Abstract
WEB-SITE FEATURE
A 19-year-old woman presented at the emergency department with chest and back pain. One month previously, she had undergone examination at a different institution, where the diagnosis was reportedly aortic dissection. The patient had a history of rheumatoid arthritis, for which she had been taking prednisone, hydroxychloroquine, and methotrexate. She had also begun taking a β-blocker as a result of the diagnosis of aortic dissection. She reported no history of chest trauma.
Physical examination revealed hypotension (blood pressure, 83/52 mmHg) and tachycardia (heart rate, 101 beats/min). Computed tomography of the chest revealed a large anterior mediastinal mass (Fig. 1). A few centimeters above the aortic valve, a 2- to 3-mm defect in the anterior wall of the aorta was seen. There was an extravasation of contrast medium into the mass.
Fig. 1 Computed tomogram of the chest shows a large anterior mediastinal mass.
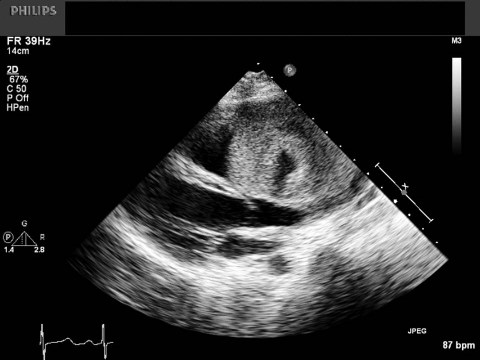
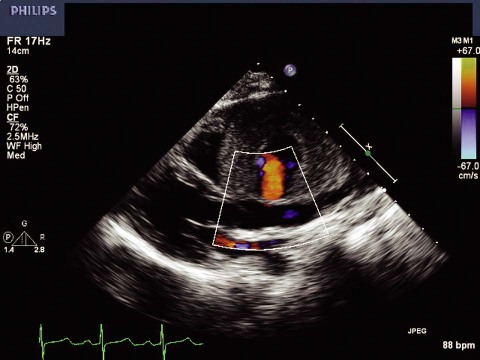
Results of 2-dimensional Doppler echocardiography confirmed the presence of a large mass in the superior and anterior mediastinum (Fig. 2). Color-flow Doppler echocardiography showed a shunt—consistent with a pseudoaneurysm—from the aorta into the mass, approximately 3 cm above the aortic valve (Fig. 3). Thick thrombus lined the outer portion of the mass. Color flow was seen within a small internal chamber of the pseudoaneurysm.
Fig. 2 Two-dimensional Doppler echocardiography shows a large mass in the superior and anterior mediastinum.
Real-time motion image is available at www.texasheart.org/journal.
Fig. 3 Color-flow Doppler echocardiography reveals a shunt from the aorta into the mass, consistent with a pseudoaneurysm.
Real-time motion image is available at www.texasheart.org/journal.
The pseudoaneurysm was surgically resected, and the small defect was oversewn and reinforced with a pericardial patch. The patient was discharged from the hospital on the 7th postoperative day in satisfactory condition. Histopathologic analysis of tissue from the luminal surface of the pseudoaneurysm revealed mixed inflammatory cells.
Comment
Ascending aortic pseudoaneurysms are infrequently seen. They typically develop after chest trauma or cardiac surgery.1,2 Our patient had no history of cardiac surgery and reported no chest trauma. Aortic pseudoaneurysms have also been reported in patients with infections (chiefly, tuberculosis) and collagen vascular diseases.3–5 Our patient did not have tuberculosis, and she reported no ulcerations that would have supported a diagnosis of Behçet disease. The mixed inflammatory cells were thought to be the result of an infectious process or an inflammatory autoimmune disease. We conclude that the patient's rheumatoid arthritis was the most likely cause of the pseudoaneurysm.
Acknowledgment
We wish to acknowledge William Gadea, PA-C, for his benevolence and his commitment to the care of this patient.
Supplementary Material
Footnotes
Address for reprints: Mary A. Anstadt, MS, RCEP, Department of Cardiology, Mail Stop 11102M, Regions Hospital, 640 Jackson St., St. Paul, MN 55101. E-mail: mary.a.anstadt@healthpartners.com
References
- 1.Deng YB, Li CL, Chang Q. Chronic traumatic pseudoaneurysm of the ascending aorta causing right ventricular inflow obstruction. Circ J 2003;67(4):359–61. [DOI] [PubMed]
- 2.Atik FA, Navia JL, Svensson LG, Vega PR, Feng J, Brizzio ME, et al. Surgical treatment of pseudoaneurysm of the thoracic aorta. J Thorac Cardiovasc Surg 2006;132(2):379–85. [DOI] [PubMed]
- 3.Choudhary SK, Bhan A, Talwar S, Goyal M, Sharma S, Venugopal P. Tubercular pseudoaneurysms of aorta. Ann Thorac Surg 2001;72(4):1239–44. [DOI] [PubMed]
- 4.Alkim H, Gurkaynak G, Sezgin O, Oguz D, Saritas U, Sahin B. Chronic pancreatitis and aortic pseudoaneurysm in Behcet's disease. Am J Gastroenterol 2001;96(2):591–3. [DOI] [PubMed]
- 5.Lau H, Cheng SW. Takayasu arteritis–a case report of aortic aneurysm. Singapore Med J 1998;39(11):507–10. [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.