Abstract
Replication-defective vaccine vectors based on vesicular stomatitis virus (VSV) lacking its envelope glycoprotein gene (G) are highly effective in animal models. However, such ΔG vectors are difficult to grow because they require complementation with the VSV G protein. In addition, the complementing G protein induces neutralizing antibodies in animals and thus limits multiple vector applications. In the process of generating an experimental Nipah virus (a paramyxovirus) vaccine, we generated two defective VSVΔG vectors, each expressing one of the two Nipah virus (NiV) glycoproteins (G and F) that are both required for virus entry to host cells. These replication-defective VSV vectors were effective at generating NiV neutralizing antibody in mice. Most interestingly, we found that these two defective viruses could be grown together and passaged in tissue culture cells in the absence of VSV G complementation. This mixture of complementing defective viruses was also highly effective at generating NiV neutralizing antibody in animals. This novel approach to growing and producing a vaccine from two defective viruses could be generally applicable to vaccine production for other paramyxoviruses or for other viruses where the expression of at least two different proteins is required for viral entry. Such an approach minimizes biosafety concerns that could apply to single, replication-competent VSV recombinants expressing all proteins required for infection.
Live-attenuated, recombinant viruses expressing proteins of other viruses can be highly effective vaccine vectors. However, obtaining regulatory approval to use live recombinant viruses as human vaccines is tedious because of concerns about potential pathogenicity. Live-attenuated, vesicular stomatitis virus (VSV) has been used extensively as an experimental vaccine vector for the past 11 years (5, 15, 18, 27, 29, 32). These vectors are grown easily to high titers and stimulate potent cellular and humoral immunity, but obtaining final U.S. Food and Drug Administration approval for use in clinical trials has been slow.
Concerns about potential VSV pathogenicity can be minimized through the use of defective viruses lacking the VSV G gene (ΔG) that are grown in complementing cell lines expressing the VSV G protein. Although these defective vectors have been just as effective as live-attenuated recombinants in preclinical trials (26), production using complementing cell lines is a major limitation (36). We describe here a new approach for growing such defective recombinants using a complementing pair of VSVΔG recombinants, each expressing one of the two glycoproteins that are both required for the entry of Nipah virus (NiV), an emerging zoonotic virus in the paramyxovirus family.
NiV has caused fatal encephalitis in humans in massive outbreaks in Malaysia, Singapore, Bangladesh, and India in recent years (3, 8). These outbreaks, apparently initiating from a bat reservoir (4), involved extensive geographical spread in a wide array of animal species including pigs, cats, dogs, horses, and humans (7, 13). Likely human-to-human transmissions of NiV were documented in recent outbreaks in Bangladesh (2004 and later), and case-fatality rates were ca. 75% (12, 14). There are currently no vaccines or effective treatments available for NiV.
NiV contains a single negative-sense RNA genome encoding six structural proteins: nucleocapsid (N), phosphoprotein (P), matrix (M), fusion (F), attachment (G), and polymerase protein (L). As in other paramyxoviruses (20), two surface glycoproteins (G and F in this case) are required for NiV entry into host cells. The viral glycoproteins are the targets of neutralizing antibody (nAb) (33). Recombinant vaccinia viruses expressing NiV G or F proteins induce protective immune responses, either in combination or separately (11). In golden hamsters, nAb was sufficient to induce protection from NiV challenge (11). Recombinant canarypox viruses encoding NiV G or F were also shown to be protective against lethal NiV infection in pigs (35). Similarly, a recombinant soluble form of NiV glycoprotein (sGNiV) elicited a protective response in a cat model (23).
VSV is a negative-strand RNA virus in the Rhabdoviridae family. It encodes five structural proteins: nucleocapsid (N), phosphoprotein (P), matrix (M), glycoprotein (G), and RNA-dependent RNA polymerase (L). VSV-based vectors expressing appropriate foreign antigens have been shown to be highly effective vaccines against numerous viral and bacterial pathogens (2, 10, 15, 16, 18, 27-29, 32). We constructed live attenuated or single-cycle recombinant VSVs (lacking VSV G) expressing either NiV G or F. All vectors induced neutralizing antibodies to NiV pseudotypes. Importantly, we found that the defective viruses expressing either NiV G or NiV F proteins could be propagated as a complementing pair in tissue culture cells in the absence of VSV G. Furthermore, inoculation of mice with the mixture of these complementing viruses led to the development of high levels of NiV neutralizing antibodies. These results suggest a general approach for the propagation of replication defective VSVΔG vectors in cases where the critical glycoprotein functions required for infection exist on at least two separate molecules.
MATERIALS AND METHODS
Plasmid constructions.
