Abstract
Background
Rehabilitation psychologists are integral members of spinal cord injury (SCI) rehabilitation teams.
Objective
To describe specific information regarding types and intensity of treatments delivered by rehabilitation psychologists to patients with various levels of SCI.
Methods
Utilizing a taxonomy of psychological interventions as a framework, rehabilitation psychologists documented time spent on specific psychology interventions for each interaction they had with 600 patients with traumatic SCI at 6 inpatient SCI rehabilitation centers. Associations of patient and injury characteristics with time spent on various psychological interventions were examined using ordinary least squares stepwise regression models.
Results
Psychologists focus the majority of the time they spend with patients with SCI on psychotherapeutic interventions of processing emotions, emotional adjustment, and family coping, while educational efforts focus mostly on coping and adjusting to the new injury. There was wide variation in the amount of time spent on psychotherapeutic and psychoeducational interventions; patient, injury, and clinician characteristics explained little of the variation in time spent.
Conclusions
Variations observed in psychological treatment delivery mirror real-world human complexity and clinical experience; they are not explained well by patient and injury characteristics and set the stage for future analyses to associate treatments with outcomes.
Keywords: Spinal cord injuries, Rehabilitation, Paraplegia, Tetraplegia, Health services research, Psychology
Introduction
Rehabilitation psychology (RP) contributes ‘psychological knowledge and skills on behalf of individuals with disabilities and chronic health conditions in order to maximize health and welfare, independence and choice, functional abilities and social role participation across the life span’ (p. 235).1 Interventions provided by rehabilitation psychologists encompass a system that includes biological, psychological, social, environmental, and political considerations and are designed to maximize a person's achievement of rehabilitation goals.2,3 Rehabilitation psychologists first assess a person's strengths and weaknesses in cognition, mood, and behavior. Next, they evaluate how these strengths and weaknesses may impact the person's ability to benefit from the rehabilitation effort and integrate successfully back into the community. Clinical interventions delivered in individual, group, and/or family formats; consultation with members of the interdisciplinary team; and advocacy on behalf of the individual also are important aspects of RP. Both the Commission on Accreditation of Rehabilitation Facilities and the World Health Organization have stressed the importance and the value of RP for inpatient rehabilitation settings.2 While psychological support and education generally are accepted as essential aspects of the rehabilitation of persons with spinal cord injury (SCI), consensus regarding the critical components of these interventions and their potential associations with positive patient outcomes remains elusive. In order to better define these critical components and to ultimately study the effectiveness and efficiency of inpatient rehabilitation treatments, detailed observations of psychological interventions are essential. In the past, some have described the rehabilitation process as a ‘black box’ of unspecified interventions.4,5 Beginning to open this ‘black box’ by describing current intervention practices will be a first step in improving the quality of care and positive outcomes for patients with SCI.
This paper aims at describing how psychological intervention time was spent and the variation in the amount of time spent among patients with differing levels and completeness of injury. Patient, injury, and clinician characteristics that are associated with time spent on common psychology activities also are discussed.
Methods
The SCIRehab project is a 5-year collaboration of six rehabilitation centers that is recording and analyzing the details of the SCI inpatient rehabilitation process for approximately 1400 patients. An early outcome of the SCIRehab project was the development and publication of a multi-disciplinary rehabilitation treatments taxonomy for patients with SCI; the psychology taxonomy6 was one of seven discipline-specific taxonomies created and contained details about psychological services provided in the acute rehabilitation setting.
The first paper in this journal series7 describes the SCIRehab project's study design such as inclusion criteria, data sources, and the analysis plan, as well as use of the practice-based evidence (PBE) research methodology.4,5,8–11 Here, we provide only a summary. The SCIRehab team included psychologists and representatives of all other rehabilitation clinical disciplines from six inpatient rehabilitation facilities: Craig Hospital, Englewood, CO; Shepherd Center, Atlanta, GA; Rehabilitation Institute of Chicago, Chicago, IL; Carolinas Rehabilitation, Charlotte, NC; the Mount Sinai Medical Center, New York, NY; and National Rehabilitation Hospital, Washington, DC. Institutional Review Board (IRB) approval was obtained at each center. Patients who were 12 years of age or older, gave (or whose parent/guardian gave) informed consent, and were admitted to the facility's SCI unit for initial rehabilitation following traumatic SCI were enrolled.
