Abstract
Background
There is a lack of published evidence regarding the amount and type of social work and case management (SW/CM) services that an individual with traumatic spinal cord injury (SCI) receives during acute inpatient rehabilitation. Such information is needed to assist in resource planning, benchmarking, and research on interventions and outcomes.
Methods
As part of the SCIRehab study social workers and case managers at six inpatient rehabilitation facilities documented details (including time spent) about the interventions provided to 600 patients with traumatic SCI during acute inpatient rehabilitation. Associations between patient and injury characteristics and time spent on these activities were examined.
Results
Patients received a mean total of 10 hours of SW/CM services, with a mean of 72.8 total minutes per week. The majority of the patients received SW/CM time spent on interdisciplinary conferencing on the patient's behalf (96%), discharge planning and services (89%), financial planning (67%), community/in-house services (66%), supportive counseling (56%), and initial assessment (54%). A minority of the patients received peer advocacy (12%), classes (24%), and education topics (30%). Total hours per stay and minutes per week varied by level of injury group. The most time per week was dedicated to patients with high tetraplegia ASIA Impairment Scale (AIS) A–C and the least to patients with C5–C8 AIS A–C. The patient and injury characteristics studied did not explain the variance seen in time spent on specific SW/CM services.
Conclusions
These descriptive data may be helpful in resource planning to anticipate and address individual patient needs and to plan for department-level training and hiring. These data also may pave the way to studying relationships of interventions with patient outcomes.
Keywords: Spinal cord injuries, Traumatic, SCIRehab Project, Practice-based evidence, Rehabilitation, Physical, Tetraplegia, Paraplegia, Social work, Case management, Comprehensive Severity Index
Introduction
Social work and case management (SW/CM) services during inpatient spinal cord injury (SCI) rehabilitation serve a variety of patient and family needs that may wax and wane in intensity throughout the rehabilitation stay. Social workers/case managers identify the needs of the patients and families on admission and reassess these needs throughout the rehabilitation process. The ultimate goal is to prepare the patient and family for a safe and effective discharge by maximizing knowledge and identifying and addressing physical, economic, and emotional barriers to optimal community discharge. SW/CM also facilitates communications between the patient/family and the rehabilitation team. Expertise in financial planning, discharge services, and community and in-home services, and organizing peer and advocacy groups are unique SW/CM contributions that may influence reintegration into the community. However, the evidence base is limited for many SW/CM interventions and time spent providing services or specific interventions. Data that describe the amount of time SCI rehabilitation social workers/case managers spend with patients and on which activities are needed. This information may be helpful in resource planning for meeting patient needs, as well as department-level training and hiring needs. These data also may pave the way to studying relationships of interventions with patient outcomes.
Evidence of the role and effect of SW/CM for patients with traumatic SCI is sparse, whether it involves acute care, acute rehabilitation care, or outpatient supportive roles. SW/CM services, in cooperation with collaborative, multidisciplinary care, have been shown to be beneficial in reducing some areas of difficulty faced by trauma patients.1 On the other hand, a randomized control trial of a disease management program that provided post-discharge emotional support, care coordination, education, and communication for patients with more than 72 hours of continuous mechanical ventilation in an intensive care unit and their caregivers did not demonstrate a statistically significant effect of disease management on long-term outcomes (depression, overall health, and caregiver burden).2 A report by the American Hospital Association when case management was still in its infancy as a profession, concluded that case management can ‘achieve a higher and/or faster level of recovery, which ultimately results in lower costs’.3 In a case study, Glidden 4 contrasted the outcomes of two patients with SCI who received different degrees of SW/CM services (one individual received continuous intervention while the other received minimal intervention), highlighting the worse financial, physical, emotional, and social stability outcomes with less SW/CM participation in the patient's care and management.
This paper aims to describe how social workers/case managers spend time with patients or on a patient's behalf during inpatient rehabilitation following traumatic SCI. Differences in how time is spent with patients with different injury levels and the percentage of patients who receive specific services are described. We also examine associations of patient and injury characteristics with time spent on specific SW/CM activities.
Methods
The SCIRehab Project is a multi-center, 5-year investigation recording and analyzing the details of the SCI inpatient rehabilitation process for approximately 1400 patients; only patients enrolled in the first year are included in this paper. Ultimately these processes will be related to first year post-injury outcomes. The study design and implementation of practice-based evidence (PBE) procedures in this project have been described previously.5,6 A SW/CM taxonomy, which classifies the types of interventions provided during acute rehabilitation, was created for the SCIRehab Project;7 clinicians collected data on the details of the main activities that are the focus of social workers/case managers in the acute rehabilitation setting and the amount of time the social worker/case manager spends on the patient's behalf in each topic area. The introductory paper to this series of SCIRehab Project articles8 describes the study design, including use of PBE research methodology5,6,9–12 inclusion criteria, data sources, and the analysis plan. Briefly, the SCIRehab team included representatives of all rehabilitation clinical disciplines (including SW/CM) from six inpatient rehabilitation facilities: Craig Hospital, Englewood, CO; Shepherd Center, Atlanta, GA; Rehabilitation Institute of Chicago, Chicago, IL; Carolinas Rehabilitation, Charlotte, NC; Mount Sinai Medical Center, New York, NY; and National Rehabilitation Hospital, Washington, DC. IRB approval was obtained at each center and patients who were 12 years of age or older, who gave (or whose parent/guardian gave) informed consent, and were admitted to the facility's SCI unit for initial rehabilitation following traumatic SCI were enrolled.
