Why do we need another metric in dyslipidemia management? Low-density-lipoprotein cholesterol (LDL-C) is currently the primary treatment target for dyslipidemia management.1 However, it has been shown that the risk for future coronary artery disease (CAD) events remains high in patients who have attained the guideline-recommended LDL-C goals. For example, in the Pravastatin or Atorvastatin Evaluation and Infection Therapy (PROVE-IT TIMI 22) trial,2 22.7% of the patients had a recurrent event at 2 years of follow-up despite attaining LDL-C levels of 67 mg/dL and receiving optimal medical care. It is important to note that this event rate is probably an underestimation of the recurrent event rate in everyday clinical practice, where patient characteristics and the dynamics of care are different from those in a randomized clinical trial setting.
Some of this residual risk is almost certainly a reflection of various other comorbid conditions that CAD patients have (for example, diabetes mellitus, hypertension, smoking, and physical inactivity) and of their genetic predisposition to recurrent events. Examining non-high-density lipoprotein cholesterol (non-HDL-C) could explain some of this “residual risk” for CAD events in these patients.
What Is Non-HDL-C and What Are the Treatment Goals?
Non-HDL-C use in clinical practice is not a new concept. The Helsinki Heart Study3 used non-HDL-C levels to randomize patients. It is important to note that non-HDL-C (unlike LDL-C) represents the cholesterol content present in all the atherogenic lipoproteins (Fig. 1). Therefore, treatment of non-HDL-C is grounded in a more holistic principle of dyslipidemia management than is LDL-C treatment.
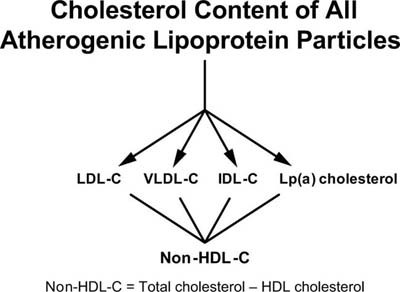
Fig. 1 Components of non-high-density lipoprotein cholesterol (non-HDL-C).
The non-HDL-C goal is 30 mg/dL above the LDL-C goal. IDL-C = intermediate-density lipoprotein cholesterol; LDL-C = low-density lipoprotein cholesterol; Lp(a) = lipoprotein (a); VLDL-C = very low-density lipoprotein cholesterol
On this basis, non-HDL-C was added as a secondary treatment target in patients with elevated triglycerides (>200 mg/dL).1 The treatment goal for non-HDL-C is 30 mg/dL above the LDL-C treatment target. For example, if the LDL-C treatment goal is <70 mg/dL, the non-HDL-C treatment target would be <100 mg/dL in a patient who has acute coronary syndrome (ACS) and a concomitant triglyceride level >200 mg/dL. It is important to note, though, that in a 2008 consensus statement by the American College of Cardiology Foundation and the American Diabetes Association,4 no triglyceride cutoff level was defined for calculating non-HDL-C.
Why Non-HDL-C Is a Better Marker of Risk than LDL-C
Non-HDL-C has been shown to be a better marker of risk in both primary and secondary prevention studies. In a recent analysis of data combined from 68 studies,5 non-HDL-C was the best predictor among all cholesterol measures, both for CAD events and for strokes. In the Incremental Decrease in End Points through Aggressive Lipid Lowering (IDEAL) trial,6 elevated non-HDL-C and apolipoprotein B (apo B) levels were the best predictors, after ACS, of adverse cardiovascular outcomes in patients who were on lipid-lowering therapy, whereas LDL-C was not associated with poor outcomes once non-HDL-C or apo B was included in the regression model. There are multiple other reasons for the usefulness of non-HDL-C. These include the following:
Non-HDL-C measures the cholesterol content of all atherogenic lipoproteins, including LDL, as described above.
Non-HDL-C is easily calculated from a lipid profile (non-HDL-C = total cholesterol minus HDL-C), and thus it incurs no additional testing cost to the healthcare system. Non-HDL-C levels can be measured from a sample in a nonfasting patient, as opposed to LDL-C measurements, which require fasting. This is especially important in hospitalized patients, who are not always fasting.
