Abstract
Objective
To examine the use of contraception in 13 countries in sub-Saharan Africa; to assess changes in met need for contraception associated with wealth-related inequity; and to describe the relationship between the use of long-term versus short-term contraceptive methods and a woman’s fertility intentions and household wealth.
Methods
The analysis was conducted with Demographic and Health Survey data from 13 sub-Saharan African countries. Wealth-related inequities in the use of contraception were calculated using household wealth and concentration indices. Logistic regression models were fitted for the likelihood of using a long-term contraceptive method, with adjustments for: wealth index quintile, fertility intentions (to space births versus to stop childbearing), residence (urban/rural), education, number of living children, marital status and survey year.
Findings
The use of contraception has increased substantially between surveys in Ethiopia, Madagascar, Mozambique, Namibia and Zambia but has declined slightly in Kenya, Senegal and Uganda. Wealth-related inequalities in the met need for contraception have decreased in most countries and especially so in Mozambique, but they have increased in Kenya, Uganda and Zambia with regard to spacing births, and in Malawi, Senegal, Uganda, the United Republic of Tanzania and Zambia with regard to limiting childbearing. After adjustment for fertility intention, women in the richest wealth quintile were more likely than those in the poorest quintile to practice long-term contraception.
Conclusion
Family planning programmes in sub-Saharan Africa show varying success in reaching all social segments, but inequities persist in all countries.
Résumé
Objectif
Étudier l’utilisation de la contraception dans 13 pays d’Afrique subsaharienne, évaluer les changements dans la satisfaction des besoins en matière de contraception par rapport aux inégalités liées à la richesse, et décrire la relation existant entre l’utilisation des méthodes contraceptives à long terme et à court terme, ainsi que les intentions d’une femme en matière de fécondité par rapport à la prospérité de son foyer.
Méthodes
L’analyse a été réalisée à partir des données de l’enquête démographique et sanitaire menée dans 13 pays d’Afrique subsaharienne. Les inégalités liées à la richesse et ayant un effet sur le recours à la contraception ont été calculées à partir des indices de richesse des ménages et des indices de concentration. Des modèles de régression logistique ont été adaptés pour refléter la probabilité d’utilisation d’une méthode contraceptive à long terme, avec les ajustements suivants: le quintile d’indice de richesse, l’intention de fécondité (espacer les naissances ou arrêter toute procréation), le domicile (urbain/rural), l’éducation, le nombre d’enfants en vie, la situation familiale et l’année de l’enquête.
Résultats
Le recours à la contraception a considérablement augmenté entre les enquêtes menées en Éthiopie, à Madagascar, au Mozambique, en Namibie et en Zambie, mais il a légèrement diminué au Kenya, au Sénégal et en Ouganda. Les inégalités liées à la richesse dans la satisfaction des besoins en matière de contraception ont décru dans la plupart des pays, notamment au Mozambique, mais elles ont augmenté au Kenya, en Ouganda et en Zambie en matière d’espacement des naissances, et au Malawi, en Ouganda, en République-Unie de Tanzanie, au Sénégal, et en Zambie en matière de limitation du nombre de grossesses. Après l’ajustement de l’intention de fécondité, les femmes appartenant au quintile le plus riche avaient une plus grande probabilité de pratiquer une contraception à long terme que celles appartenant au quintile le plus pauvre.
Conclusion
Les programmes de planification familiale en Afrique subsaharienne présentent différents degrés de succès pour atteindre tous les segments de la société, toutefois des inégalités persistent et ce, dans tous les pays.
Resumen
Objetivo
Analizar el uso de anticonceptivos en 13 países del África subsahariana, evaluar los cambios en las necesidades de anticoncepción cubiertas en relación con una distribución desigual de la riqueza y describir la relación existente entre el uso de métodos anticonceptivos (comparando el uso a largo y corto plazo) y las intenciones de embarazo de una mujer en función del nivel económico de la unidad doméstica.
Métodos
El análisis se realizó empleando los datos de una encuesta sobre salud y datos demográficos procedentes de 13 países del África subsahariana. Se calcularon las desigualdades en el uso de métodos anticonceptivos relacionadas con el nivel económico, empleando los índices de concentración y de economía de la unidad familiar. Respecto a la probabilidad de emplear un método anticonceptivo a largo plazo, se adaptaron modelos logísticos de regresión con ajustes del quintil de ingresos, la intención de embarazo (espaciar los nacimientos frente a dejar de tener hijos), la residencia (urbana/rural), la educación, el número de hijos vivos, el estado civil y el año de la encuesta.
Resultados
El uso de métodos anticonceptivos ha aumentado considerablemente entre las encuestas de Etiopía, Madagascar, Mozambique, Namibia y Zambia, si bien ha registrado un ligero descenso en Kenya, Senegal y Uganda. Las desigualdades de tipo económico a la hora de cubrir la necesidad de utilizar métodos anticonceptivos han disminuido en la mayoría de los países, especialmente en Mozambique, pero han aumentado en Kenya, Uganda y Zambia en relación al espaciamiento de los embarazos, y en Malawi, República Unida de Tanzanía, Senegal, Uganda y Zambia respecto a la reducción de la maternidad. Tras realizar el ajuste de la intención de embarazo, era más probable que las mujeres que se encontraban en el quintil más rico emplearan un método anticonceptivo a largo plazo que las mujeres que se situaron en el quintil más pobre.
