39 patients). Of these 39 patients, 67% received some gait training and spent 43.6 minutes per week (SD 46.0) and 6.9 total hours (SD 7.9) on this training. There are 73 patients with AIS A and 20 patients with AIS B in this high tetraplegia group and only 2 patients in each of these AIS groups worked on gait training and for very short amounts of time.
Patients spent nearly a quarter (23%) of the time in PT group therapy. Groups are used for a variety of reasons: to supplement individual therapy sessions and enhance generalization of foundational skills, to reinforce functional goals, to provide peer interactions, and to allow patients to share alternative methods of skill performance. For example, a patient may attend a wheelchair group to practice skills learned during individual training, share ideas for how to master a particular skill (e.g. wheelies or door management), and continue to prepare for community mobility. Attending a lower extremity strengthening group helps to build muscles that facilitate progression toward gait training. Finally, groups can be used to accommodate changes in staffing models and to maximize hours of therapy provided.36 Others have demonstrated that group therapy may be beneficial for other disciplines, and in other patient diagnoses.37 Whether group or individual PT is more beneficial for the treatment of SCI is not yet known.
Assessment
One would expect all patients to have time documented as spent on initial assessment; however, only 87% of SCIRehab patients have assessment time recorded. This variability is due to some facilities having acute care hospitals on site; PTs assess patients during the acute care phase and then do not repeat evaluations as the patient transitions through the levels of care within the same system. Informal re-assessments that occur as a part of and during therapeutic work were not documented separately in the assessment category as PTs assess patient progress as a part of routine provision of treatment services.
Activities shared with other disciplines
It is common for PTs to share responsibility of setting goals and working toward maximal independence for some task training (e.g. transfers, bed mobility, and wheelchair mobility) with occupational therapists (OTs). Examining only the time that transfer training is done by PT (or only by OT) would not be an accurate reflection of the intensity of the practice of the activity. For example, PTs worked on transfer training skills with patients for 55.7 minutes per week of the rehabilitation stay; however, patients practiced transfers for a total of 71.8 minutes per week (mean) when combining work done with both PT and OT. Similarly, the total time patients worked on power wheelchair mobility training was 19.2 minutes per week (12.9 with PT and 6.3 with OT) and on bed mobility the total time was 23.9 minutes (18.5 with PT and 5.4 with OT).38 Reinforcement and repetition among both disciplines impact improvement in task performance and, thus, examining time spent by both disciplines is needed to obtain an accurate reflection of time and tasks that patients focus on during therapy sessions. Variations in quantity of therapy activity may also be explained by site-specific allocation of responsibility among disciplines in addition to PT and OT. Wound care and airway/respiratory management are shared among PT, OT, respiratory therapists, and/or nursing depending on facility care protocols. Only 16% of SCIRehab patients received respiratory management from PT, and most of these had C1–C4 or C5–C8 level injuries, which is consistent with impaired respiratory function associated with these levels of neurologic injury. Provision of aquatic therapy is dependent on physical accessibility of a pool. While 83% of SCIRehab patients received equipment evaluation and provision from PTs, OTs and nurses also provide this service depending on facility staffing, care protocols, or the patient's discharge location (skilled nursing facility vs. home).