NiV G and F genes, codon optimized for mammalian expression by using the JCAT program (http://www.jcat.de/), were synthesized and provided by Blue Heron Biotechnology, Inc., Bothell, WA. Based on our previous experience with codon optimization in VSV vectors, such optimization typically results in a small increase in protein expression. The synthetic genes, with built-in flanking 3′ and 5′ restriction enzyme sites (XhoI and NheI), were released from the pUC plasmids by XhoI-NheI digestions and cloned into XhoI-NheI-digested pVSVXN2 (30) to generate pVSV-G(NiV) and pVSV-F(NiV), respectively.
To generate pVSVΔG-G(NiV) and pVSVΔG-F(NiV), the VSV G gene was first removed from the full-length plasmids pVSV-G(NiV) and pVSV-F(NiV) by MluI-XhoI digestions. The 5′ overhangs of the digested vector backbones were then filled in with T4 DNA polymerase (New England Biolabs), and the products were purified and religated.
The pCAGGS-G(NiV) and pCAGGS-F(NiV) plasmids were made by cloning the codon optimized NiV G and F genes into the XhoI-NheI-digested pCAGGS vector (24). Construction of pCAGGS-G was previously described (25).
Recombinant virus recovery.
Recombinant VSVs were recovered from the four plasmids pVSV-G(NiV), pVSV-F(NiV), pVSVΔG-G(NiV), and pVSVΔG-F(NiV) as described previously (31). Briefly, for each recovery BHK-21 cells were grown to 70% confluence in Dulbecco modified Eagle medium (DMEM) containing 5% fetal bovine serum (FBS) and infected with vTF7-3 (9), a vaccinia virus recombinant expressing T7 RNA polymerase, at a multiplicity of infection (MOI) of 10 for 1 h in serum-free DMEM. After this, one of the pVSV plasmids was transfected together with the support plasmids (pBS-N, pBS-P, pBS-L, and pBS-G) encoding VSV proteins N, P, L, and G, respectively. For the recovery of VSV-G(NiV) and VSV-F(NiV), transfected cell supernatants were transferred onto fresh BHK-21 cells at 48 h posttransfection, and media containing the two viruses were collected after 48 h. Virus stocks were prepared from individual plaques grown in BHK-21 cells and stored at −70°C. For VSVΔG virus recoveries, the transfection supernatants were transferred onto BHK-21 cells that had been transfected (described below) with pCAGGS-G (25), and media containing VSV G-complemented VSVΔG-G(NiV) and VSVΔG-F(NiV) were collected after 48 h. The viruses were plaque purified on BHK-G cells (31), and VSV G-complemented stocks were prepared and stored at −70°C.
Metabolic labeling of cells infected with recombinant viruses and SDS-PAGE of cell lysates.
BHK-21 cells were infected with recombinant viruses at an MOI of 20. At 5 h, cells were washed with methionine-free DMEM, followed by labeling with 100 μCi of [35S]methionine in 1 ml of methionine-free DMEM for 45 min at 37°C. Cells were then washed twice with phosphate-buffered saline (PBS) and lysed with detergent lysis buffer (1% Nonidet P-40, 0.4% deoxycholate, 50 mM Tris-HCl [pH 8.0], 62.5 mM EDTA) on ice for 5 min. Lysates were collected in Eppendorf tubes, clarified at 16,000 × g for 2 min at 4°C, and subjected to SDS-PAGE on a 4 to 12% Bis-Tris NuPAGE gel (Invitrogen, California). Protein bands were visualized by scanning the dried gel using a Fujifilm BAS 1800 imaging system.
Antisera and antibodies.
Polyclonal mouse sera against NiV G and F were kindly provided by Paul Rota, Centers for Disease Control and Prevention, Atlanta, GA. These sera were obtained from mice immunized and boosted with vaccinia virus recombinants expressing NiV G or F. The anti-VSV G monoclonal antibodies (MAbs) I1 and I14 were used to detect VSV G expression (22).
Indirect immunofluorescence.
BHK-21 cells grown on glass coverslips were infected with either recombinant wild-type (rwt)-VSV, VSV-G(NiV), VSV-F(NiV), VSVΔG-G(NiV), or VSVΔG-F(NiV), and at 4 h postinfection (hpi) the cells were washed twice with PBS and fixed with 3% paraformaldehyde at room temperature for 20 min. After this, cells were washed with PBS containing 10 mM glycine (PBS-glycine) and incubated with primary antibodies (equal mixture of VSV G MAbs I1 and I14 or anti-NiV G or anti-NiV F mouse sera) at a dilution of 1:200. After primary antibody incubation, the cells were washed with PBS-glycine and incubated with goat anti-mouse Alexa Flour 594 IgG (Molecular Probes, Eugene, OR) diluted at 1:500. Thereafter, the cells were washed twice with PBS-glycine, mounted on slides using ProLong Gold antifade reagent with DAPI (4′,6′-diamidino-2-phenylindole; Molecular Probes), and imaged using a Nikon Eclipse 80i fluorescence microscope using a ×40 objective lens.
Transfection of pCAGGS plasmids.