Conclusión
Los programas de planificación familiar en el África subsahariana surten efecto de manera irregular en todos los segmentos de la sociedad, si bien las desigualdades persisten en todos los países.
ملخص
الغرض
تحرّي استخدام موانع الحمل في 13 بلداً من البلدان الواقعة جنوب الصحراء الكبرى الأفريقية؛ لتقييم التغيرات في تلبية الاحتياجات لموانع الحمل المرتبطة بالإجحاف المتعلق بالثروة؛ ووصف العلاقة بين استخدام وسائل منع الحمل طويلة الأمد مقابل وسائل منع الحمل قصيرة الأمد، والنية لدى المرأة للإنجاب وثروة الأسرة.
الطريقة
أُجري تحليل لمعطيات مسح ديموغرافي صحي في 13 بلداً جنوب الصحراء الأفريقية. وحُسِبَ الإجحاف المتعلق بالثروة في استخدام موانع الحمل عن طريق مؤشرات ثروة الأسرة ومؤشرات الكثافة. وجرى مواءمة نماذج التحوّف اللوجستي حسب أرجحية استخدام طرق موانع الحمل طويلة الأمد، مع إجراء تصحيحات لـ: الكمية الجزئية الخُمسية لمؤشر الثروة، والنية للإنجاب (المباعدة بين الولادات مقابل منع الحمل)، ومحل الإقامة (الحضر/الريف)، والتعليم، وعدد الأطفال الأحياء، والحالة الزوجية، والسنة التي أجري فيها المسح.
النتائج
ازداد استخدام موانع الحمل بدرجة كبيرة في أثيوبيا، ومدغشقر، وموزمبيق، وناميبيا، وزامبيا، ولكنه انخفض قليلاً في كينيا، والسنغال، وأوغندا. وقد انخفض الإجحاف المتعلق بالثروة في تلبية الاحتياجات لموانع الحمل في أغلب البلدان ولاسيما موزمبيق، لكنه ازداد في كينيا، وأوغندا، وزامبيا في ما يخص المباعدة بين الولادات، وفي مالاوي، والسنغال، وجمهورية تنزانيا المتحدة، وأوغندا، وزامبيا في ما يخص تقليل مرات الحمل. وبعد إجراء التصحيح على النية للإنجاب، وجد أن النساء في الكمية الجزئية الخُمسية الأكثر غناء وثروة كن أكثر ترجيحاً من النساء في الكمية الجزئية الخمسية الأكثر فقراً من حيث استخدام موانع الحمل طويلة الأمد.
الاستنتاج
تُظهِر برامج تنظيم الأسرة في البلدان الواقعة جنوب الصحراء الكبرى الأفريقية تفاوتاً في النجاح من حيث الوصول إلى جميع فئات المجتمع، ولكن الإجحاف مازال جاثماً على جميع البلدان.
Резюме
Цель
Проанализировать использование противозачаточных средств в 13 странах Африки к югу от Сахары, чтобы оценить динамику удовлетворения потребностей в предотвращении беременности, обусловленную неравенством в благосостоянии, и описать связь между использованием долгосрочных либо краткосрочных методов предотвращения беременности, с одной стороны, и репродуктивными намерениями женщин и благосостоянием домохозяйств, с другой.
Методы
Был проведен анализ данных Исследования в области демографии и здравоохранения по 13 странам Африки к югу от Сахары. Производился расчет обусловленного благосостоянием неравенства в использовании противозачаточных средств с применением индекса благосостояния домохозяйств и индекса концентрации. Осуществлялась подгонка моделей логистической регрессии по вероятности использования долгосрочного метода предотвращения беременности с поправкой на квинтиль индекса благосостояния, репродуктивные намерения (установление интервала между рождениями или прекращение деторождений), место жительства (городские/сельские районы), образование, количество живущих детей, семейное положение и год проведения исследования.
Результаты
В период между исследованиями уровень использования противозачаточных средств значительно возрос в Замбии, Мадагаскаре, Мозамбике, Намибии и Эфиопии, но несколько снизился в Кении, Сенегале и Уганде. В большинстве стран, особенно в Мозамбике, обусловленное благосостоянием неравенство в удовлетворении потребности в предотвращении беременности снизилось, однако в Замбии, Кении и Уганде оно возросло с учетом установления интервала между рождениями, а в Замбии, Малави, Объединенной Республике Танзании и Уганде – с учетом прекращения деторождений. С поправкой на репродуктивные намерения, женщины из богатейшей квинтили благосостояния с большей вероятностью, чем женщины из беднейшей квинтили, использовали долгосрочные методы предотвращения беременности.
Вывод
Охват всех сегментов общества при осуществлении программ планирования семьи в странах Африки к югу от Сахары достигается с переменным успехом, однако во всех странах сохраняется неравенство.