Patient/injury and clinician data
Trained data abstractors collected patient and injury data from patient medical records. The International Standards of Neurological Classification of SCI13 were used to describe the motor level and completeness of injury. Patients with ASIA Impairment Scale (AIS) grade D were grouped together regardless of injury level. Patients with AIS classifications of A, B, and C were grouped together and separated by motor level to determine the remaining three injury groups: high tetraplegia (C1–C4), low tetraplegia (C5–C8), and paraplegia (T1 and below). These injury categories were selected because they were each large enough for analysis and created groupings thought to have relatively homogenous functional ability within groups and clear differences between the groups. The Comprehensive Severity Index (CSI®) was used to score the extent of deviation from normal physiological status each of a patient's complications and comorbidities constituted at the time of rehabilitation admission and over time within the center.14–18 The higher the patient's CSI score, the more deviant from normal (‘the sicker’) the patient was. The Functional Independence Measure (FIM®) was used to describe a patient's independence in motor and cognitive abilities at rehabilitation admission and discharge.19,20 The social worker/case manager who documented treatment data for the SCIRehab Project completed a clinician profile that included their years of SCI rehabilitation experience at the start of the project.
SW/CM treatment data
The social worker/case manager at each SCIRehab Project site inputs details about each study patient and their relevant family circumstances into a handheld personal digital assistant (PDA)
(Hewlett Packard PDA hx2490b, Palo Alto, CA) containing a modular custom application of the SCIRehab point-of-care documentation system, which incorporated the SW/CM taxonomy (PointSync Pro version 2.0, MobileDataforce, Boise, ID, USA). This taxonomy, which is summarized in Table 1, has been described in detail previously,7 and includes areas of focus that are commonly employed in an SCI rehabilitation setting.
Table 1.
SW/CM taxonomy of interventions and sub-interventions
| Discharge planning and servicesHomeHome accessibilityBarriers to dischargeNursing home/long-term acute careAssisted livingReferring facilityTransitional living facilityAlternative living environmentHome healthPersonal care servicesOutpatient therapyDay rehabilitation programAdult day careSubstance abuse programMedical follow-upDurable medical equipment (DME)Supplies/meds | Community/in-house servicesWaiver programLifelinesCrime victims assistanceVocationalDepartment of agingCorrespondenceChaplainLegal aide/legal servicesTransportationHousingService recovery/care coordinationOther services |
| Financial planningSupplemental Security Insurance (SSI)Social Security Disability Insurance (SSDI)FundraisingTrust fund/facility fundsMedicare/MedicaidInsuranceAlternative benefits/funding/self-payWorkers compensation | Supportive counselingPhysical/psychological abuseAlcohol/substance abuseCultural considerationsCoping/adjustmentKnowledge of injuryMedical comorbiditiesSexuality |
| Peer/advocacy provide information and initiate referralNational organizationsSupport groupsIndependent living centers | EducationSCI written materialsAdvance directivesCommunity re-entryGuardianship |
| Team and patient/family conferencesMedicalGoal settingDischargeBehaviorLegalOther |
Each clinician was trained and tested on use of the documentation system; reliability testing was performed quarterly throughout the data collection period. Entered into the PDA were the date/time of each interaction with or on behalf of a patient, the number of minutes spent on each SW/CM activity, who the interaction included (patient, family, caregiver, clinical team member, community resource person, or any combination of the above), whether the interaction involved providing education, and if it was in response to a referral. This was done each time during the day the social worker/case manager interacted with the patient or acted on behalf of the patient for more than 5 minutes at a time. Intervention minutes were combined to equal the approximate duration of time spent during each day of rehabilitation.
Data analysis
Time spent on SW/CM interventions each day was summed to obtain the total number of hours spent during the rehabilitation stay. Because total time is correlated highly with length of stay (LOS), which increases the opportunity to receive services, we calculated the average minutes per week and used this as another measure of service intensity. Contingency tables/chi-square tests and analysis of variance were used to test differences across injury groups for categorical and continuous variables, respectively (P < 0.05 was considered statistically significant).
Patient and injury characteristics associated with time spent on SW/CM interventions were examined using ordinary least-squares stepwise regression models.21,22 The predictors used were: age at injury, gender, marital status, race (white, African American, Hispanic, other), admission FIM motor score, admission FIM cognitive score, severity of illness score (CSI), injury group C1–C4 ABC, injury group C5–C8 ABC, injury group Para ABC, injury group AIS D, clinician experience, traumatic etiology (vehicular, violence, falls, sports, medical/surgical complication, other), work-related injury, number of days from trauma to rehabilitation admission, body mass index (BMI, kg/m2)>40, BMI 30–40, BMI <30, language (English, English sufficient for understanding, no English), payer (Medicare, worker compensation, private, Medicaid), employment status at time of injury (employed, student, retired, unemployed, other), and ventilator use at rehabilitation admission. Only the models for activities that at least 70% of patients participated in and those with an R2 value of greater than 0.2 are reported.
