Cardiac disease in the pregnant patient can present challenges in cardiovascular and maternal-fetal management.1 It is important to understand that even in normal patients, pregnancy imposes some dramatic physiologic changes upon the cardiovascular system. These include an increase in plasma volume by 50%, an increase in resting pulse by 17%, and an increase in cardiac output by 50%. After delivery, the heart rate normalizes within 10 days; by 3 months postpartum, stroke volume, cardiac output, and systemic vascular resistance return to the pre-pregnancy state. General guidelines for the management of pregnant women with heart disease are outlined below.
Prosthetic Heart Valves
Anticoagulation for mechanical heart valves should be adjusted, because warfarin must be discontinued during the 1st trimester due to the well-documented risk of embryopathy. Current guidelines support 3 approaches: 1) low-molecular-weight (LMW) heparin administered subcutaneously twice daily throughout pregnancy, 2) unfractionated heparin administered subcutaneously twice daily throughout pregnancy, or 3) unfractionated or LMW heparin administered subcutaneously twice daily until gestational week 13, followed by warfarin from weeks 13 to 35, followed by a return to unfractionated or LMW heparin administered subcutaneously twice daily until delivery.2 Individual management approaches should be discussed jointly by the cardiologist, obstetrician, and patient. Aspirin for bioprosthetic heart valves is safe in pregnancy and need not be adjusted. Antibiotic prophylaxis for delivery (vaginal or caesarean section) is not recommended by the 2008 American Heart Association/American Dental Association guidelines. However, some obstetricians still routinely administer antibiotic agents at the time of rupture of membranes.
Acquired Heart Disease
Acute coronary syndromes and myocardial infarction are rare in pregnancy (1–2 per 35,000 deliveries) but can occur in all stages.3 The usual coronary risk factors apply, and additional risk factors include advanced maternal age, thrombocytosis, blood transfusion, and preeclampsia. Cardiac catheterization is permissible in pregnant patients, with appropriate abdominal lead coverage for the mother and fluoroscopy time minimized. Thrombolytic agents can be given, but the guidelines for percutaneous coronary intervention should be followed. Direct-current cardioversion is also safe in pregnancy. Supraventricular and ventricular tachycardia should be treated by both nonpharmacologic and pharmacologic means, as in the nonpregnant patient. However, amiodarone should be avoided, because it crosses the placenta and can have toxic effects on the fetus.
The indications for a permanent pacemaker follow the standard guidelines. The need to implant a cardiac defibrillator should be weighed against the need to delay this procedure until after delivery.
Congenital Heart Disease
Several recent studies have addressed congenital heart disease (CHD) in pregnancy. In general, regurgitant lesions are well tolerated, whereas obstructive lesions are poorly tolerated. One well-cited retrospective study4 found no maternal deaths during analysis of 90 pregnancies in mothers who had CHD. However, 17% had pulmonary edema and 12% had cardiac events (most frequently a nonsustained tachyarrhythmia). A recent meta-analysis of 2,491 pregnancies in patients with CHD5 showed a miscarriage rate of 15% and a lower cardiovascular event rate of 6%. This study also found an 8% incidence of congenital heart disease in the offspring, which is similar to the findings of other studies.
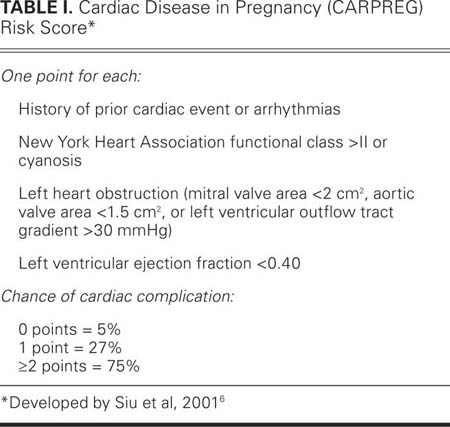
The Cardiac Disease in Pregnancy (CARPREG) Risk Score (Table I) can be calculated to estimate a woman's cardiac risk during pregnancy.6 One point is assigned for each of the following risk factors: a history of cardiac event or arrhythmia, New York Heart Association functional class greater than II or cyanosis, left-heart obstruction (mitral valve area <2 cm2, aortic valve area <1.5 cm2, or left ventricular outflow tract gradient >30 mmHg), and left ventricular ejection fraction (LVEF) < 0.40. Zero points confers a 5% risk of cardiac complications, 1 point a 27% risk, and 2 or more points a 75% risk.