For transfection of pCAGGS plasmids, 10 μg of DNA was diluted in 0.6 ml of Opti-MEM (Invitrogen) and 30 μl of Lipofectamine Reagent (Invitrogen) was diluted in 0.6 ml of Opti-MEM. The DNA and Lipofectamine mixtures were then combined and incubated at room temperature for 30 min. BHK-21 cells (3 × 106 cells plated overnight) were washed once with PBS and once with Opti-MEM, and 4.8 ml of Opti-MEM was added, followed by the addition of the DNA-Lipofectamine mix, followed by further incubation at 37°C for 5 h. Thereafter, the transfection mix was removed from the plate and replaced with DMEM containing 10% FBS and left overnight at 37°C.
Generation of NiV pseudotypes.
To obtain VSVΔG-eGFP1 pseudotyped with NiV G and F proteins, BHK-21 cells were first cotransfected with pCAGGS-G(NiV) and pCAGGS-F(NiV). Transfected cells showing extensive cell-to-cell fusion were infected with VSV-G complemented VSVΔG-eGFP1(19). At 1 h postinfection, the input virus was removed, cells were washed twice with PBS, and DMEM containing 5% FBS was added to the cells. Medium containing VSVΔG-eGFP1 pseudotyped with NiV G and F was collected after 24 h, and virus was titered on BHK-21 cells by counting the number of green fluorescent protein (GFP)-expressing cells.
Coinfection of BHK-21 cells with complementing ΔG viruses.
BHK-21 cells were simultaneously infected with VSVΔG-G(NiV) and VSVΔG-F(NiV) at an MOI of 5 each. As controls, BHK-21 cells were infected separately with VSVΔG-G(NiV) or VSVΔG-F(NiV) at an MOI of 10 each or mock infected in serum-free DMEM. After 1 h of virus adsorption, infection medium was replaced with DMEM containing 5% FBS, followed by incubation overnight at 37°C. Supernatants were collected at 20 to 24 hpi, clarified by centrifugation at 2,000 rpm for 5 min, and stored at −70°C.
Immunizations.
Six- to eight-week-old female BALB/c mice were obtained from Charles River Laboratories, Wilmington, MA, and then acclimatized for 1 week before immunization. Animals were housed under BSL-2 conditions in microisolator cages. Viruses were diluted in serum-free DMEM for immunizations. For intranasal (i.n.) inoculations, 106 PFU of the appropriate virus was administered in a volume of 25 μl to animals that were lightly anesthetized with 20% isoflurane (Baxter, Deerfield, IL) diluted in propylene glycol (vol/vol). For intramuscular (i.m.) immunizations, 106 PFU of the appropriate virus was administered in a volume of 50 μl into the left hind leg muscle. Animals vaccinated with a mixture of two different viruses received 0.5 × 106 PFU of each virus. The coinfection supernatant was used at approximately 5 × 103 PFU/mouse. Yale University Institutional Animal Care and Use Committee approved all immunizations.
Virus neutralization assays.
To measure NiV neutralizing antibodies in serum, VSVΔG-eGFP1/NiV G-F pseudotypes were first incubated with anti-VSV G MAb I1 (22) at a dilution of 1:1,000 for 30 min at 37°C to neutralize any trace infection due to residual VSV G that may have been incorporated into the particles pseudotyped with NiV G and F proteins. Pooled serum samples from each immunization group were serially diluted in serum-free DMEM and mixed with approximately 50 infectious pseudotype particles in a final volume of 80 μl. The mixture was incubated at 37°C for 1 h, and 60 μl of each dilution was transferred to a monolayer of BHK-21 cells grown in a 96-well plate. After incubation at 37°C for 1 h, 60 μl of DMEM containing 10% FBS was added to each well, and the cells were incubated for 20 to 24 h at 37°C. Infection was determined by visualizing the number of GFP-expressing cells using an Olympus CK-40 microscope equipped with epifluorescence. The neutralization titer was defined as the reciprocal of the highest serum dilution at which duplicate wells for each sample showed complete neutralization of 50 PFU of NiV pseudotype on BHK-21 cells.
The VSV neutralization assay was performed as described previously (29). Pooled serum samples from each immunization group were used for the assays, which were performed in duplicates. The VSV neutralization titers were defined as the highest dilution of serum that could completely neutralize infectivity of 100 PFU of VSV on BHK-21 cells.
RESULTS
Construction and characterization of VSV recombinants expressing NiV G or F proteins.