Results
Details of patient demographic and injury characteristics are presented for the sample as a whole and for each of the four injury groups separately in the first article in this SCIRehab series 8 (Table 1). The sample was 81% male, 65% white, 38% married, mostly not obese (82% had a BMI of <30 kg/m2), 65% were employed at the time of injury, and the patients had an average age of 37 years. Vehicular accidents were the most common cause of injury (49%), followed by falls (23%), and sports and violent etiologies (11% each). The mean rehabilitation LOS was 55 days (range 2–259 days, standard deviation (SD) 37, median 43). The mean total FIM score at admission was 53 (SD 15), with a mean motor score of 24 (SD ± 12) and a cognitive score of 29 (SD ± 6). A mean of 32 days (SD ± 28) had elapsed from the time of injury to the time of rehabilitation admission.
All 600 patients had at least some SW/CM intervention during their rehabilitation stay. The percent of patients receiving each type of SW/CM intervention and sub-intervention is summarized in Table 2. Most patients (89%) received discharge planning and services intervention. This category of intervention included multiple sub-intervention areas; at least half of the study patients worked with the social worker/case manager to address home accessibility and barriers to discharge issues, as well as planning for medical follow-up and durable medical equipment needs. Plans for provision of supplies and medications also were addressed often (with 48% of patients). Of all sessions that addressed discharge planning, barriers to discharge was included in 79% of these sessions.
Table 2.
SW/CM interventions and sub-interventions: percent patients receiving, percent sessions in which interventions included, and percent of sessions for intervention that include sub-intervention
| Intervention Sub-intervention | % of 600 patients that received | % of all sessions that included the intervention/sub-intervention | % of sessions for the intervention that included the sub-intervention |
|---|---|---|---|
| Initial assessment* | 53.7 | 5.2 | — |
| Discharge planning and Services | 88.7 | ||
| Home | 51.0 | 13.0 | 43.0 |
| Home accessibility | 57.8 | 17.5 | 57.7 |
| Barriers to discharge | 58.7 | 14.8 | 79.1 |
| Nursing home / long-term acute care | 15.3 | 6.2 | 20.3 |
| Assisted living | 2.2 | 0.4 | 1.3 |
| Referring facility | 3.5 | 0.3 | 1.1 |
| Transitional living facility | 6.0 | 1.0 | 3.2 |
| Alternative living environment | 13.5 | 1.9 | 6.4 |
| Home health | 36.8 | 10.6 | 41.5 |
| Personal care services | 22.7 | 3.8 | 15.0 |
| Outpatient therapy | 43.5 | 7.5 | 29.4 |
| Day rehab program | 29.5 | 5.4 | 20.9 |
| Adult day care | 1.3 | 0.1 | 0.4 |
| Substance abuse program | 0.8 | 0.1 | 0.3 |
| Medical follow-up | 51.0 | 9.1 | 25.4 |
| Durable medical equipment | 50.0 | 12.7 | 49.7 |
| Supplies/medications | 48.3 | 8.4 | 32.9 |
| Financial planning | 66.7 | — | |
| Social Security Income/Social Security Disability income (SSI/SSDI) | 40.7 | ||
| Fundraising | 11.5 | 11.1 | 42.9 |
| Trust fund/facility fund | 16.2 | 1.1 | 4.4 |
| Medicaid/Medicare | 35.3 | 1.6 | 6.1 |
| Insurance | 44.5 | 8.0 | 30.8 |
| Alternative benefits/funding/self-pay options | 31.3 | 11.5 | 44.2 |
| Workers compensation | 7.5 | 1.7 | 18.7 |
| Community/in-house services | 66.3 | — | |
| Waiver program | 12.7 | 2.1 | 11.9 |
| Lifelines | 2.3 | 0.2 | 1.2 |
| Crime victims assistance | 3.3 | 0.4 | 2.6 |
| Vocational | 20.0 | 2.3 | 13.4 |
| Department of aging | 2.3 | 0.2 | 1.0 |
| Correspondence | 24.5 | 4.5 | 25.7 |
| Chaplain | 1.2 | 0.1 | 0.5 |
| Legal aide/services | 9.5 | 1.1 | 6.3 |
| Other services | 32.7 | 5.0 | 29.0 |
| Transportation | 38.5 | 6.1 | 35.3 |
| Housing | 19.5 | 2.2 | 12.8 |
| Service recovery/care | 8.2 | 1.3 | 7.3 |
| Supportive counseling | 55.7 | — | |
| Physical/psychological abuse | 1.5 | 0.1 | 0.7 |
| Alcohol/substance abuse | 2.5 | 0.2 | 1.4 |
| Cultural considerations | 3.3 | 0.3 | 1.8 |
| Coping/adjustment | 51.3 | 16.2 | 92.0 |
| Knowledge of injury | 30.8 | 3.8 | 21.3 |
| Medical comorbidities | 11.5 | 1.4 | 8.1 |
| Sexuality | 2.3 | 0.2 | 1.2 |
| Education | 29.8 | — | |
| SCI written materials | 17.8 | 1.6 | 47.5 |
| Advance directives | 5.2 | 0.6 | 19.3 |
| Community re-entry | 16.5 | 1.7 | 51.1 |
| Guardianship | 1.3 | 0.1 | 2.9 |
| Peer/advocacy Groups | 11.7 | ||
| National organizations | 8.0 | 1.2 | 59.8 |
| Support groups | 7.2 | 1.1 | 53.3 |
| Independent living centers | 8.3 | 1.7 | 84.6 |
| Team conferences/consults† | 95.7 | ||
| Medical | 54.7 | 10.9 | 66.3 |
| Goal setting | 49.0 | 10.3 | 62.9 |
| Discharge | 53.7 | 10.6 | 64.9 |
| Behavior | 17.2 | 4.5 | 27.7 |
| Education | 29.0 | 3.9 | 24.1 |
| Legal | 4.0 | 0.4 | 2.7 |
| Other | 27.0 | 4.4 | 27.0 |
| Classes led by social worker/case manager* | 23.8 | — |
*No additional data (subtopics) collected.