摘要
目的
旨在调查撒哈拉沙漠以南非洲地区13个国家避孕情况;评估与贫富差距相关联的避孕需求的满足情况;描述长期与短期避孕方法使用的关系以及妇女生育意愿与家庭财富的关系。
方法
本文结合撒哈拉以南非洲地区13个国家的人口统计和健康调查数据进行了分析。运用家庭财富和集中指数对避孕中与财富有关的不平等进行了计算。设立逻辑回归模型,确定使用长期避孕方法的可能性。模型中,对财富指数五分位数、生育意愿(间隔生育或停止生育),居住地(城市/农村)、教育、现有子女数量、婚姻状况和调查年份均进行了调整。
结果
调查之间,埃塞俄比亚、马达加斯加、莫桑比亚、纳米比亚和赞比亚避孕措施的使用大幅增加,而肯尼亚、塞内加尔和乌干达则略有下降。大多数国家满足避孕需求情况中与财富相关的不平等现象均有下降,然而就生育间隔而言,肯尼亚、乌干达和赞比亚的不平等现象增加;就限制生育而言,马拉维、塞内加尔、坦桑尼亚共和国、乌干达和赞比亚的不平等现象也出现增加。生育意愿调整之后,最富有的五分位数组的妇女比那些最贫困的五分位数组的妇女更有可能采用长期避孕。
结论
撒哈拉以南非洲地区的计划生育计划显示出触及所有社会阶层的不同程度的成功,但是不平等现象在所有国家依然存在。
Introduction
Global health has improved considerably over the last four decades, but everywhere the health status of the poor compares unfavourably with that of the more affluent sectors of society.1 In Africa, one in 26 women of reproductive age dies from a maternal cause, as opposed to one in 9400 in Europe.2 Parallel disparities in fertility and in contraceptive use are found between poor and wealthy countries. The world’s total fertility rate has dropped dramatically, from 5 children per woman in the early 1950s to 2.6 children per woman today,3 largely owing to more widespread use of modern contraceptives, especially in the developing world.4 Furthermore, in 1960 only around 9% of married women in the developing world practiced any form of contraception;2 today, this figure is 62%. Yet in less developed countries modern contraceptive methods are used by only 43% of women of reproductive age overall, and a wide gap in use is seen between the highest and lowest wealth quintiles (52% versus 35%, respectively).2 This gap between the rich and poor in the use of contraception has persisted despite general global improvements in socioeconomic status and the expansion of family planning services.5 Health disparities between the rich and poor remain an “intractable” challenge.1,6
An inequity exists when people are unfairly deprived of something they want or require to protect them from an unwanted or undesirable condition.7 Differences in mortality and morbidity that relate to socioeconomic class constitute an inequity. The poor do not have the same access to life-saving and health-maintaining interventions as the rich, yet they aspire to the same healthy lives as those who are economically better off.1 However, a difference in fertility between the rich and poor is not an inequity provided the poor have higher fertility because they want to have more children. Only by examining differences in fertility intentions and in contraceptive use through an equity lens can we determine if the poor are being deprived of something they wish they had (i.e. family planning) to avoid something they do not desire (i.e. pregnancy). The more a population meets its need for family planning, the less likely it is that an underlying inequity exists. On the other hand, women who do not want to have more children but who use a short-term or spacing method of contraception are not meeting their need, and neither are women who merely want to space births but who use a long-term or permanent contraceptive method.
This study first reviews trends in the use of short-term and long-term methods of contraception in 13 developing countries in sub-Saharan Africa. It then measures population-level changes in met need (i.e. satisfied demand) for contraception as a function of wealth-related inequity. Finally, it explores relationships at the individual level between the type of contraceptive method used by a woman, her reproductive goals or intentions and her household wealth.
Methods
Demographic and Health Survey (DHS)8 data were obtained for 13 sub-Saharan African countries that were selected based on the following criteria: (i) having had at least two DHS surveys, one of them after 2000, and (ii) a rate of use of modern methods of contraception among married women, as ascertained by the most recent DHS, of at least 10.0%. For countries where three or more surveys had been conducted, we used data from the two most recent ones. All data analysed were collected between 1997 and 2006.
DHSs are nationally-representative surveys that use standardized questionnaires to ask women of reproductive age about their sociodemographic characteristics, reproductive behaviour and use of maternal health services. The need for contraception, both met and unmet, is estimated from each survey based on standard DHS definitions – a woman is considered to have met her need for contraceptives for spacing births when she is using some family planning method and indicates that she wants to conceive sometime in the future but not within the next two years or is undecided; a woman is considered to have met her need for contraceptives to limit births when she is using some method of family planning and states that she wants to have no more children in the future.9
We grouped contraceptive methods into two categories: long-term methods (intrauterine devices, implants and sterilization), usually used to limit childbearing, and short-term methods (pills, condoms, spermicides, injectables, other modern methods and all traditional methods), better suited for women who want to delay but not forfeit having a child. We used data from all women of reproductive age and included traditional methods of contraception in the analysis because they are widely practised in sub-Saharan African countries.
DHSs do not collect data on household income; instead, they measure wealth based on household-level ownership of various assets (e.g. bicycles, cars, radios) and on housing characteristics (e.g. flooring material, drinking water source, type of toilet facility). The asset (wealth) index uses principal-components analysis to divide the population into wealth quintiles.10 Each household asset is assigned a weight or factor score and the resulting asset scores are standardized in relation to a normal distribution with a mean of 0 and a standard deviation of 1.