Predicting time spent on PT activities
Multivariate regression analyses (for PT activities that had R2 values over 0.2 using the potential predictors used here) confirm descriptive analyses. The strongest predictor of more time spent on manual wheelchair mobility training, for example, was belonging to injury group Para ABC (semi-partial R2 =0.15), while inclusion to injury group C5–C8 ABC was a significant but weaker predictor (semi-partial R2 = 0.01). Most (96%) of the patients in the Para ABC group received manual wheelchair mobility training and they had the highest mean amount of time spent in the activity (mean 70 minutes per week). Of the C5–C8 group, 90% received manual wheelchair mobility training and they had the next highest mean minutes per week, although significantly less than the Para ABC group, amount of time (mean 27 minutes per week). Clinically, patients with low tetraplegia or paraplegia are most appropriate for functional manual wheelchair mobility training. Patients with high tetraplegia typically are not able to propel a manual wheelchair, while patients with AIS D injuries progress to functional ambulation as the primary mode of mobility, with less dependence on a manual wheelchair. Other predictors of therapy time also fit with clinical expectations. For example, patients who spend a longer time in acute care may be more medically complicated or have special issues (such as pressure ulcers) that make them less able to tolerate more advanced activities such as wheelchair mobility, resulting in their spending more time on basic activities such as ROM/stretching. However, some variables found to be predictive of time spent in specific PT activities will require further investigation. For example, one would not expect race to impact time spent on manual wheelchair mobility, bed mobility, or assessment. Similarly, it is not clear why etiology of injury was associated with less time spent on manual wheelchair mobility (sports related), and more time on transfers (vehicular). It is possible that other characteristics (such as injury severity, spinal stabilization, and the presence of other injuries such as limb fractures) may be associated with injury etiology, and that these characteristics, rather than the etiology itself, influence treatment type or intensity.
We conducted regression analyses to examine patient, injury, and clinician characteristics associated with time spent in PT activities. Typical PBE analytical strategy does not include center-specific effects because it is thought that center effects may result from underlying differences in patient, injury, or clinician characteristics among centers. Thus, looking directly at the impact of patient or injury characteristics rather than center effects may be more informative and may facilitate the application of findings to centers beyond those included in this study. We acknowledge, however, that there may be additional center-specific factors that may also influence the amount of time spent on PT activities. When centers were allowed to enter the regression models reported here for functional training (wheelchair mobility, transfers, bed mobility, and ROM/stretching), the explanatory power increased by 0.02–0.04. This minimal increase suggests that focusing on patient and injury characteristics is most helpful in explaining time spent in PT work, that center effects add little explanatory power, and that the significant variation in time spent on PT activities should prove useful in the eventual effort to correlate interventions with key patient outcomes.
Related work
Few investigations have sought to characterize the nature of inpatient PT interventions for SCI at the level of detail provided in the current investigation. During the time that the SCIRehab classification system was being developed, another classification system specific to SCI rehabilitation was being developed by van Langeveld and colleagues,8 the Spinal Cord Injury-Interventions Classification System (SCI-ICS). As part of work to validate the SCI-ICS, van Langeveld and colleagues performed a feasibility study in which a group of 36 clinicians (PTs, OTs, and sports therapists) used the system to describe in- or outpatient interventions they provided to patients with SCI over a 3–5-week period of typical clinical practice.9 Direct comparison of our findings with those of van Langeveld is difficult due to differences in the structure of the classification system, the inclusion of OT and sports therapy interventions in addition to PT interventions, and the inclusion of both inpatient and outpatient therapy sessions in their data set. However, some similarities in the nature of interventions delivered are apparent. The top five activities by amount of therapy time recorded (in minutes) were ‘muscle power’ (14.5% of therapy minutes), ‘wheelchair driving and hand biking’ (10.6%), ‘muscle length’ (9.5%), ‘walking’ (8.2%), and ‘joint mobility’ (6.6%). These activities also were observed in our sample, particularly strengthening, ROM/stretching, and transfers.
Future studies
Our injury grouping convention kept patients with AIS C together with those with AIS A and B for all motor levels of injury. Distinguishing incomplete injuries (AIS C) from complete injuries will be important when PT treatments are associated with patient outcomes at 1 year post injury. Patients with motor incomplete injuries will most likely achieve higher functional levels than their counterparts with similar injury level, but motor complete (AIS A or B) injury classification. Evidence suggests that individuals with AIS C classification have the potential to achieve improvements in walking with locomotor training39,40 and, therefore, PTs are more likely to employ locomotor training with these patients but not with patients with complete injuries. Similarly, PTs often focus more on strengthening activities for patients with AIS C, as preparation for functional activities that may not be appropriate for their counterparts with similar motor level but complete injuries.
Given the amount of PT provided in group settings, it would be valuable to compare the functional effectiveness of group to individual therapy. Group therapy requires fewer therapists and, therefore, consumes fewer resources. The question is whether improvements in strength, ROM, and function achieved in group sessions are comparable to improvements achieved with individual treatments.
