Abstract
The transmission of simian immunodeficiency and Ebola viruses to humans in recent years has heightened awareness of the public health significance of zoonotic diseases of primate origin, particularly from chimpanzees. In this study, we analyzed 71 fecal samples collected from 2 different wild chimpanzee (Pan troglodytes) populations with different histories in relation to their proximity to humans. Campylobacter spp. were detected by culture in 19/56 (34%) group 1 (human habituated for research and tourism purposes at Mahale Mountains National Park) and 0/15 (0%) group 2 (not human habituated but propagated from an introduced population released from captivity over 30 years ago at Rubondo Island National Park) chimpanzees, respectively. Using 16S rRNA gene sequencing, all isolates were virtually identical (at most a single base difference), and the chimpanzee isolates were most closely related to Campylobacter helveticus and Campylobacter upsaliensis (94.7% and 95.9% similarity, respectively). Whole-cell protein profiling, amplified fragment length polymorphism analysis of genomic DNA, hsp60 sequence analysis, and determination of the mol% G+C content revealed two subgroups among the chimpanzee isolates. DNA-DNA hybridization experiments confirmed that both subgroups represented distinct genomic species. In the absence of differential biochemical characteristics and morphology and identical 16S rRNA gene sequences, we propose to classify all isolates into a single novel nomenspecies, Campylobacter troglodytis, with strain MIT 05-9149 as the type strain; strain MIT 05-9157 is suggested as the reference strain for the second C. troglodytis genomovar. Further studies are required to determine whether the organism is pathogenic to chimpanzees and whether this novel Campylobacter colonizes humans and causes enteric disease.
Humans are coming into closer proximity with wild primates for a variety of reasons, including habitat fragmentation and loss from deforestation, forest encroachment, competition for food and natural resources, bushmeat hunting, and expanding research and ecotourism activities. Evidence that humans and great apes are exchanging microorganisms due to socioecological practices and ecological overlap is accumulating at an alarming rate. Unknowingly, they may become links in each others' host-pathogen cycles. Infectious disease transmission from humans to chimpanzees (Pan troglodytes) and gorillas (Gorilla gorilla), in particular, is becoming more of a concern, with the Red List from the World Conservation Union (IUCN) classifying them as endangered and critically endangered species, respectively, and with pathogenic organisms undoubtedly expected to contribute to declines in wild ape populations and possibly even to contribute to species decimation (21, 23, 27, 54, 55, 57).
Surveillance and reporting of known, uncommon, and new infectious agents in wild primate populations are increasingly important. In 2001, campylobacteriosis, salmonellosis, and shigellosis in free-ranging human-habituated mountain gorillas in Uganda were reported (33). In 2007, Escherichia coli strains isolated from habituated chimpanzees were genetically more similar to isolates obtained from humans employed in chimpanzee research and tourism than to E. coli isolates obtained from humans in a local village with no regular interactions with these chimpanzees (10).
In our study, we cultured feces for Campylobacter species in 2 groups of wild chimpanzees residing in different National Parks in Tanzania. One group has lived in close proximity to humans studying their behavior and ecology for over 40 years, and in more recent years, to humans involved in ecotourism activities (32). The second group is not habituated to humans and does not tolerate contact with humans for any length of time. It is comprised of chimpanzees once held in captivity and introduced into the wild in the late 1960s and/or their offspring. In this report, we characterize by phenotypic, genotypic, and phylogenetic analyses a novel species of Campylobacter, Campylobacter troglodytis, which was isolated from the feces of human-habituated chimpanzees.
MATERIALS AND METHODS
Animals.
Two different groups of wild chimpanzees (Pan troglodytes) from Tanzania National Parks were studied. Group 1 consisted of individually identified chimpanzees (Pan troglodytes schweinfurthii) that reside in the Mahale Mountains National Park in western Tanzania (latitude 6°S, longitude 30°E). They belong to the M group, a group of chimpanzees that have been reported to have loose stools with fluid consistency over the past 14 years and intermittent respiratory illnesses (12, 20, 32). The M group is habituated to human presence and tolerates observation from close proximity for extended periods. They are regularly observed by local trackers and guides, as well as tourists and researchers from around the world. The M group was once comprised of 101 individuals and is now estimated to contain only 63 individuals (21, 32). At the time of the study, there were no clinical signs of disease in group 1. Chimpanzees in group 2 live in Rubondo Island National Park, which is surrounded by Lake Victoria (latitude 2°S, longitude 31°E). They originated from a group of 17 chimpanzees that were released from captivity between 1966 and 1969. All 17 introduced chimpanzees were born in the wild, but prior to their release, they were reportedly housed for between 3.5 months and 9 years in various European zoos. There has been little to no human contact with these animals since the time of their release, and they do not tolerate observation or close proximity to humans for any period of time. Most of the group 2 chimpanzees cannot be individually recognized. Group 2 chimpanzees have been reported to have intermittent loose and watery stools during the past several years. The studies were approved by the Institutional Animal Care and Use Committee.
Fecal samples.
All feces were collected noninvasively as part of a long-term chimpanzee health-monitoring program. Only fresh, uncontaminated feces were collected from the forest floor. Fecal consistency was recorded as firm, loose, or watery, and fecal occult blood testing was performed on each sample using Hemoccult tests (Beckman Coulter, Fullerton, CA). A total of 71 fecal samples were obtained. From group 1, during June 2005, 56 samples were collected from 29 individuals: 13 males (7 adults, 4 adolescents, and 2 juveniles) and 16 females (8 adults, 3 adolescents, and 5 juveniles); their feces were collected immediately after the chimps were observed defecating to preclude contamination. From group 2, 15 fecal samples were collected on 6 different days between August 2004 and February 2005. Only fresh feces (none older than 12 h) were collected where chimpanzee origin was confirmed by directly observing defecation, finding feces directly under chimpanzee night nests, or immediate chimpanzee tracking after chimpanzee vocalization and subsequent collection without direct observation of defecation. Of the 15 samples from group 2, 8 were collected from different individuals who were directly observed defecating at one tracking location during a single sighting of 11 chimpanzees. In an adjacent but different tracking location, 3 other samples were collected on a single day from under 3 different chimpanzee night nests. Two samples were collected from 2 distant tracking locations and were more than likely from 2 different individual chimpanzees. In one case, chimps were heard vocalizing and were tracked, and a sample was obtained without directly observing the individual defecating or finding the specimen directly under a night nest. Since this population is not habituated, genders and age groups for the samples are not known, and although highly unlikely, it is possible that the same individual was sampled more than once.