Patient/injury and clinician data
Patient and injury data were collected from patient medical records by trained data abstractors. The International Standards of Neurological Classification of SCI (ISNCSCI)12 and its American Spinal Injury Association Impairment Scale (AIS) were used to describe the motor level and completeness of injury; patients were placed into one of four injury groups. Patients with AIS grade D were grouped together regardless of injury level. Patients with AIS class A, B, and C were grouped together and separated by motor level to create the remaining three categories: high tetraplegia (C1–C4), low tetraplegia (C5–C8), and paraplegia (T1 and below). These injury categories were selected because they were each large enough for analysis and created groupings thought to have relatively homogenous functional ability within groups and clear differences between the groups. The Comprehensive Severity Index (CSI®) was used to obtain a measure of medical severity of illness at the time of admission to the rehabilitation unit and over time during rehabilitation. Higher CSI scores are indicative of greater severity based on the abnormality of diagnosis-specific symptoms.13–17 The Functional Independence Measure (FIM®) was used to describe a patient's independence in specific motor and cognitive abilities at rehabilitation admission and discharge.18,19 Psychologists who documented treatment for the SCIRehab project completed a clinician profile that included their years of SCI rehabilitation experience at the start of the project.
Psychology treatment data
Psychologists at each project site input details about each interaction with each study patient into handheld personal digital assistants (PDA; Hewlett Packard PDA hx2490b, Palo Alto, CA) containing a modular custom application incorporating the psychology activities taxonomy (PointSync Pro version 2.0, MobileDataforce, Boise, ID, USA), which has been described previously.6 The six primary types of psychology treatments provided in an SCI setting include four interventions that are in direct contact with patients (initial assessment, psychoeducational interventions, psychotherapeutic interventions, and SCI classes led by a psychologist) and two interventions that are conducted on a patient's behalf (time psychologists spend consulting with other providers, community resource contacts, and/or family members and time spent participating in interdisciplinary conferencing that addresses patients goals and needs). Sub-categories included in these six interventions are provided in Table 1.
Table 1.
Psychology interventions and sub-interventions: percent patients receiving, percent sessions in which interventions included, percent of sessions for intervention that includes sub-intervention
| Intervention | Sub-intervention | % of 600 patients who received | % of all sessions that included the intervention/sub-intervention | % of sessions for the intervention that included the sub-intervention |
|---|---|---|---|---|
| Formal assessment | 52.0 | 9.5 | — | |
| Mood | 45.5 | 7.7 | 71.3 | |
| Psychosocial/education/employment/support systems | 41.5 | 5.1 | 47.2 | |
| Psychotropic medications | 9.0 | 1.1 | 10.1 | |
| Substance use/abuse | 19.7 | 1.5 | 14.3 | |
| Pain | 29.7 | 3.2 | 29.9 | |
| Psychiatric treatment | 10.2 | 0.8 | 7.3 | |
| Coping style | 31.3 | 3.4 | 31.4 | |
| Strengths to assist rehab process | 30.3 | 2.9 | 27.3 | |
| Patients concerns related to hospital/injury | 39.0 | 5.8 | 54.0 | |
| Cognition | 37.2 | 5.7 | 52.9 | |
| Psychotherapeutic intervention | 91.3 | 49.3 | — | |
| Desensitization to negative stigmas | 16.8 | 1.9 | 3.4 | |
| Processing emotions | 71.5 | 26.0 | 46.9 | |
| Emotional adjustment | 81.5 | 30.8 | 55.5 | |
| Circumstances associated with injury | 81.5 | 11.3 | 20.3 | |
| Family functioning or coping | 61.0 | 22.0 | 39.7 | |
| Building rapport/engagement | 26.7 | 4.4 | 8.0 | |
| Positive reinforcement | 42.8 | 18.8 | 33.9 | |
| Pain management | 19.0 | 3.3 | 6.0 | |
| Locus of control issues | 34.3 | 6.0 | 10.9 | |
| Peer mentoring | 12.7 | 2.1 | 3.7 | |
| Psychoeducational intervention | 82.7 | 29.0 | — | |
| Goal setting | 30.7 | 8.2 | 25.1 | |
| Substance use/abuse | 35.8 | 3.1 | 9.3 | |
| Coping with and adjusting to SCI | 68.7 | 22.5 | 68.9 | |
| Wellness and life style modification | 33.8 | 8.6 | 26.4 | |
| Relationship issues | 40.7 | 6.9 | 21.0 | |
| Sexuality post injury | 45.0 | 5.5 | 16.9 | |
| Problem-solving/decision-making skills | 42.7 | 8.5 | 26.0 | |
| Self-advocacy/assertiveness | 44.7 | 7.0 | 21.4 | |
| Pain management | 14.2 | 2.0 | 6.1 | |
| Classes led by psychologist* | 21.8 | 2.0 | — | |
| Consultation (>10 minutes) on behalf of patient | 30.2 | 10.3 | — | |
| With physician | 30.7 | 8.2 | 25.1 | |
| With team members | 25.7 | 8.6 | 73.7 | |
| With family | 13.2 | 3.1 | 26.5 | |
| With community resource person | 1.8 | 0.2 | 1.4 | |
| With other health professional | 2.8 | 0.3 | 2.6 | |
| Interdisciplinary conferencing on behalf of patient*,† | 94.0 | — | — |
*No additional data (sub-topics) collected.