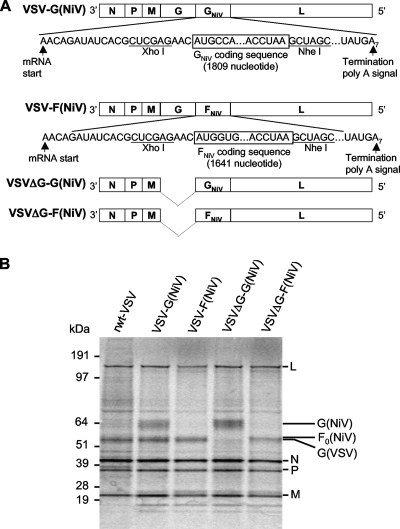
To generate VSV recombinants expressing either NiV G or F proteins, NiV genes were inserted into the plasmid vector pVSVXN2 (30) between the VSV G and L genes (Fig. 1 A). The resulting plasmids pVSV-G(NiV) and pVSV-F(NiV) were used to recover VSV-G(NiV) and VSV-F(NiV) recombinants using established procedures (21). In order to recover single-cycle VSV recombinants expressing either NiV G or F genes, the VSV G genes were deleted from the above-mentioned plasmids to generate pVSVΔG-G(NiV) and pVSVΔG-F(NiV) (Fig. 1A), and these plasmids were then used to recover VSVΔG-G(NiV) and VSVΔG-F(NiV) on BHK-21 cells expressing VSV G (31). VSV recombinants lacking the VSV G gene must be complemented with VSV G in order to produce infectious particles.
FIG. 1.
VSV recombinants encoding the NiV G and F genes and their protein expression profiles. (A) Schematic representation of VSV recombinants with insertion of NiV G or F genes between VSV G and L in the full-length VSV vector or between VSV M and L genes in the single-cycle VSVΔG vectors. The gene order is shown in 3′-5′ direction on the negative-strand RNA genome. (B) SDS-PAGE analysis of crude lysates from BHK-21 cells infected with the indicated viruses, followed by metabolic labeling with [35S]methionine for 45 min at 5 h postinfection. The protein molecular mass markers are indicated to the left side, and the virus-encoded proteins are indicated to the right side of the gel image.
To verify the expression of the NiV G and F proteins from these recombinants, we performed metabolic labeling with [35S]methionine of BHK-21 cells that had been infected with VSV recombinants. Cells were infected with VSV-G(NiV), VSV-F(NiV), VSVΔG-G(NiV), VSVΔG-F(NiV), or rwt-VSV. Lysates from infected cells were separated by SDS-PAGE and analyzed on a Fujifilm imaging system (Fig. 1B). Because VSV infection shuts off host protein synthesis, the cell lysate from rwt-VSV-infected cells primarily show the viral proteins L, G, N, P, and M (Fig. 1B, lane 1). Cells infected with VSV-G(NiV) expressed a protein of the mobility expected for NiV G (Fig. 1B, lane 2), along with other VSV proteins. Cells infected with VSVΔG-G(NiV) expressed NiV G and all other VSV proteins except G (Fig. 1B, lane 4). Expression of NiV F was detected in VSVΔG-F(NiV)-infected cells (Fig. 1B, lane 5) but was not resolved from VSV G in the lysate from cells infected with VSV-F(NiV) (Fig. 1A, lane 3). Based on mobility in SDS-PAGE, this band is consistent with the ∼60-kDa F0 precursor form of the F protein.
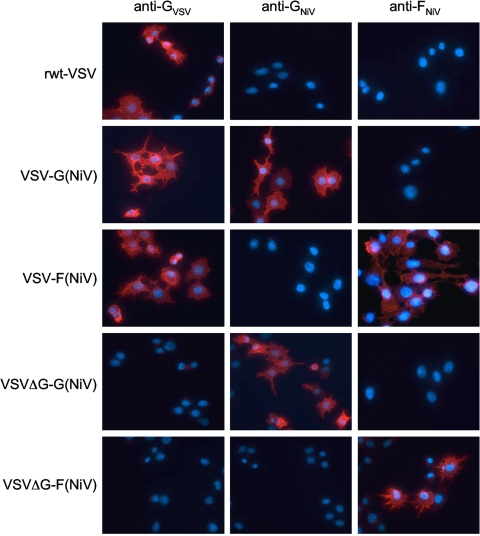
To examine localization of the NiV G and NiV F proteins expressed from the VSV recombinants, we used indirect immunofluorescence microscopy. BHK-21 cells were infected with VSV-G(NiV), VSV-F(NiV), VSVΔG-G(NiV), VSVΔG-F(NiV), or rwt-VSV, then fixed and stained with mouse anti-NiV G, anti-F, or MAbs to VSV G, followed by an Alexa Fluor 594-conjugated anti-mouse secondary antibody. As shown in Fig. 2, NiV G was expressed on the cell surface, while NiV F expression appeared to be on the cell surface, as well as in cytoplasmic vesicles. This internal pattern of F expression is typical of that seen previously for NiV F protein, which is rapidly endocytosed from the cell surface (6). VSV G protein was expressed on the cell surface except where ΔG viruses were used, while cells infected with rwt-VSV showed no staining for NiV G or F protein (Fig. 2).
FIG. 2.