Using a clean wooden applicator stick, a small amount of feces, approximately the size of a small grape, from each sample was placed in a 1-dram vial prefilled with brucella broth with 20% glycerol. The fecal sample was totally submerged, and the vial caps were tightened completely. The vials were stored frozen at approximately −20°C in a solar-powered freezer. The freezer was closed tightly and padlocked. The freezer temperature was monitored and recorded using freezer minimum-maximum thermometers. Frozen samples were transported on dry ice to the United States for analysis at the Division of Comparative Medicine, Massachusetts Institute of Technology.
Bacterial isolation and biochemical characterization.
Feces were homogenized in 1 ml of phosphate-buffered saline (PBS), and aliquots were placed on CVA (cefoperzone, vancomycin, and amphotericin B) plates or TVP (trimethoprim, vancomycin, and polymyxin) plates and filtered through a 0.45-μm filter onto Trypticase soy agar plates with 5% sheep blood. Selective-medium plates were also used and were prepared as follows: blood agar base (Oxoid; Remel), 5% horse blood (Quad Five, Ryegate, MT), 50 μg amphotericin B/ml, 100 μg vancomycin/ml, 3.3 μg polymyxin B/ml, 200 μg bacitracin/ml, and 10.7 μg nalidixic acid/ml. After incubation under microaerobic conditions (the culture vessels were evacuated to 25 in. of mercury and filled with 80:10:10 N2-CO2-H2) at 37°C, suspect colonies were identified as presumptive campylobacter based on colony morphology, biochemical reactions, phase microscopy, and Gram staining.
Biochemical characterization of urease, catalase, and oxidase production, as well as sensitivity to nalidixic acid and cephalothin, were conducted as previously described by our laboratory (48). For other tests, the inoculum size was adjusted to 106 CFU/ml, and bacteria were grown on a basal medium of brucella agar supplemented with 5% horse blood according to the method of On and Holmes (36). Tests for growth in the presence of 1% bile, 1% glycine, 0.1% selenite, 0.04% triphenyltetrazolium chloride (TTC), and salt were conducted as described by On and Holmes (36). The method of Hwang and Ederer (14) was used for hippurate hydrolysis. Nitrate reduction was conducted according to the method of Cook (4). Discs were used for indoxyl acetate hydrolysis (35) and also for alkaline phosphatase production (Rosco Diagnostica, Denmark). All cultures were incubated for 3 days in a microaerobic environment. Control cultures were Campylobacter jejuni 81-176 (bile, salt, hippurate, selenite, TTC, nitrate, glycine, and growth at 42°C), Helicobacter canis type strain (alkaline phosphatase), Helicobacter cinaedi type strain (alkaline phosphatase), Helicobacter pylori SS1 (bile, salt, hippurate, selenite, TTC, nitrate, glycine, and growth at 42°C), and Campylobacter coli (hippurate hydrolysis). Data for the reference species were taken from On et al. (37), Debruyne et al. (5), Zanoni et al. (59), and Rossi et al. (42).
Genomic-DNA extraction for rRNA gene sequencing.
For PCR of genomic DNA, isolates were grown on blood agar plates, harvested, and washed once with PBS, and a High Pure PCR template preparation kit (Roche Molecular Biochemicals) was used for DNA extraction according to the manufacturer's specifications.
Genus-specific PCR.
Campylobacter genus-specific primers that amplified a 280-base product on the 16S rRNA gene were used as previously described (47).
16S rRNA sequence analysis.
Amplification of the 16S rRNA cistrons, 16S rRNA gene sequencing, and analysis of the 16S rRNA data were performed as described elsewhere (6, 38). For alignment, the 16S rRNA gene sequences were entered into RNA, a program designed and maintained at Forsyth Institute for analysis of 16S rRNA. The database contains over 600 sequences for Helicobacter, Wolinella, Arcobacter, and Campylobacter strains and >2,000 sequences for other bacteria.
Whole-cell protein profiling.
Strains were grown on Mueller-Hinton agar supplemented with 5% sterile horse blood and incubated at 37°C for 48 h under microaerobic conditions. Protein extraction and SDS-PAGE were performed as described by Pot et al. (41). The similarity of the obtained normalized SDS-PAGE patterns was determined by the Pearson correlation coefficient, and clustering was performed by the unweighted pair group method with arithmetic mean (UPGMA), using BioNumerics software version 5.0 (Applied Maths).
AFLP analysis.
Amplified fragment length polymorphism (AFLP) analysis using the restriction enzyme combination HindIII/HhaI was performed as described previously (5). The amplified and fluorescently labeled fragments were loaded on a denaturing polyacrylamide gel on an ABI Prism 377 automated sequencer. GeneScan version 3.1 software (Applied Biosystems) was used for data collection, and the generated profiles were imported, using the CrvConv filter, into BioNumerics version 4.61 (Applied Maths, Belgium) for normalization and further analysis. After normalization, the obtained AFLP profiles were imported into an in-house AFLP reference database containing profiles from type and reference strains of all established Campylobacter species. The similarity between profiles was determined by the Pearson correlation coefficient, and cluster analysis was performed by UPGMA.
hsp60 sequence analysis.
hsp60 sequences were generated as described previously (5, 19). For tree construction, sequences were aligned using the ClustalX software package (51), and clustering was performed by the neighbor-joining method (45) using BioNumerics v. 5.1. Unknown bases were discarded for the analysis. Bootstrap values were determined using 500 replicates.