†May or may not include the patient/family.
Social workers/case managers worked with 67% of the 600 patients on financial planning; social security disability insurance was discussed with 41% of patients, insurance plans with 45%, Medicare or Medicaid with 35%, workers compensation with 7%, and alternate benefits/funding/self-pay or other options with 31% of patients. Work also was done to coordinate fundraising efforts and explore trust funds with a small percentage of patients (12%), but when it was addressed, it was addressed often (was a part of 43% of all sessions that included any financial planning).
Social workers/case managers provided information and coordination for services offered in the community and the rehabilitation facility; the most commonly addressed were transportation issues. Supportive counseling was documented as being provided to 56% of patients; most of this work focused on coping and adjustment issues, which was addressed in 92% of all sessions involving supportive counseling. A smaller percentage of patients received information about community re-entry programs, advanced directives, and guardianship, as well as receiving facility pamphlets and other written materials describing spinal cord injuries. Social workers/case managers provided information about community peer or advocacy groups such as national organizations, support groups, and independent living centers to a small percentage of patients (12%). These clinicians participated in interdisciplinary team conferences for almost all patients (96%) and the most common issues addressed during these conferences were discharge planning, goal setting, and medical issues.
Table 3 lists the mean amount of time (total hours during rehabilitation and a calculated average of minutes per week) social workers/case managers spent on each type of service directly with patients or on the patient's behalf, for the total sample and for injury groups separately. The mean amount of total time spent was 10 hours (median 5.6 hours, range, 0.1–89.5, SD 11.6); the calculated mean minutes per week was 73 (median 55 minutes, range 2–365, SD 56). The SW/CM activity that consumed the most time was discharge planning and services (24 minutes per week), followed by financial planning (9 minutes per week). In addition, social workers/case managers spent considerable time participating in interdisciplinary conferences (18 minutes per week).
Table 3.
SW/CM: percent of patients receiving each type of activity, mean total hours (standard deviation), and mean minutes/week (standard deviation), by injury category*
| SW/CM activities for all patients | Full SCIRehab sample n = 600 | C1–4 AIS ABC, n = 132 | C5–8 AIS ABC, n = 151 | Para AIS ABC, n = 223 | AIS D, n = 94 |
|---|---|---|---|---|---|
| All SW/CM activities (%) | 100 | 100 | 100 | 100 | 100 |
| Total hours (SD)† | 10.0 (11.6) | 16.1 (17.3) | 9.9 (9.4) | 8.1 (8.8) | 6.0 (6.0) |
| Minutes per week (SD)† | 72.8 (56.3) | 83.2 (64.6) | 61.6 (42.3) | 72.0 (58.5) | 77.8 (56.1) |
| Initial assessment (%) | 54 | 51 | 52 | 51 | 66 |
| Total hours (SD) | 0.5 (0.6) | 0.5 (0.5) | 0.5 (0.6) | 0.5 (0.6) | 0.6 (0.6) |
| Minutes per week (SD)† | 4.9 (9.8) | 2.7 (4.0) | 3.1 (4.3) | 4.9 (10.0) | 11.1 (16.7) |
| Discharge plan and services (%) | 89 | 94 | 87 | 88 | 84 |
