Abstract
Background/objective
Length of stay (LOS) for rehabilitation treatment after spinal cord injury (SCI) has been documented extensively. However, there is almost no published research on the nature, extent, or intensity of the various treatments patients receive during their stay. This study aims at providing such information on a large sample of patients treated by specialty rehabilitation inpatient programs.
Methods
Six hundred patients with traumatic SCI admitted to six rehabilitation centers were enrolled. Time spent on various therapeutic activities was documented by each rehabilitation clinician after each patient encounter. Patients were grouped by neurologic level and completeness of injury. Total time spent by each rehabilitation discipline over a patient's stay and total minutes of treatment per week were calculated. Ordinary least squares stepwise regression models were used to identify patient and injury characteristics associated with time spent in rehabilitation treatment overall and within each discipline.
Results
Average LOS was 55 days (standard deviation 37), during which 180 (106) hours of treatment were received, or 24 (5) hours per week. Extensive variation was found in the amount of treatment received, between and within neurologic groups. Total hours of treatment provided throughout a patient's stay were primarily determined by LOS, which in turn was primarily predicted by medical acuity. Variation in minutes per week of treatment delivered by individual disciplines was predicted poorly by patient and injury characteristics.
Conclusions
Variations between and within SCI rehabilitation patient groups in LOS, minutes of treatment per week overall, and for each rehabilitation discipline are large. Variation in treatment intensity was not well explained by patient and injury characteristics. In accordance with practice-based evidence methodology, the next step in the SCIRehab study will be to determine which treatment interventions are related with positive outcomes (at 1 year post injury), after controlling for patient and injury differences.
Keywords: Spinal cord injuries, Rehabilitation, Health services research, Occupational therapy, Physical therapy, Rehabilitation nursing, Psychology, Speech–language pathology, Social work, Case management, Recreation therapy, Practice-based evidence, Paraplegia, Tetraplegia
Introduction
The spinal cord injury (SCI) rehabilitation literature is replete with reports and discussions of length of stay (LOS). In one of the first evaluations of SCI rehabilitation published in the United States, Berns et al.1 described 31 individuals sent for rehabilitation in 1950–1953. The average rehabilitation stay for the group was 138 days (range 37–365 days), despite the fact that only 2 of the 31 patients had tetraplegia (both with C7 neurological level), some already had received (partial) rehabilitative interventions, almost all had been injured for more than a year (some for more than 10 years) and had been living at home, and 7 were employed at the time of admission. In the United States, LOS for rehabilitation treatment after SCI has decreased dramatically since the days of the Berns et al. study. Data from the SCI model systems allow consistent comparisons for the 35-year period from 1973 to 2008.2 The decrease in rehabilitation duration is found for all SCI impairment categories. For patients with incomplete paraplegia, median LOS decreased from 68 to 29 days, and it was reduced from 84 to 42 days for patients with complete paraplegia. Median LOS was reduced by two-thirds for those with incomplete tetraplegia (from 104 to 34 days), and almost as much for patients with complete tetraplegia (from 142 to 59 days). The pressures of managed care, as much as improvements in medical and rehabilitative expertise, seem to have driven the rehabilitation LOS declines.3
In other countries, LOS is longer than in the United States. In Japan, for a group of patients with paraplegia injured in 2000–2004, mean rehabilitation LOS was 116 days.4 In four European countries, rehabilitation LOS in recent years, across all neurological categories of injury, ranged from 47 days in Russia5 to 240 days in the Netherlands,6 with 177 days in Denmark5 and 122 days in Italy.7
In contrast to the many available citations on overall LOS for SCI rehabilitation admissions, published information on the type and extent of services delivered during rehabilitation is scant. Most research reports on rehabilitation focus on outcomes (functional status gain, discharge destination, etc.)8–11 and differences in outcomes between patient subgroups (by level and completeness of injury, age, ethnicity, etc.)8,9,11–13 rather than on resource use. The resources needed to bring about optimal functioning given neurological limitations are generally not discussed in this literature; at best, LOS is used as an indicator of global resource use. The majority of reports on SCI rehabilitation do not even report what therapies were used by patients.3,5,7,14–16 For the United States, only one study has been published focusing on the relationship between therapeutic intensity and functional outcomes that provides insight into resource use. Heinemann et al.17 reported that in 1990–1991 in eight rehabilitation centers, patients with SCI received an average of 4.9 hours of nursing care (including indirect care) per day during their first week after admission, and 3.3 hours per day during their last week. During both periods, teaching (including teaching of activities of daily living) took up about half of the nursing time. An earlier paper on the same sample reported that these patients received an average of 77 hours of occupational therapy (OT), 73 hours of physical therapy (PT), 12 hours of psychology (PSY), 2 hours of social work/case management (SW/CM), 1 hour of speech therapy (ST), 3 hours of vocational rehabilitation, and 4 hours of therapeutic recreation (TR) during their entire stay (mean duration 65 days). The time spent with TR is likely an underestimate because only billed hours were included, and not all hours of TR were billed. The total number of therapy hours per stay (excluding nursing teaching and other care) was 172, or 2.6 hours per day.18
There seems to be an internal contradiction in the totality of the literature on SCI rehabilitation outcomes: while the assumption is that the package of treatments patients receive during rehabilitation improves their functioning level and as a result quality of life, the research has focused exclusively on individual patient characteristics that may explain differences in these outcomes (age, co-morbidities, level and completeness of injury, etiology of injury, etc.). There is almost no research on the nature, extent, or intensity of the various treatments patients receive, or on the impact of differences in treatments received, by those in SCI specialty units or in other, generic rehabilitation programs, on outcomes.
The SCIRehab project is a multicenter collaborative study that is describing and quantifying the interventions provided during rehabilitation, with the goal of relating those interventions and services to outcomes. An early contribution of the SCIRehab project to the field of SCI rehabilitation research and practice was the development of a comprehensive, multidisciplinary taxonomy for describing the details of the SCI rehabilitation process, and of a technology for efficiently documenting the elements of those treatment procedures by all clinicians in all disciplines after each treatment session or patient encounter. Each discipline's taxonomy and the documentation development process were described in a series of papers (Journal of Spinal Cord Medicine 2009;32(3):251–335), which can be referred to for documentation content and process details, as well as the extraordinary contribution of clinical expertise underlying the development of the taxonomy and other elements of the documentation; these will not be reiterated in this article.19–27
The purpose of this paper is to describe time spent on rehabilitation treatments for the patients enrolled during the first year of the SCIRehab project. The distribution of the time for each rehabilitation discipline, the variation in therapy time between patients, and predictors (patient and injury characteristics) of that variation are provided. The details of discipline-specific interventions are presented in the seven discipline articles that follow.28–34
Methods
This study uses practice-based evidence (PBE) research methodology19,20,35–39 that encourages the employment of a multidisciplinary project team to design data collection instruments to answer broad research questions posed at the outset of a study, and to contribute clinical expertise to study analyses. PBE study data focus on the nature of the care a patient receives; the research does not attempt to introduce new processes or alter the plan of care. The SCIRehab team, which includes representatives of all rehabilitation clinical disciplines and researchers from all centers participating in SCIRehab, incorporated four elements of practical clinical trials40 into the study's design: (1) identify clinically relevant interventions to measure, (2) enroll a diverse population of study participants, (3) include heterogeneous practice settings, and (4) collect data on a broad range of health outcomes.
SCIRehab facilities
The SCIRehab study is led by the Rocky Mountain Regional Spinal Injury System at Craig Hospital and involves collaboration with five other specialized SCI rehabilitation programs (Shepherd Center, Atlanta GA; Rehabilitation Institute of Chicago, Chicago, IL; Carolinas Rehabilitation, Charlotte, NC; the Mount Sinai Medical Center, New York, NY; and National Rehabilitation Hospital, Washington, DC) and with the Institute for Clinical Outcomes Research, Salt Lake City, UT. Clinical facilities were selected based on their willingness to participate, geographic diversity, and expertise in treatment of patients with SCI. They are not a probability sample of the rehabilitation facilities that provide care for patients with SCI in the United States, but do provide variation in setting, care delivery patterns, and various patient clinical and demographic characteristics, all of which may affect outcomes. Each SCIRehab facility obtained Institutional Review Board (IRB) approval for this observational study. The number of participants enrolled in the SCIRehab project's first year ranged from 35 to 260 per facility, for a total of 600.