DNA-DNA hybridization experiments.
DNA-DNA hybridizations were performed between strains MIT 05-9149T and MIT 05-9157. DNA was extracted from 0.25 to 0.5 g (wet weight) cells as described by Pitcher et al. (40). DNA-DNA hybridizations were performed with photobiotin-labeled probes in microplate wells (7) using an HTS7000 Bio Assay Reader (Perkin Elmer) for the fluorescence measurements. The hybridization temperature was 30°C.
Determination of mol% G+C content.
For the determination of the mol% G+C content, DNA was enzymatically degraded into nucleosides as described by Mesbah and Whitman (30). The nucleoside mixture was separated by high-performance liquid chromatography (HPLC) using a Waters SymmetryShield C8 column maintained at 37°C. The solvent was 0.02 M (NH4)H2PO4 (pH 4.0) with 1.5% acetonitrile. Nonmethylated λ phage DNA (Sigma) was used as the calibration reference.
Electron microscopy.
Isolates identified as C. troglodytis were examined by electron microscopy. Cells grown on blood agar for 48 h were gently suspended in 10 mM Tris-HCl buffer (pH 7.4) at a concentration of about 108 cells per ml. Samples were negatively stained with 1% (wt/vol) phosphotungstic acid (pH 6.5) for 20 to 30 s. Specimens were examined with a Jeol model JEM-1200EX transmission electron microscope operating at 100 kV.
Nucleotide sequence accession numbers.
The 16S rRNA and hsp60 sequence accession numbers in GenBank for the C. troglodytis sp. nov. type strain (MIT 05-9149) are HQ864828 and FN421420, respectively.
RESULTS
Prevalence of Campylobacter spp. in group 1 and group 2.
All fecal samples were firm in consistency, except for 6 in group 1, which were loose. Of these 6, two were positive for the novel campylobacter (Table 1). Thirty-one of the 56 samples in group 1 were positive for fecal occult blood, 4 of which tested positive for the novel campylobacter (Table 1). The age groups and genders of chimpanzees positive for the novel campylobacter are provided in Table 1. All group 2 fecal samples were firm in consistency; 4 of the 15 samples were positive for occult blood, 10 were negative, and 1 sample was not tested.
TABLE 1.
Consistencies and occult blood test results by age group and gender for stools testing positive for C. troglodytis
| Accession no. | Age groupa | Gender | Stool consistencyb | Fecal occult blood test result |
|---|---|---|---|---|
| 05-9149 (no. 3) | Adult | Female | Firm | Positive |
| 05-9150 (no. 4) | Adult | Female | Firm | Positive |
| 05-9156 (no. 10) | Infant | Female | Loose | Negative |
| 05-9157 (no. 11) | Adult | Male | Firm | Positive |
| 05-9159 (no. 13) | Adolescent | Male | Firm | Negative |
| 05-9164 (no. 18) | Juvenile | Female | Loose | Positive |
Age groups: infant (0 to 3 years), juvenile (4 to 8 years), adolescent (9 to 14 years), and adult (>15 years) (32).
Stool consistency was reported as firm, loose, or runny.
Of the 56 samples collected from chimpanzees at the Mahale Mountains National Park (group 1), 19 and 49 were Campylobacter positive by culture and PCR analyses, respectively. Although 8 samples from chimpanzees at Rubondo Island (group 2) tested positive for Campylobacter by PCR, all samples were negative for Campylobacter spp. by culture.
Biochemical characterization.
All isolates were positive for catalase, oxidase, alkaline phosphatase, growth at 37 and 42°C, growth on 1% glycine, and sensitivity to nalidixic acid (Table 2). All isolates were negative for urease, growth at 25°C, and growth on 3% NaCl. Most isolates were positive for growth on triphenyltetrazolium chloride (9/11), and 9/11 isolates were also negative for selenite reduction and growth on 2% NaCl and on 2% bile. Eight of 10 were negative for indoxyl acetate, and 7/10 were negative for nitrate reduction. Only 1 isolate was sensitive to cephalothin. Taking into account variable reactions, similar results for biochemical tests were shared with C. jejuni, Campylobacter hyointestinalis (both subspecies), Campylobacter lari, Campylobacter rectus, and Campylobacter sputorum. It is notable that 3 isolates of C. troglodytis were positive for hippurate hydrolysis.
TABLE 2.