| Total hours (SD)† | 3.2 (4.9) | 6.1 (7.9) | 2.8 (3.4) | 2.5 (3.3) | 1.8 (2.1) |
| Minutes per week (SD)† | 23.9 (25.6) | 31.5 (30.6) | 17.2 (18.3) | 23.3 (25.7) | 25.4 (24.6) |
| Financial planning (%) | 67 | 79 | 73 | 65 | 45 |
| Total hours (SD)† | 1.4 (2.5) | 2.4 (3.6) | 1.4 (2.0) | 1.1 (2.1) | 0.5 (0.9) |
| Minutes per week (SD)† | 9.1 (12.7) | 11.8 (14.1) | 8.8 (10.3) | 9.0 (14.0) | 5.8 (10.1) |
| Community in house (%) | 66 | 74 | 69 | 64 | 56 |
| Total hours (SD)† | 0.8 (1.5) | 1.4 (2.3) | 0.8 (1.1) | 0.7 (1.1) | 0.5 (1.1) |
| Minutes per week (SD) | 6.4 (10.6) | 8.2 (14.5) | 5.0 (7.2) | 6.3 (8.9) | 6.7 (12.2) |
| Supportive counseling (%) | 56 | 66 | 61 | 51 | 44 |
| Total hours (SD)† | 0.8 (1.7) | 1.4 (2.6) | 0.8 (1.4) | 0.6 (1.1) | 0.6 (1.2) |
| Minutes per week (SD) | 5.4 (9.1) | 7.0 (11.1) | 4.7 (7.1) | 4.6 (7.9) | 6.1 (11.1) |
| Education (%) | 30 | 34 | 34 | 24 | 30 |
| Total hours (SD) | 0.1 (0.3) | 0.1 (0.3) | 0.1 (0.3) | 0.1 (0.2) | 0.1 (0.3) |
| Minutes per week (SD) | 1.1 (3.0) | 0.9 (1.8) | 1.1 (2.4) | 0.9 (2.3) | 1.9 (5.5) |
| Peer advocacy groups (%) | 12 | 17 | 13 | 12 | 2 |
| Total hours (SD) | 0.1 (0.6) | 0.2 (0.7) | 0.2 (0.8) | 0.1 (0.5) | 0.0 (0.0) |
| Minutes per week (SD) | 0.6 (2.8) | 0.7 (2.4) | 0.7 (3.0) | 0.8 (3.4) | 0.1 (0.4) |
| Interdisciplinary conferencing‡ (%) | 96 | 98 | 97 | 96 | 90 |
| Total hours (SD) | 2.3 (1.8) | 3.1 (2.2) | 2.7 (1.7) | 2.0 (1.6) | 1.5 (1.4) |
| Minutes per week (SD) | 17.7 (9.2) | 17.0 (7.0) | 17.6 (8.6) | 18.3 (10.1) | 17.4 (10.3) |
| Classes (%) | 24 | 30 | 25 | 23 | 17 |
| Total hours (SD)† | 0.6 (1.3) | 0.8 (1.4) | 0.7 (1.5) | 0.5 (1.2) | 0.3 (0.9) |
| Minutes per week (SD) | 3.2 (7.1) | 3.3 (6.3) | 3.2 (6.4) | 3.6 (7.9) | 2.2 (6.8) |
*Hours and minutes per week are averages over all 600 patients, not just based on those who did receive one or more sessions of a particular activity.
†Statistically significant differences in time spent among injury groups.
‡Time spent by social worker/case manager.
Significant differences among injury groups were seen in time (both total hours and minutes per week) spent on discharge planning and services and financial planning; patients in the AIS D injury group received less total time (but not minutes per week) than patients in the other injury groups for discharge planning and services and less total time and minutes per week on financial planning. Patients in the AIS D group had more minutes per week dedicated to initial assessment than the other injury groups. Patients with high tetraplegia (C1–C4, ABC) received more time in many of the activities than the other injury groups, specifically greater total hours and minutes per week were spent on discharge planning and services and financial planning, while more total hours (but not minutes per week) were spent working on community/in-house services and supportive counseling. Patients in the C5–C8 ABC group received the fewest minutes per week of discharge planning and services.
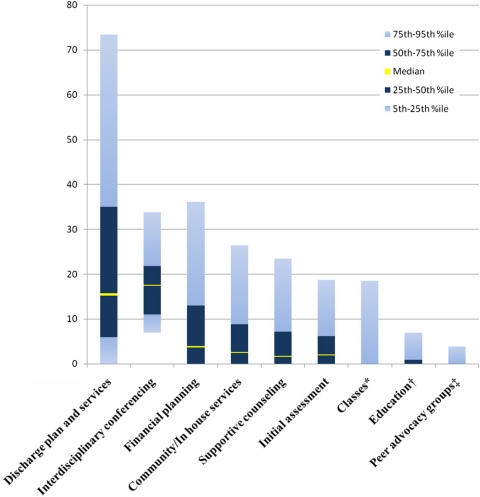
The substantial variation in time spent on the various SW/CM activities is depicted in Fig. 1. The greatest range in time spent occurred in discharge planning and services, where the interquartile range was 6–34 minutes/week (median 16).
Figure 1.