Limitations
Rehabilitation centers were selected to participate based on their willingness, geographic diversity, and expertise in treatment of patients with SCI. These facilities offer variation in setting, care delivery patterns, and patient clinical and demographic characteristics; however, they are not a probability sample of the rehabilitation facilities that provide care for patients with SCI in the United States and time reported on specific activities may not be generalizable to all rehabilitation centers. It is also important to note that data reported in this investigation were derived from supplemental documentation that was completed by clinicians in addition to their required clinical documentation. While a variety of efforts were made to maximize completeness of documentation, including cross-checking with clinical documentation of therapy delivered and communications with clinical staff, it is expected that some treatment activities that occurred are not represented in the research data set.
Conclusion
First-year data collection yielded both expected and unexpected trends in SCI rehabilitation that has provided insight into the type of interventions currently being delivered during inpatient rehabilitation for patients with SCI. The three most common individual therapy activities for patients with high tetraplegia were ROM/stretching, strengthening, and transfers; for patients with low tetraplegia, more time was spent on transfers than strengthening. For patients with paraplegia, the most common individual PT activities were transfers, ROM/stretching, and strengthening. The most prominent activities differed for patients with AIS D: gait training, strengthening, and balance exercises. Strengthening was the most common group therapy activity for patients in each of the injury categories. Significant variation in time spent on these activities was seen within and among injury groups. Further investigation remains underway and treatment processes related to patient outcomes will be examined.
Acknowledgements
The contents of this paper were developed under grants from the National Institute on Disability and Rehabilitation Research, Office of Rehabilitative Services, US Department of Education, to Craig Hospital (grant # H133A060103 and # H133N060005), the National Rehabilitation Hospital (grant # H133N060028), Rehabilitation Institute of Chicago (grant # H133N060014), Mount Sinai School of Medicine (grant # H133N060027), Shepherd Center (grant # H133N060009), and Carolinas Rehabilitation. The opinions contained in this publication are those of the grantees and do not necessarily reflect those of the US Department of Education.
References
- 1.Ustun T, Chatterji S, Buckenbach J, Kostanjsek N, Schneider M. The international classification of functioning, disability, and health: a new tool for understanding disability and health. Disabil Rehabil 2003;25:565–71 [DOI] [PubMed] [Google Scholar]
- 2.van der Putten J, Stevenson V, Playford E, Thompson A. Factors affecting functional outcome in patients with nontraumatic spinal cord lesions after inpatient rehabilitation. Neurorehabil Neural Repair 2001;15(2):99–104 [DOI] [PubMed] [Google Scholar]
- 3.Pagliacci MC, Celani MG, Zampolini M, Spizzichino L, Franceschini M, Baratta S, et al. An Italian survey of traumatic spinal cord injury. The Gruppo Italiano studio epidemiologico Mielolesioni study. Arch Phys Med Rehabil 2003;84(9):1266–75 [DOI] [PubMed] [Google Scholar]
- 4.Sumida M, Fujimoto M, Tokuhiro A, Tominaga T, Magara A, Uchida R. Early rehabilitation effect for traumatic spinal cord injury. Arch Phys Med Rehabil 2001;82(3):391–5 [DOI] [PubMed] [Google Scholar]
- 5.Scivoletto G, Morganti B, Molinari M. Early vs. delayed inpatient spinal cord injury rehabilitation: an Italian study. Arch Phys Med Rehabil 2005;86(3):512–6 [DOI] [PubMed] [Google Scholar]