†Time spent by psychologist.
In addition to the interventions described in Table 1, which includes formal patient assessment, PDA documentation also included a modified version of the Brief Symptom Inventory-18 (BSI-18).20,21 The modified BSI, a self-report inventory that uses a five-point rating scale to capture anxiety, depression, and somatic symptoms, was added because there was no consistent measure to document anxiety and depression assessments at the six SCIRehab sites. The SCIRehab project team selected the six anxiety and six depression BSI-18 items, but opted not to use the six somatic items, because somatic symptoms in patients with SCI may reflect physiologic effects of the SCI itself rather than the patient's emotional status.22–25 The modified BSI-18 was scored by assigning a value of 0–4 for each item response and then summing the item raw scores for each dimension (anxiety and depression). In cases where data were missing for up to two items per dimension, the rounded mean score of the non-missing items was imputed. Finally, the raw scores for each dimension were converted to T scores and compared to norms derived for a sample with oncological disease reported by Derogatis,20 which were considered more appropriate than the community norms derived for a sample of healthy individuals, given that both SCI and oncology populations deal with the uncertainty of medical outcomes and somatic issues likely to elicit similar emotional reactions.
Each psychologist was trained and then tested quarterly on use of the PDA documentation system. Daily entries were compared by the site SCIRehab coordinator with patient schedules or billing records to ensure that all psychology sessions were included.7 The date/time of each psychology session, the number of minutes spent on intervention activities performed in the session, and activity-specific details were entered into the PDA. Activity minutes were combined to equal the approximate duration of the full session.
Data analysis
Analyses reported here include patients enrolled in the SCIRehab project's first year of enrollment. Our primary means of quantifying the intensity of psychology intervention was the total number of hours spent on specific activities for the full sample and for each injury group separately during the inpatient rehabilitation stay. Longer lengths of stay allow more time to provide services and to build relationships necessary for more in-depth psychological intervention. As a secondary measure of intensity, we calculated the average minutes per week spent on each activity. Contingency tables/chi-square tests and analysis of variance were used to test differences across injury groups for categorical and continuous variables, respectively. A P value less than 0.05 was considered statistically significant.
Patient and injury characteristics associated with time spent on those psychology activities in which at least 70% of patients participated were examined using ordinary least squares stepwise regression models. The strength of the model is determined by the R2 value, which indicates the amount of variation explained by the significant variables. Type II semi-partial correlation coefficients allowed for comparison of the unique contribution of each predictor variable after controlling for all other variables in the model.26,27 Parameter estimates indicate the direction and strength of the association between each independent variable with the dependent variable.
Predictor variables used included gender, marital status, racial/ethnic group, traumatic SCI etiology, body mass index (BMI), English-speaking status, third-party payer, pre-injury occupational status, severity of illness (CSI) score, age at the time of injury, admission FIM motor and cognitive scores, experience level of the clinician, and injury grouping. The same predictor variables were used to determine if patient characteristics were associated with completion of the modified BSI-18. The only regression analysis reported in this paper is for psychoeducational interventions as this is the only model in which at least 70% of patients participated and that had an R2 value of greater than 0.20.
Results
Six hundred patients with traumatic SCI were enrolled in the SCIRehab project during the first year of data collection at the six rehabilitation study centers. Details of patient and injury characteristics are presented for the sample as a whole and for each of the four injury groups separately in the first article in this SCIRehab series7 (Table 1). The sample was 81% male, 65% white (22% black), 38% married, most were not obese (82% had a BMI of <30), and 65% were employed at the time of injury. Vehicular accidents were the most common cause of injury (49%), falls were the next most common (23%), followed by etiologies of sports (12%) and violence (11%); the remaining 5% were classified as other. The mean rehabilitation length of stay (LOS) was 55 days (range 2–259, standard deviation (SD) 37, median 43). The mean total admission FIM score was 53 (motor score of 24 and cognitive score of 29), and a mean of 32 days elapsed from the time of injury to the time of rehabilitation admission.
Nearly all patients (596/600 or 99%) enrolled in the SCIRehab project during the first year received psychological services during their inpatient rehabilitation. Psychologists documented details of treatment provided during 8748 psychology sessions for these 596 patients (average number of sessions per patient = 14.7). Most treatment was conducted via one-on-one interactions with patients (6517 sessions), and about 16% of treatment time was delivered in a group (including classes led by a psychologist) setting.