Variation in time spent (minutes/week) on each of nine SW/CM interventions.Notes: *24% of sample, all above 75th percentile (median=0); †30% of sample, all above 50th percentile (median=0); ‡12% of sample, all above 75th percentile (median=0)
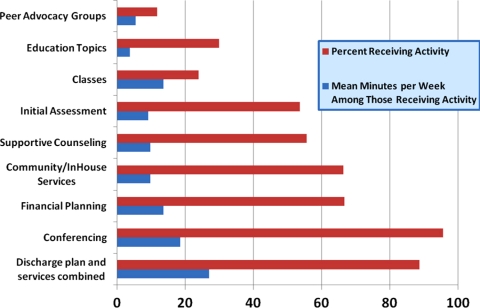
The percentage of patients who received each SW/CM activity and the mean number of minutes per week spent on that activity for those patients is summarized in Fig. 2. Social workers/case managers participated in interdisciplinary conferencing and worked on discharge planning and services for almost all patients; the greatest amount of time (mean minutes per week) was spent on these activities. A majority of the patients also received financial planning, community/in-house services, supportive counseling, and initial assessment. Only a minority of patients worked with their social worker/case manager on exploring peer or advocacy group options, receiving education (SCI materials, advance directives, community re-entry, or guardianship), or participating in classes led by social workers/case managers.
Figure 2.
Percent of patients receiving each of nine SW/CM interventions and mean minutes per week of the intervention for patients receiving it.
The SCIRehab Project team set minimum thresholds for reporting regression models that associated time spent on discipline-specific activities with patient and injury characteristics. A minimum of 70% of patients must have participated in an activity and the regression model for that activity must have reached a total R2 value of 0.20 or higher. The only SW/CM activities that met the 70% participation criterion (Table 2) were discharge planning/services and interdisciplinary conferences (in which social workers/case managers participated on the patient's behalf), but neither achieved an R2 > 0.20; and thus are reported here in detail. The R2 value for the model predicting time spent on discharge planning and services was 0.13, with the severity of illness (CSI) score being the strongest predictive variable.
Discussion
Data from the first year of data collection on the SCIRehab project provide descriptive information about the types of SW/CM services provided and time spent on these services. Taken as a whole, significant differences were seen in total hours and minutes per week among injury groups. As expected, the most time was spent with patients with C1–C4 AIS ABC, and unexpectedly, the least time was spent with patients in the C5–C8 AIS ABC injury group. The variation in the range of time spent across SW/CM activities is not surprising. Due to the structure and goals of inpatient rehabilitation SW/CM programs, we would expect the greatest amount of clinical time to be spent on assessment, discharge services and planning, financial planning, and interdisciplinary conferencing. We also would expect to see a range in the amount of time spent on these activities with differences across injury severity groups. We would expect that all patients in a rehabilitation center would receive at least some initial assessment and discharge planning and services. However, no SW/CM documentation was recorded for 26 of the 600 patients, which may explain the lack of discharge planning and services work with some patients. The initial patient assessment and some discharge planning may be performed during the acute care portion of the hospitalization before transfer to the rehabilitation service, and social workers/case managers may use information from these initial assessments as a baseline for rehabilitation care. Services delivered prior to rehabilitation admission are not included in the SCIRehab database. Thus, the data may suggest that initial assessment and discharge planning was not done for all patients when, in fact, they may have been completed prior to rehabilitation admission and brought forward (without repeating) for use in the rehabilitation center. Of the 68 patients who received no documented discharge planning and services, 42 were treated at one center where it is common to admit patients to a different level program and then later admit the patient to the acute SCI program. Only three patients had an LOS of less than 10 days and only 12 (including the three) had LOS <20 days. Of the 68 without documented discharge planning and services, over 90% of patients went home and none left against medical advice. No SW/CM documentation was recorded for 26 of the 600 patients, partially explains the lack of discharge planning and services in some patients.
Only 56% of patients had supportive counseling recorded (Table 2). It appears that SW/CM time in acute SCI rehabilitation focuses more highly on discharge issues. In all of the participating centers, psychology services were available to allow counseling issues to be addressed through other professional means.
Patients in injury group C1–C4 ABC present many case management challenges, and thus it is not surprising to find they consumed the greatest amount of SW/CM time overall and within the activities of financial planning and discharge planning and services. These patients often are ventilator dependent, and as such require much intervention to deal with adjustment issues and procurement of specialized placement, equipment, and supplies. Extensive family training, which may include ventilator management, resuscitation techniques, coordination of home care services, resource development, etc., also is needed. Discharge plans may change during the rehabilitation process as families realize the extensive requirements of caring for a patient who cannot be weaned from the ventilator. However, nursing home placement for patients requiring ventilator support has become more and more difficult, and in some states nursing homes will not admit these patients. Social workers/case managers may need to initiate transfer processes to nursing homes in other areas of the country known to accept patients with ventilator requirements. Alternatively, patients may return to the transferring acute care hospital, but this often requires risk-sharing negotiations in advance of the rehabilitation admission. Another alternative would be to seek other family members who could be trained in managing care for the patient at home. These explorations and negotiations, including meetings with family members and the treatment team, consume much SW/CM time. If these alternatives do not come to fruition, patients may remain in the rehabilitation hospital for long periods of time; ongoing discussions are required with hospital administrators regarding cost factors and continued exploration of placement options.
SCIRehab patients with AIS D level of injury had significantly more minutes per week spent on initial assessment, less time total hours and minutes per week on discharge planning and services and financial planning (total hours and minutes per week). The fewer number of total hours spent with patients with AIS D may be explained by shorter LOS for these patients (mean 36 days compared to 55 days for the sample as a whole). We hypothesize that clinicians realize the amount of time the patient will be in the rehabilitation facility and spread their education/counseling over the anticipated LOS. Patients with AIS D injuries typically return to their homes and accessibility issues are minimal. Although patients with AIS D may or may not qualify for social security or other benefits due to the incompleteness of their injury, returning to work also may be foreseen in the near future, which makes financial planning easier.