We used the concentration index, which varies between −1 and +1, to measure wealth-related inequity in contraceptive use. A concentration index of 0 indicates a lack of income inequality, while the more the index deviates from zero, the greater the magnitude of the wealth-related inequality. A negative concentration index indicates that a given unfavourable condition or practice is found more often among the poor, while a positive index suggests that a favourable condition or practice (i.e. contraceptive use) is found less often among the poorer than among the wealthier social strata.
We conducted univariate and bivariate analyses to examine the associations of interest and trends in contraceptive use and related wealth-inequity over time. After pooling the two survey samples for each country, we fitted logistic regression models for the likelihood of using a long-term rather than a short-term method of contraception as a function of two key covariates: (i) the woman’s reproductive goal or intention at the time (spacing versus limiting childbearing) and (ii) household wealth quintile. Models were adjusted for women’s residence (urban/rural), education, number of living children, marital status (married/in union and single/divorced/widowed) and year of survey. Also, models were estimated for the sample of women of reproductive age who were using contraception in each DHS survey year. All analyses were adjusted for complex survey design using Taylor’s linearization method11 and they were conducted using Stata version 9.1 (StataCorp. LP, College Station, United States of America).
Results
Table 1 presents an overview of the use of contraception at two points in time for the 13 sub-Saharan African countries. The number of years elapsed between the two selected surveys ranged between 4 and 8 (Malawi and Senegal, respectively) but was most commonly 5 or 6. Overall, the use of contraception remained at low to moderate levels at the time of the second survey and ranged from 8.7% in Senegal (2005) to 46.6% in Namibia (2006/07). The contraceptive prevalence rate decreased between surveys in three countries and increased substantially in five. In percentage points, the changes were as follows: Senegal, −2.1 (1997 to 2005); Kenya, −1.5 (1998 to 2003); Uganda, −0.5 (2000–01 to 2006); Mozambique, +19.6 (1997 to 2003); Namibia, +8.8 (2000 to 2006–07); Madagascar, +5.6 (1997 to 2003–04); Zambia, +5.4 (1996 to 2001–02); and Ethiopia, +4.4 (2000 to 2005). There was a modest rise (from +1 to +2 percentage points) in all the other countries except for the United Republic of Tanzania, which showed no overall change between 1999 and 2004/05.
Table 1. Use and change in use of short-term and long-term contraceptive methods between successive Demographic and Health Surveys (DHS), by country and survey year.
| Country | DHS year | n | Method |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| All |
Short-terma |
Long-termb |
||||||||
| Use (%) | Change in usec | Use (%) | Change in usec | Use (%) | Change in usec | |||||
| Cameroon | 2004 | 10 656 | 26.1 | 2.1 | 24.6 | 2.3 | 1.4 | −0.3 | ||
| Cameroon | 1998 | 5 501 | 24.0 | 22.3 | 1.7 | |||||
| Ethiopia | 2005 | 14 070 | 10.3 | 4.4 | 10.0 | 4.4 | 0.4 | 0.1 | ||
| Ethiopia | 2000 | 15 367 | 5.9 | 5.6 | 0.3 | |||||
| Ghana | 2003 | 5 691 | 20.7 | 2.7 | 17.9 | 1.4 | 2.6 | 1.1 | ||
| Ghana | 1998 | 4 843 | 18.0 | 16.5 | 1.5 | |||||
| Kenya | 2003 | 8 195 | 28.4 | −1.5 | 22.7 | −0.4 | 5.7 | −1.1 | ||
| Kenya | 1998 | 7 881 | 29.9 | 23.1 | 6.8 | |||||
| Madagascar | 2003–04 | 7 949 | 21.6 | 5.6 | 20.2 | 5.4 | 1.3 | 0.1 | ||
| Madagascar | 1997 | 7 060 | 16.0 | 14.8 | 1.2 | |||||
| Malawi | 2004 | 11 698 | 25.7 | 0.7 | 20.4 | −0.5 | 5.3 | 1.3 | ||
| Malawi | 2000 | 13 220 | 25.0 | 20.9 | 4.0 | |||||
| Mozambique | 2003 | 12 418 | 25.6 | 19.6 | 24.7 | 19.8 | 0.8 | −0.3 | ||
| Mozambique | 1997 | 8 779 | 6.0 | 4.9 | 1.1 | |||||
| Namibia | 2006–07 | 9 804 | 46.6 | 8.8 | 40.7 | 8.3 | 5.9 | 0.6 | ||
| Namibia | 2000 | 6 755 | 37.8 | 32.4 | 5.3 | |||||
| Rwanda | 2005 | 11 321 | 9.6 | 2.2 | 9.0 | 2.3 | 0.5 | −0.2 | ||
| Rwanda | 2000 | 10 421 | 7.4 | 6.7 | 0.7 | |||||
| Senegal | 2005 | 14 602 | 8.7 | −2.1 | 7.5 | −1.5 | 1.1 | −0.9 | ||
| Senegal | 1997 | 8 593 | 10.8 | 9.0 | 2.0 | |||||
| Uganda | 2006 | 8 531 | 19.6 | −0.5 | 17.3 | −0.9 | 2.2 | 0.4 | ||
| Uganda | 2000–01 | 7 246 | 20.1 | 18.2 | 1.8 | |||||
| United Republic of Tanzania | 2004–05 | 10 329 | 22.5 | 0.2 | 19.8 | −0.5 | 2.6 | 0.5 | ||
| United Republic of Tanzania | 1999 | 4 029 | 22.3 | 20.3 | 2.1 | |||||
| Zambia | 2001–02 | 7 658 | 24.6 | 5.4 | 22.7 | 5.3 | 1.7 | 0.0 | ||
| Zambia | 1996 | 8 021 | 19.2 | 17.4 | 1.7 | |||||
a Includes pills, condoms, spermicides, injectables, other modern methods, lactational amenorrhea and traditional contraceptive methods.
b Includes intrauterine devices, implants and female and male sterilization.
c In percentage points.