Elevated levels of non-HDL-C in combination with normal levels of LDL-C identify a subset of patients with elevated levels of LDL particle number, elevated apo B concentrations, and LDL of small, dense morphology.7 Measuring apo B and LDL particle concentration adds expense, is not standardized for the most part, and is not currently endorsed in major national cholesterol-treatment guidelines in the United States. On the other hand, non-HDL-C adds no further cost, uses a standard (fasting or nonfasting) lipid panel for calculation, and is endorsed in that calculation by current guidelines. Paying attention to non-HDL-C may obviate the need for expensive tests that measure LDL particle number, total apo B concentration, or LDL phenotype (type A or B). This has the potential of improving patient care without increasing the cost to the healthcare system.
The increase in the incidence of metabolic syndrome probably decreases the accuracy of risk prediction for CAD events when LDL-C is used for that purpose, whereas non-HDL-C, total apo B concentration, and LDL particle concentration retain predictive capability in this patient population.8
Elevated levels of non-HDL-C are treatable by increasing the intensity of currently available lipid-lowering agents, as well as lifestyle modification. All of the currently available lipid-lowering agents (statins, fibrates, niacin, fish-oil products, and intestinally active agents) decrease non-HDL-C levels.
Current Goal Attainment for Non-HDL-C
Although LDL-C goal attainment has improved, non-HDL-C goal attainment remains poor. In a 2003 survey by the National Cholesterol Education Program (NCEP Evaluation ProjecT Utilizing Novel E-Technology [NEPTUNE II]),9 62% of CAD patients achieved the LDL-C goal of <100 mg/dL, but only 33% achieved both LDL-C and non-HDL-C goals. Our recent analyses have shown that although goal attainment of LDL-C <100 mg/dL was seen in 80% of CAD patients, the combined goal attainment for LDL-C (<100 mg/dL) and non-HDL-C (<130 mg/dL) remained low, at 51%. Under stringent criteria for LDL-C (<70 mg/dL) and non-HDL-C (<100 mg/dL), this goal attainment fell to 13%.10
Challenges to Non-HDL-C Goal Attainment and Future Directions
As stated above, although non-HDL-C is a better marker of risk than is LDL-C, the goal attainment for non-HDL-C remains poor. Although the reasons for this lower goal attainment have not been explored, possibilities include deficiencies in providers' knowledge of the importance of non-HDL-C, of how to perform the calculation for non-HDL-C, and of treatment goals for non-HDL-C. Other limiting factors could include problems with patients' tolerance of or compliance with higher doses of statins or with the addition of lipid-lowering medications from other classes (which often is needed to attain non-HDL-C goals). It has been suggested that direct reporting of non-HDL-C on standard lipid-panel results would improve goal attainment for non-HDL-C.11 The impact of this direct reporting—either alone or coupled with measures like audit and feedback—to the providers about their performance on goal attainment for non-HDL-C is not known. Improving goal attainment for non-HDL-C will probably require multiple system-level interventions that incorporate measures geared towards better dissemination of cholesterol-management guidelines to the providers, together with continual feedback on their performance. The need to test these strategies for better guideline dissemination in general and for non-HDL-C guidelines in particular will become even more important once the Adult Treatment Panel IV guidelines have been published.
Footnotes
Address for reprints: Salim S. Virani, MD, Health Services Research & Development (152), Michael E. DeBakey Veterans Affairs Medical Center, 2002 Holcombe Blvd., Houston, TX 77030. E-mail: salim.virani@va.gov
Presented at the Risk, Diagnosis and Treatment of Cardiovascular Disease in Women symposium; Denton A. Cooley Auditorium, Texas Heart Institute, Houston; 11 September 2010.