Most patients received psychotherapeutic and/or psychoeducational interventions during their rehabilitation stay (Table 1). The category of psychoeducational interventions included nine topic areas; the topic that consumed the most psychology treatment time was ‘coping with and adjusting to SCI’. Of the 600 patients, 69% received education about this topic, which was addressed in 69% of sessions in which any psychoeducational intervention was provided. The most common of the 10 psychotherapeutic intervention topics was ‘emotional adjustment’; it was addressed with 82% of patients and in 56% of sessions that involved any psychotherapeutic intervention. The only topic that was included in the taxonomy in both the psychoeducational and the psychotherapeutic intervention categories was ‘pain management’. It was addressed less frequently – 398 sessions with 142 patients. Of all sessions that included any psychotherapeutic or psychoeducational intervention, only 17% included discussions of pain management.
SCIRehab patients received a mean total of 10.6 hours (range 0–82, SD 10.5, median 7.5) of psychology intervention. Table 2 presents time spent within specific psychology activities for the full sample and for the four injury groups separately, expressed as total hours over the full rehabilitation stay and as an average number of minutes per week. Significant differences among the four groups were seen in the amount of time spent in each activity. Among the psychology activities documented by clinicians, psychotherapeutic interventions and psychoeducational interventions comprised the majority of time spent.
Table 2.
Psychology activities: percent patients receiving each type of service, mean total hours, and mean minutes per week (SD)*
| Full SCIRehab sample n = 600 | C1–C4 AIS A, B, C n = 132 | C5–C8 AIS A, B, C n = 151 | Para AIS A, B, C n = 223 | AIS D n = 94 | |
|---|---|---|---|---|---|
| Any psychology intervention (%) | 99 | 100 | 99 | 100 | 97 |
| Total hours† | 10.6 (10.5) | 15.5 (12.5) | 12.7 (13.0) | 8.3 (6.4) | 5.5 (6.6) |
| Minutes/week† | 77.4 (42.2) | 84.3 (40.8) | 79.8 (43.0) | 79.2 (41.2) | 59.8 (40.9) |
| Psychotherapeutic intervention (%) | 91 | 98 | 96 | 92 | 72 |
| Total hours† | 3.9 (5.9) | 5.9 (6.6) | 5.3 (8.6) | 2.8 (3.0) | 1.5 (2.1) |
| Minutes/week† | 27.6 (26.6) | 33.0 (27) | 31.3 (29.1) | 26.3 (23.9) | 17.3 (24.8) |
| Psychoeducational intervention (%) | 82 | 87 | 87 | 83 | 63 |
| Total hours† | 2.9 (3.2) | 3.8 (3.6) | 3.6 (3.8) | 2.7 (2.6) | 1.4 (2.0) |
| Minutes/week† | 24.9 (24.8) | 23.8 (20.7) | 26.3 (24.6) | 28.7 (27.6) | 15.0 (20.8) |
| Interdisciplinary conferencing (%) | 94 | 98 | 95 | 95 | 83 |
| Total hours† | 1.9 (1.6) | 2.7 (2.0) | 2.1 (1.5) | 1.5 (1.4) | 1.2 (1.4) |
| Minutes/week | 13.3 (7.1) | 14.0 (5.6) | 13.3 (6.5) | 13.5 (7.5) | 12.2 (8.7) |
| Formal Assessment (%) | 52 | 56 | 46 | 50 | 62 |
| Total hours† | 0.9 (2.0) | 1.6 (3.0) | 0.6 (1.3) | 0.6 (1.2) | 1.0 (2.4) |
| Minutes/week† | 6.1 (10.4) | 7.2 (11.6) | 3.7 (7.2) | 5.2 (8.3) | 10.9 (14.7) |
| Consultation (%) | 30 | 44 | 32 | 27 | 16 |
| Total hours† | 0.6 (1.9) | 1.2 (2.4) | 0.7 (2.2) | 0.5 (1.6) | 0.2 (0.5) |
| Minutes/week† | 3.0 (8.4) | 4.6 (9.6) | 3.0 (8.8) | 2.9 (8.8) | 1.2 (3.7) |
| Classes (%) | 22 | 24 | 27 | 20 | 15 |
| Total hours | 0.3 (0.6) | 0.3 (0.6) | 0.4 (0.7) | 0.2 (0.5) | 0.3 (0.6) |
| Minutes/week | 2.3 (6.1) | 1.7 (4.1) | 2.3 (5.1) | 2.5 (6.9) | 2.9 (7.8) |
*Hours and minutes per week are averages over all 600 patients, not just based on those who did receive one or more sessions of a particular activity.
†Statistically significant differences in mean total hours or minutes per week among groups.