TABLE I. Cardiac Disease in Pregnancy (CARPREG) Risk Score*
High Cardiac Risk Pregnancy States
Contraindications to pregnancy generally consist of 4 states7: Marfan syndrome with dilated aortic root (>4 cm), pulmonary hypertension (pulmonary vascular resistance, >6 Wood units), moderate-to-severe left ventricular outflow tract obstruction (≥30 mmHg), and LVEF < 0.30 (Table II). If a woman with one of these conditions becomes pregnant, early consultation with a maternal-fetal medicine specialist and a cardiologist should be done in order to evaluate the patient's risk and develop the plan of care. Pregnancy with pulmonary hypertension (Fig. 1) confers a prohibitively high cardiac risk and carries a combined maternal and fetal mortality rate that approaches 50%. Termination of pregnancy should be considered in this condition.7
TABLE II. Contraindications for Pregnancy
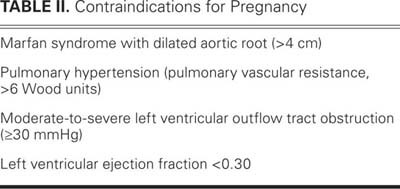
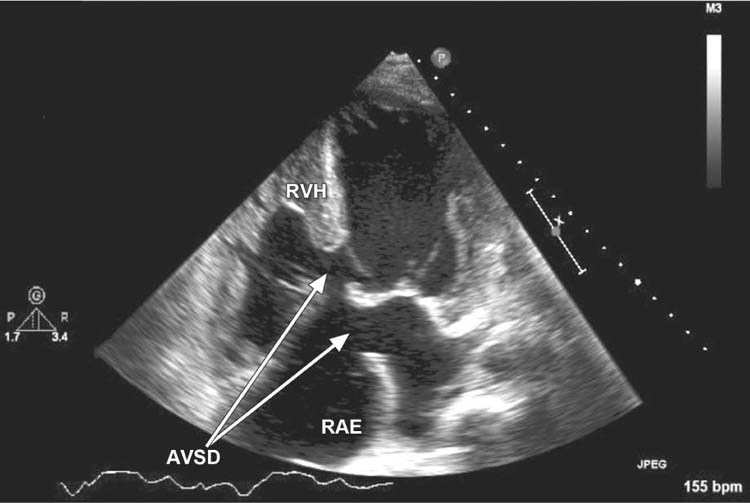
Fig. 1 Transthoracic echocardiogram (apical 4-chamber view) shows complete atrioventricular canal defect with secondary pulmonary hypertension. Note the large atrioventricular septal defect (AVSD), right ventricular hypertrophy (RVH), and right atrial enlargement (RAE).
Peripartum Cardiomyopathy
Peripartum cardiomyopathy is defined as a dilated cardiomyopathy with congestive heart failure within the last month of pregnancy or within 5 months of delivery.8 This condition occurs at a rate of 1 in 2,289 live births and risk factors are multiparity, advanced maternal age, preeclampsia, gestational hypertension, and African descent. Some studies show a 75% recovery rate to normal ventricular function.9 Animal studies have suggested that a prolactin metabolite associated with peripartum cardiomyopathy can be cardiotoxic and that treatment with bromocriptine may be beneficial.10 Although the cause is not well understood, the treatment remains similar to that for congestive heart failure patients in general.
Conclusion
Successful pregnancies can be achieved when cardiac complications are managed during pregnancy. In order to optimize maternal and neonatal outcomes, close collaboration between the maternal-fetal medicine specialist and the cardiologist is important.
Footnotes
Address for reprints: Wayne J. Franklin, MD, FACC, Section of Cardiology, Texas Children's Hospital, 6621 Fannin St., MC 19-345C, Houston, TX 77030. E-mail: wjf@bcm.edu
Presented at the Risk, Diagnosis and Treatment of Cardiovascular Disease in Women symposium; Denton A. Cooley Auditorium, Texas Heart Institute, Houston; 11 September 2010.
References
- 1.Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA, et al. ACC/AHA 2008 Guidelines for the Management of Adults with Congenital Heart Disease: Executive Summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to develop guidelines for the management of adults with congenital heart disease). Circulation 2008;118(23):2395–451. [DOI] [PubMed]
- 2.Bates SM, Greer IA, Pabinger I, Sofaer S, Hirsh J; American College of Chest Physicians. Venous thromboembolism, thrombophilia, antithrombotic therapy, and pregnancy: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th ed.). Chest 2008;133(6 Suppl): 844S-886S. [DOI] [PubMed]
- 3.Roth A, Elkayam U. Acute myocardial infarction associated with pregnancy. J Am Coll Cardiol 2008;52(3):171–80. [DOI] [PubMed]
- 4.Khairy P, Ouyang DW, Fernandes SM, Lee-Parritz A, Economy KE, Landzberg MJ. Pregnancy outcomes in women with congenital heart disease. Circulation 2006;113(4):517–24. [DOI] [PubMed]
- 5.Drenthen W, Pieper PG, Roos-Hesselink JW, van Lottum WA, Voors AA, Mulder BJ, et al. Outcome of pregnancy in women with congenital heart disease: a literature review. J Am Coll Cardiol 2007;49(24):2303–11. [DOI] [PubMed]
- 6.Siu SC, Sermer M, Colman JM, Alvarez AN, Mercier LA, Morton BC, et al. Prospective multicenter study of pregnancy outcomes in women with heart disease. Circulation 2001;104 (5):515–21. [DOI] [PubMed]
- 7.Bowater SE, Thorne SA. Management of pregnancy in women with acquired and congenital heart disease. Postgrad Med J 2010;86(1012):100–5. [DOI] [PubMed]
- 8.Demakis JG, Rahimtoola SH. Peripartum cardiomyopathy. Circulation 1971;44(5):964–8. [DOI] [PubMed]
- 9.Amos AM, Jaber WA, Russell SD. Improved outcomes in peripartum cardiomyopathy with contemporary. Am Heart J 2006;152(3):509–13. [DOI] [PubMed]
- 10.Pyatt JR, Dubey G. Peripartum cardiomyopathy: current understanding, comprehensive management review and new developments. Postgrad Med J 2011;87(1023):34–9. [DOI] [PubMed]