- 6.Scivoletto G, Morganti B, Molinari M. Neurologic recovery of spinal cord injury patients in Italy. Arch Phys Med Rehabil 2004;85(3):485–9 [DOI] [PubMed] [Google Scholar]
- 7.Eastwood EA, Hagglund K, Ragnarsson K, Gordon W, Marino R. Medical rehabilitation length of stay and outcomes for persons with traumatic spinal cord injury–1990–1997. Arch Phys Med Rehabil 1999;80(11):1457–63 [DOI] [PubMed] [Google Scholar]
- 8.van Langeveld S, Post M, van Asbeck F, Postma K, ten Dam D, Pons K. Development of a classification of physical therapy, occupational therapy and sports therapy interventions to document mobility and self-care in spinal cord injury rehabilitation. J Neurol Phys Ther 2008;32(1):2–7 [DOI] [PubMed] [Google Scholar]
- 9.van Langeveld S, Post M, van Asbeck F, Postma K, ten Dam D, Pons K. Feasibility of a classification system for physical therapy, occupational therapy and sports therapy interventions for mobility and self-care in spinal cord injury rehabilitation. Arch Phys Med Rehabil 2008;89(8):1454–9 [DOI] [PubMed] [Google Scholar]
- 10.Natale A, Taylor S, LaBarbera J, Mumma S, Bensimon L, McDowell S, et al. SCIRehab: the physical therapy taxonomy. J Spinal Cord Med 2009;32(3):270–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gassaway J, Whiteneck G, Dijkers M. SCIRehab: clinical taxonomy development and application in spinal cord injury rehabilitation research. J Spinal Cord Med 2009;32(3):260–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Whiteneck G, Dijkers M, Gassaway J, Jha A. SCIRehab: new approach to study the content and outcomes of spinal cord injury rehabilitation. J Spinal Cord Med 2009;32(3):251–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnson K, Bailey J, Rundquist J, Dimond P, McDonald C, Reyes I, et al. SCIRehab: the supplemental nursing taxonomy. J Spinal Cord Med 2009;32(3):328–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ozelie R, Sipple C, Foy T, Cantoni K, Kellogg K, Lookingbill J, et al. SCIRehab: the occupational therapy taxonomy. J Spinal Cord Med 2009;32(3):283–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilson C, Huston T, Koval J, Gordon S, Schwebel A, Gassaway J. SCIRehab: the psychology taxonomy. J Spinal Cord Med 2009;32(3):318–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gordan W, Dale B, Brougham R, Spivack-David D, Georgeadis A, Adornato V, et al. SCIRehab: the speech language pathology taxonomy. J Spinal Cord Med 2009;32(3):306–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cahow C, Skolnick S, Joyce J, Jug J, Dragon C, Gassaway J. SCIRehab: the therapeutic recreation taxonomy. J Spinal Cord Med 2009;32(3):297–305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abeyta N, Freeman E, Primack D, Harmon A, Dragon C, Hammond F, et al. SCIRehab: the social work/case management taxonomy. J Spinal Cord Med 2009;32(3):335–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Whiteneck G, Gassaway J, Dijkers M, Charlifue S, Backus D, Chen D, et al. SCIRehab: inpatient treatment time across disciplines in spinal cord injury rehabilitation. J Spinal Cord Med 2011;34(2):135–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Horn S, Gassaway J. Practice-based evidence study design for comparative effectiveness research. Med Care 2007;45(10 October, Suppl 2):S50–7 [DOI] [PubMed] [Google Scholar]
- 21.DeJong G, Hsieh C, Gassaway J, Horn S, Smout R, Putman K, et al. Characterizing rehabilitation services for patients with knee and hip replacement in skilled nursing and inpatient rehabilitation facilities. Arch Phys Med Rehabil 2009;90(8):1284–96 [DOI] [PubMed] [Google Scholar]
- 22.Gassaway J, Horn S, DeJong G, Smout R, Clark C, James R. Applying the clinical practice improvement approach to stroke rehabilitation: methods used and baseline results. Arch Phys Med Rehabil 2005;86(12 Suppl 2):S16–33 [DOI] [PubMed] [Google Scholar]