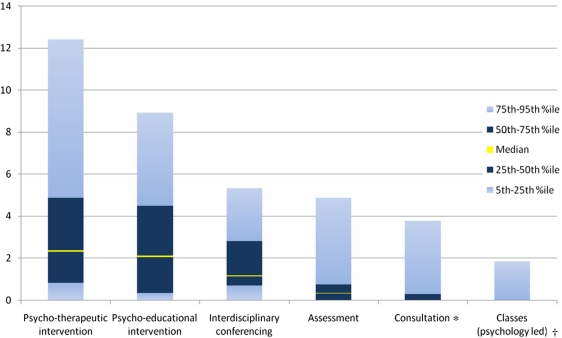
Fig. 1 depicts the wide variation in total hours spent on each of the psychology activities for the entire SCIRehab sample. The interquartile range (IQR) for psychotherapeutic interventions was 0.8–4.8 hours (median 2.3 hours) and for psychoeducational interventions was 0.3–4.5 hours (median 2.1 hours). Similar patterns in variation were seen when we examined each injury group separately. At least one formal assessment was documented for 52% of patients and the IQR was 0–0.8 hours (median 0.3 hours).
Figure 1.
Variation in time spent (total hours) on psychology activities.
Notes: *30% of sample, median = 0. †22% of sample, all above 75th percentile.
We examined the association of patient/injury characteristics and clinician experience with time spent on specific psychology interventions in which at least 70% of patients participated; only psychoeducational intervention had a total R2 value >0.20 and, thus, is reported here (Table 3). The regression model for psychoeducational interventions explains 24% of the variation in time spent (R2 = 0.24). The parameter estimate for the independent variable of clinician experience is 1.26, indicating that clinicians with more experience provide an average of approximately 1¼ minutes per week more of psychoeducational interventions than clinicians with less experience, and the semi-partial R2 indicates that this is the largest explanatory variable (unique contribution is 10% of the total R2 after controlling for other variables in the model). The parameter estimate for the severity of illness score is −0.20, which indicates that for each additional severity point, 0.20 fewer minutes were spent. Therefore, a patient with a severity score of 100 would be predicted to receive 20 fewer minutes per week of psychoeducational interventions (parameter estimate of 0.20 × 100) than a patient with the lowest severity score of 0. Other patient/injury characteristics associated with more time (positive parameter estimate) included injury group Para ABC, and English as primary language. Independent variables associated with less time (in addition to higher severity of illness score) included injury group AIS D, higher admission FIM cognitive score, medical/surgical etiology of injury, and Medicaid as the payer.
Table 3.
Patient and injury characteristics associated with time (minutes per week) in psychology activities*,†
| Psychoeducational interventions |
||
|---|---|---|
| Total R2 | 0.24 |
|
| Independent variable | Parameter estimate | Type II semi-partial R2 |
| Injury group: AIS D | −9.06 | 0.01 |
| Injury group: Para ABC | 4.74 | 0.01 |
| Clinician experience | 1.26 | 0.10 |
| Language – English | 15.50 | 0.02 |
| Admission FIM cognitive score | −0.54 | 0.01 |
| Severity of illness score (CSI) | −0.20 | 0.05 |
| Traumatic etiology – medical/surgical complication | −13.85 | 0.01 |
| Payer – Medicaid | −5.31 | 0.01 |
*Psychology activities included in table only if more than 70% of patients participated and the total R2 > 0.20.
†Independent variables allowed into models: age at injury, male, married, race – white, race – black, race – Hispanic, race – other, admission FIM motor score, admission FIM cognitive score, severity of illness score (CSI), injury group: C1–C4 ABC, injury group: C5–C8 ABC, injury group: Para ABC, injury group: AIS D, clinician experience, traumatic etiology – vehicular, traumatic etiology – violence, traumatic etiology – falls, traumatic etiology – sports, traumatic etiology – medical/surgical complication, traumatic etiology – other, work-related injury, number of days from trauma to rehabilitation admission, BMI >40, BMI 30–40, BMI < 30, language – English, language – no English, language – English sufficient for understanding, payer – Medicare, payer – worker compensation, payer – private, payer – Medicaid, employment status at the time of injury – employed, employment status at the time of injury – student, employment status at the time of injury – retired, employment status at the time of injury – unemployed, employment status at the time of injury – other, ventilator use rehabilitation admission.
The modified BSI-18 was administered to 60% of SCIRehab patients; little variation in T scores was evident among the injury groups (Table 4). Logistical regression analysis failed to reveal an association between patient or injury characteristics and whether clinicians administered the modified BSI-18. For those patients who had BSI data available, higher anxiety and depression scores were correlated with more psychoeducational and psychotherapeutic interventions for patients in the two tetraplegia injury groups. Additionally, higher depression scores in patients with paraplegia correlated with greater amounts of time spent in any psychology interventions. There was no correlation between amount of time spent in psychology intervention and BSI scores for patients in the AIS D injury group.
Table 4.