Cellular localization of NiV G and F proteins expressed from recombinant VSV vectors. The photos are indirect immunofluorescence microscope images of BHK-21 cells infected with the indicated viruses. Cells were fixed at 4 h postinfection and stained with either an equal mixture of two anti-VSV G MAbs (I1 and I14) or with anti-NiV G or anti-NiV F polyclonal mouse sera, followed by an anti-mouse Alexa Flour 594-conjugated secondary antibody staining. In all fields cell nuclei are shown stained with DAPI. Photographs were taken with a Nikon 80i fluorescence microscope equipped with a Cool Snap EZ charge-coupled-device camera.
To verify expression of functional NiV F and G proteins on the surface of infected cells, we coinfected cells with VSV-G(NiV) and VSV-F(NiV) and observed extensive cell-cell fusion giving rise to multinucleated cells (syncytia) that results from the cooperation of functional F and G proteins (data not shown, but see Fig. 5A). No syncytia were observed in cells singly infected with VSV-G(NiV) or VSV-F(NiV).
Immunization of mice with VSV-G(NiV) and/or VSV-F(NiV) elicits an NiV neutralizing antibody response.
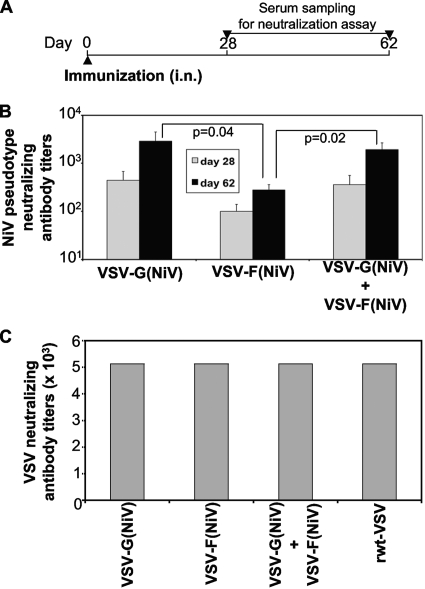
To determine whether the VSV recombinants expressing NiV G or F proteins were immunogenic, mice were immunized by the i.n. route with VSV-G(NiV) or VSV-F(NiV), either separately or in combination. A control group of mice was immunized with rwt-VSV. Serum was isolated from blood collected from these mice at 28 and 62 days postimmunization and screened for NiV nAb. The immunization timeline is given in Fig. 3 A. To measure titers of nAbs to NiV G or F proteins, we used VSVΔG-eGFP1 (19) pseudotyped with NiV G and F proteins. This is a neutralization assay similar to that described by others, which correlates well with direct determination of NiV neutralization titers (17, 34).
FIG. 3.
A single intranasal immunization of mice with live-attenuated VSVs expressing NiV G or F induces antibody neutralizing VSVΔG(NiV) pseudotypes. (A) Timeline of mice immunization indicating the day of immunization (day 0) and days for serum isolation (day 28 and 62). (B) NiV pseudotype neutralizing titer in mouse serum at 28 (gray bar) and 62 (black bar) days postimmunization. Groups of mice (n = 5) were immunized i.n. with 106 PFU of VSV-G(NiV) or VSV-F(NiV) either separately or in combination VSV-G(NiV) + VSV-F(NiV) (0.5 × 106 PFU of each virus). A control group of mice (n = 3) receiving rwt-VSV showed no NiV pseudotype neutralizing activity (not shown). All assays were performed in triplicate. Error bars indicate the standard deviation. Statistical significance of differences in nAb titer was calculated using two-tailed t test. (C) VSV neutralizing antibody titers in mouse serum at 28 days postimmunization. All assays were performed in duplicate, which gave identical results.
As shown in Fig. 3B, mice developed NiV nAbs after i.n. immunizations with VSV-G(NiV) and/or VSV-F(NiV). Immunization with VSV-G(NiV) alone or VSV-G(NiV) and VSV-F(NiV) combined induced significantly higher nAb levels (5- to 10-fold) than VSV-F(NiV) alone (Fig. 3B). The increased immunogenicity of G compared to F protein is consistent with earlier results obtained with vaccinia virus recombinants (33). We found also that serum nAb levels obtained 1 month after a single immunization using VSV vectors expressing NiV G or F were equivalent to those obtained in sera from mice primed and boosted with vaccinia virus recombinants expressing NiV G or F (see Materials and Methods). Anti-vector nAb titers directed against VSV G were also measured using pooled day 28 serum samples from each immunization group (Fig. 3C). All groups of recombinant VSV-immunized mice showed identical levels of VSV nAb (1:5,120).
Intramuscular immunization of mice with single-cycle VSV recombinants expressing NiV G or F induces NiV neutralizing antibody.