An uptake of short-term contraceptive methods was observed in Mozambique (+19.8 percentage points), Namibia (+8.3), Madagascar (+5.4), Zambia (+5.3) and Ethiopia (+4.4). In contrast, in the latest survey round the rate of use of long-term methods was found to be almost negligible; it ranged from 0.4% to 5.9% and exceeded 5% only in Namibia, Kenya and Malawi. Moreover, percentage-point increases in the use of long-term methods had been small to negligible and five countries (Cameroon, Kenya, Mozambique, Rwanda and Senegal) had experienced a reversal trend in use. In Mozambique, a parallel shift towards the use of short-term, spacing methods took place.
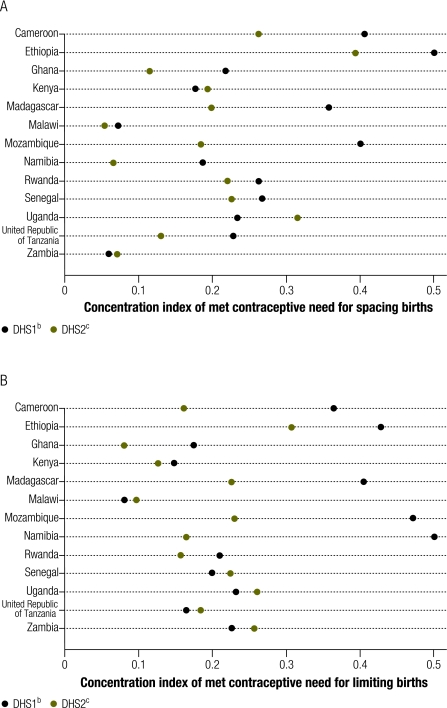
Poorer women use contraception much less than wealthier women.1,12 In this study we explored whether this reflected poorer women’s desire to have more children or their lower economic status. In Fig. 1, parts A and B, concentration indices in the met need for contraception to space (A) and limit childbearing (B) have been plotted. For the first survey analysed, concentration indices in the met need for contraception to space births were highest in Ethiopia (0.500) and lowest in Zambia (0.071) and Malawi (0.073). Wealth-related inequalities measured with the concentration index in the met need for contraception to limit future births were highest in Namibia, followed by Mozambique and Ethiopia (concentration index > 0.400), and lowest in Malawi (concentration index = 0.080). At the time of the last survey, the wealth-related inequality in the met need for contraception to space births was still highest in Ethiopia (concentration index = 0.400) and lowest in Malawi, Namibia and Zambia (concentration index < 0.100): Similarly, the wealth-related inequality in the met need for contraception to limit future births was highest in Ethiopia (concentration index = 0.300) and lowest in Ghana and Malawi (concentration index < 0.100).
Fig. 1.
Concentration indexa of met contraceptive needs for spacing and for limiting births in the two most recent Demographic and Health Surveys (DHS), by country
a A concentration index of 0 indicates that there is no wealth-related inequality in met need for spacing births. The more the index deviates from 0, the higher the existing wealth-related inequality in met need for spacing births.
b DHS1 refers to the next to last DHS.
c DHS2 refers to the most recent DHS conducted in each country.
Fig. 2, parts A and B, shows changes between the time of the first and second survey in the concentration indices for met need for contraception to space (A) and limit (B) births. Income-related inequalities in met need for contraception have decreased in most countries overall, but they have increased in Kenya, Uganda and Zambia with regard to spacing births, and in Malawi, Senegal, Uganda, the United Republic of Tanzania and Zambia with respect to limiting childbearing. The gap between the poorest and richest strata of society in the use of contraception to space births seems to have become much smaller in Mozambique (concentration index change > 0.200), while the gap in the use of contraception to stop childbearing showed the greatest reduction in Namibia (concentration index change > 0.300) and Mozambique (concentration index change > 0.200).
Fig. 2.
Change between successive Demographic and Health Surveys (DHS) in the concentration indexa of met contraceptive needs for spacing and for limiting births, by country
a A concentration index of 0 indicates that there is no wealth-related inequality in met contraceptive need. A positive change in the index represents a decrease in wealth-related inequality; a negative change in the index represents an increase in wealth-related inequality.
