Abstract
We report that a toxin neutralization assay (TNA) can detect a decrease in the immunogenicity of anthrax vaccines as a consequence of brief exposure to elevated temperature. This attribute of TNA may help in adopting immunogenicity as a replacement of the current potency test, which involves protection from lethal challenge.
All anthrax vaccine that enters the Strategic National Stockpile must maintain its potency through protracted storage periods. Thus, robust, practical, and meaningful potency tests are essential to evaluate vaccine manufacturing consistency and stability. The stability of protective antigen (PA), a major antigen included in anthrax vaccines, is critical to establish the suitability of a formulation for long-term storage. PA is denatured at temperatures as low as 40°C (4, 7, 9), which can jeopardize vaccine potency if the product is heated at any time prior to its administration, even during manufacturing. The current potency assay for anthrax vaccines is an active protection test that consumes many animals and requires security and biosafety measures because of the use of virulent Bacillus anthracis. To circumvent these drawbacks, immunogenicity assays have been developed in which lethal challenge is replaced with the measurement of differential antibody induction using in vitro tests.
We assessed whether a toxin neutralization assay (TNA) can detect changes in antibody response as a consequence of the exposure of an experimental recombinant PA vaccine (rPAV) and BioThrax, a commercial vaccine, to high temperatures for brief periods. The number of possible time/temperature combinations to which a vaccine can be exposed before use is very high. Therefore, we selected a few combinations to model the possibility of using murine immunogenicity to detect anthrax vaccine exposure to nonideal storage conditions.
We used a published method (3), slightly modified, to measure neutralizing activity in mouse sera. The reference serum and samples were prediluted with Dulbecco's modified Eagle medium (DMEM) and serially diluted (1:2) in a 96-well microtiter plate. Predilution was made to achieve full neutralization curves, i.e., to obtain upper and lower asymptotes. Lethal toxin (LT; 100 ng/ml of PA plus 80 ng/ml of lethal factor in DMEM) was added, and mixtures were incubated (37°C and 5% CO2) for 30 min. One well in each column contained only the sample at the lowest dilution tested (sample control [SC]). One column contained normal mouse serum diluted 1:25 in DMEM. Toxin activity was confirmed by the addition of LT to four wells (LT control), while four wells were used to verify cell viability (reagent control). Toxin-serum mixtures were added to J774A.1 cells seeded in a second 96-well plate (40% to 60% confluence) and incubated (37°C and 5% CO2) for 4 h. Cell viability was estimated with a vital dye, MTT [3-(4,5-dimethyl-2-thiazolyl)-2,5-diphenyl-2H-tetrazolium bromide] (2). The absorbance per well (determined as the change in optical density [ΔOD] at 570 and 690 nm) was transformed to the percentage of neutralization (N%) as follows: N% = 100(OD − ODmin/ODmax − ODmin), where ODmax and ODmin represent the maximum and minimum ΔOD, respectively, in each titration curve. For incomplete curves (no upper asymptote), SC's ΔOD was used as ODmax. Four-parameter logistic regression was performed, constraining the upper and lower asymptotes to 100% and 0% neutralization, respectively.
TNA validity was assessed using the following criteria: the average ΔOD for LT control wells should be <0.4, and the average ΔOD for reagent control wells should be >0.8. The reference curve should have an ODmax of >0.8 and an ODmin of <0.4, and the value of ODmax minus ODmin should be >0.8. The coefficient of determination (r2) for the reference should be ≥0.99. The percent coefficient of variation (%CV) of the two ΔOD values at each dilution of the reference curve must be less than 25%.
Samples with an ODmax of ≤0.4 were considered to have 0% neutralization. Nonmonotonic response at the upper plateau was eliminated by imputing 100% neutralization to dilutions lower than those corresponding to an ODmax that gave a lower ΔOD reading. Parallelism was assessed by the r2 (6) and the dilution effect (DE) method (5). The neutralizing activity (U/ml) for samples that met either parallelism criterion was calculated by multiplying the neutralization factor (NF50 = ED50 sample/ED50 reference, where ED50 represents the reciprocal of the dilution corresponding to 50% neutralization read from each fitted curve [sample and reference serum]) by the activity of the reference serum (MR02-2; 713 U/ml), which is an anti-PA, freeze-dried, immunoglobulin-enriched preparation obtained by immunizing mice multiple times with an experimental rPAV (1).