Biochemical comparison of C. troglodytis and other Campylobacter spp.a
| Campylobacter sp. | Catalase | Oxidase | Urease | Nitrate reduction | Alkaline phosphatase | Indoxyl acetate hydrolysis | Growth at 25°C | Growth at 37°C | Growth at 42°C | Hippurate hydrolysis | Growth in 1% glycine | Growth in 1% bile | Growth in 2% NaCl | Selenite reduction | Growth on TTC | Sensitive to nalidixic acid (30 μg) | Sensitive to cephalothin (30 μg) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C. troglodytis | + (11/11) | + (11/11) | − (11/11) | − (7/11) | + (11/11) | − (8/10) | 0/11 | 11/11 | 11/11 | − (8/11) | + (11/11) | − (9/11) | − (9/11) | − (9/11) | + (9/11) | 10/10 | 1/10 |
| C. avium | weak | + | − | + | − | + | − | + | + | + | − | V | − | − | − | + | − |
| C. canadensis | V | + | V | V | − | − | − | + | + | − | V | M | ND | ND | ND | V | + |
| C. cuniculorum | + | + | − | + | − | + | − | + | M | − | − | V | − | − | V | V | F |
| C. coli | + | + | − | + | − | + | − | + | + | − | + | M | − | V | + | + | − |
| C. consisus | − | V | − | F | V | − | − | + | M | − | F | − | F | F | − | M | + |
| C. curvis | − | + | − | + | V | V | − | Vc | V | F | + | − | V | − | V | − | + |
| C. fetus subsp. fetusb | + | + | − | + | − | − | + | + | M | − | + | + | − | M | − | V | + |
| C. fetus subsp. veneralis | M | + | − | + | − | − | + | + | − | − | − | + | − | − | − | F | + |
| C. gracilis | V | − | − | M | − | V | − | −c | V | − | + | − | V | − | − | V | + |
| C. helveticus | − | + | − | + | − | + | − | + | + | − | V | + | − | − | − | + | + |
| C. hominis | − | + | − | − | − | − | − | + | F | − | + | ND | + | − | ND | V | + |
| C. hyointestinalis subsp. hyointestinalis | + | + | − | + | − | − | − | + | + | − | + | + | − | + | − | − | M |
| C. hyointestinalis subsp. lawsonni | + | + | − | + | F | − | − | + | + | − | V | M | − | + | − | − | + |
| C. insulaenigrae | + | + | − | + | ND | − | − | + | − | − | + | ND | − | ND | ND | − | − |
| C. jejuni subsp. doyleib | V | + | − | − | − | + | − | + | − | + | F | + | − | − | V | + | + |
| C. jejuni subsp. jejuni | + | + | − | + | − | + | − | + | + | + | + | + | − | + | + | + | − |
| C. lanienae | + | + | − | + | + | − | − | + | + | − | − | ND | − | + | ND | − | − |
| C. lari | + | + | V | + | − | − | − | + | + | − | + | + | M | + | + | V | − |
| C. lari subsp. concheus | + | ND | ND | ND | ND | ND | ND | ND | + | + | + | + | − | ||||
| C. mucosalis | − | + | − | − | M | − | − | + | + | − | V | + | + | − | − | F | + |
| C. peloridis | + | ND | ND | ND | ND | ND | ND | ND | + | − | + | ND | M | ND | ND | M | M |
| C. rectus | F | + | − | + | − | + | − | −c | F | − | + | − | V | + | − | F | + |
| C. showae | + | V | − | + | − | − | − | Vc | V | − | V | − | + | + | − | + | + |
| C. sputorum | V | + | Vb | + | − | − | − | + | + | − | + | V | + | + | − | F | + |
| C. upsaliensis | − | + | − | + | − | + | − | + | + | − | + | + | − | + | V | + | M |
+, 90 to 100% of strains positive; −, 0 to 10% of strains positive; F, 11 to 25% of strains positive; V, 26 to 74% of strains positive; M, 75 to 89% of strains positive; ND, not determined. Data for reference species were taken from Lawson et al. (26), Logan et al. (28), On et al. (37), Foster et al. (8), Debruyne et al. (5), Rossi et al. (42), Stanley et al. (50), and Zanoni et al. (59).
Strains of biovar paraureolyticus are urease positive; others are negative (34).
These strains grow at 37°C under anaerobic conditions.
16S rRNA sequence analysis.
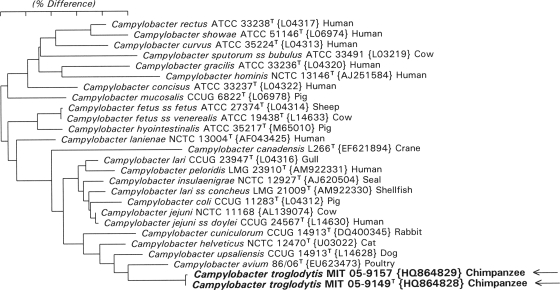
Using DNA extracted from the culture, the16S rRNA gene was amplified and sequenced for 6 out of the 17 samples that tested positive by both culture and PCR. Analyses showed novel gene sequences in all 6, with all strains being essentially identical; 2 isolates differed only by a single base. Phylogenetic relationships based on 16S rRNA sequence similarity values are shown in Fig. 1. By 16S rRNA analysis, the novel campylobacter was most closely related to the named species Campylobacter helveticus and Campylobacter upsaliensis (94.7% and 95.9% similarity). It is also related to two unclassified Campylobacter isolates from hamsters and cotton topped tamarins (95.5% and 95.2% similarity; unpublished observations), forming a distinct subcluster in the campylobacter phylogenetic tree, as shown in Fig. 1.
FIG. 1.
Phylogenetic tree constructed from the 16S rRNA sequence similarity values. The scale bar represents 5% difference in nucleotide sequences, determined by measuring the lengths of the horizontal lines connecting two species.
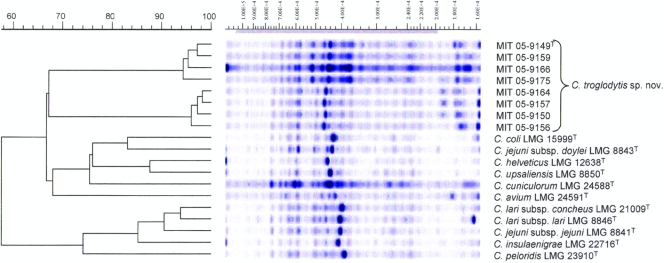
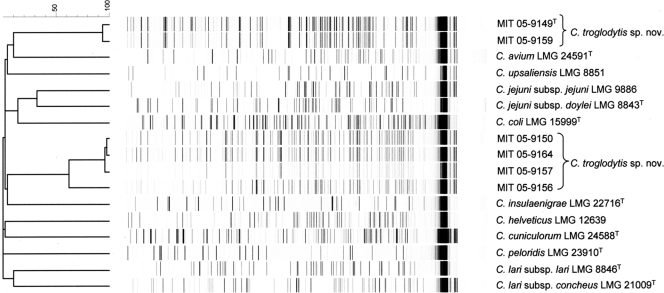
Whole-cell protein and AFLP fingerprinting.
The six strains included in the biochemical analyses and an additional two strains were chosen for whole-cell protein and AFLP fingerprinting. Data for Campylobacter reference strains were available from previous studies (5). Unexpectedly, the protein profiles of the eight strains revealed the presence of two subgroups. The first subgroup comprised the strains MIT 05-9149T, MIT 05-9159, MIT 05-9166, and MIT 05-9175; the second subgroup comprised strains MIT 05-9150, MIT 05-9156, MIT 05-9157, and MIT 05-9164. The protein profiles of both subgroups were clearly different from each other and from those of other Campylobacter species (Fig. 2). For two strains (MIT 05-9166 and MIT 05-9175), repeated analyses failed to generate good-quality AFLP profiles; the remaining isolates again formed the same two subgroups (Fig. 3). The two subgroups had very different AFLP profiles that also allowed us to distinguish them from other Campylobacter species.