Enrollment criteria
The SCIRehab facilities enrolled all patients who were 12 years of age or older, gave (or whose parent/guardian gave) informed consent, and were admitted to the facility's SCI unit for initial rehabilitation following traumatic SCI. Duration of the acute-hospital inpatient admission preceding rehabilitation was not an enrollment criterion. Patients requiring transfer to acute care units or facilities during their rehabilitation program were retained in the study, no matter how long they spent in acute care before returning to the rehabilitation unit, but their acute care days were not counted as part of the rehabilitation stay. To restrict the study to initial rehabilitation cases, a small number of patients were excluded who spent more than 2 weeks in another rehabilitation center prior to admission to the SCIRehab facility. To ensure complete rehabilitation data, patients who spent more than a week of their rehabilitation stay on a non-SCI rehabilitation unit in the SCIRehab facility (staff of the non-SCI units were not trained in the data collection methods) also were excluded. There were no other exclusion criteria.
Patient and injury data
Most patient and injury data were abstracted from patient medical records using a database specifically designed for the study. In addition, all six sites collected the National Institute on Disability and Rehabilitation Research SCI Model Systems' standardized information on injury through community discharge (Form I) and follow-up status at 1 year post injury (Form II), and submitted these data to the National SCI Database maintained by the National Spinal Cord Injury Statistical Center in Birmingham, Alabama; data were obtained from this database and merged into the SCIRehab project database.
The International Standards of Neurological Classification of SCI (ISNCSCI) and its American Spinal Injury Association Impairment Scale (AIS)41 were used to describe the neurologic level and completeness of injury; the Functional Independence Measure (FIM®) served to describe a patient's functional independence in motor and cognitive tasks at admission and discharge, and monitor functional gains;42,43 and the Comprehensive Severity Index (CSI®) was used to provide an overall summary measure of how ill (extent of deviation from ‘normal’) a patient was over time during the stay in the center.37 The CSI is age and disease specific, is scored independent of treatments received, and provides an objective, consistent method of defining patient severity of illness based on over 2100 signs, symptoms, and physical findings related to a patient's disease(s), not just on the basis of diagnostic information (ICD-9-CM coding) alone. The CSI uses weighting algorithms based on the severity level of signs and symptoms associated with each ICD-9 diagnostic code to calculate severity scores separately for each of a patient's diseases at admission (first 3 days), discharge (last 3 days), and throughout the patient's stay using data from the entire rehabilitation stay. The full-stay severity score was used in this study. The CSI has been validated extensively in inpatient (adult and pediatric), ambulatory, rehabilitation, and long-term care settings.37,44–50 The SCIRehab project's physician team reviewed and approved CSI criteria and algorithms for common co-morbidities and complications of patients with traumatic SCI, including a four-level categorization of individual indicator variables (level 1: normal to mild; level 2: moderate; level 3: severe; and level 4: catastrophic or life threatening), which is used in calculating the CSI.
The following categories for body mass index (BMI) were used: morbidly obese (>40 kg/m2 in height), obese (30–40 kg/m2), and other (<30 kg/m2), which includes the standard underweight, normal, and overweight categories. These categories were selected to focus on obesity and morbid obesity as they may have a substantial impact on rehabilitation interventions.
Clinician characteristics
Clinicians who contributed treatment data to the SCIRehab project completed a clinician profile to provide information about their education and experience in rehabilitation and, specifically, the number of years they had worked in SCI rehabilitation. The average clinician experience of those treating a particular patient was calculated by weighting the experience of each clinician in a discipline by the number of hours of treatment each clinician provided.
Process (treatment) data
PBE study methodology calls for data that describe the care a patient receives in detail. Some of these data can be obtained from medical chart review by trained abstracters, but additional data requirements for the SCIRehab project necessitated the completion of discipline-specific documentation by each clinician as he/she delivered care – the point-of-care (POC) documentation. The SCIRehab project's use of electronic data capture (a modular custom application (PointSync Pro version 2.0, MobileDataforce, Boise, ID, USA) for use on a handheld personal digital assistant (PDA; Hewlett Packard PDA hx2490b, Palo Alto, CA) to record details about each treatment session provided by each clinical discipline has been described previously.19,20 Each discipline developed documentation strategies to capture details of the care provided to patients. At the core of the documentation was a taxonomy of the discipline's most important treatment activities and interventions; these taxonomies have been described in detail in previous articles.20–26
After identifying the type of a therapy session (group or individual), PT, OT, TR, and ST clinicians captured the following session details: date/time of the session, identity of the center, patient and therapist, intervention activities performed in the session complete with activity-specific details, and session-level variables, such as co-treatment with another therapist or discipline, and degree of patient and family participation. Also recorded were factors that may limit session activities (such as patient fatigue) and a few measures of patient achievement/improvement.21,23,25,26 PSY and SW/CM clinicians recorded interactions with or on behalf of patients that typically occur at multiple times over the course of a day, rather than in scheduled sessions. For each day, these clinicians indicated intervention activities or topic/content areas addressed, with whom, and for how long.24,27 Nursing representatives completed supplementary documentation to record the content and intensity of bedside education and of care management activities, which are not included in significant detail in regular nursing documentation.22
Each discipline chose to use time (number of minutes) to quantify the dosage of their interventions. This approach is similar to dosage measurement in previous PBE studies,37,39 and is the most practical and efficient way of quantifying the amount of a specific treatment a patient receives. Each clinician documented the number of minutes spent on every separate activity, rounded to the nearest multiple of 5 minutes; interventions that consumed less than 5 minutes were not included in the documentation. The activity minutes combined equal the approximate duration of time spent each day of rehabilitation by each clinical discipline.
POC documentation training and reliability of data recording
The project team provided clinician training at each of the SCIRehab centers; training sessions were separate for the six disciplines participating in the project. Each clinician was provided with a PDA and attended a 1.5-hour training session during which PDA functionality and documentation content were described, demonstrated, and practiced. Training sessions were supplemented by discipline-specific manuals that provided step-by-step instructions for entering data, definitions for terms used, and the interventions taxonomy. Clinicians practiced using the PDAs for a day and returned for a 1-hour session to have key training issues reinforced and questions answered. Clinicians who were hired at a later time or rotated to the units were trained by their discipline's lead clinician and the local study coordinator.
Discipline-specific written case scenarios were used to test the reliability of the data produced by clinicians; this was done quarterly during the data collection period.19 Lead clinicians in each discipline developed a written description of that discipline's interactions with a hypothetical patient during a session, shift or day, and assigned the codes. Each clinician read the case scenario and selected codes on their PDAs to ‘document’ the patient interaction. Entries were compared to the leaders' consensus answers; the degree of correspondence provided an estimate of the clinician's knowledge and application of the system. The overall agreement score for all reliability sessions for all disciplines was 89%. Scores were calculated for five major POC documentation areas: (1) general session information, including time/date, family involvement, and amount of care a patient directs (96% agreement); (2) activities/interventions (92%); (3) sub-activity/intervention details (86%); (4) patient factors (e.g. illness) affecting the session (93%); and (5) a participation scale, asking for the clinician's rating of the patient's active involvement (80%).19 Reports were provided to clinicians that included aggregate scores for all clinicians of a particular discipline in a SCIRehab center, as well as clinician-specific accounts that depicted correct and incorrect entries made by each clinician; these reports helped to guide ongoing education in POC documentation.
POC data completeness
The SCIRehab project local coordinators compared POC entries for each discipline with scheduling and/or billing records to ensure that all billed sessions were included in the POC system. If a session had been scheduled or billed but not documented, the coordinator reported this to the therapist and the lead clinician involved so that it could be added. While memory and notes might be insufficient to complete all data fields, the main elements generally could be supplied.
Data analysis
The analyses reported here focus on therapy intensity, overall and by patient injury group defined using the ISNCSCI. Patients with AIS grade D are grouped together regardless of injury level. Patients with AIS classification A, B, and C are combined and split by motor level to create the remaining three categories: patients with high tetraplegia (C1–C4), low tetraplegia (C5–C8), and paraplegia (T1 and below). For categorical variables, contingency tables are used to display differences in frequencies, and chi-square tests to examine differences across these four neurological injury groups. For continuous measures ANOVA is used to assess the statistical significance of differences in means across injury groups. A two-sided P value <0.05 is considered statistically significant.
Total time spent by each rehabilitation discipline over a patient's entire stay is used as the first measure of therapy intensity. However, since total time has an approximately linear relationship with the opportunity to provide services as determined primarily by LOS, total minutes of treatment per week are calculated as another measure of intervention intensity. Box plots are used to depict variation in LOS and rehabilitation intervention time.