Initially, we measured the toxin-neutralizing activity in serum samples collected 28 days postimmunization from two groups of mice immunized with a single dose of either BioThrax (0.2 ml intraperitoneally [i.p.]) or rPAV (formulated at 25°C; 3 μg i.p.) and from two groups immunized with each vaccine heated at 100°C for 2 min. We found significant decreases (rPAV, P = 0.004, and BioThrax, P < 0.0001 [Student's t test]) in immunogenicity in the groups immunized with the heated vaccines (Fig. 1). Interestingly, BioThrax incubated at 100°C for 2 min (Fig. 1, Biothrax-100) elicited neutralizing titers that were similar to the neutralizing titers elicited by unheated rPAV (Fig. 1, rPAV-RT). This effect can be attributed to a larger amount of PA in BioThrax (its exact content is unknown) or to the presence of other antigens in this vaccine that may induce a neutralizing response.
FIG. 1.
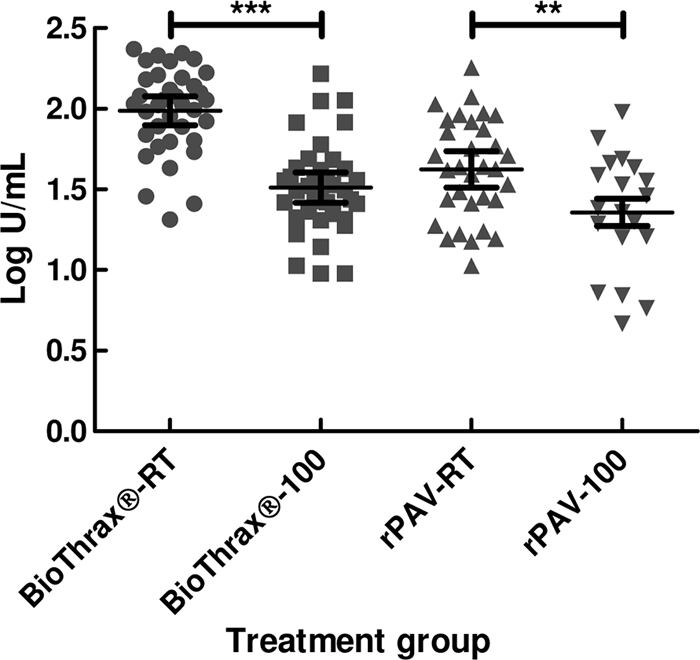
Serum PA-neutralizing activity in mice (40 animals per group) immunized with anthrax vaccines subjected to high temperature. Vaccines were heated at 100°C for 2 min. RT, control group (BioThrax stored at 2 to 8°C or rPAV freshly formulated at 25°C); 100, exposure to 100°C. Log10 neutralizing activity (U/ml) is shown on the y axis. Pairs of mean log10 neutralizing activities by vaccine type were compared by Student's t test. **, P < 0.01; ***, P < 0.001. The central horizontal line in each group represents the mean of the log10 neutralizing activities (U/ml), and the two additional horizontal lines represent the limits of the 95% confidence interval (CI) for each estimate. Activities in U/ml (95% CI): BioThrax-RT, 97.9 (78.6 to 115.03); BioThrax-100, 32.4 (26.1 to 40.3); rPAV-RT, 44.4 (34.4 to 57.1); rPAV-100, 21.8 (14.7 to 32.4).
To study the effects of exposure to milder temperatures, we performed a supplementary experiment using 45°C and 70°C, keeping 100°C as a positive control. We found an inversely proportional decrease in immunogenicity with each temperature relative to that elicited by untreated rPAV (Fig. 2 A) (45°C, P = 0.049; 70°C, P = 0.011; and 100°C, P < 0.001 [Dunnett's test]). While Reuveny et al. (8) showed that exposure of rPAV to 40°C during 6 days caused a 3-fold decrease of its immunogenicity in guinea pigs, as measured by TNA, we could detect exposure to an analogous temperature for a period as brief as 2 min. Remarkably, relatively elevated neutralizing immunogenicity remained even after exposure of the vaccines to the highest temperature tested (100°C).
FIG. 2.

Serum PA-neutralizing activities in mice immunized with rPAV subjected to different temperatures (20 animals per group). Vaccines were heated at the indicated temperatures (°C, on the x axis) for 2 min. RT, control group (freshly formulated rPAV at 25°C). Log10 neutralizing activity (U/ml) is shown on the y axis. (A) Serum activities, excluding nonparallel curves, according to the DE method. (B) Serum activities, excluding nonparallel curves, according to the r2 method. Mean log10 neutralizing activities were compared by Dunnett's multiple comparison test, using the RT group as the control group. *, P < 0.05; ***, P < 0.001. Activities in U/ml (95% CI): (A) RT, 37.1 (26.9 to 51.3); 45, 20.6 (14.0 to 30.2); 70, 17.4 (12.9 to 23.3); and 100, 13.0 (7.4 to 22.9); (B) RT, 29.8 (19.3 to 46.0); 45, 21.3 (14.6 to 31.1); 70, 14.8 (11.3 to 19.5); and 100, 13.9 (8.3 to 23.2).