FIG. 2.
Dendrogram and whole-cell protein profiles of eight chimpanzee strains and of type or reference strains of their nearest phylogenetic neighbors. The similarity of the obtained normalized patterns was determined by the Pearson product moment correlation coefficient, and clustering was performed by UPGMA.
FIG. 3.
Dendrogram representing the AFLP fingerprints of six chimpanzee strains and of type or reference strains of their nearest phylogenetic neighbors. Similarity was determined by the Pearson product moment correlation coefficient, and clustering was performed by UPGMA.
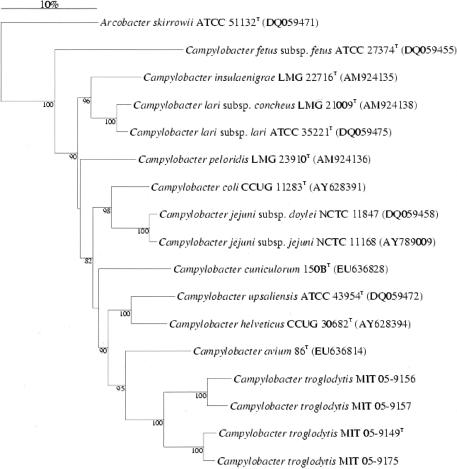
hsp60 sequence analysis.
Two strains of each subgroup (MIT 05-9149T and MIT 05-9175 representing the first subgroup and MIT 05-9156 and MIT 05-9157 representing the second) were subsequently chosen for hsp60 sequence analysis. Phylogenetic relationships based on hsp60 sequence similarity values are shown in Fig. 4. By hsp60 sequence analysis, both pairs of strains were again clearly different from each other and from other Campylobacter species. The nearest phylogenetic neighbors of subgroup 1 strains were the subgroup 2 strains (87% similarity) and Campylobacter avium (83%), C. upsaliensis (83%), C. helveticus (82%), and Campylobacter cuniculorum (82%). The nearest phylogenetic neighbors of subgroup 2 strains were the subgroup 1 strains and C. avium (81%), C. upsaliensis (80%), C. helveticus (80%), and C. coli (79%).
FIG. 4.
Neighbor-joining phylogenetic tree based on partial hsp60 gene sequences. Bootstrap values (500 replicates) higher than 60% are indicated at the nodes.
DNA-DNA hybridization experiments and determination of the mol% G+C content.
Strains MIT 05-9149T (subgroup 1) and MIT 05-9157 (subgroup 2) exhibited a hybridization level of 30%; their DNA base ratios were 34 and 38 mol%, respectively.
Electron microscopy.
By electron microscopy, the organisms from both subgroups were curved, measured on average 2.5 to 3.0 μm by 0.25 to 0.3 μm, and had a single, nonsheathed polar flagellum, although one flagellum at each end of the organism was sometimes seen (Fig. 5).
FIG. 5.
Transmission electron microscope image of the novel Campylobacter isolated from chimpanzees. Note the curved morphology and single unsheathed flagellum.
DISCUSSION
Members of the genus Campylobacter, currently comprising some 20 species, are Gram-negative asaccharolytic bacteria with microaerobic growth requirements and have a low G+C content (24, 53). They are considered either to be biochemically inert or to have indistinct biochemical characteristics (46). They colonize mucosal surfaces (the gastrointestinal tract, oral cavity, or urogenital tract) of healthy and diseased humans, livestock, domestic and wild animals, and birds, particularly poultry. Most of these species have been associated with disease in humans, with occurrence worldwide (9, 25, 49). Food-borne and waterborne transmission from fecal contamination are the most frequently reported modes of human acquired infection (3).
Campylobacter spp. have been reported to be pathogenic in various captive, domestic, and wild primate species (2, 15-17, 52). Studies to date suggest that C. jejuni occurs frequently in nonhuman primates, particularly in juveniles, and is associated with diarrhea (43, 44, 58). Morton et al. suggest that C. jejuni is not a natural pathogen of wild macaques in Indonesia but infects them postcapture (31). Campylobacters have been reported in feces of both tourist-habituated and non-tourist-habituated mountain gorillas (Gorilla beringei beringei) in Uganda (18, 33).
In this study, we isolated and identified a Gram-negative, nonsporulating bacterium with microaerobic growth requirements from chimpanzees living in the wild but with frequent contact with humans. Among the strains examined, two subgroups could be distinguished. Strains belonging to these subgroups had clearly different whole-cell protein and AFLP profiles, hsp60 sequences, and DNA base compositions; however, by 16S rRNA analysis, morphology, and biochemical criteria, they were indistinguishable. A DNA-DNA hybridization value of 30% in a representative strain of each subgroup demonstrated that they represent distinct genomic species. The divergence in 16S rRNA gene sequences toward C. upsaliensis and C. helveticus and the unique whole-cell protein and AFLP profiles convincingly demonstrate that these bacteria do not belong to one of the established Campylobacter species. Therefore, we believe that it is appropriate to classify both genomic species into a single nomenspecies, for which we propose the name Campylobacter troglodytis below.
Our finding of C. troglodytis is the first report of this possible bacterial pathogen in the feces of wild chimpanzees. We found C. troglodytis in the feces of all age groups (infant, juvenile, adolescent, and adult) of M-group chimpanzees, in loose and firm stools, and in stools that tested positive and negative for fecal occult blood (Table 1). Other chimpanzees in the M group have been observed to have loose stools with positive and negative fecal occult blood tests. Factors including diet and intestinal pathogens may account for loose stools, and colitis from infectious or noninfectious diseases may account for the presence of blood in the feces. For example, in the M group residing at Mahale Mountains, various parasites, including Bertiella, Oesophagostomum, Prosthenorchis, Strongyloides, and Trichuris species, have been reported (13, 20, 22). In addition, rotavirus has been detected in the feces of M-group chimpanzees (21). The potential pathogenicity of C. troglodytis in wild chimpanzees should be investigated, and additional studies should be conducted to determine if other potential bacterial, viral, and helminth and protozoan pathogens may be present in this population.