Ordinary least squares stepwise regression models are used to identify patient and injury characteristics, as either continuous or dummy variables, associated with time spent in rehabilitation treatment, overall and for each discipline. The strength of a regression model is determined by the R2 value, which indicates the amount of variation explained by the significant independent variables. Parameter estimates indicate the direction and strength of the association between each independent variable (predictor) and the dependent variable. Rather than reporting the partial R2 at each step of the stepwise regression (indicating the added variance accounted for by each new variable), type II semi-partial R2 values are reported, indicating the proportion of the variance in the dependent variable that is uniquely associated with the predictor variable after controlling for all other variables in the model. The sums of the squared type II semi-partial coefficients do not add to the total R2, as common variance among the predictors also contributes to the total R2. Use of semi-partial correlation coefficients is especially useful when the purpose of the research is predictive.51,52 All independent variables were checked for colinearity, and if any pair was highly correlated (r > 0.75), only one of the pair was allowed to enter the models.
The discipline-specific articles that follow in this series describe the intensity of specific activities/interventions provided by each treating discipline;28–34 this article only addresses time for all therapeutic activities combined.
Results
Patient characteristics
From the fall of 2007 through the fall of 2008, 600 patients with traumatic SCI were enrolled at the 6 SCIRehab rehabilitation centers; these are the subjects included in the first-year data set analyzed here. The percent of eligible patients who consented to be enrolled was 90% overall, and varied from 71 to 97% per center. Patient and injury characteristics are presented in Table 1 for the sample as a whole and for each of the four injury groups (as defined by lesion level and AIS).
Table 1.
Patient and injury characteristics, by injury group
| Total SCIRehab Sample n = 600 | C1–C4 AIS A, B, C n = 132 | C5–C8 AIS A, B, C n = 151 | Para AIS A, B, C n = 223 | AIS D n = 94 | |
|---|---|---|---|---|---|
| Length of rehabilitation stay – days, mean (SD)* | 54.6 (37.1) | 74.1 (43.2) | 64.9 (37.7) | 44.9 (28.8) | 33.6 (24.1) |
| Age at injury – years, mean (SD)* | 37.2 (16.6) | 41.9 (17.0) | 33.7 (15.6) | 33.4 (14.2) | 45.3 (18.5) |
| Gender, % male | 80.5 | 80.3 | 80.8 | 81.6 | 77.7 |
| Race/ethnicity % | |||||
| White | 64.8 | 68.2 | 72.9 | 59.2 | 60.6 |
| Black | 21.5 | 19.7 | 16.6 | 24.7 | 24.5 |
| Hispanic | 8.0 | 7.6 | 6.0 | 9.9 | 7.5 |
| Other | 5.7 | 4.6 | 4.6 | 6.3 | 7.5 |
| Primary language % | |||||
| English primary language | 95.0 | 96.2 | 97.4 | 93.7 | 92.6 |
| Understands sufficient English | 2.5 | 1.5 | 0.7 | 3.1 | 5.3 |
| No English | 2.5 | 2.3 | 2.0 | 3.1 | 2.1 |
| Payer %* | |||||
| Medicare | 6.8 | 9.1 | 3.3 | 4.0 | 16.0 |
| Medicaid | 18.0 | 13.6 | 21.2 | 22.0 | 9.6 |
| Private insurance/payer | 65.8 | 67.4 | 67.6 | 63.2 | 67.0 |
| Worker's compensation | 9.3 | 9.9 | 8.0 | 10.8 | 7.5 |
| Marital status at injury, % married | 38.0 | 43.9 | 31.8 | 38.6 | 38.3 |
| Education %* | |||||
| Less than high school diploma | 20.2 | 15.2 | 25.8 | 20.6 | 17.0 |
| High school diploma or General Equivalency Diploma (GED) | 46.5 | 56.1 | 42.4 | 48.0 | 36.2 |
| More than high school diploma | 27.0 | 25.0 | 26.5 | 25.6 | 34.0 |
| Other/unknown | 6.3 | 3.8 | 5.3 | 5.8 | 12.8 |
| Employment status before injury %* | |||||
| Working | 65.0 | 69.7 | 60.9 | 67.7 | 58.5 |
| Student | 16.2 | 8.3 | 23.2 | 16.1 | 16.0 |
| Other | 18.8 | 22.0 | 15.9 | 16.1 | 25.5 |
| Injury etiology %* | |||||
| Vehicular | 49.3 | 47.7 | 45.0 | 52.5 | 51.1 |
| Violence | 11.0 | 7.6 | 9.3 | 16.1 | 6.4 |
| Sports | 11.7 | 13.6 | 23.2 | 4.0 | 8.5 |
| Fall or falling object | 23.2 | 28.0 | 21.2 | 19.7 | 27.7 |
| Other | 4.8 | 3.0 | 1.3 | 7.6 | 6.4 |
| BMI at admission %* | |||||
| Less than 30 | 81.8 | 81.1 | 86.8 | 82.1 | 74.5 |
| 30–40 | 15.5 | 16.7 | 11.9 | 13.5 | 24.5 |
| More than 40 | 2.7 | 2.3 | 1.3 | 4.5 | 1.1 |
| Admission total FIM, mean (SD)* | 53.0 (14.8) | 40.7 (6.8) | 45.8 (7.8) | 62.2 (12.8) | 60.0 (17.3) |
| Admission motor FIM, mean (SD)* | 24.1 (12.1) | 14.1 (2.3) | 17.6 (5.5) | 32.2 (10.4) | 29.2 (15.1) |
| Admission cognitive FIM, mean (SD)* | 28.9 (5.6) | 26.6 (6.4) | 28.3 (5.2) | 30.0 (5.1) | 30.8 (5.2) |
| Admission CSI, mean (SD)* | 21.2 (19.4) | 29.2 (25.4) | 20.8 (18.5) | 20.0 (16.8) | 13.3 (11.7) |
| Maximum CSI, mean (SD)* | 40.2 (33.2) | 58.3 (42.8) | 41.8 (29.5) | 36.1 (28.0) | 22.0 (19.3) |
| Days from injury to rehabilitation, mean (SD)* | 31.7 (28.1) | 42.1 (30.5) | 33.0 (28.7) | 31.5 (28.1) | 15.5 (12.4) |
*Statistically significant differences among injury groups.
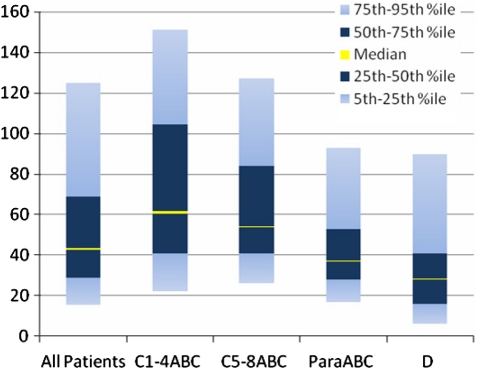
The mean rehabilitation LOS (excluding interruptions requiring transfer to an acute unit) was 55 days (range 2–259, standard deviation (SD) 37, median 43, 25th percentile 29, 75th percentile 69). Significant differences were seen among injury groups, and the LOS within each group varied widely as shown in the distributions in Fig. 1. Patients in injury group C1–C4: ABC had the longest LOS (mean 74 days), followed by patients in the C5–C8: ABC group (65 days), and patients in the Para: ABC group (45 days). The lowest mean LOS was seen in the AIS D group (34 days).
Figure 1.
Length of rehabilitation stay (in days) by injury group.
Rehabilitation interventions
Table 2 presents the average years of clinician experience in SCI rehabilitation and the mean time spent on rehabilitation interventions overall and by each rehabilitation discipline separately. Time spent by all disciplines (combined and separately) is reported as mean total hours during the rehabilitation stay and, to control somewhat for varying lengths of stay, as mean minutes per week of the rehabilitation stay. In addition, each discipline's total time is reported as a percentage of the patient's total rehabilitation therapy time. SCIRehab patients received a mean total of 180 hours (range 7–641 hours, SD 106, median 152, 25th percentile 104, 75th percentile 232) of therapy from the 7 disciplines completing POC documentation (PT, OT, TR, ST, nursing, PSY, and SW/CM). Statistically significant differences were seen among injury groups. The majority of hours spent on rehabilitation interventions were provided by PT (32%) and OT (28%); bedside education and care management activities provided by nursing accounted for 17%, TR activities comprised 9%, and PSY and SW/CM comprised 6% each. ST, whose interventions primarily focus on communication and swallowing issues for patients with a ventilator or tracheostomy and/or patients with cognitive-communication disorders, provided the remaining 2% of treatment time.
Table 2.