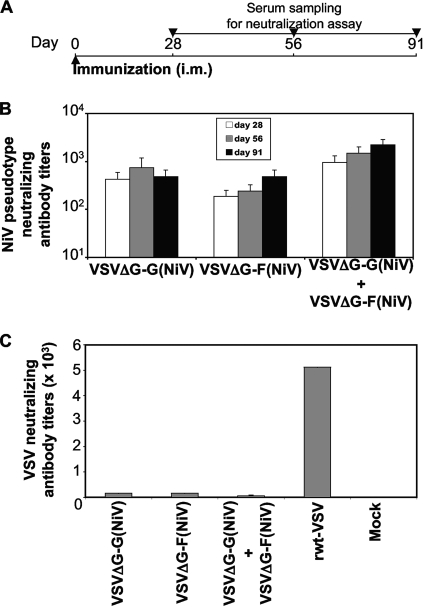
We next determined whether single-cycle VSV vectors expressing NiV G or F would also elicit nAb responses to NiV. Since the single-cycle vectors are relatively poor vectors when given i.n., yet generate strong immune responses when given by the i.m. route (26), three groups of mice were immunized i.m. with VSVΔG-G(NiV), VSVΔG-F(NiV), or a combination of the two vectors. Control mice were infected with rwt-VSV or mock infected. Serum samples obtained 28, 56, and 91 days postimmunization were used in the NiV pseudotype neutralization assay (Fig. 4 A).
FIG. 4.
Induction of neutralizing antibodies in mice following single intramuscular immunization with single-cycle VSV recombinants expressing NiV G or F. (A) Timeline of immunization indicating day of immunization (day 0) and serum sampling (days 28, 56, and 91). (B) Serum NiV pseudotype nAb titers in mice at 28 (white bar), 56 (gray bar), and 91 (black bar) days postimmunization. Groups of mice (n = 5) were immunized i.m. with 106 PFU of the indicated viruses (0.5 × 106 PFU of each virus in the combination group). A control group of mice (n = 3) receiving similar dose of rwt-VSV and another group (n = 2) left as an uninfected control (mock) showed undetectable NiV neutralizing antibody titers (not shown). All assays were performed in triplicate. Error bars indicate the standard deviation. (C) VSV neutralizing antibody titers in mouse serum at day 28 postimmunization. All assays were performed in duplicate. Error bars indicate the standard deviation.
All three single-cycle VSV immunization regimens elicited NiV nAb titers as shown in Fig. 4B. The group that received the combination of vectors, VSVΔG-G(NiV) + VSVΔG-F(NiV) showed the highest nAb titers. Consistent with the results from the replication competent vectors, the nAb titers induced by the VSVΔG-G(NiV) were significantly greater than those induced by the VSVΔG-F(NiV) vector at days 28 and 56 (P = 0.02). Also, the nAb titers induced by the combined VSVΔG-G(NiV) + VSVΔG-F(NiV) vectors were significantly greater than those induced by the VSVΔG-F(NiV) vector alone at all time points (P < 0.01).
Evaluation of VSV neutralizing titers (Fig. 4C) with day 28 serum samples showed that all mice immunized with different VSVΔG recombinants had low VSV nAb titers (ranging from 1:40 to 1:160), which is consistent with the fact that these viruses do not encode a VSV G protein but do carry G protein on the particles generated by complementation with VSV G (Fig. 4C). In contrast, the rwt-VSV-immunized mice had high VSV nAb titers (1:5,120). Sera from mock-infected animals showed undetectable levels of VSV nAbs.
VSVΔG recombinants expressing NiV G or F copropagate in the absence of VSV G complementation.
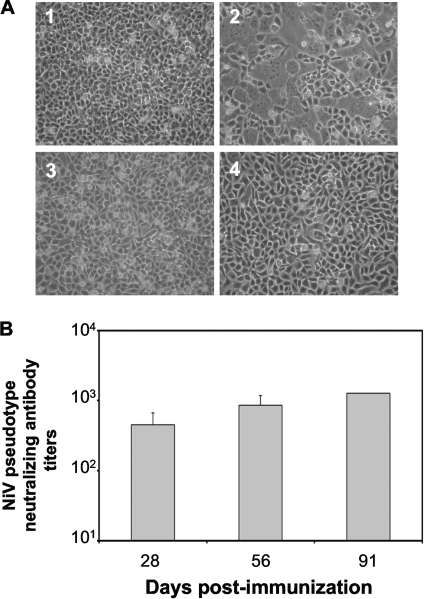
Although VSVΔG recombinants expressing foreign proteins can be highly effective vaccines (19, 26), their preparation requires complementation with VSV G. This is typically performed in cells transiently transfected with a DNA encoding VSV G or in an inducible cell line expressing VSV G (31, 36). To determine whether the VSVΔG recombinants expressing NiV G or F might be grown as a complementing pair, we initially infected BHK-21 cells separately or simultaneously with VSVΔG-G(NiV) and VSVΔG-F(NiV) that had been complemented with VSV G. The coinfected cells showed extensive fusion resulting in syncytia across the entire dish (Fig. 5 A, panel 2), while no such fusion could be seen in separately infected or mock-infected cells (Fig. 5A, panels 1, 3, and 4). Because expression of both NiV G and F is required to cause membrane fusion, the extensive fusion indicated that coinfection had occurred.