One of the nearest neighbors of C. troglodytis phylogenetically is C. upsaliensis, a catalase-negative or weakly positive campylobacter that was first described when it was isolated from dogs in 1983 and was then reported in cats in 1989 (9, 46). C. troglodytis differs from C. upsaliensis in that C. troglodytis is negative for nitrate reductase and indoxyl acetate hydrolysis. C. upsaliensis has been reported to be a potential human pathogen, with reports of gastroenteritis and bacteremia in healthy hosts and opportunistic infections in immunocompromised individuals (11, 39, 56). Diarrheic disease in children in socially disadvantaged groups and day care centers has also been reported (1, 11, 29). C. helveticus, also isolated from domestic cats and dogs, has not been reported to cause disease in humans (50, 56). Recently, C. avium has been identified in birds, Campylobacter peloridis and C. cuniculorum in humans and molluscs, and Campylobacter insulaenigrae in mammals (5, 8, 42, 59). C. troglodytis may or may not be of human origin, given that the feces of humans residing in this locale have not been specifically cultured for the organism. Another distinct possibility is that the bacterium colonizes the intestinal tracts of other wild animals, including rodents and other species of nonhuman primates. More studies are required to determine its host distribution and pathogenicity.
Taxonomy.
C. troglodytis sp. nov. (tro·glo·dy·tis) N.L. gen. n. troglodytis of a chimpanzee (Pan troglodytes), from which the bacterium was isolated. Cells are slender and slightly curved (0.2 by 2 to 3 μm). The bacterium is Gram negative and nonsporulating, being motile with a single nonsheathed flagellum at one end. Organisms grow on solid agar and appear as small pinpoint colonies. The organism grows at 37°C and 42°C, but not at 25°C. It is catalase and oxidase positive but hippurate, urease, and indole acetate hydrolysis negative. It is gamma-glutamyl transpeptidase negative and alkaline phosphatase hydrolysis negative. It does not reduce nitrate to nitrite and does not grow in 1% glycine. It is susceptible to nalidixic acid and has intermediate susceptibility to cephalothin. The type strain is MIT 05-9149 (CCUG 60849). Strain MIT 05-9157 is a representative of the second C. troglodytis genomovar. Its hsp60 sequence accession number in GenBank is FN421421. The DNA base ratios of strains MIT 05-9149T and MIT 05-9157 are 34 and 38 mol%, respectively.
Acknowledgments
This work was supported by grants NSF 0238069 (T.J.S.) and NIH R01CA067529 (J.G.F.).
Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the NSF.
We are sincerely grateful to the Tanzania National Parks, Tanzania Wildlife Research Institute, and Tanzania Commission for Science and Technology. We thank Park management and staff at Mahale Mountains and Rubondo Island National Parks for their assistance and our chimpanzee trackers for their expertise, help, and wonderful companionship in the field. Finally, we thank Hans G. Trueper of the University of Bonn for his help and insight in naming the organism.
Footnotes
Published ahead of print on 28 January 2011.
REFERENCES
- 1.Albert, M. J., W. Tee, A. Leach, V. Asche, and J. L. Penner. 1992. Comparison of a blood-free medium and a filtration technique for the isolation of Campylobacter spp. from diarrhoeal stools of hospitalised patients in central Australia. J. Med. Microbiol. 37:176-179. [DOI] [PubMed] [Google Scholar]
- 2.Andrade, M. C., et al. 2007. Circulation of Campylobacter spp. in rhesus monkeys (Macaca mulatta) held in captivity: a longitudinal study. Mem. Inst. Oswaldo Cruz 102:53-57. [DOI] [PubMed] [Google Scholar]
- 3.Brown, P. E., et al. 2004. Frequency and spatial distribution of environmental Campylobacter spp. Appl. Environ. Microbiol. 70:6501-6511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cook, G. T. 1950. A plate test for nitrate reduction. J. Clin. Pathol. 3:359-362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Debruyne, L., S. L. On, E. De Brandt, and P. Vandamme. 2009. Novel Campylobacter lari-like bacteria from humans and molluscs: description of Campylobacter peloridis sp. nov., Campylobacter lari subsp. concheus subsp. nov. and Campylobacter lari subsp. lari subsp. nov. Int. J. Syst. Evol. Microbiol. 59:1126-1132. [DOI] [PubMed] [Google Scholar]
- 6.Dewhirst, F. E., et al. 1999. Phylogeny of the defined murine microbiota: altered Schaedler flora. Appl. Environ. Microbiol. 65:3287-3292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ezaki, T., Y. Hashimoto, and E. Yabuuchi. 1989. Fluorometric deoxyribonucleic acid hybridization in microdilution wells as an alternative to membrane-filter hybridization in which radioisotopes are used to determine genetic relatedness among bacterial strains. Int. J. Syst. Bacteriol. 39:224-229. [Google Scholar]
- 8.Foster, G., et al. 2004. Campylobacter insulaenigrae sp. nov., isolated from marine mammals. Int. J. Syst. Evol. Microbiol. 54:2369-2373. [DOI] [PubMed] [Google Scholar]
- 9.Fox, J. G., et al. 1989. “Campylobacter upsaliensis” isolated from cats as identified by DNA relatedness and biochemical features. J. Clin. Microbiol. 27:2376-2378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goldberg, T. L., et al. 2007. Patterns of gastrointestinal bacterial exchange between chimpanzees and humans involved in research and tourism in western Uganda. Biol. Conserv. 135:511-517. [Google Scholar]
- 11.Goossens, H., et al. 1995. Investigation of an outbreak of Campylobacter upsaliensis in day care centers in Brussels: analysis of relationships among isolates by phenotypic and genotypic typing methods. J. Infect. Dis. 172:1298-1305. [DOI] [PubMed] [Google Scholar]
- 12.Hanamura, S., et al. 2008. Chimpanzee deaths at Mahale caused by a flu-like disease. Primates 49:77-80. [DOI] [PubMed] [Google Scholar]
- 13.Huffman, M. A., S. Gotoh, L. A. Turner, M. Hamai, and K. Yoshida. 1997. Seasonal trends in intestinal nematode infection and medicinal plant use among chimpanzees in the Mahale Mountains, Tanzania. Primates 38:111-125. [Google Scholar]