Mean (SD) Clinician experience and treatment time by various disciplines, by injury group*
| Total SCIRehab Sample n = 600 | C1–C4 AIS A, B, C n = 132 | C5–C8 AIS A, B, C n = 151 | Para AIS A, B, C n = 223 | AIS D n = 94 | |
|---|---|---|---|---|---|
| All therapies combined | |||||
| # years SCI rehabilitation experience of clinicians† | 6.7 (3.4) | 7.6 (3.5) | 6.7 (2.8) | 6.7 (3.5) | 5.8 (3.6) |
| Total # hours† | 179.7 (106.0) | 232.5 (114.9) | 220.8 (105.2) | 148.6 (79.8) | 113.1 (84.6) |
| # minutes per week† | 1442 (293.5) | 1398 (302.6) | 1495 (311.4) | 1454 (286.3) | 1390 (252.0) |
| Physical therapy | |||||
| # years SCI rehabilitation experience of clinicians | 5.8 (4.8) | 6.4 (5.5) | 5.6 (4.3) | 5.9 (4.8) | 5.0 (4.4) |
| Total # hours† | 56.9 (36.0) | 67.0 (35.5) | 67.9 (37.2) | 50.6 (33.5) | 40.0 (30.6) |
| Percent of total hours, all disciplines† | 31.7 (7.9) | 28.8 (6.1) | 30.0 (6.0) | 33.0 (9.2) | 35.3 (7.8) |
| # minutes per week† | 455.6 (129.2) | 404.5 (118.6) | 446.7 (105.5) | 475.7 (141.1) | 494.0 (126.3) |
| Occupational therapy | |||||
| # years SCI rehabilitation experience of clinicians† | 6.1 (5.3) | 7.2 (5.9) | 6.7 (5.4) | 5.5 (5.0) | 5.2 (4.7) |
| Total # hours† | 51.9 (35.5) | 69.0 (37.9) | 69.0 (37.3) | 37.7 (24.0) | 34.3 (28.2) |
| Percent of total hours, all disciplines† | 28.4 (7.6) | 29.6 (6.8) | 30.6 (6.6) | 25.9 (8.3) | 29.3 (7.0) |
| # minutes per week† | 406.7 (113.4) | 410.5 (103.3) | 452.2 (99.2) | 372.0 (119.6) | 410.6 (107.0) |
| Speech language pathology | |||||
| # years SCI rehabilitation experience of clinicians | 6.5 (3.7) | 6.9 (5.5) | 6.4 (4.0) | 6.5 (2.3) | 6.0 (2.8) |
| Total # hours† | 3.9 (10.2) | 8.0 (16.2) | 2.9 (6.4) | 2.6 (7.8) | 2.9 (7.7) |
| Percent of total hours, all disciplines† | 1.7 (3.6) | 2.8 (4.3) | 1.3 (3.0) | 1.2 (2.9) | 2.1 (4.3) |
| # minutes per week† | 24.1 (47.5) | 37.5 (56.2) | 18.2 (38.5) | 18.1 (41.2) | 29.1 (57.0) |
| Therapeutic recreation | |||||
| # years SCI rehabilitation experience of clinicians | 7.5 (8.6) | 8.9 (9.4) | 7.1 (8.3) | 7.0 (8.4) | 7.6 (8.2) |
| Total # hours† | 17.2 (16.3) | 18.7 (14.5) | 23.2 (20.6) | 16.1 (14.5) | 7.9 (9.1) |
| Percent of total hours, all disciplines† | 9.7 (7.7) | 8.5 (5.8) | 10.8 (8.2) | 10.9 (8.6) | 6.7 (5.9) |
| # minutes per week† | 152.1 (144.4) | 128.0 (99.1) | 177.5 (163.3) | 171.4 (163.0) | 99.5 (92.3) |
| Psychology | |||||
| # years SCI rehabilitation experience of clinicians† | 15.3 (6.5) | 16.6 (6.5) | 15.7 (6.2) | 15.2 (6.6) | 13.0 (6.5) |
| Total # hours† | 10.6 (10.5) | 15.6 (12.4) | 12.7 (13.0) | 8.3 (6.4) | 5.5 (6.6) |
| Percent of total hours, all disciplines† | 5.5 (3.3) | 6.3 (3.2) | 5.5 (3.5) | 5.5 (3.0) | 4.4 (3.6) |
| # minutes per week† | 77.7 (42.4) | 85.4 (41.6) | 79.8 (43.0) | 79.2 (41.3) | 59.8 (40.9) |
| Social work/case management | |||||
| # years SCI rehabilitation experience of clinicians† | 12.8 (8.1) | 13.7 (8.4) | 12.9 (7.5) | 13.2 (8.1) | 10.2 (8.3) |
| Total # hours† | 10.0 (11.6) | 16.1 (17.3) | 9.9 (9.4) | 8.1 (8.8) | 6.0 (6.0) |
| Percent of total hours, all disciplines† | 5.1 (4.0) | 6.0 (4.5) | 4.1 (2.8) | 5.1 (4.2) | 5.5 (4.1) |
| # minutes per week† | 72.8 (56.3) | 83.2 (64.6) | 61.6 (42.3) | 72.0 (58.5) | 77.8 (56.1) |
| Nursing bedside education/care management | |||||
| # years SCI rehabilitation experience of clinicians | 6.1 (2.9) | 6.2 (2.6) | 6.1 (2.7) | 6.2 (2.8) | 6.1 (3.7) |
| Total # hours† | 30.6 (20.7) | 40.0 (22.7) | 36.7 (20.3) | 26.3 (17.8) | 17.9 (14.7) |
| Percent of total hours, all disciplines | 17.9 (7.6) | 18.1 (7.0) | 17.5 (7.6) | 18.5 (8.0) | 16.7 (7.7) |
| # minutes per week | 264.3 (140.9) | 260.3 (131.3) | 267.9 (141.1) | 274.9 (152.0) | 239.2 (124.2) |
*Hours and minutes per week are averages over all 600 patients, not just based on those who received intervention by each discipline.
†Statistically significant differences in total hours or mean minutes per week among groups.
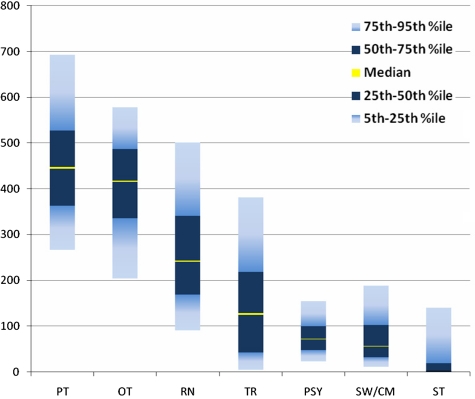
The 7 rehabilitation disciplines provided a mean total of 1442 minutes (24.0 hours) of therapy per week of rehabilitation (range 658–2842 hours, SD 294, median 1427, 25th percentile 1251, 75th percentile 1596). Fig. 2 displays the variation in the amount of time spent by each discipline.
Figure 2.
Total minutes of therapy per patient per week, by discipline.
Predictors of treatment dosage
The association of patient characteristics (age at the time of injury, gender, race/ethnicity, education level, marital status, BMI, occupational status, payer, and English language competency); injury characteristics (injury group, etiology, work relatedness, CSI severity of illness, admission FIM motor and cognitive scores, and ventilator use at rehabilitation admission), and clinician characteristics (years of experience in SCI rehabilitation) with rehabilitation treatment time and LOS are presented in Table 3. Table 4 presents similar information for the time spent by each rehabilitation discipline. Both tables only report variables that were significant predictors of at least one dependent variable, but notes at the bottom of each table specify the full details of all variables included in the analyses as potential predictors.
Table 3.
Patient and injury characteristics associated with treatment time in rehabilitation and LOS: multiple regression results*
| Total hours of therapy during rehabilitation |
Rehabilitation LOS |
Minutes of therapy per week during rehabilitation |
||||
|---|---|---|---|---|---|---|
| Total R2 | 0.89 |
0.56 |
0.17 |
|||
| Independent variable | Parameter estimate | Type II semi-partial R2 | Parameter estimate | Type II semi-partial R2 | Parameter estimate | Type II semi-partial R2 |
| Rehabilitation LOS | 2.57 | 0.47 | – | |||
| Days from injury to rehabilitation admission | −0.11 | <0.01 | ||||
| Age at injury | −0.40 | <0.01 | −2.33 | 0.01 | ||
| Race – other† | 17.50 | 0.01 | ||||
| Married | 7.93 | <0.01 | ||||
| Injury group | ||||||
| C5–C8: ABC | 12.91 | <0.01 | 5.98 | <0.01 | ||
| AIS D | −99.21 | 0.01 | ||||
| Traumatic etiology | ||||||
| Vehicular | −5.74 | 0.01 | ||||
| Violence | −13.59 | <0.01 | −131.07 | 0.02 | ||
| Medical/surgical complications | −146.84 | 0.01 | ||||
| BMI >40 | −18.15 | <0.01 | ||||
| English primary language | 11.56 | <0.01 | ||||
| Payer | ||||||
| Medicaid | −68.76 | 0.01 | ||||
| Workers' compensation | 13.71 | 0.01 | ||||
| Ventilator use at rehabilitation admission | −21.91 | <0.01 | 21.17 | 0.02 | −152.96 | 0.02 |
| Severity score (CSI) | 0.48 | 0.11 | −2.11 | 0.04 | ||
| Admission FIM motor score | −0.63 | <0.01 | −0.76 | 0.05 | ||
| Clinician experience‡ | 2.72 | 0.01 | 1.46 | 0.02 | 10.70 | 0.01 |
*Independent variables allowed into models: age at injury, male, married, race – white, race – black, race – Hispanic, race – other, admission FIM motor score, admission FIM cognitive score, severity of illness score (CSI), injury group: C1–C4 ABC, injury group: C5–C8 ABC, injury group: Para ABC, injury group: AIS D, clinician experience, traumatic etiology – vehicular, traumatic etiology – violence, traumatic etiology – falls, traumatic etiology – sports, traumatic etiology – medical/surgical complication, traumatic etiology – other, work-related injury, number of days from trauma to rehabilitation admission, BMI >40, BMI 30–40, BMI <30, language – English, language – no English, language – English sufficient for understanding, payer – Medicare, payer – worker compensation, payer – private, payer – Medicaid, employment status at the time of injury – employed, employment status at the time of injury – student, employment status at the time of injury – retired, employment status at the time of injury – unemployed, employment status at the time of injury – other, ventilator use at rehabilitation admission.