It is puzzling that patients with C5–C8 AIS A–C injuries received significantly fewer minutes per week on discharge planning and services than patients in the other injury categories. Whether patients with paraplegia had greater discharge planning and service needs than those with low tetraplegia and AIS D or they simply received more time is not known. For example, it might be that the greater independence of an individual with paraplegia creates greater need for discharge planning and services. On the other hand, it might be that the greater independence of patients with paraplegia may have allowed them to seek out more SW/CM intervention time while those with low tetraplegia were more at the mercy of scheduled time when the social worker/case manager meets with them. Of course, those with paraplegia and AIS D receiving more time than those with low tetraplegia may be a factor of a constant number of hours being spread over fewer weeks. These ad-hoc explanations will be explored in greater depth when the full SCIRehab sample is complete.
Less than 30% of SCIRehab patients participated in classes led by SW/CM; however, this may be more reflective of care practices at the centers and timing of the rehabilitation stay than of patient receipt of educational information. SCI education classes are conducted routinely within SCI centers; however, other disciplines, e.g. nursing and physical therapy, typically teach most of these classes. Social workers/case managers lead classes at some centers; at other centers, they do not. Additionally, at most sites, the classes are offered weekly with a rotating schedule for the teaching discipline. Thus, each patient can be expected to experience different classes led by different disciplines depending on the patient's LOS and the timing of the stay in the cycle with short-stay patients less likely to have their stay overlap with the class taught by the social worker/case manager.
It is of interest that only a minority (12% of patients) received information on peer advocacy from the social workers/case managers. During initial rehabilitation, a patient with acute SCI may not yet see the benefit of participating in peer advocacy or may still be in a phase of denial making these issues seem irrelevant. Peer advocacy also may be under-reported here as it is only peer activities recorded by the social workers/case managers; once the social workers/case managers refers the patient to peer advocacy, interactions would no longer be under SW/CM oversight.
We conducted regression analyses to examine patient, injury, and clinician characteristics associated with time spent in SW/CM interventions. However, the patient and injury characteristics that we examined explain very little of the variance we see in time spent on SW/CM interventions, whether overall or in specific activities. Typical PBE analytical strategy does not include center-specific effects because it is thought that center effects may result from underlying differences in patient, injury, or clinician characteristics among centers. We acknowledge, however, that there may be additional center-specific factors that may influence the amount of time spent on SW/CM activities. For example, this study did not measure patient and family dynamics or quantify the level of family support available to the patients. When center identifiers were allowed to enter the regression models in which at least 70% of patients participated (discharge planning/services and interdisciplinary conferences), the explanatory power increased from 0.13 to 0.22 for discharge planning/services and from 0.03 to 0.16 for interdisciplinary conferencing. This minimal increase suggests that center effects add little explanatory power and that the significant variation in time spent on SW/CM activities should prove useful in the eventual effort to correlate interventions with key patient outcomes.
Study limitations
The six SCIRehab sites were selected to participate based on their willingness, geographic diversity, and expertise in treatment of patients with SCI, and offer variation in setting, care delivery patterns, and patient clinical and demographic characteristics. However, they are not a probability sample of the rehabilitation facilities that provide care for patients with SCI in the United States, and time reported overall or on specific activities may not be generalizable to all rehabilitation centers.
Data are only as complete as the data entered by each social workers/case managers; some intervention time may not have been included. We offer this as the most plausible explanation for why all patients do not have time recorded for work on discharge planning and services. Additionally, this project does not include any interventions that occurred in less than 5-minute increments and certainly social workers/case managers may provide much meaningful assistance in brief intervals – e.g. making a phone call to confirm an arrangement or ask for one specific piece of information. Social workers/case managers in particular have to fit much of what they do into available (and often small) periods of time. Unlike therapy disciplines, SW/CM do not have scheduled blocks of time with each patient.
Future research directions
It will be important to study the relationship of services received and time spent on various activities during inpatient SCI rehabilitation to various rehabilitation outcomes.
Conclusion
These descriptive study data may help in resource planning and benchmarking on both the hospital and the individual patient levels, and will be helpful in planning studies on the impact of SW/CM intervention on SCI outcomes.
Acknowledgements
The contents of this paper were developed under grants from the National Institute on Disability and Rehabilitation Research, Office of Rehabilitative Services, US Department of Education, to Craig Hospital (grant no.s H133A060103 and H133N060005), Carolinas Rehabilitation, Rehabilitation Institute of Chicago (grant no. H133N060014), and Shepherd Center (grant no. H133N060009). The opinions contained in this publication are those of the grantees and do not necessarily reflect those of the US Department of Education.