- 14.Hwang, M. N., and G. M. Ederer. 1975. Rapid hippurate hydrolysis method for presumptive identification of group B streptococci. J. Clin. Microbiol. 1:114-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson, L. D., L. M. Ausman, R. M. Rolland, L. V. Chalifoux, and R. G. Russell. 2001. Campylobacter-induced enteritis and diarrhea in captive cotton-top tamarins (Saguinus oedipus) during the first year of life. Comp. Med. 51:257-261. [PubMed] [Google Scholar]
- 16.Kalashnikova, V. A., E. K. Dzhikidze, Z. K. Stasilevich, and M. G. Chikobava. 2002. Detection of Campylobacter jejuni in healthy monkeys and monkeys with enteric infections by PCR. Bull. Exp. Biol. Med. 134:299-300. [DOI] [PubMed] [Google Scholar]
- 17.Kalashnikova, V. A., E. K. Dzhikidze, Z. K. Stasilevich, R. I. Krylova, and T. I. Kebu. 2006. Campylobacter in the etiology of acute intestinal infections in primates. Vestn. Ross. Akad. Med. Nauk. 1:6-10. [PubMed] [Google Scholar]
- 18.Kalema-Zikusoka, G., J. M. Rothman, and M. T. Fox. 2005. Intestinal parasites and bacteria of mountain gorillas (Gorilla beringei beringei) in Bwindi Impenetrable National Park, Uganda. Primates 46:59-63. [DOI] [PubMed] [Google Scholar]
- 19.Kärenlampi, R. I., T. P. Tolvanen, and M. L. Hänninen. 2004. Phylogenetic analysis and PCR-restriction fragment length polymorphism identification of Campylobacter species based on partial groEL gene sequences. J. Clin. Microbiol. 42:5731-5738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kaur, T., and M. A. Huffman. 2004. Descriptive urological record of chimpanzees (Pan troglodytes) in the wild and limitations associated with using multi-reagent dipstick test strips. J. Med. Primatol. 33:187-196. [DOI] [PubMed] [Google Scholar]
- 21.Kaur, T., et al. 2008. Descriptive epidemiology of fatal respiratory outbreaks and detection of a human-related metapneumovirus in wild chimpanzees (Pan troglodytes) at Mahale Mountains National Park, western Tanzania. Am. J. Primatol. 70:755-765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kawabata, M., and T. Nishida. 1991. A preliminary note on the intestinal parasites of wild chimpanzees in the Mahale Mountains, Tanzania. Primates 32:275-278. [Google Scholar]
- 23.Köndgen, S., et al. 2008. Pandemic human viruses cause decline of endangered great apes. Curr. Biol. 18:260-264. [DOI] [PubMed] [Google Scholar]
- 24.Korczak, B. M., et al. 2006. Genetic relatedness within the genus Campylobacter inferred from rpoB sequences. Int. J. Syst. Evol. Microbiol. 56:937-945. [DOI] [PubMed] [Google Scholar]
- 25.Kuwabara, S. 2004. Guillain-Barré syndrome: epidemiology, pathophysiology and management. Drugs 64:597-610. [DOI] [PubMed] [Google Scholar]
- 26.Lawson, A. J., S. L. On, J. M. Logan, and J. Stanley. 2001. Campylobacter hominis sp. nov., from the human gastrointestinal tract. Int. J. Syst. Evol. Microbiol. 51:651-660. [DOI] [PubMed] [Google Scholar]
- 27.Leendertz, F. H., et al. 2006. Pathogens as drivers of population declines: the importance of systematic monitoring in great apes and other threatened mammals. Biol. Conserv. 131:325-337. [Google Scholar]
- 28.Logan, J. M., A. Burnens, D. Linton, A. J. Lawson, and J. Stanley. 2000. Campylobacter lanienae sp. nov., a new species isolated from workers in an abattoir. Int. J. Syst. Evol. Microbiol. 50:865-872. [DOI] [PubMed] [Google Scholar]
- 29.Megraud, F., and F. Bonnet. 1986. Unusual campylobacters in human faeces. J. Infect. 12:275-276. [DOI] [PubMed] [Google Scholar]
- 30.Mesbah, M., and W. B. Whitman. 1989. Measurement of deoxyguanosine/thymidine ratios in complex mixtures by high-performance liquid chromatography for determination of the mole percentage guanine + cytosine of DNA. J. Chromatogr. 479:297-306. [DOI] [PubMed] [Google Scholar]
- 31.Morton, W. R., et al. 1983. Identification of Campylobacter jejuni in Macaca fascicularis imported from Indonesia. Lab. Anim. Sci. 33:187-188. [PubMed] [Google Scholar]
- 32.Nishida, T., et al. 2003. Demography, female life history, and reproductive profiles among the chimpanzees of Mahale. Am. J. Primatol. 59:99-121. [DOI] [PubMed] [Google Scholar]
- 33.Nizeyi, J. B., et al. 2001. Campylobacteriosis, salmonellosis, and shigellosis in free-ranging human-habituated mountain gorillas of Uganda. J. Wildl. Dis. 37:239-244. [DOI] [PubMed] [Google Scholar]
- 34.On, S. L., H. I. Atabay, J. E. Corry, C. S. Harrington, and P. Vandamme. 1998. Emended description of Campylobacter sputorum and revision of its infrasubspecific (biovar) divisions, including C. sputorum biovar paraureolyticus, a urease-producing variant from cattle and humans. Int. J. Syst. Bacteriol. 48:195-206. [DOI] [PubMed] [Google Scholar]
- 35.On, S. L., and B. Holmes. 1992. Assessment of enzyme detection tests useful in identification of campylobacteria. J. Clin. Microbiol. 30:746-749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.On, S. L., and B. Holmes. 1991. Effect of inoculum size on the phenotypic characterization of Campylobacter species. J. Clin. Microbiol. 29:923-926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.On, S. L., B. Holmes, and M. J. Sackin. 1996. A probability matrix for the identification of campylobacters, helicobacters and allied taxa. J. Appl. Bacteriol. 81:425-432. [DOI] [PubMed] [Google Scholar]
- 38.Paster, B. J., and F. E. Dewhirst. 1988. Phylogeny of Campylobacter, Wolinellas, Bacteroides gracilis, and Bacteroides ureolyticus by 16S ribosomal ribonucleic acid sequencing. Int. J. Syst. Bacteriol. 38:56-62. [Google Scholar]
- 39.Patton, C. M., et al. 1989. Human disease associated with “Campylobacter upsaliensis” (catalase-negative or weakly positive Campylobacter species) in the United States. J. Clin. Microbiol. 27:66-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pitcher, D. G., N. A. Saunders, and R. J. Owen. 1989. Rapid extraction of bacterial genomic DNA with guanidium thiocyanate. Lett. Appl. Microbiol. 8:151-156. [Google Scholar]
- 41.Pot, B., P. Vandamme, and K. Kersters. 1994. Analysis of electrophoretic whole-organism protein fingerprinting. Wiley, Chichester, United Kingdom.