This work was supported by the Houston VA Health Services Research & Development Center of Excellence (grant number HFP90-020). Dr. Virani is supported by a Department of Veterans Affairs Health Services Research & Development Service (HSR&D) Career Development Award (grant number: CDA 09-028). The views expressed in this article are those of the author and do not necessarily represent the views of the Department of Veterans Affairs.
References
- 1.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001;285(19):2486–97. [DOI] [PubMed]
- 2.Cannon CP, Braunwald E, McCabe CH, Rader DJ, Rouleau JL, Belder R, et al. Intensive versus moderate lipid lowering with statins after acute coronary syndromes [published erratum appears in N Engl J Med 2006;354(7):778]. N Engl J Med 2004;350(15):1495–504. [DOI] [PubMed]
- 3.Frick MH, Elo O, Haapa K, Heinonen OP, Heinsalmi P, Helo P, et al. Helsinki Heart Study: primary-prevention trial with gemfibrozil in middle-aged men with dyslipidemia. Safety of treatment, changes in risk factors, and incidence of coronary heart disease. N Engl J Med 1987;317(20):1237–45. [DOI] [PubMed]
- 4.Brunzell JD, Davidson M, Furberg CD, Goldberg RB, Howard BV, Stein JH, Witztum JL. Lipoprotein management in patients with cardiometabolic risk: consensus conference report from the American Diabetes Association and the American College of Cardiology Foundation. J Am Coll Cardiol 2008;51(15):1512–24. [DOI] [PubMed]
- 5.Emerging Risk Factors Collaboration, Di Angelantonio E, Sarwar N, Perry P, Kaptoge S, Ray KK, et al. Major lipids, apolipoproteins, and risk of vascular disease. JAMA 2009;302 (18):1993–2000. [DOI] [PMC free article] [PubMed]
- 6.Kastelein JJ, van der Steeg WA, Holme I, Gaffney M, Cater NB, Barter P, et al. Lipids, apolipoproteins, and their ratios in relation to cardiovascular events with statin treatment. Circulation 2008;117(23):3002–9. [DOI] [PubMed]
- 7.Ballantyne CM, Andrews TC, Hsia JA, Kramer JH, Shear C; ACCESS Study Group. Atorvastatin Comparative Cholesterol Efficacy and Safety Study. Correlation of non-high-density lipoprotein cholesterol with apolipoprotein B: effect of 5 hydroxymethylglutaryl coenzyme A reductase inhibitors on non-high-density lipoprotein cholesterol levels. Am J Cardiol 2001;88(3):265–9. [DOI] [PubMed]
- 8.Sattar N, Williams K, Sniderman AD, D'Agostino R Jr, Haffner SM. Comparison of the associations of apolipoprotein B and non-high-density lipoprotein cholesterol with other cardiovascular risk factors in patients with the metabolic syndrome in the Insulin Resistance Atherosclerosis Study. Circulation 2004;110(17):2687–93. [DOI] [PubMed]
- 9.Davidson MH, Maki KC, Pearson TA, Pasternak RC, Deedwania PC, McKenney JM, et al. Results of the National Cholesterol Education (NCEP) Program Evaluation ProjecT Utilizing Novel E-Technology (NEPTUNE) II survey and implications for treatment under the recent NCEP Writing Group recommendations. Am J Cardiol 2005;96(4):556–63. [DOI] [PubMed]
- 10.Virani SS, Woodard LD, Landrum CR, Pietz K, Wang D, Ballantyne CM, Petersen LA. Institutional, provider, and patient correlates of LDL and non-HDL cholesterol goal attainment according to the Adult Treatment Panel III Guidelines. Am Heart J (in press). [DOI] [PubMed]
- 11.Blaha MJ, Blumenthal RS, Brinton EA, Jacobson TA, National Lipid Association taskforce on non-HDL cholesterol. The importance of non-HDL cholesterol reporting in lipid management [monograph on the Internet]. J Clin Lipidol 2008;2(4):267–73. Available at: http://www.lipidjournal.com/article/S1933-2874(08)00274-2/abstract [cited 2011 Feb 1]. [DOI] [PubMed]