References
- 1.Zatzick D, Roy-Byrne P, Russo J, Rivara F, Droesch R, Wagner A, et al. A randomized effectiveness trial of stepped collaborative care for acutely injured trauma survivors. Arch Gen Psychiatry 2004;61(1):498–506 [DOI] [PubMed] [Google Scholar]
- 2.Douglas S, Daily B, Kelley C, O'Toole E, Montenegro H. Impact of a disease management program upon caregivers of chronically ill patients. Chest 2005;128(6):3925–36 [DOI] [PubMed] [Google Scholar]
- 3.American Hospital Association Council on Patient Services Case management: an aid to quality and continuity of care. Chicago, IL: American Hospital Association; 1987 [Google Scholar]
- 4.Glidden M. Spinal cord injury and case management. Top Spinal Cord Inj Rehabil 1999;4(4):16–23 [Google Scholar]
- 5.Gassaway J, Whiteneck G, Dijkers M. SCIRehab: clinical taxonomy development and application in spinal cord injury rehabilitation research. J Spinal Cord Med 2009;32(3):260–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Whiteneck G, Dijkers M, Gassaway J, Jha A. SCIRehab: new approach to study the content and outcomes of spinal cord injury rehabilitation. J Spinal Cord Med 2009;32(3):251–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abeyta N, Freeman E, Primack D, Hammond FM, Dragon C, Harmon A, et al. SCIRehab: the social work/case management taxonomy. J Spinal Cord Med 2009;32(3):335–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whiteneck G, Gassaway J, Dijkers M, Charlifue S, Backus D, Chen D, et al. SCIRehab: inpatient treatment time across disciplines in spinal cord injury rehabilitation: therapy time across disciplines. J Spinal Cord Med 2011;34(2):135–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Horn S, Gassaway J. Practice-based evidence study design for comparative effectiveness research. Med Care 2007;45Suppl 2:S50–7 [DOI] [PubMed] [Google Scholar]
- 10.DeJong G, Hsieh C, Gassaway J, Horn S, Smout R, Putman K, et al. Characterizing rehabilitation services for patients with knee and hip replacement in skilled nursing and inpatient rehabilitation facilities. Arch Phys Med Rehabil 2009;90(8):1284–96 [DOI] [PubMed] [Google Scholar]
- 11.Gassaway J, Horn S, DeJong G, Smout R, Clark C, James R. Applying the clinical practice improvement approach to stroke rehabilitation: Methods used and baseline results. Arch Phys Med Rehabil 2005;8612 Suppl 2:S16–33 [DOI] [PubMed] [Google Scholar]
- 12.Horn S, DeJong G, Ryser D, Veazie P, Teraoka J. Another look at observational studies in rehabilitation research: Going beyond the holy grail of the randomized controlled trial. Arch Phys Med Rehabil 2005;8612 Suppl 2:S8–15 [DOI] [PubMed] [Google Scholar]
- 13.Marino R. ed. Reference manual for the international standards for neurological classification of spinal cord injury. Chicago, IL: American Spinal Injury Association; 2003 [Google Scholar]
- 14.Horn S, Sharkey S, Rimmasch H. Clinical practice improvement: a methodology to improve quality and decrease cost in health care. Oncol Issues 1997;12(1):16–20 [Google Scholar]
- 15.Horn S, Sharkey P, Buckle J, Backofen J, Averill R, Horn R. The relationship between severity of illness and hospital length of stay and mortality. Med Care 1991;29(4):305–17 [DOI] [PubMed] [Google Scholar]
- 16.Ryser D, Egger M, Horn S, Handrahan D, Ghandi P, Bigler E. Measuring medical complexity during inpatient rehabilitation following traumatic brain injury. Arch Phys Med Rehabil 2005;86(6):1108–17 [DOI] [PubMed] [Google Scholar]
- 17.Averill R, McGuire T, Manning B, Fowler D, Horn S, Dickson P, et al. A study of the relationship between severity of illness and hospital cost in New Jersey hospitals. Health Serv Res 1992;27(5):587–617 [PMC free article] [PubMed] [Google Scholar]
- 18.Clemmer T, Spuhler V, Oniki T, Horn S. Results of a collaborative quality improvement program on outcomes and costs in a tertiary critical care unit. Crit Care Med 1999;27(9):1768–74 [DOI] [PubMed] [Google Scholar]
- 19.Fiedler R, Granger C. Functional Independence Measure: a measurement of disability and medical rehabilitation. In: Chino N, Melvin J. (eds.) Functional evaluation of stroke patients. Tokyo, Japan: Springer-Verlag; 1996. p. 75–92 [Google Scholar]
- 20.Fiedler R, Granger C, Russell C. UDS(MR)SM: follow-up data on patients discharged in 1994–1996. Uniform Data System for Medical Rehabilitation. Am J Phys Med Rehabil 2000;79(2):184–92 [DOI] [PubMed] [Google Scholar]
- 21.Stevens J.2003. Partial and semipartial correlations. Available from: www.uoregon.edu/~stevensj/MRA/partial.pdf. (accessed 2010 Feb 10)
- 22.Stevens J. Intermediate statistics: a modern approach. 2nd ed. Mahwah, NJ: Lawrence Erlbaum Associates, Inc.; 1999 [Google Scholar]