Abstract
Enterococcus hirae, a Gram-positive bacterium, is a rare isolate in clinical specimens. We report an unusual case of a relapse of prosthetic valve endocarditis due to E. hirae 6 months after the initial episode. Clonal relationship was proven by genomic analysis.
CASE REPORT
In April 2008, a 78 year-old woman presented with a 5-month history of fever, generalized weakness, and a 7-kg weight loss. She had a history of diabetes mellitus and hypertension and had undergone in 2001 an aortic valve replacement with a bioprosthetic valve. On admission, her temperature was 38°C, and cardiac examination revealed a 3/6 systolic murmur. Transthoracic and transesophageal echocardiographies showed no evidence of endocarditis.
Five blood cultures yielded colonies of Gram-positive cocci with a morphology typical of Streptococcus. On blood agar culture, colonies were circular and smooth and reached 0.2 to 0.5 mm after 24 to 48 h of incubation in the presence of 5% CO2. The strain was identified by phenotypic determination and genetic analysis. The phenotypic identification was based upon colony and Gram stain morphologies and a negative catalase reaction. The cocci reacted with both Lancefield group F and D antisera (Streptex; Diamondial, Sees, France). The biochemical identification remained difficult even by a semiautomated system. Accurate identification to the species level was not possible with the IDGP N052 card (bioMérieux, Marcy l'Etoile, France) due to low discrimination (50.52% for Enterococcus durans and 49.48% for Enterococcus faecium). The Rapid ID 32 Strep identification system (bioMérieux) failed, producing an unacceptable profile for Enterococcus gallinarum with the current database.
The strain was correctly identified to the species level as Enterococcus hirae by genetic methods using 16S rRNA and sodAint gene sequencing (where “int” represents “internal”) as previously described (5, 12). Sequence analysis of this strain yielded 99.81% and 99.76% identities with the sequences of the 16S rRNA gene (GenBank accession no. AB362598) of type strain of E. hirae and the sodA gene (GenBank accession no. AJ387916) of E. hirae, respectively. As the growth was deficient, antibiotic susceptibility testing was performed with an agar diffusion technique using a Mueller-Hinton agar supplemented with 5% horse blood (bioMérieux). The strain was susceptible to amoxicillin (MIC, 0.032 μg/ml, as measured by the Etest technique), moxifloxacin, vancomycin, teicoplanin, erythromycin, and rifampin but resistant to clindamycin, tetracycline, and fosfomycin and exhibited low-level resistance to streptomycin, kanamycin, and gentamicin.
Despite our patient's normal echocardiography, a diagnosis of possible infective endocarditis was established (Table 1), and intravenous amoxicillin (200 mg per kg of body weight per day) and gentamicin (3 mg per kg per day) were initiated. After 2 weeks, gentamicin was discontinued and rifampin (20 mg per kg per day) was initiated. Antimicrobial treatment was administered for 6 weeks. The patient improved clinically and became afebrile 48 h after antibiotic initiation, and blood cultures became negative. Colonoscopy investigation revealed multiple colonic polyps, which were endoscopically removed. Histological examination showed no evidence of cancer.
Table 1.
List of modified Duke criteria for each episode of endocarditis in our patienta
| Category | Duke criterion from: |
|
|---|---|---|
| First episode | Second episode | |
| Major criteria | 5 separate blood cultures yielded Enterococcus hirae | Echocardiography was positive for infective endocarditis, with demonstration of aortic vegetation |
| 2 separate blood cultures yielded E. hirae | ||
| Minor criteria | Bioprosthetic aortic valve | Bioprosthetic aortic valve |
| Fever | Fever | |
Note that the sensitivity of the modified Duke criteria is diminished when infection affects a prosthetic valve.
Four months after discontinuation of antimicrobial therapy, the patient was readmitted for fever. Echocardiography showed a vegetation involving the aortic prosthetic valve, and antimicrobial therapy with amoxicillin and gentamicin was initiated. Two days later, the two blood cultures obtained before initiation of antimicrobial therapy yielded a Gram-positive coccus with the same cultural characteristics and the same antibiotic susceptibility pattern as described above, which was identified as Enterococcus hirae. A diagnosis of definite endocarditis was made according to the modified Duke criteria (7) (Table 1), and the patient received the same antimicrobial therapy as for the initial episode, i.e., intravenous amoxicillin for 6 weeks, intravenous gentamicin for 2 weeks, and oral rifampin for 4 weeks. Her poor general condition contraindicated surgery.