The first column in Table 2 shows the adjusted odds ratios (ORs), with their 95% confidence intervals (CIs), for the use of long-term rather than short-term contraceptive methods among women who reported wanting to space rather than limit childbearing. An OR of 1 indicates that women wanting to space births were no more likely to use long-term methods of contraception than women wanting to stop having children altogether. Thus, the higher the OR, the greater the likelihood that women will be using a long-term method to space births rather than to stop having children. In only 7 of the 13 study countries (Cameroon, Malawi, Mozambique, Namibia, Uganda, the United Republic of Tanzania and Zambia) were women more than 75% less likely to be using long-term methods of contraception to space births rather than to limit births at both survey time points. The last column in Table 2 shows the odds of women in the wealthiest quintile (the lowest being the reference) using a long-term method of contraception after adjustment for their fertility intention – only results for Cameroon, Kenya and Zambia were statistically significant at both time points. The small number of women using long-term methods of contraception in each wealth quintile, especially the poorest one, accounts for the wide CIs around the adjusted OR estimates and may explain why these estimates do not reach statistical significance for other countries.
Table 2. Odds of a woman using a long-term method of contraceptiona when wanting to space rather than limit childbearing and for those in the richest versus than the poorest wealth quintile, by country and Demographic and Health Survey (DHS) year.
| Country | DHS year | Wanting to spaceb OR (95% CI) | Richest wealth quintilec OR (95% CI) |
|---|---|---|---|
| Cameroon | 2004 | 0.24 (0.13–0.41) | 1.20 (0.41–3.53) |
| Cameroon | 1998 | 0.11 (0.04–0.31) | 4.12 (1.04–16.30) |
| Ethiopia | 2005 | 0.66 (0.36–1.23) | 1.53 (0.17–13.69) |
| Ethiopia | 2000 | 0.23 (0.09–0.62) | 2.59 (0.39–17.35) |
| Ghana | 2003 | 0.34 (0.16–0.73) | 2.62 (0.80–8.58) |
| Ghana | 1998 | 0.38 (0.18–0.82) | 0.53 (0.18–1.53) |
| Kenya | 2003 | 0.57 (0.39–0.83) | 3.52 (1.67–7.39) |
| Kenya | 1998 | 0.48 (0.32–0.72) | 2.74 (1.52–4.94) |
| Madagascar | 2003–04 | 0.39 (0.13–1.15) | 2.18 (0.50–9.56) |
| Madagascar | 1997 | 0.38 (0.19–0.77) | 0.83 (0.27–2.62) |
| Malawi | 2004 | 0.09 (0.05–0.15) | 2.05 (1.11–3.80) |
| Malawi | 2000 | 0.03 (0.01–0.07) | 1.54 (0.90–2.65) |
| Mozambique | 2003 | 0.09 (0.03–0.22) | 3.03 (0.82–11.22) |
| Mozambique | 1997 | 0.16 (0.06–0.41) | 1.24 (0.35–4.39) |
| Namibia | 2006–07 | 0.06 (0.03–0.14) | 3.30 (1.44–7.58) |
| Namibia | 2000 | 0.16 (0.09–0.29) | 2.19 (0.61–7.80) |
| Rwanda | 2005 | 0.34 (0.16–0.70) | 1.34 (0.49–3.65) |
| Rwanda | 2000 | 0.18 (0.07–0.44) | 4.39 (0.79–24.26) |
| Senegal | 2005 | 0.49 (0.24–0.99) | 1.94 (0.69–5.43) |
| Senegal | 1997 | 0.29 (0.14–0.61) | 2.86 (0.44–18.77) |
| Uganda | 2006 | 0.13 (0.06–0.28) | 0.78 (0.38–1.61) |
| Uganda | 2000–01 | 0.13 (0.06–0.29) | 1.43 (0.59–3.47) |
| United Republic of Tanzania | 2004–05 | 0.24 (0.14–0.39) | 2.14 (1.03–4.44) |
| United Republic of Tanzania | 1999 | 0.14 (0.05–0.46) | 1.07 (0.24–4.77) |
| Zambia | 2001–02 | 0.14 (0.05–0.40) | 6.35 (1.93–20.95) |
| Zambia | 1996 | 0.09 (0.03–0.23) | 6.37 (2.10–19.37) |
CI, confidence interval; OR, odds ratio.
a The samples comprise only women who were using a method of contraception at the time of the survey. The model was adjusted for women’s residence, education, age, parity, marital status and complex survey design.
b The reference category is the intention to limit childbearing.
c The reference category is the poorest wealth quintile.
Discussion
By and large, changes in contraceptive practices among women of reproductive age in the 13 study countries between the mid-1990s and mid-2000s have been marginal, with a few exceptions. More specifically, between the last two DHS surveys, the use of contraception showed substantial percentage point increases in five of the countries (Ethiopia, Madagascar, Mozambique, Namibia and Zambia) and marginal declines in three (Kenya, Senegal and Uganda). Since reversals in population-level use of contraception are historically infrequent, these declines merit further examination.
In all five countries with substantial increases in the use of contraception, short-term methods, primarily injectables, were increasingly relied upon. This finding is not surprising since women of reproductive age are more likely to use contraception to space rather than to stop childbearing.13 Moreover, the use of short-term methods has increased, while the use of long-term methods has not changed significantly in the 13 countries and has declined in five. In Mozambique, the large positive trend in the use of contraception accompanied the country’s return to peace following the end of civil war in the early 1990s and the restoration of its health system and care functions.