- 42.Rossi, M., et al. 2009. Campylobacter avium sp. nov., a new hippurate-positive species isolated from poultry. Int. J. Syst. Evol. Microbiol. 59:2364-2369. [DOI] [PubMed] [Google Scholar]
- 43.Russell, R. G., M. J. Blaser, J. I. Sarmiento, and J. G. Fox. 1989. Experimental Campylobacter jejuni infection in Macaca nemestrina. Infect. Immun. 57:1438-1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Russell, R. G., J. I. Sarmiento, J. G. Fox, and P. Panigrahi. 1990. Evidence of reinfection with multiple strains of Campylobacter jejuni and Campylobacter coli in Macaca nemestrina housed under hyperendemic conditions. Infect. Immun. 58:2149-2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Saitou, N., and M. Nei. 1987. The neighbor-joining method: a new method for reconstructing phylogenetic trees. Mol. Biol. Evol. 4:406-425. [DOI] [PubMed] [Google Scholar]
- 46.Sebald, M., and M. Vèron. 1963. Teneur en bases de I'ADN et classification des Vibrions. Ann. Inst. Pasteur 105:897-910. [PubMed] [Google Scholar]
- 47.Shen, Z., Y. Feng, F. E. Dewhirst, and J. G. Fox. 2001. Coinfection of enteric Helicobacter spp. and Campylobacter spp. in cats. J. Clin. Microbiol. 39:2166-2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shen, Z., et al. 2005. A novel enterohepatic Helicobacter species ′Helicobacter mastomyrinus' isolated from the liver and intestine of rodents. Helicobacter 10:59-70. [DOI] [PubMed] [Google Scholar]
- 49.Skirrow, M. B. 1994. Diseases due to Campylobacter, Helicobacter and related bacteria. J. Comp. Pathol. 111:113-149. [DOI] [PubMed] [Google Scholar]
- 50.Stanley, J., et al. 1992. Campylobacter helveticus sp. nov., a new thermophilic species from domestic animals: characterization, and cloning of a species-specific DNA probe. J. Gen. Microbiol. 138:2293-2303. [DOI] [PubMed] [Google Scholar]
- 51.Thompson, J. D., T. J. Gibson, F. Plewniak, F. Jeanmougin, and D. G. Higgins. 1997. The CLUSTAL_X windows interface: flexible strategies for multiple sequence alignment aided by quality analysis tools. Nucleic Acids Res. 25:4876-4882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tresierra-Ayala, A., and H. Fernández. 1997. Occurrence of thermotolerant Campylobacter species in domestic and wild monkeys from Peru. Zentralbl. Veterinarmed. B 44:61-64. [DOI] [PubMed] [Google Scholar]
- 53.Vandamme, P., and J. De Ley. 1991. Proposal for a new family, Campylobacteraceae. Int. J. Syst. Bacteriol. 41:451-455. [Google Scholar]
- 54.Vogel, G. 2007. Conservation. Scientists say Ebola has pushed western gorillas to the brink. Science 317:1484. [DOI] [PubMed] [Google Scholar]
- 55.Walsh, P. D., et al. 2003. Catastrophic ape decline in western equatorial Africa. Nature 422:611-614. [DOI] [PubMed] [Google Scholar]
- 56.Wieland, B., et al. 2005. Campylobacter spp. in dogs and cats in Switzerland: risk factor analysis and molecular characterization with AFLP. J. Vet. Med. B Infect. Dis. Vet. Public Health 52:183-189. [DOI] [PubMed] [Google Scholar]
- 57.Wolfe, N. D., et al. 1998. Wild primate populations in emerging infectious disease research: the missing link? Emerg. Infect. Dis. 4:149-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Young, V. B., D. B. Schauer, and J. G. Fox. 2000. Animal models of Campylobacter infection, p. 287-301. In I. Nachamkin and M. J. Blaser (ed.), Campylobacter, 2nd ed. ASM Press, Washington, DC.
- 59.Zanoni, R. G., L. Debruyne, M. Rossi, and J. V. P. Revez. 2009. Campylobacter cuniculorum sp. nov., from rabbits. Int. J. Syst. Evol. Microbiol. 59:1666-1671. [DOI] [PubMed] [Google Scholar]