The evolution was quickly favorable; the patient became afebrile, and blood cultures remained negative. Echocardiography performed 1 month later did not reveal any vegetation or dysfunction of the aortic bioprosthesis. Control by colonoscopy showed a 20-mm colonic polyp, which was removed; histological examination revealed an adenoma without evidence of neoplasia.
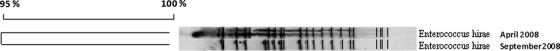
Both E. hirae isolates were then genetically compared in order to distinguish relapse from reinfection of the endocarditis. Analysis of the genomic patterns of both isolates after pulsed-field gel electrophoresis after restriction with SmaI showed that they were clonally related (Fig. 1), according to the criteria of Tenover et al. (16).
Fig. 1.
Pulsed-field gel electrophoresis banding patterns after SmaI digestion of both clinical isolates of E. hirae. Percentages of similarity are shown above the dendrogram. Isolate dates are on the right.
The patient remained clinically well 1 year after completion of therapy.
Enterococci are frequently identified as important causes of infections in humans, such as bacteremia, endocarditis, and urinary tract infections. Most enterococcal strains isolated from clinical samples belong to two species, Enterococcus faecalis and Enterococcus faecium. Enterococcus hirae causes infections mainly in various animal species (2, 3), and only three cases of human infection have been reported to date (1, 4, 11). In these three reports, E. hirae was responsible for septicemia, spondylodiscitis, and native valve endocarditis.
We describe a case of E. hirae prosthetic valve endocarditis, which relapsed despite adequate antibiotic therapy according to the European guidelines (14). The patient initially presented with E. hirae bacteremia, and a diagnosis of possible endocarditis was established, as she met one major and two minor criteria of the modified Duke criteria for the diagnosis of endocarditis (7). When bacteremia relapsed, a diagnosis of definite endocarditis was made, as the patient met two major criteria. To the best of our knowledge, our case constitutes the first description of prosthetic valve endocarditis due to E. hirae and the fourth report of human infection caused by this bacterium. The source of infection in our patient was probably the digestive tract, as colonoscopy showed multiple colonic polyps. Currently, there is no demonstrated relationship between E. hirae infection and colonic pathology, but very few cases of infections due to this particular bacterium have been reported; however, enterococci are commensal species of the human intestinal tract, and E. hirae has been involved in colonic pathology in animals (6, 9). Therefore, we decided to perform a colonoscopy in order to seek intestinal disease, as is recommended for other bacteria colonizing the gastrointestinal tract.
The only other reported case of E. hirae endocarditis, by Poyart et al. in 2002, was a 72-year-old man with native valve endocarditis who was treated with ampicillin, gentamicin, and rifampin (11). Despite the in vitro susceptibility of the strain, this regimen was not able to sterilize the vegetation, and endocarditis recurred 3 months after discontinuation of antimicrobial treatment. The same phenomenon occurred in our patient, although adequate antimicrobial therapy was administered for 6 weeks, suggesting that E. hirae is a difficult-to-treat bacterium that causes relapsing infections (8). Moreover, we hypothesize that the particularly low virulence of this strain living likely in a dormant state may explain the delayed relapse. The treatment of infections due to this particular bacterium may necessitate prolonged antimicrobial therapy and a closer surveillance of clinical parameters (echocardiography and blood cultures after discontinuation of antibiotics) in order to detect a relapse. For our patient, we chose to add rifampin to the amoxicillin-gentamicin combination which is recommended for treatment of enterococcal prosthetic valve endocarditis (14). Rifampin has shown good activity against Staphylococcus aureus biofilm (13) and is recommended for treatment of staphylococcal prosthetic valve endocarditis (14). However, it has not been extensively studied for Enterococcus species infections, although some promising results have been reported (10, 18). As optimal therapy for the treatment of E. hirae infection remains unknown and valve replacement was contraindicated for our patient, we hypothesized that the addition of rifampin might optimize antibiotic therapy and reduce the risk of relapse.
Finally, identification of enterococci other than Enterococcus faecalis and Enterococcus faecium, in the absence of additional tests (11), remains difficult, with potentially serious implications for clinical management. As reported previously, the Vitek2 automated system may experience difficulties in properly identifying E. hirae and Lactococcus garvieae, another Gram-positive coccus involved in endocarditis. Accurate identification of enterococci can be achieved with molecular techniques (17).