FIG. 5.
Syncytium formation and induction of NiV neutralizing antibodies by complementing VSVΔG recombinants expressing NiV G and F. (A) Monolayer of BHK-21 cells infected simultaneously with 5 MOI each of VSVΔG-G(NiV) and VSVΔG-F(NiV) (panel 2) showed extensive syncytium formation. Mock-infected cells (panel 1) or cells infected separately with 10 MOI of VSVΔG-G(NiV) (panel 3) or 10 MOI of VSVΔG-F(NiV) (panel 4) served as controls. (B) NiV pseudotype nAb titers in mouse serum at 28, 56, and 91 days after i.m. immunization with 5 × 103 PFU of copropagated mixture of VSVΔG-G(NiV) and VSVΔG-F(NiV). All assays were performed in triplicate. Error bars indicate the standard deviation.
We next collected supernatants from the coinfected cells and determined whether infectious, complemented virus could be recovered. We found that supernatants from the coinfected cells were infectious and could be passaged indefinitely (at least 25 passages) in the absence of VSV G complementation and continued to cause syncytium formation. Supernatants from the infected cells were passaged at a 1:2 dilution for the first 11 passages (P1 to P11) and thereafter at a 1:50 dilution up to passage 25 (P12 to P25). Plaque assays performed with these supernatants on BHK-21 cells showed plaques that were readily distinguishable from VSV plaques because they contained large syncytia, indicating the expression of both NiV G and F proteins. The formation of plaques by the stock was neutralized by antibody to either NiV G or NiV F. The maximal titer obtained was 106 PFU/ml by P15.
We carried out further characterization of this copropagated mixture of viruses using indirect immunofluorescence microscopy of infected cells at 24 h after infection. We found expression of both G and F proteins in the syncytia within all plaques, as would be expected (data not shown). In addition, there were single infected cells expressing G or F proteins. The single cells expressing G or F proteins were present in similar numbers, suggesting that copropagation of the particles established an approximately 1:1 ratio of the two genotypes.
A propagated stock of VSVΔG-G(NiV) and VSVΔG-F(NiV) induces nAbs in mice.
We next sought to determine whether copropagated VSVΔG-G(NiV) and VSVΔG-F(NiV) stock would induce NiV nAbs. Mice were inoculated i.m. with the copropagated stock and serum samples taken at the indicated time points postimmunization (Fig. 5B) were tested for the presence of NiV nAbs using the NiV pseudotype neutralization assay. As shown in Fig. 5B, the coinfection supernatant induced high NiV nAb titer (>1,000) by day 91 postimmunization. The serum samples were negative for any VSV neutralizing antibodies, as would be expected because the viruses were grown without VSV G complementation (data not shown).
DISCUSSION
We have reported here on the development of both replication-competent, attenuated VSV vectors and replication-deficient single-cycle VSV recombinants (lacking VSV G) expressing the NiV G or F genes. All vectors were effective at inducing NiV nAb in mice after i.n. or i.m. immunizations. Notably, we also found that replication-defective viruses expressing either NiV G or F proteins could be propagated as a complementing pair in tissue culture cells in the absence of VSV G. We further showed that cell culture supernatants containing a mixture of these complementing viruses, when inoculated in mice, elicited high levels of NiV nAbs. The nAb titers achieved with a single inoculation with any of the vectors were comparable to those obtained with priming and boosting with vaccinia vectors expressing the NiV G or F proteins. Because vaccinia virus vectors protect from lethal NiV challenge in animal models (11), it is likely that the VSV vectors would also provide protection.
Use of the single-cycle VSVΔG vector greatly reduces concerns about potential VSV pathogenesis associated with replication-competent, live-attenuated VSV vaccines. However, the production of such defective vectors requires complementation by expression of VSV G. Since VSV G expression is toxic to cells (1), large-scale production of such vectors is problematic because it requires transient DNA transfection or use of a cell line in which VSV G expression is tightly regulated (31, 36).
The novel approach we describe here, reciprocal complementation of two defective VSVs lacking the VSV G gene, eliminates the need for complementation with VSV G protein. In addition, it has the major advantage of generating a mixture of defective, complemented viruses in which no VSV G protein is present to induce anti-vector immunity. The copropagated VSVΔG-G(NiV) and VSVΔG-F(NiV) stock elicited high levels of NiV nAbs in the absence of any neutralizing antibody to the VSV G protein. Thus, this VSVΔG vector platform could be used for multiple vaccine applications without generating vector-neutralizing antibody.