Notably, in most countries, wealth-related inequalities in the reported met need for contraception have declined between surveys. However, such inequalities have increased in Kenya and Uganda with respect to the met need for spacing births, while the opposite has occurred in Mozambique, where practice of lactational amenorrhea by around 7.5% of all women in 2003 may reflect a satisfaction of latent demand for contraception by means of prolonged breastfeeding and postpartum abstinence. Mozambique is the only one of the 13 study countries that experienced a significant increase in reliance on traditional methods between surveys, probably owing to the availability and acceptance of modern contraception in the countries studied14 and the lower use-effectiveness of traditional methods.15 Wealth-related inequalities in the met need for contraception to limit births have declined most sharply in Namibia and Mozambique, where both the use of contraception in general and of short-term contraceptive methods in particular has increased significantly between surveys.
We examined whether the form of contraception being used by women in the 13 study countries was concordant with their fertility intentions. Such concordance could mean that a woman was familiar with the different contraceptive methods and knew for how long each one protects against pregnancy, it could reflect a particular method’s greater availability, affordability and acceptability or simply a woman’s preference for a specific method.16 As expected, when childbearing intentions are controlled for, women in the richest wealth quintile appear to be more likely than women in the poorest wealth quintile to use long-term contraception, which is more expensive than short-term contraception and usually provided at clinics. Thus, closing this particular gap between the rich and the poor in developing countries will entail addressing women’s access to contraceptives and making all methods affordable. As an example, the cost to a couple of using contraception consistently for one year (i.e. couple–year of protection) ranges from 0.1% (for intrauterine devices) to 6.7% (for male condoms) of the annual per capita household consumption expenditure (281.03 United States dollars) in Ghana,17,18 one of richest countries we studied.17 Clearly, with the cost per couple–year of protection being so similar for short-term and for long-term methods of contraception, and since wealth-related inequalities are greater in the use of long-term methods, simply making short-term methods more widely available or improving their distribution will not suffice to close the rich–poor gap.
Our study has several limitations. We used cross-sectional survey data, which can only reveal associations rather than causal relationships between covariates and the outcomes of interest. Although the wealth index has been widely employed to explore health inequities using DHS data, there is concern that it is strongly influenced by community- and household-level factors19 and may not be robust enough to examine changes in health inequities. Given that the DHS follows a standardized methodology, the wealth index provides the opportunity to make within- and cross-country comparisons at multiple time points. Importantly, in the DHS the need for family planning is designated as having been met based on a woman's expressed desire to either space or limit future births and not on her stated wish to use family planning methods to do so, yet the former was used as a proxy for the latter in our analysis. Thus, our findings need to be interpreted with caution, since women may have used or not used contraception for reasons not included in the regression equations. Furthermore, we did not adjust for other important factors (e.g. cultural, social, relationship-related) that could influence women’s use of contraception but that are not explored in the DHS. We also lack data on contraceptive supply-side factors — distribution mechanisms, stock-outs, changes in family planning programme strength or in donors’ financial support can greatly influence the overall use of contraception and the method mix. Programme downturns will most likely be felt by the poor.
Additionally, the time between the two DHS surveys differed slightly for the 13 countries. Because the use of long-term methods of contraception is low among all women as well as among women using some form of contraception, estimating multivariate models with highly skewed outcomes is statistically challenging. The large survey sample sizes provide statistical power buffers but do not overcome the empirical limitations that stem from attempting to explain variations in the choice of contraceptive methods when little choice occurs.
Family planning interventions are among the most cost-effective health interventions because they are closely related to maternal and infant health and survival.20–23 Modern contraception is more than a technical advance; it has caused a genuine “reproductive revolution” and is considered a “social vaccine”. However, the extent to which family planning programmes succeed in reaching all segments of the population varies between and within countries but is disappointingly low in all of them. Indeed, it is safe to say that the need for contraception is not being adequately addressed among all segments of society, and especially so among the poor.24
Commonly accepted components of successful family planning programmes include improvements in geographic and public–private sector access to a broad mix of contraceptive methods, availability of competent health-care providers, promotion of active behavioural change through communications interventions, and political will.6,25,26 While we cannot determine how much each of these factors contributed to our findings in the 13 study countries, delivering family planning services that address clients’ needs, a common aspect of the rationale and philosophy behind family planning programmes around the world, can effectively increase the use of contraceptive methods.13 As greater use is attained, the success of family planning programmes will increasingly depend upon how well their services are tailored to the unique needs of specific groups of users and how effectively they address equity issues in service delivery. Moreover, ensuring that the type of family planning offered matches a woman’s fertility intentions is key to improving family planning services.
Competing interests:
None declared.
References
- 1.Ahmed S, Creanga AA, Gillespie DG, Tsui AO. Economic status, education and empowerment: implications for maternal health service utilization in developing countries. PLoS ONE. 2010;5:e11190. doi: 10.1371/journal.pone.0011190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.2009 world population data sheet [Internet]. Washington: Population Reference Bureau; 2009. Available from: http://www.prb.org/Publications/Datasheets/2009/2009wpds.aspx [accessed 17 January 2011].
- 3.State of the world population 2007: unleashing the potential of urban growth New York: United Nations Population Fund; 2007. Available from: http://www.unfpa.org/swp/ [accessed 17 January 2011].