Thus, misidentification of unusual Enterococcus species by the different semiautomated commercial identification methods might occur, and accurate molecular identification is required, as this species remains rare (8, 15).
Acknowledgments
We are grateful to E. Carbonnelle for helpful discussion.
Footnotes
Published ahead of print on 19 January 2011.
REFERENCES
- 1. Canalejo E., Ballesteros R., Cabezudo J., Garcia-Arata M. I., Moreno J. 2008. Bacteraemic spondylodiscitis caused by Enterococcus hirae. Eur. J. Clin. Microbiol. Infect. Dis. 27:613–615 [DOI] [PubMed] [Google Scholar]
- 2. Devriese L. A., et al. 1992. Enterococcus hirae in septicaemia of psittacine birds. Vet. Rec. 130:558–559 [DOI] [PubMed] [Google Scholar]
- 3. Devriese L. A., Haesebrouck F. 1991. Enterococcus hirae in different animal species. Vet. Rec. 129:391–392 [DOI] [PubMed] [Google Scholar]
- 4. Gilad J., et al. 1998. Enterococcus hirae septicemia in a patient with end-stage renal disease undergoing hemodialysis. Eur. J. Clin. Microbiol. Infect. Dis. 17:576–577 [DOI] [PubMed] [Google Scholar]
- 5. Janda J. M., Abbott S. L. 2007. 16S rRNA gene sequencing for bacterial identification in the diagnostic laboratory: pluses, perils, and pitfalls. J. Clin. Microbiol. 45:2761–2764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lapointe J. M., Higgins R., Barrette N., Milette S. 2000. Enterococcus hirae enteropathy with ascending cholangitis and pancreatitis in a kitten. Vet. Pathol. 37:282–284 [DOI] [PubMed] [Google Scholar]
- 7. Li J. S., et al. 2000. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin. Infect. Dis. 30:633–638 [DOI] [PubMed] [Google Scholar]
- 8. Murray B. E. 1990. The life and times of the Enterococcus. Clin. Microbiol. Rev. 3:46–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nicklas J. L., Moisan P., Stone M. R., Gookin J. L. 2010. In situ molecular diagnosis and histopathological characterization of enteroadherent Enterococcus hirae infection in pre-weaning-age kittens. J. Clin. Microbiol. 48:2814–2820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pankey G., Ashcraft D., Patel N. 2005. In vitro synergy of daptomycin plus rifampin against Enterococcus faecium resistant to both linezolid and vancomycin. Antimicrob. Agents Chemother. 49:5166–5168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Poyart C., et al. 2002. Native valve endocarditis due to Enterococcus hirae. J. Clin. Microbiol. 40:2689–2690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Poyart C., Quesnes G., Trieu-Cuot P. 2000. Sequencing the gene encoding manganese-dependent superoxide dismutase for rapid species identification of enterococci. J. Clin. Microbiol. 38:415–418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Saginur R., et al. 2006. Multiple combination bactericidal testing of staphylococcal biofilms from implant-associated infections. Antimicrob. Agents Chemother. 50:55–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Task Force on the Prevention, Diagnosis, and Treatment of Infective Endocarditis of the European Society of Cardiology 2009. Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009). The Task Force on the Prevention, Diagnosis, and Treatment of Infective Endocarditis of the European Society of Cardiology (ESC). Eur. Heart J. 30:2369–2413 [DOI] [PubMed] [Google Scholar]
- 15. Tendolkar P. M., Baghdayan A. S., Shankar N. 2003. Pathogenic enterococci: new developments in the 21st century. Cell. Mol. Life Sci. 60:2622–2636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tenover F. C., et al. 1995. Interpretative chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J. Clin. Microbiol. 33:2233–2239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Vinh D. C., Nichol K. A., Rand F., Embil J. M. 2006. Native-valve bacterial endocarditis caused by Lactococcus garvieae. Diagn. Microbiol. Infect. Dis. 56:91–94 [DOI] [PubMed] [Google Scholar]
- 18. Whitman M. S., et al. 1993. Antibiotic treatment of experimental endocarditis due to vancomycin- and ampicillin-resistant Enterococcus faecium. Antimicrob. Agents Chemother. 37:2069–2073 [DOI] [PMC free article] [PubMed] [Google Scholar]