†Race ‘other’ subcategory includes Native American, Asian/Pacific Islander, and unknown.
‡Clinician experience is for all disciplines combined.
Table 4.
Patient and injury characteristics associated with minutes of therapy per week of rehabilitation, separately for each discipline*
| Total R2 | PT minutes per week during rehabilitation |
OT minutes per week during rehabilitation |
TR minutes per week during rehabilitation |
ST minutes per week during rehabilitation |
SW/CM minutes per week during rehabilitation |
PSY minutes per week during rehabilitation |
RN minutes per week during rehabilitation |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0.21 |
0.18 |
0.20 |
0.28 |
0.17 |
0.13 |
0.09 |
||||||||
| Independent variable | Parameter estimate | Type II semi-partial R2 | Parameter estimate | Type II semi-partial R2 | Parameter estimate | Type II semi-partial R2 | Parameter estimate | Type II semi-partial R2 | Parameter estimate | Type II semi-partial R2 | Parameter estimate | Type II semi-partial R2 | Parameter estimate | Type II semi-partial R2 |
| Days from injury to rehabilitation admission | −0.72 | 0.02 | −0.18 | 0.01 | ||||||||||
| Age at injury | −0.84 | 0.01 | ||||||||||||
| Male | −12.24 | 0.01 | ||||||||||||
| Race | ||||||||||||||
| White | 40.87 | 0.02 | 32.69 | 0.01 | ||||||||||
| Hispanic | 22.95 | 0.01 | ||||||||||||
| Injury group | ||||||||||||||
| C5–C8, ABC | 40.43 | 0.02 | −8.14 | 0.01 | −17.48 | 0.02 | ||||||||
| Para, ABC | 20.64 | 0.01 | ||||||||||||
| AIS D | −75.31 | 0.03 | 14.07 | 0.01 | −15.16 | 0.02 | −42.82 | 0.01 | ||||||
| Traumatic etiology | ||||||||||||||
| Vehicular | 8.87 | 0.01 | ||||||||||||
| Violence | −40.41 | 0.01 | ||||||||||||
| Sports | 19.74 | 0.01 | ||||||||||||
| Other | 172.10 | 0.01 | ||||||||||||
| BMI | ||||||||||||||
| >40 | −70.13 | 0.01 | −68.67 | 0.01 | ||||||||||
| <30 | −33.93 | 0.01 | 10.56 | 0.01 | ||||||||||
| English primary language | 19.43 | 0.01 | ||||||||||||
| Payer | ||||||||||||||
| Medicaid | −36.26 | 0.01 | ||||||||||||
| Medicare | 19.70 | 0.01 | ||||||||||||
| Employment status before injury | ||||||||||||||
| Employed | 63.02 | 0.02 | ||||||||||||
| Student | 131.55 | 0.07 | 13.36 | 0.01 | ||||||||||
| Other† | 28.45 | 0.01 | 110.39 | 0.03 | ||||||||||
| Ventilator use at rehabilitation admission† | −50.44 | 0.01 | −56.24 | 0.01 | ||||||||||
| Severity score (CSI) | −0.66 | 0.02 | −0.97 | 0.07 | −0.65 | 0.02 | 0.24 | 0.02 | 0.43 | 0.06 | −0.48 | 0.01 | ||
| Admission FIM motor score | −2.68 | 0.06 | ||||||||||||
| Admission FIM cognitive score | 2.58 | 0.01 | −3.43 | 0.14 | −1.02 | 0.02 | ||||||||
| Clinician experience‡ | 4.54 | 0.03 | 2.05 | 0.01 | −2.44 | 0.01 | −1.79 | 0.02 | −1.51 | 0.04 | 1.19 | 0.03 | ||
*Independent variables allowed into models: age at injury, male, married, race – white, race – black, race – Hispanic, race – other, admission FIM motor score, admission FIM cognitive score, severity of illness score (CSI), injury group: C1–C4 ABC, injury group: C5–C8 ABC, injury group: Para ABC, injury group: AIS D, clinician experience, traumatic etiology – vehicular, traumatic etiology – violence, traumatic etiology – falls, traumatic etiology – sports, traumatic etiology – medical/surgical complication, traumatic etiology – other, work-related injury, number of days from trauma to rehabilitation admission, BMI >40, BMI 30–40, BMI <30, language – English, language – no English, language – English sufficient for understanding, payer – Medicare, payer – worker compensation, payer – private, payer – Medicaid, employment status at time of injury – employed, employment status at time of injury – student, employment status at time of injury – retired, employment status at time of injury – unemployed, employment status at time of injury – other, ventilator use at rehabilitation admission.
†Employment status at injury ‘other’ subcategory includes retired, unemployed, homemaker, on-job training, sheltered workshop, and unknown.
‡Clinician experience is for the discipline named in the column heading only.
Several patient/injury characteristics explained 89% of the variation in total treatment time (R2 = 0.89). LOS was the strongest predictor of total hours of therapy; when it was analyzed as the sole predictor of total hours, the R2 for LOS was 0.87; when it was included with other variables and all statistically significant predictors were considered, the type II semi-partial R2 for LOS was 0.47. The parameter estimate was 2.57, which indicates that for each added day of rehabilitation, patients received about 2.5 additional hours of therapy. The other factors that were associated (weakly) with longer treatment time (more total hours) were injury group C5–C8: ABC, being married, and treatment by clinicians with more experience (combined for all rehabilitation disciplines providing care to a patient). Ventilator use at rehabilitation admission, violent etiology of injury, older age, BMI >40 kg/m2, longer time from injury to rehabilitation admission, and higher admission motor FIM scores were significantly associated with less total treatment time, as indicated by their negative parameter estimates.
While LOS explained the majority of variation in total treatment time, several patient characteristics together explained 56% of the variance in LOS. Severity of illness as measured by the CSI explained 11% (semi-partial R2) of the variation. The parameter estimate for the CSI score (independent variable) was 0.48, which indicates that for each additional severity point, 0.48 more days were spent in rehabilitation. Therefore, a patient with a high severity score of 100 (only 8% of cases were at or above 100) would be predicted to receive 48 more days of inpatient rehabilitation than a patient with the lowest CSI score of 0 (parameter estimate of 0.48 × 100). Other factors associated with longer LOS included: ventilator use at the start of rehabilitation, worker compensation as payer source, English speaking, injury group C5–C8: ABC, race – other, and treatment by clinicians with more experience. The ‘race – other’ group included Native American (n = 4), Asian/Pacific Islander (n = 14), and unknown (n = 16) race/ethnicity. Higher admission FIM motor score and violent etiology of injury were associated with shorter LOS.
Patient and injury characteristics explained only about 17% of the variation in rehabilitation treatment time expressed as minutes per week. Fewer minutes per week was associated significantly with higher CSI severity of illness scores (semi-partial R2 = 0.04), older age, ventilator use at rehabilitation admission, injury group AIS D, etiologies of violence and medical–surgical complications, and Medicaid payer. More clinician experience was the only variable associated with more minutes per week.