- 4.Bongaarts J. Trends in unwanted childbearing in the developing world. Stud Fam Plann. 1997;28:267–77. doi: 10.2307/2137858. [DOI] [PubMed] [Google Scholar]
- 5.Gakidou E, Vayena E. Use of modern contraception by the poor is falling behind. PLoS Med. 2007;4:e31. doi: 10.1371/journal.pmed.0040031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boerma JT, Bryce J, Kinfu Y, Axelson H, Victora CG, Countdown 2008 Equity Analysis Group Mind the gap: equity and trends in coverage of maternal, newborn, and child health services in 54 Countdown countries. Lancet. 2008;371:1259–67. doi: 10.1016/S0140-6736(08)60560-7. [DOI] [PubMed] [Google Scholar]
- 7.Gillespie D, Ahmed S, Tsui A, Radloff S. Unwanted fertility among the poor: an inequity? Bull World Health Organ. 2007;85:100–7. doi: 10.2471/BLT.06.033829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Demographic and Health Surveys. Calverton: Measure DHS, ICF Macro. Available from: http://www.measuredhs.com/ [accessed 17 January 2011].
- 9.Demographic and Health Surveys Recode Manual. Calverton: Measure DHS, ICF Macro. Available from: http://www.measuredhs.com/pubs/pdf/DHSQ6/DHS6_Woman's_QRE_4_November_2010.pdf [accessed 17 January 2011].
- 10.Rutstein SO, Johnson K. The DHS wealth index (DHS Comparative Reports No. 6). Calverton: ORC Macro; 2004. [Google Scholar]
- 11.Wolter KM. Introduction to variance estimation New York: Springer; 2003. [Google Scholar]
- 12.Sedgh G, Hussain R, Bankole A, Singh S. Women with an unmet need for contraception in developing countries and their reasons for not using a method (Occasional Report No. 37). New York: Guttmacher Institute; 2007. Available from: http://www.policyarchive.org/handle/10207/bitstreams/5945.pdf [accessed 17 January 2011].
- 13.Jansen WH., 2nd Existing demand for birth spacing in developing countries: perspectives from household survey data. Int J Gynaecol Obstet. 2005;89(Suppl 1):S50–60. doi: 10.1016/j.ijgo.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 14.Ross J, Hardee K, Mumford E, Eid S. Contraceptive method choice in developing countries. Int Fam Plan Perspect. 2001;28:32–40. doi: 10.2307/3088273. [DOI] [Google Scholar]
- 15.Kost K, Singh S, Vaughan B, Trussell J, Bankole A. Estimates of contraceptive failure from the 2002 National Survey of Family Growth. Contraception. 2008;77:10–21. doi: 10.1016/j.contraception.2007.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Seiber EE, Bertrand JT, Sullivan TM. Changes in contraceptive method mix in developing countries. Int Fam Plan Perspect. 2007;33:117–23. doi: 10.1363/3311707. [DOI] [PubMed] [Google Scholar]
- 17.World development indicators database [Internet]. Washington: The World Bank. Available from: http://data.worldbank.org/data-catalog/world-development-indicators/wdi-2010 [accessed 17 January 2011].
- 18.Ghana Demographic and Health Survey 2008 Accra and Calverton: Ghana Statistical Service & ICF Macro; 2009. Available from: http://www.measuredhs.com/pubs/pdf/FR221/FR221.pdf [accessed 17 January 2011].
- 19.Howe LD, Hargreaves JR, Ploubidis GB, De Stavola BL, Huttly SR. Subjective measures of socio-economic position and the wealth index: a comparative analysis. Health Policy Plan. 2010 doi: 10.1093/heapol/czq043. [DOI] [PubMed] [Google Scholar]
- 20.Benagiano G, Bastianelli C, Farris M. Contraception: a social revolution. Eur J Contracept Reprod Health Care. 2007;12:3–12. doi: 10.1080/13625180601012311. [DOI] [PubMed] [Google Scholar]
- 21.Conde-Agudelo A, Belizán JM. Maternal morbidity and mortality associated with interpregnancy interval: cross sectional study. BMJ. 2000;321:1255–9. doi: 10.1136/bmj.321.7271.1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhu BP, Rolfs RT, Nangle BE, Horan JM. Effect of the interval between pregnancies on perinatal outcomes. N Engl J Med. 1999;340:589–94. doi: 10.1056/NEJM199902253400801. [DOI] [PubMed] [Google Scholar]
- 23.Rutstein SO. Effects of preceding birth intervals on neonatal, infant and under-five years mortality and nutritional status in developing countries: evidence from the demographic and health surveys. Int J Gynaecol Obstet. 2005;89(Suppl 1):S7–24. doi: 10.1016/j.ijgo.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 24.Townsend JW. Program strategies for reducing inequities in reproductive health services. Stud Fam Plann. 2010;41:139–42. doi: 10.1111/j.1728-4465.2010.00236.x. [DOI] [PubMed] [Google Scholar]
- 25.Robinson W, Ross J, editors. The global family planning revolution: three decades of population policies and programs Washington: The World Bank; 2007. Available from: http://siteresources.worldbank.org/INTPRH/Resources/GlobalFamilyPlanningRevolution.pdf [accessed 17 January 2011].
- 26.DaVanzo J, Adamson D. Family planning in developing countries: an unfinished success story [Internet]. Santa Monica: Rand Corporation; 1998. Available from: http://www.rand.org/pubs/issue_papers/IP176.html [accessed 17 January 2011].