The responses induced by heated vaccines generated titration curves that were nonparallel to the reference curve more often than those corresponding to untreated vaccine (Table 1). This was most prominent at the highest temperatures. When the r2 method was used to evaluate parallelism, significant decreases in immunogenicity were detected only at 70°C and 100°C (Fig. 2B) (45°C, P = 0.456; 70°C, P = 0.029; and 100°C, P = 0.019 [Dunnett's test]). The nonparallelism of antibody titration curves may be additional, albeit indirect evidence of structural alterations of PA.
TABLE 1.
Samples excluded from analysis, by treatment group
The data presented herein, along with results obtained by other authors (4, 8, 10), support the concept that TNA can quantify differences among anthrax vaccine batches that have been altered by exposure to high temperature during storage. However, these experiments represent only a first step toward the development of an alternative potency test for anthrax vaccines, based on their immunogenicity for the mouse. Further refinements of the procedure will include assigning unitage to a standard reference serum, the production of a reference vaccine, and the establishment of acceptance criteria based on the behavior of vaccine lots that have been shown to be efficacious in the target population.
Acknowledgments
This project was supported by the Biomedical Advanced Research and Development Authority and by J.C.-V.'s appointment to the Research Participation Program at the Center for Biologics Evaluation and Research administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and the U.S. Food and Drug Administration. J.C.-V. is also grateful for the support from COTEPABE and the Instituto Politécnico Nacional (México). L.S. was supported in part by a CBER director's Critical Path grant.
We thank L. Wagner, J. Keller, D. Horne, and B. Meade for their useful comments and critical reading of the manuscript. BioThrax was kindly provided by the Division of Scientific Resources, National Center for Preparedness, Detection and Control of Infectious Diseases, CDC (Atlanta, GA). rPA (lot NR-140) and recombinant LF (rLF; lot NR-142) were provided by NIH/NIAID's Biodefense and Emerging Infections Research Resources Repository (BEI Resources).
The findings and conclusions in this article have not been formally disseminated by the Food and Drug Administration and should not be construed to represent any Agency determination or policy.
Footnotes
Published ahead of print on 8 December 2010.
REFERENCES
- 1.Berthold, I., M. Pombo, L. Wagner, and J. L. Arciniega. 2005. Immunogenicity in mice of anthrax recombinant protective antigen in the presence of aluminum adjuvants. Vaccine 23:1993-1999. [DOI] [PubMed] [Google Scholar]
- 2.Hansen, M. B., S. E. Nielsen, and K. Berg. 1989. Re-examination and further development of a precise and rapid dye method for measuring cell growth/cell kill. J. Immunol. Methods 119:203-210. [DOI] [PubMed] [Google Scholar]
- 3.Hering, D., et al. 2004. Validation of the anthrax lethal toxin neutralization assay. Biologicals 32:17-27. [DOI] [PubMed] [Google Scholar]
- 4.Jiang, G., et al. 2006. Anthrax vaccine powder formulations for nasal mucosal delivery. J. Pharm. Sci. 95:80-96. [DOI] [PubMed] [Google Scholar]
- 5.Klein, J., et al. 1999. Validation of assays for use with combination vaccines. Biologicals 27:35-41. [DOI] [PubMed] [Google Scholar]
- 6.Li, H., et al. 2008. Standardized, mathematical model-based and validated in vitro analysis of anthrax lethal toxin neutralization. J. Immunol. Methods 333:89-106. [DOI] [PubMed] [Google Scholar]
- 7.Radha, C., P. Salotra, R. Bhat, and R. Bhatnagar. 1996. Thermostabilization of protective antigen—the binding component of anthrax lethal toxin. J. Biotechnol. 50:235-242. [DOI] [PubMed] [Google Scholar]
- 8.Reuveny, S., et al. 2001. Search for correlates of protective immunity conferred by anthrax vaccine. Infect. Immun. 69:2888-2893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singh, S., et al. 2002. Gln277 and Phe554 residues are involved in thermal inactivation of protective antigen of Bacillus anthracis. Biochem. Biophys. Res. Commun. 296:1058-1062. [DOI] [PubMed] [Google Scholar]
- 10.Singh, S., et al. 2004. Thermal inactivation of protective antigen of Bacillus anthracis and its prevention by polyol osmolytes. Biochem. Biophys. Res. Commun. 322:1029-1037. [DOI] [PubMed] [Google Scholar]