Several of the predictors of total treatment time also were statistically significant in predicting time spent per week by each rehabilitation discipline (Table 4). A greater severity of illness as measured by CSI was associated with significantly less treatment time per week of PT, OT, and TR and less education/care management time per week by nursing (negative parameter estimates); higher severity of illness was associated with more time per week spent by ST and SW/CM (positive parameter estimates). Injury group AIS D was associated with less treatment time per week by nursing (bedside education/care management), TR, and PSY. In contrast, injury group C5–C8: ABC received more OT and less ST and SW/CM time per week. Higher FIM motor score on admission was associated with less OT time per week, while a higher FIM cognitive score was associated with more treatment time per week by PT and less treatment time per week by ST and PSY. More clinician experience (computed for each discipline separately) was associated with more time per week spent by PT, OT, and PSY, but less time per week spent by TR, ST, and SW/CM.
Discussion
The SCIRehab project is, to our knowledge, the first study that examines SCI inpatient rehabilitation comprehensively, using a set of nomenclatures to describe components of the rehabilitation process, documenting the type of intervention and the amount of time spent in each intervention. The information from the study's POC system provides the first detailed accounting of time spent by clinicians in each discipline providing SCI rehabilitation to people with various levels and completeness of injury. These data provide a unique opportunity to understand how patients with SCI spend their treatment time during their inpatient rehabilitation stay and what services clinicians deliver. As the SCIRehab study progresses, these data will provide the opportunity to study the relationships among (1) patient and injury characteristics, (2) the rehabilitation process, and (3) outcomes of interest achieved at 1 year after injury.
Tables in this paper provide the first documentation of the amount of time spent in treating four subgroups of people with SCI differentiated by level and completeness of injury, including the average total hours and the minutes per week spent by each discipline. Based on total hours of treatment throughout the inpatient rehabilitation stay, PT and OT combined accounted for approximately 60% of the entire therapy time; nursing (bedside education and care management) accounted for 17%, TR for 9%, PSY and SW/CM for 6% each, and ST for 2%. A similar distribution was found when treatment time per week was examined. The predominance of PT and OT interventions is not surprising since a primary focus of SCI inpatient rehabilitation is to increase independence in a broad spectrum of physical skills, which is the primary responsibility of PT and OT. Furthermore, most payers expect rehabilitation programs to provide a focus on PT and OT activities, and accreditation agencies require such programs. It should be remembered that documented nursing interventions only included education and care management provided by registered nurses. The relatively small amount of nursing time is explained by the exclusion of much direct nursing care provided by registered nurses and all care and education provided by licensed practical nurses and non-licensed nursing staff. Specifically, time dedicated to such nursing responsibilities as providing personal and wound care, administering medications, etc. was not documented.
In addition to documenting the average amounts of time spent in SCI rehabilitation interventions, a major contribution of this study is its identification of the extent of variability in intervention time from patient to patient. The interquartile range of the total hours of treatment throughout the entire rehabilitation stay, and across all disciplines, was quite large. The 75th percentile of total treatment time was more than double the 25th percentile, indicating that the 25% of patients with the most treatment time all received more than twice the treatment time delivered to the quarter of patients with the least treatment time. There was a similarly large interquartile range in the rehabilitation LOS, suggesting that variation in total treatment time might simply be due to variation in LOS. In order to control for the effect of LOS, treatment minutes per week is probably a better measure of intensity of interventions over the course of the entire hospitalization. However, calculating minutes per week reduced, but did not eliminate, variation in treatment time. For total treatment minutes per week across all disciplines combined, the 75th percentile was still 28% more than the 25th percentile. For PT and OT time, the 75th percentile was 45% more than the 25th percentile; for PSY and nursing, it was still more than twice the 25th percentile; for SW/CM, there was more than a 3-fold difference; and for TR, there was more than a 5-fold difference.
Clearly, much variance from patient to patient remains after controlling for LOS by calculating treatment time in terms of average minutes per week. Furthermore, there was relatively more variance in the minutes per week delivered by each discipline (as assessed by the 75th to 25th percentile ratio) than in the total treatment time across all disciplines. The reduction in overall treatment time variance achieved by calculating minutes per week rather than total hours masks substantial remaining variance within disciplines, indicating that there is a likely counterbalancing among discipline treatment times, such that a person receiving relatively larger amounts of treatment from one discipline may receive relatively less of one or more other disciplines. Differences in the amount of treatment patients receive from particular disciplines may be related to need (e.g. individuals with high tetraplegia receiving more ST than those with paraplegia) as well as supply or practice pattern variation (e.g. either an OT or a PT addressing an issue where both disciplines have expertise). Another potential reason for this counterbalancing of discipline time may be that rehabilitation facilities, which under the Medicare 3-hour rule are required by the Inpatient Rehabilitation Facility Prospective Payment System to deliver that many hours of services a day, do not receive additional reimbursement for providing more than 3 hours of services per day. The reimbursement by other payers may be structured differently, but even so, the number of active therapy hours that can be delivered in a day is limited by logistical issues. The papers that follow describe how therapists distributed time over major activity groups and offer additional information on patient differences and the treatments most commonly differentiating patients with many vs. few hours per week received.
In addition to variability in intervention time from patient to patient, significant differences were found in the years of SCI rehabilitation experience of clinicians who provide treatment to patients in the four neurologic injury groups. The larger number of years of experience of clinicians who provide treatment to patients with high tetraplegia may be reflective of clinical teams assigning clinicians with more experience to patients with greater care needs and assigning junior staff to patients with lower levels of injury.
The finding that total treatment time was explained predominantly by rehabilitation LOS should not be surprising as the longer LOS would result in increased opportunities for interventions by all treatment disciplines. The Medicare 3-hour rule requiring that on at least 5 days per week, patients receive at least 3 hours of therapy by OT, PT, ST, and orthotics/prosthetics has set a standard for all patients, whatever their payer, and most programs will have treatment times that are close to the standard, if not exceeding it. The discovery that the strongest predictor of LOS was the CSI score is similar to findings reported in the Post-Stroke Rehabilitation Outcomes Project.53 The higher CSI score implies a greater number and/or more severe co-morbidities, secondary medical conditions, and complications, which likely require greater medical attention and usually take a long time to manage. However, it is surprising that the CSI explains more of the variance in LOS and minutes of therapy per week than does the traditional major predictor used in SCI rehabilitation research, neurological injury group. While neurological category still has an effect (explaining about 1% of the variance in both instances), the independent effect of CSI (11% for LOS and 4% for minutes of treatment per week) is much larger.
Compared to the strong predictive models for total hours of treatment and LOS, relatively little variation in minutes of therapy (total or by discipline) per week is predicted by any of the individual or injury characteristics or by clinician experience. Although not strong predictive models, the variables explaining variation in minutes per week (Tables 3 and 4) seem to correspond with clinical expectations. Interestingly, the longer LOS for individuals with higher CSI did not mean that there was increased time per week spent in PT, OT, TR, or even nursing education; higher CSI actually predicted less time per week in each of these areas. This is likely explained by the fact that higher CSI implies greater illness or disability or medical complications, and therefore a lower tolerance for the types of interventions that may be provided by PT, OT, or TR. Less nurse education time per week is more difficult to explain, but it may be that the longer LOS provided the opportunity to spread a relatively fixed amount of educational content across more weeks, thereby reducing intensity. The time not used by PT, OT, TR, or nursing appeared to be spent in providing more ST and SW/CM. This finding also makes sense, given that LOS also varied with age, ventilator use, and medical–surgical complications. Individuals on ventilators often need more assistance with communication and swallowing, and thus need more ST. Furthermore, individuals with higher CSI, and on ventilators, may have more complicated discharge plans and require more intervention from SW/CM.
In this study, regression analyses were conducted to examine patient and injury characteristics associated with time spent in therapy during rehabilitation. Following typical PBE analytic strategy, center identity was not included among the predictors because the goal was not to compare one center to another but, instead, to identify underlying differences in patient and injury characteristics that help explain variation in treatment intensity (minutes per week). While center differences in treatment patterns should be acknowledged, they may reflect other variables not included in the analysis, rather than pure center effects. For instance, other patient and injury variables not entered into the regression analyses (e.g. bladder management techniques) may differ by center, and appear to be center effects, when center identity is just a surrogate for those measures. Alternatively, unmeasured characteristics of the centers (e.g. bed size, staffing ratios, etc.) that impact treatment delivery may ‘hide’ behind center identity. Keeping these caveats in mind, when center identity was allowed to enter the regression models reported here, the explained variation generally increased substantially. For total treatment time per week (across all disciplines), the center effect added 11% explained variance to the 17% explained by patient and injury factors. For the total minutes of treatment per week for each discipline separately, center effects added 3–30% explained variance to the 9–28% explained by patient and injury variables. In the two disciplines providing the most therapy (PT and OT) and in ST, the added center effects were smaller than the combined patient and injury effects. In the other four disciplines (Registered Nurse (RN), TR, SW, and PSY), the variance explained by added center effects was larger than the variance explained by patient and injury characteristics. The combination of patient, injury, and center effects explained 28–48% of the variance in treatment intensity, leaving the majority of the variance unexplained, which bodes well for the potential success of the PBE methodology. The significant variation in time spent that is not explained by patient and injury factors should prove useful in the eventual effort to correlate interventions with key patient outcomes. Ultimately, it will be variation in treatment patterns (whether the variation was due to patient, injury, clinician, or center characteristics) found associated with better outcomes that will lead to improvement in SCI rehabilitation.