Modified BSI-18 completion rates and anxiety and depression scale T scores (mean and SD)
| Full SCIRehab sample (n = 600) | C1–C4 AIS A, B, C (n = 132) | C5–C8 AIS A, B, C (n = 151) | Para AIS A, B, C (n = 223) | AIS D (n = 94) | |
|---|---|---|---|---|---|
| Completion (%) | 60 | 60 | 65 | 57 | 61 |
| Anxiety T scores | 50.8 (10.3) | 52.2 (10.4) | 51.8 (10.5) | 49.2 (9.3) | 51.0 (11.8) |
| Depression T scores | 53.0 (9.6) | 53.7 (10.6) | 53.1 (8.8) | 52.3 (9.4) | 53.3 (9.9) |
Discussion
The first year of data collection on the SCIRehab project yielded important descriptive information regarding the frequency with which various psychological interventions are provided to persons with SCI during inpatient rehabilitation. The variation found in the patient, clinician, and intervention variables mirrors the reality of clinical practice and reflects the complexity of human beings who sustain SCI and the professionals who treat them. Some of the differences observed were predictable, while others suggest new hypotheses that can be analyzed as the project progresses. The data support the importance of collaboration between research and clinical practice that ultimately strengthens our knowledge base and confirms or challenges the clinician's ‘hunch’.
Assessment of patients' psychological, cognitive, and psychosocial concerns and needs is a standard aspect of clinical care within SCI rehabilitation. It is, thus, somewhat counterintuitive that only 52% of the initial 600 patients in this study had formal assessment interventions documented by treating psychologists, while the vast majority had psychoeducational and psychotherapeutic interventions documented (Table 1). The lower frequency of assessment (as compared to psychotherapeutic and psychoeducational interventions) is most likely a reflection of the timing of psychological assessment and admission to inpatient rehabilitation. SCI rehabilitation psychologists at several SCIRehab sites were involved in assessment and treatment of newly injured patients during their acute hospitalization prior to transfer to the rehabilitation unit. Because this assessment occurred early in the continuum of care following the SCI and before rehabilitation admission, it was not captured by data collection efforts in the current study.
The modified BSI-18 (to assess anxiety and depression) was included as a separate PDA documentation item, which was to be completed once during a patient's rehabilitation stay. It was envisioned as a standard part of the SCIRehab data collection process by psychologists even though a basic tenet of PBE methodology is to capture data about what is being done in standard clinical practice rather than to introduce new practices or interventions as part of the study. Clinicians were encouraged to administer the modified BSI-18 to all patients but also to use clinical judgment to determine if administration of the measure was not appropriate in certain circumstances. This may explain why BSI data are not available on some patients and why regression modeling failed to identify meaningful associations between patient and injury characteristics and the administration of the modified BSI-18.
A high percentage of patients received psychotherapeutic intervention that involved ‘processing emotions’ and/or ‘emotional adjustment’. While these two sub-topics sound similar, they have unique meanings in the psychological treatment of persons with SCI. ‘Processing emotions’ is aimed at the grieving process and involves validation and normalization of the patient's feelings of anger, sadness, anxiety, depression, etc. In contrast, ‘emotional adjustment’ includes discussions about how adjustment to the disability and/or use of coping strategies is progressing.
‘Pain management’ was recorded as being addressed with less than 20% of patients. However, it is possible that pain management was addressed indirectly through psychotherapeutic interventions focused on emotions (e.g. anxiety), which can interfere with effective coping and management of pain. Similarly, education that focuses on teaching the patient about adjustment to disability may indirectly help the patient cope with SCI-related pain. It also is important to note that pain management strategies addressed didactically in lecture or class format were recorded elsewhere and would be included in the ‘classes’ activity in Tables 1 and 2.
The only robust regression model (R2 > 0.20) that associated patient and injury characteristics with variation in time spent was for psychoeducational interventions. As might be expected, patients in the AIS D injury group received fewer minutes per week of psychoeducational intervention. This likely reflected, in part, their improving neurological status during rehabilitation and clinicians' assumption of decreased need for educational interventions that focused on preparation for long-term disability. Additionally, patients in this injury group may be buoyed psychologically by physical improvement and expectations for ongoing gains and, consequently, less interested in intensive psychoeducation as a means of support during rehabilitation. While patients with AIS D injuries and the clinicians treating them may assume a lesser need for psychoeducational intervention during inpatient rehabilitation, research indicating a higher risk of suicide among patients with incomplete paraplegia28 may challenge the validity of these assumptions.
The observed association between more clinician experience and increased number of minutes of psychoeducational interventions delivered to patients is not surprising. More experienced clinicians presumably have gained more knowledge about SCI-specific topics through professional education, as well as valuable practical information from their previous patients, thus resulting in a more robust clinical ‘toolbox’ with which to educate newly injured patients.