- 23.Horn S, DeJong G, Ryser D, Veazie P, Teraoka J. Another look at observational studies in rehabilitation research: going beyond the holy grail of the randomized controlled trial. Arch Phys Med Rehabil 2005;86(12 Suppl 2):S8–15 [DOI] [PubMed] [Google Scholar]
- 24.Marino R. editor. Reference manual for the international standards for neurological classification of SCI. Chicago, IL: American Spinal Injury Association; 2003 [Google Scholar]
- 25.Horn S, Sharkey S, Rimmasch H. Clinical practice improvement: a methodology to improve quality and decrease cost in health care. Oncol Issues 1997;12(1):16–20 [Google Scholar]
- 26.Horn S, Sharkey P, Buckle J, Backofen J, Averill R, Horn R. The relationship between severity of illness and hospital length of stay and mortality. Med Care 1991;29(4):305–17 [DOI] [PubMed] [Google Scholar]
- 27.Ryser D, Egger M, Horn S, Handrahan D, Ghandi P, Bigler E. Measuring medical complexity during inpatient rehabilitation following traumatic brain injury. Arch Phys Med Rehabil 2005;86:1108–17 [DOI] [PubMed] [Google Scholar]
- 28.Averill R, McGuire T, Manning B, Fowler D, Horn S, Dickson P, et al. A study of the relationship between severity of illness and hospital cost in New Jersey hospitals. Health Serv Res 1992;27(5):587–617 [PMC free article] [PubMed] [Google Scholar]
- 29.Clemmer T, Spuhler V, Oniki T, Horn S. Results of a collaborative quality improvement program on outcomes and costs in a tertiary critical care unit. Crit Care Med 1999;27(9):1768–74 [DOI] [PubMed] [Google Scholar]
- 30.Fiedler R, Granger C. Functional independence measure: a measurement of disability and medical rehabilitation. In: Chino N, Melvin J. (eds.) Functional evaluation of stroke patients. Tokyo: Springer-Verlag; 1996. pp. 75–92 [Google Scholar]
- 31.Fiedler R, Granger C, Russell C. UDS(MR)SM: follow-up data on patients discharged in 1994–1996. Uniform data system for medical rehabilitation. Am J Phys Med Rehabil 2000;79(2):184–92 [DOI] [PubMed] [Google Scholar]
- 32.Stevens J. Partial and semipartial correlations. 2003. [accessed 2010 Feb 10]; Available from: www.uoregon.edu/~stevensj/MRA/partial.pdf
- 33.Stevens J. Intermediate statistics: a modern approach. 2nd ed. Mahwah, NJ: Lawrence Erlbaum Associates, Inc.; 1999 [Google Scholar]
- 34.Forrest G, Sisto S, Barbeau H, Kirshblum S, Wilen J, Bond Q, et al. Neuromotor and musculoskeletal responses to locomotor training for an individual with chronic motor complete AIS-B spinal cord injury. J Spinal Cord Med 2008;31(5):509–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Winchester P, McColl R, Querry R, McColl R, Foreman N, Mosby J, et al. Changes in supraspinal activation patterns following robotic locomotor therapy in motor-incomplete spinal cord injury. Neurorehabil Neural Repair 2005;19(4):313–24 [DOI] [PubMed] [Google Scholar]
- 36.Gelsomino K, Kirkpatrick L, Hess R, Gahimer J. A descriptive analysis of physical therapy group intervention in five midwestern inpatient rehabilitation facilities. J Phys Ther Educ 2000;14:12–20 [Google Scholar]
- 37.Gauthier L, Dalziel S, Gauthier S. The benefits of group occupational therapy for patients with Parkinson's disease. Am J Occup Ther 1987;41(6):360–5 [DOI] [PubMed] [Google Scholar]
- 38.Foy T, Perritt G, Thimmaiah D, Heisler L, Offutt J, Cantoni K, et al. SCIRehab: occupational therapy treatment time during inpatient spinal cord injury rehabilitation. J Spinal Cord Med 2011;34(2):164–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Field-Fote E, Lindley S, Sherman A. Locomotor training approaches for individuals with spinal cord injury: a preliminary report of walking-related outcomes. J Neurol Phys Ther 2005;29(3):127–37 [DOI] [PubMed] [Google Scholar]
- 40.Dobkin B, Apple D, Barbeau H, Basso M, Behrman A, Deforge D, et al. Weight-supported treadmill vs. over-ground training for walking after acute incomplete SCI. Neurology 2006;66(4):484–93 [DOI] [PMC free article] [PubMed] [Google Scholar]