Limitations
Participating rehabilitation centers provide variation in setting, care delivery patterns, and patient clinical and demographic characteristics and were selected to participate based on their willingness, geographic diversity, and expertise in treatment of patients with SCI. However, they are not a probability sample of the rehabilitation facilities that provide care for patients with SCI in the United States and time reported within specific disciplines may not be generalizable to all rehabilitation centers. The facilities involved include some of the largest SCI rehabilitation programs in the United States but the extent of bias resulting from unique referral patterns and from the fact that 10% of the eligible patients refused enrollment in this observational study is unknown.
No data were collected for the hours of treatment delivered by respiratory care, chaplaincy, and rehabilitation engineering; these disciplines tend to deliver small and less easily quantifiable amounts of care. Therapies that take up little time may have a major impact on patient outcomes, as may the activities of the attending and consulting physicians. While most of the work of rehabilitation physicians is patient assessment and ordering of therapies, the counseling of patient and family that physicians perform was not documented in the POC system. Physician contact was crudely captured through billing records, but those data are not reported in this manuscript. As previously emphasized, a large component of nursing care, including the time spent in bathing/hygiene activities, wound care, bladder and bowel management, etc., is not included in the data reported here. Only patient teaching and care management by rehabilitation nurses with at least RN preparation were recorded. Even for the disciplines using the POC system, time reported may have been in error through omissions, duplicate reports, and documentation errors within reported sessions. As indicated, therapist reports were compared with billing and other information to identify missed sessions, and these were completed retroactively. However, where no formal administrative reporting system existed (e.g. participation in TR-organized ‘social activities’) contacts not reported through the POC system may have been missed. It is also important to note that data reported were derived from supplemental documentation that was completed by clinicians in addition to their required clinical documentation.
Reporting the demographic and injury information, the neurological classification, and the CSI relied on abstracting of the medical record. As is common, these records sometimes had missing or ambiguous information, which could not always be supplemented from other documents or clinician memory.
Conclusion
This study provides the first comprehensive quantification of the SCI inpatient rehabilitation process, reporting the details of how clinicians spend their time with or for patients. Variations between and within SCI rehabilitation neurological injury groups in total hours of treatment during rehabilitation, LOS, total minutes of treatment per week, and treatment minutes per week for each rehabilitation discipline are large. A total of 89% of the variation in total treatment time was explained, primarily by LOS; 56% of variation in LOS was explained, with severity of illness accounting for 11% of the variation and a combination of patient and injury characteristics accounting for the remaining variation. Variation in treatment intensity was not well explained by patient and injury characteristics. When treatment minutes per week were summed across all disciplines, only 17% of the variation was explained; for treatment intensity by discipline, 9–28% of treatment minutes per week were explained.
In accordance with PBE methodology, the next step in the SCIRehab study will be to determine which treatment interventions are related with positive outcomes (at 1 year post injury), after controlling for patient and injury differences. The prospect of this approach being successful is enhanced by the fact that substantial variation was found in the amount of treatment time provided by various disciplines and by the fact that this variation in treatment time was not well explained by patient, injury, or clinician characteristics. This leaves the majority of treatment intensity variation available for predicting outcomes.
Acknowledgements
The contents of this paper were developed under grants from the National Institute on Disability and Rehabilitation Research, Office of Rehabilitative Services, US Department of Education, to Craig Hospital (grant # H133A060103 and # H133N060005), Carolinas Rehabilitation, Mount Sinai School of Medicine (grant # H133N060027), National Rehabilitation Hospital (grant # H133N060028), Rehabilitation Institute of Chicago (grant # H133N060014), and Shepherd Center (grant # H133N060009). The opinions contained in this publication are those of the grantees and do not necessarily reflect those of the US Department of Education.
References
- 1.Berns S, Lowman E, Rusk H, Covalt D, editors. Spinal cord injury. Rehabilitation costs and results in 31 successive cases including a follow-up study. Rehabilitation Monograph XIII New York: The Institute of Physical Medicine and Rehabilitation, New York University-Bellevue Medical Center; 1957 [Google Scholar]
- 2.National Spinal Cord Injury Statistical Center Annual report for the Spinal Cord Injury Model Systems 2008 (Table 51). Birmingham: University of Alabama; 2009 [Google Scholar]
- 3.Eastwood EA, Hagglund K, Ragnarsson K, Gordon W, Marino R. Medical rehabilitation length of stay and outcomes for persons with traumatic spinal cord injury – 1990–1997. Arch Phys Med Rehabil 1999;80(11):1457–63 [DOI] [PubMed] [Google Scholar]
- 4.Yokoyama O, Sakuma F, Itoh R, Sashika H. Paraplegia after aortic aneurysm repair versus traumatic spinal cord injury: functional outcome, complications, and therapy intensity of inpatient rehabilitation. Arch Phys Med Rehabil 2006;87(9):1189–94 [DOI] [PubMed] [Google Scholar]
- 5.Fromovich-Amit Y, Biering-Sørensen F, Baskov V, Juocevicius A, Hansen H, Gelernter I, et al. Properties and outcomes of spinal rehabilitation units in four countries. Spinal Cord 2009;47(8):597–603 [DOI] [PubMed] [Google Scholar]
- 6.Post M, Dallmeijer A, Angenot E, van Asbeck F, van der Woude L. Duration and functional outcome of spinal cord injury rehabilitation in the Netherlands. J Rehabil Res Dev 2005;423 Suppl 1:75–85 [DOI] [PubMed] [Google Scholar]
- 7.Pagliacci MC, Celani MG, Zampolini M, Spizzichino L, Franceschini M, Baratta S, et al. An Italian survey of traumatic spinal cord injury. The Gruppo Italiano Studio Epidemiologico Mielolesioni study. Arch Phys Med Rehabil 2003;84(9):1266–75 [DOI] [PubMed] [Google Scholar]
- 8.McKinley W, Santos K, Meade M, Brooke K. Incidence and outcomes of spinal cord injury clinical syndromes. J Spinal Cord Med 2007;30(3):215–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnston M, Wood K, Millis S, Page S, Chen D. Perceived quality of care and outcomes following spinal cord injury: minority status in the context of multiple predictors. J Spinal Cord Med 2004;27(3):241–51 [DOI] [PubMed] [Google Scholar]
- 10.Meiners T, Böhm V, Schlüter E. Analyse von FIM-Werten während der stationären Behandlung nach akuter Querschnittlähmung (Analysis of FIM-values during the hospital treatment of patients with acute spinal cord injury). E Rehabilitation (Stuttg) 2004;43(3):129–36 [DOI] [PubMed] [Google Scholar]
- 11.Garcia R, Gaebler-Spira D, Sisung C, Heinemann A. Functional improvement after pediatric spinal cord injury. Am J Phys Med Rehabil 2002;81(6):458–63 [DOI] [PubMed] [Google Scholar]
- 12.Jakob W, Wirz M, van Hedel H, Dietz V, EM-SCI Study Group Difficulty of elderly SCI subjects to translate motor recovery – ‘body function’ – into daily living activities. J Neurotrauma 2009;26(11):2037–44 [DOI] [PubMed] [Google Scholar]
- 13.Seel R, Huang M, Cifu D, Kolakowsky-Hayner S, McKinley W. Age-related differences in length of stays, hospitalization costs, and outcomes for an injury-matched sample of adults with paraplegia. J Spinal Cord Med 2001;24(4):241–50 [DOI] [PubMed] [Google Scholar]
- 14.Osterthun R, Post M, van Asbeck F. Characteristics, length of stay and functional outcome of patients with spinal cord injury in Dutch and Flemish rehabilitation centres. Spinal Cord 2009;47(4):339–44 [DOI] [PubMed] [Google Scholar]
- 15.Pagliacci M, Celani M, Spizzichino L, Zampolini M, Aito S, Citterio A, et al. Spinal cord lesion management in Italy: a 2-year survey. Spinal Cord 2003;41(11):620–8 [DOI] [PubMed] [Google Scholar]