We conducted regression analyses to examine patient and injury characteristics associated with time spent in specific activities. Typical PBE analytic strategy does not include center-specific effects because it is thought that center effects may result from underlying differences in patient, injury, or clinician characteristics among the centers. Thus, centers were not entered into these models. However, we acknowledge that additional center-specific factors may influence the amount of time spent on specific areas of psychological services. And, indeed, when centers were allowed to enter the regression model reported here (time spent in psychoeducational interventions), the explanatory power increased by 14%. This increase suggests that focusing on patient and injury characteristics is most helpful in explaining time spent in psychology work, that center effects add some additional explanatory power, and that the significant variation in time spent on psychology activities should prove useful in the eventual effort to correlate interventions with key patient outcomes.
Significant variations in total number of hours and minutes per week of psychological interventions were observed when the four level of injury groups were compared (Table 2). Patients with higher levels of injury, and thus more severe disability, received more time in inpatient rehabilitation presumably because of the complexity of their medical care, more extensive educational needs, and larger number of skills needed to maximize functional independence. We acknowledge that longer LOS provides greater opportunity to provide psychological services. It also provides for the opportunity to build relationships necessary for more in-depth psychological intervention. Thus, we used total hours of time spent in psychological interventions as our primary measure of intensity but also calculated the mean minutes per week spent on each psychological intervention to remove the influence of LOS. The variation we found in both total hours and calculated minutes per week likely reflects practice differences between clinical sites as well as clinician-specific practice differences within sites.
Study limitations
SCIRehab facilities offer variation in setting, care delivery patterns, and patient clinical and demographic characteristics and were selected to participate based on their willingness, geographic diversity, and expertise in treatment of patients with SCI. Thus, these centers are not a probability sample of the rehabilitation facilities that provide care for patients with SCI in the United States and information reported on specific activities may not be generalizable to all rehabilitation centers.
Study data are only as complete as the data entered by each psychologist for each patient interaction. Study coordinators at each project site compared project documentation with billing records and patient schedules to ensure that documentation was as complete as possible. Despite these efforts, it is possible that some psychology intervention time may not have been included.
Conclusion
The large variations in time spent on selected psychological interventions observed among and within injury-level groups, which mirror real-world human complexity and clinical experience, are critical to the success of PBE study. It is anticipated that the large variations observed will allow more robust analysis of correlations between the various patient, clinician, and treatment variables and the primary outcome measures of the SCIRehab project, such as community participation, pain management, and perceived quality of life, as the project begins to open the ‘black box’ of unspecified interventions in the rehabilitation process.
Acknowledgements
The contents of this paper were developed under grants from the National Institute on Disability and Rehabilitation Research, Office of Rehabilitative Services, US Department of Education, to Craig Hospital (grant #H133A060103 and #H133N060005), National Rehabilitation Hospital (grant number H133N060028), Rehabilitation Institute of Chicago (grant #H133N060014), Shepherd Center (grant #H133N060009), and Carolinas Rehabilitation. The opinions contained in this publication are those of the grantees and do not necessarily reflect those of the US Department of Education.
References
- 1.Scherer M, Banks M, Blair K, Bost R, Hough S, Kurylo M, et al. Rehabilitation psychology. In: Weiner I, Craighead W, (eds.) The concise Corsini encyclopedia of psychology and behavioral science. 4th ed. Hoboken, NJ: John Wiley & Sons; 2010. pp. 1444–7 [Google Scholar]
- 2.Cox D, Hess D, Hibbard M, Layman D, Stewart R. Specialty practice in rehabilitation psychology. Prof Psychol Res Pr 2010;41(1):82–8 [Google Scholar]
- 3.Larson P, Sachs P. A history of division 22. In: Dewsbury DA, (ed.) Unification through division: histories of the divisions of the American Psychological Association. Vol. V Washington, DC: American Psychological Association; 2000 [Google Scholar]