- 16.Tooth L, McKenna K, Geraghty T. Rehabilitation outcomes in traumatic spinal cord injury in Australia: functional status, length of stay and discharge setting. Spinal Cord 2003;41(4):220–30 [DOI] [PubMed] [Google Scholar]
- 17.Heinemann AW, Kirk P, Hastie BA, Semik P, Hamilton BB, Linacre JM, et al. Relationships between disability measures and nursing effort during medical rehabilitation for patients with traumatic brain and spinal cord injury. Arch Phys Med Rehabil 1997;78(2):143–9 [DOI] [PubMed] [Google Scholar]
- 18.Heinemann A, Hamilton B, Linacre J, Wright B, Granger C. Functional status and therapeutic intensity during inpatient rehabilitation. Am J Phys Med Rehabil 1995;74(4):315–26 [DOI] [PubMed] [Google Scholar]
- 19.Gassaway J, Whiteneck G, Dijkers M. SCIRehab: clinical taxonomy development and application in spinal cord injury rehabilitation research. J Spinal Cord Med 2009;32(3):260–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Whiteneck G, Dijkers M, Gassaway J, Jha A. SCIRehab: new approach to study the content and outcomes of spinal cord injury rehabilitation. J Spinal Cord Med 2009;32(3):251–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Natale A, Taylor S, LaBarbera J, Mumma S, Bensimon L, McDowell S, et al. SCIRehab: the physical therapy taxonomy. J Spinal Cord Med 2009;32(3):270–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnson K, Bailey J, Rundquist J, Dimond P, McDonald C, Reyes I, et al. SCIRehab: the supplemental nursing taxonomy. J Spinal Cord Med 2009;32(3):328–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ozelie R, Sipple C, Foy T, Cantoni K, Kellogg K, Lookingbill J, et al. SCIRehab: the occupational therapy taxonomy. J Spinal Cord Med 2009;32(3):283–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilson C, Huston T, Koval J, Gordon S, Schwebel A, Gassaway J. SCIRehab: the psychology taxonomy. J Spinal Cord Med 2009;32(3):318–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gordan W, Dale B, Brougham R, Spivack-David D, Georgeadis A, Adornato V, et al. SCIRehab: the speech language pathology taxonomy. J Spinal Cord Med 2009;32(3):306–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cahow C, Skolnick S, Joyce J, Jug J, Dragon C, Gassaway J. SCIRehab: the therapeutic recreation taxonomy. J Spinal Cord Med 2009;32(3):297–305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abeyta N, Freeman E, Primack D, Harmon A, Dragon C, Hammond F, et al. SCIRehab: the social work/case management taxonomy. J Spinal Cord Med 2009;32(3):335–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hammond F, Gassaway J, Abeyta N, Freeman E, Primack D. SCIRehab: social work and case management treatment time during inpatient spinal cord injury rehabilitation. J Spinal Cord Med 2010;33:TBA [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taylor S, LaBarbera J, McDowell S, Zanca J, Natale A, Mumma S, et al. SCIRehab: physical therapy treatment time during inpatient spinal cord injury rehabilitation. J Spinal Cord Med 2011;34(2):151–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gassaway J, Dijkers M, Rider C, Edens K, Cahow C, Joyce J. SCIRehab: therapeutic recreation treatment time during inpatient spinal cord injury rehabilitation. J Spinal Cord Med 2011;34(2):178–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huston T, Gassaway J, Wilson C, Gordon C, Koval J, Schwebel A. SCIRehab: psychology treatment time during inpatient spinal cord injury rehabilitation. J Spinal Cord Med 2011;34(2):198–206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rundquist J, Gassaway J, Bailey J, Lingefelt P, Reyes I, Thomas J. SCIRehab: nursing bedside education and care management time during inpatient spinal cord injury rehabilitation. J Spinal Cord Med 2011;34(2):207–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Foy T, Perritt G, Thimmaiah D, Heisler L, Offutt J, Cantoni K, et al. SCIRehab: occupational therapy treatment time during inpatient spinal cord injury rehabilitation. J Spinal Cord Med 2011;34(2):164–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brougham R, Spivack-David D, Adornato V, Gordan W, Dale B, Georgeadis A, et al. SCIRehab: speech language pathology therapy treatment time during inpatient spinal cord injury rehabilitation. J Spinal Cord Med 2011;34(2):188–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Horn S, Gassaway J. Practice-based evidence study design for comparative effectiveness research. Med Care 2007;45Suppl 2:S50–7 [DOI] [PubMed] [Google Scholar]
- 36.DeJong G, Horn S, Gassaway J, Stam HJ. Practice-based evidence for post-acute policy and practice: the case of joint replacement rehabilitation. Presented at Annual Conference of the American Congress of Rehabilitation Medicine, Washington, DC; 2007 [Google Scholar]
- 37.Gassaway J, Horn S, DeJong G, Smout R, Clark C, James R. Applying the clinical practice improvement approach to stroke rehabilitation: methods used and baseline results. Arch Phys Med Rehabil 2005;8612 Suppl 2:S16–33 [DOI] [PubMed] [Google Scholar]
- 38.Horn S, DeJong G, Ryser D, Veazie P, Teraoka J. Another look at observational studies in rehabilitation research: going beyond the holy grail of the randomized controlled trial. Arch Phys Med Rehabil 2005;8612 Suppl 2:S8–15 [DOI] [PubMed] [Google Scholar]
- 39.DeJong G, Hsieh C, Gassaway J, Horn S, Smout R, Putman K, et al. Characterizing rehabilitation services for patients with knee and hip replacement in skilled nursing and inpatient rehabilitation facilities. Arch Phys Med Rehabil 2009;90(8):1284–96 [DOI] [PubMed] [Google Scholar]
- 40.Tunis S, Stryer D, Clancy C. Practical clinical trials: increasing the value of clinical research for decision making in clinical and health policy. JAMA 2003;290(1):1624–32 [DOI] [PubMed] [Google Scholar]
- 41.Marino R, editor. Reference manual for the International Standards for Neurological Classification of SCI. Chicago, IL: American Spinal Injury Association; 2003 [Google Scholar]
- 42.Fiedler R, Granger C, Russell C. UDS(MR)SM: follow-up data on patients discharged in 1994–1996. Uniform data system for medical rehabilitation. Am J Phys Med Rehabil 2000;79(2):184–92 [DOI] [PubMed] [Google Scholar]
- 43.Fiedler R, Granger C. Functional independence measure: a measurement of disability and medical rehabilitation. In: Chino N, Melvin J. (eds.) Functional evaluation of stroke patients. Tokyo: Springer-Verlag; 1996. p. 75–92 [Google Scholar]
- 44.Horn S, editor. Clinical practice improvement; implementation and evaluation. New York, NY: Faulkner and Gray; 1997 [Google Scholar]
- 45.Horn S, Sharkey P, Buckle J, Backofen J, Averill R, Horn R. The relationship between severity of illness and hospital length of stay and mortality. Med Care 1991;29(4):305–17 [DOI] [PubMed] [Google Scholar]
- 46.Ryser D, Egger M, Horn S, Handrahan D, Ghandi P, Bigler E. Measuring medical complexity during inpatient rehabilitation following traumatic brain injury. Arch Phys Med Rehabil 2005;86:1108–17 [DOI] [PubMed] [Google Scholar]
- 47.Averill R, McGuire T, Manning B, Fowler D, Horn S, Dickson P, et al. A study of the relationship between severity of illness and hospital cost in New Jersey hospitals. Health Serv Res 1992;27(5):587–617 [PMC free article] [PubMed] [Google Scholar]
- 48.Clemmer T, Spuhler V, Oniki T, Horn S. Results of a collaborative quality improvement program on outcomes and costs in a tertiary critical care unit. Crit Care Med 1999;27(9):1768–74 [DOI] [PubMed] [Google Scholar]
- 49.Horn S, Torres AJ, Willson D, Dean J, Gassaway J, Smout R. Development of a pediatric age- and disease-specific severity measure. J Pediatr 2002;141(4):496–503 [DOI] [PubMed] [Google Scholar]
- 50.Willson D, Horn S, Smout R, Gassaway J, Torres A. Severity assessment in children hospitalized with bronchiolitis using the pediatric component of the Comprehensive Severity Index (CSI®). Pediatr Crit Care Med 2000;1(2):127–32 [DOI] [PubMed] [Google Scholar]
- 51.Stevens J. Intermediate statistics: a modern approach. 2nd ed. Mahwah, NJ: Lawrence Erlbaum Associates, Inc.; 1999 [Google Scholar]
- 52.Stevens J. Partial and semipartial correlations; 2003 [accessed 2010 Feb 10]. Available from: www.uoregon.edu/~stevensj/MRA/partial.pdf [Google Scholar]
- 53.Horn S, DeJong G, Smout R, Gassaway J, James R, Conroy B. Stroke rehabilitation patients, practice, and outcomes: is earlier and more aggressive therapy better? Arch Phys Med Rehabil 2005;8612 Suppl 2:S101–14 [DOI] [PubMed] [Google Scholar]