- 4.Gassaway J, Horn S, DeJong G, Smout R, Clark C, James R. Applying the clinical practice improvement approach to stroke rehabilitation: methods used and baseline results. Arch Phys Med Rehabil 2005;86(12 Suppl 2):S16–33 [DOI] [PubMed] [Google Scholar]
- 5.Whiteneck G, Dijkers M, Gassaway J, Jha A. SCIRehab: new approach to study the content and outcomes of spinal cord injury rehabilitation. J Spinal Cord Med 2009;32(3):251–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wilson C, Huston T, Koval J, Gordon S, Schwebel A, Gassaway J. SCIRehab: the psychology taxonomy. J Spinal Cord Med 2009;32(3):318–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Whiteneck G, Gassaway J, Dijkers M, Charlifue S, Backus D, Chen D, et al. SCIRehab: inpatient treatment time across disciplines in spinal cord injury rehabilitation. J Spinal Cord Med 2011;34(2):135–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gassaway J, Whiteneck G, Dijkers M. SCIRehab: clinical taxonomy development and application in spinal cord injury rehabilitation research. J Spinal Cord Med 2009;32(3):260–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Horn S, Gassaway J. Practice-based evidence study design for comparative effectiveness research. Med Care 2007;45(Suppl 2):S50–7 [DOI] [PubMed] [Google Scholar]
- 10.DeJong G, Hsieh C, Gassaway J, Horn S, Smout R, Putman K, et al. Characterizing rehabilitation services for patients with knee and hip replacement in skilled nursing and inpatient rehabilitation facilities. Arch Phys Med Rehabil 2009;90(8):1284–96 [DOI] [PubMed] [Google Scholar]
- 11.Horn S, DeJong G, Ryser D, Veazie P, Teraoka J. Another look at observational studies in rehabilitation research: going beyond the holy grail of the randomized controlled trial. Arch Phys Med Rehabil 2005;86(12 Suppl 2):S8–15 [DOI] [PubMed] [Google Scholar]
- 12.Marino R. editor. Reference manual for the international standards for neurological classification of SCI. Chicago, IL: American Spinal Injury Association; 2003 [Google Scholar]
- 13.Horn S, Sharkey S, Rimmasch H. Clinical practice improvement: a methodology to improve quality and decrease cost in health care. Oncol Issues 1997;12(1):16–20 [Google Scholar]
- 14.Horn S, Sharkey P, Buckle J, Backofen J, Averill R, Horn R. The relationship between severity of illness and hospital length of stay and mortality. Med Care 1991;29(4):305–17 [DOI] [PubMed] [Google Scholar]
- 15.Ryser D, Egger M, Horn S, Handrahan D, Ghandi P, Bigler E. Measuring medical complexity during inpatient rehabilitation following traumatic brain injury. Arch Phys Med Rehabil 2005;86:1108–17 [DOI] [PubMed] [Google Scholar]
- 16.Averill R, McGuire T, Manning B, Fowler D, Horn S, Dickson P, et al. A study of the relationship between severity of illness and hospital cost in New Jersey hospitals. Health Serv Res 1992;27(5):587–617 [PMC free article] [PubMed] [Google Scholar]
- 17.Clemmer T, Spuhler V, Oniki T, Horn S. Results of a collaborative quality improvement program on outcomes and costs in a tertiary critical care unit. Crit Care Med 1999;27(9):1768–74 [DOI] [PubMed] [Google Scholar]
- 18.Fiedler R, Granger C, Russell C. UDS(MR)SM: follow-up data on patients discharged in 1994–1996. Uniform data system for medical rehabilitation. Am J Phys Med Rehabil 2000;79(2):184–92 [DOI] [PubMed] [Google Scholar]
- 19.Fiedler R, Granger C. Functional independence measure: a measurement of disability and medical rehabilitation. In: Chino N, Melvin J, (eds.) Functional evaluation of stroke patients. Tokyo: Springer-Verlag; 1996. pp. 75–92 [Google Scholar]
- 20.Derogatis L. editor. BSI-18: administration, scoring and procedures manual. Minneapolis, MN: National Computer Systems; 2000 [Google Scholar]
- 21.Derogatis LR, Melisaratos N. The brief symptom inventory: an introductory report. Psychol Med 1983;13(3):595–605 [PubMed] [Google Scholar]
- 22.Simon G, VonKorff M, Piccinelli M, Fullerton C, Ormel J. An international study of the relation between somatic symptoms and depression. N Engl J Med 1999;341(18):1329–35 [DOI] [PubMed] [Google Scholar]
- 23.Kroenke KPCC. The interface between physical and psychological symptoms. J Clin Psychol 2003;5(Suppl 7):11–8 [Google Scholar]
- 24.Kalpakjian C, Bombardier C, Schomer K, Brown P. Measuring depression in persons with spinal cord injury: a systematic review. J Spinal Cord Med 2009;32(1):6–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.DeVivo M. Epidemiology of traumatic spinal cord injury. Spinal cord medicine. Philadelphia, PA: Lippincott, Williams & Wilkins; 2002 [Google Scholar]
- 26.Stevens J. Intermediate statistics: a modern approach. 2nd ed. Mahwah, NJ: Lawrence Erlbaum Associates, Inc.; 1999 [Google Scholar]
- 27.Stevens J. Partial and semipartial correlations; 2003. [accessed 2010 Feb 10]. Available from: www.uoregon.edu/~stevensj/MRA/partial.pdf
- 28.Dijkers M, Abela M, Gans B, Gordon W. The aftermath of spinal cord injury. In: Stover S, DeLisa J, Whiteneck G, (eds.) Spinal cord injury: clinical outcomes from the model systems. Gaithersburg, MD: Aspen; 1995 [Google Scholar]