When a single cell is coinfected with the replication-defective VSVΔG recombinants each expressing one of the two NiV glycoproteins, some of the virus particles that bud from the infected cell should contain both NiV G and F proteins, while the packaged genomes would be either VSVΔG-G(NiV) or VSVΔG-F(NiV). Propagation of this complementing virus mixture is relatively slow in tissue culture presumably because it is dependent on coinfection of cells with at least two different particles, one expressing the NiV G gene and the other expressing the NiV F gene. Spread of such complemented virus in animals would also be expected to be inefficient for the same reason. We observed no signs of pathogenicity in mice inoculated with the mixture of two viruses.
Because of possible biosafety concerns, we have not generated a VSVΔG recombinant expressing both NiV G and NiV F proteins. Based on our findings here, such a recombinant would likely be viable and could be an effective Nipah virus vaccine, but it would require extensive testing to rule out potential pathogenicity.
Is there a possibility of recombination occurring between complementing VSVΔG-G(NiV) and VSVΔG-F(NiV) to generate a virus expressing both NiV G and F proteins from the same genome? We think this highly unlikely for the following reasons. In our own unpublished studies, we have not been able to detect even a simple recombination event between two different defective VSVs despite the presence of a >than-800 nucleotide homology where recombination could occur. Our results are consistent with early studies that failed to detect recombination between temperature sensitive mutants of VSV falling into different complementation groups (37). A recombination event that would bring both the NiV G and F genes into one genome with the appropriate transcription start and stop signals would be have to be complex. Such a recombination would presumably require at least two nonhomologous recombination events to bring an G or F transcription unit into one of the short noncoding regions flanking the existing genes.
If such a recombination event were to occur, the virus obtained would be expected to grow to high titers and rapidly displace the complementing viruses that achieve only low titers. During 25 passages of the complementing viruses, we observed a gradual increase in titer that did not exceed 106 PFU/ml. The increase may reflect an optimization of the ratios of the two genomes.
We also looked directly for recombination by determining the nucleotide sequences upstream of the G or F genes in the mixture of ΔG viruses. To do this, we performed reverse transcription using random octamer priming on the RNA isolated from virus obtained from passage 18. We then performed PCR with the random primers and specific reverse primers near the beginning of the G or F genes. PCR products were size selected and then cloned and sequenced. We sequenced ∼750 nucleotide inserts from 32 clones. The sequences all showed that the upstream M gene sequences flanking both the G and F genes (16 clones from each) were identical to the original sequences, with the exception of a few point mutations in some clones (data not shown).
The reciprocal complementation system we have described for NiV vaccine development could be applicable to vaccine development for other paramyxoviruses or other enveloped viruses that have at least two proteins required for binding and entry into cells. It might also be applied to viruses where the functions of a single binding and entry protein could be artificially separated into two components encoded by separate genes. This approach also minimizes biosafety concerns generated by single replication-competent recombinant vectors expressing a full complement of foreign envelope proteins required for infectivity.
Acknowledgments
We thank Paul Rota for providing antisera to NiV G and F proteins.
This study was supported by NIH grant AI057158.
Footnotes
Published ahead of print on 22 December 2010.
REFERENCES
- 1.Burns, J. C., T. Friedmann, W. Driever, M. Burrascano, and J. K. Yee. 1993. Vesicular stomatitis virus G glycoprotein pseudotyped retroviral vectors: concentration to very high titer and efficient gene transfer into mammalian and nonmammalian cells. Proc. Natl. Acad. Sci. U. S. A. 90:8033-8037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chattopadhyay, A., et al. 2008. Single-dose, virus-vectored vaccine protection against Yersinia pestis challenge: CD4+ cells are required at the time of challenge for optimal protection. Vaccine 26:6329-6337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chua, K. B., et al. 2000. Nipah virus: a recently emergent deadly paramyxovirus. Science 288:1432-1435. [DOI] [PubMed] [Google Scholar]
- 4.Chua, K. B., et al. 2002. Isolation of Nipah virus from Malaysian Island flying-foxes. Microbes Infect. 4:145-151. [DOI] [PubMed] [Google Scholar]
- 5.Clarke, D. K., et al. 2007. Synergistic attenuation of vesicular stomatitis virus by combination of specific G gene truncations and N gene translocations. J. Virol. 81:2056-2064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diederich, S., M. Moll, H. D. Klenk, and A. Maisner. 2005. The Nipah virus fusion protein is cleaved within the endosomal compartment. J. Biol. Chem. 280:29899-29903. [DOI] [PubMed] [Google Scholar]
- 7.Eaton, B. T., C. C. Broder, and L. F. Wang. 2005. Hendra and Nipah viruses: pathogenesis and therapeutics. Curr. Mol. Med. 5:805-816. [DOI] [PubMed] [Google Scholar]
- 8.Enserink, M. 2004. Emerging infectious diseases. Nipah virus (or a cousin) strikes again. Science 303:1121. [DOI] [PubMed] [Google Scholar]
- 9.Fuerst, T. R., E. G. Niles, F. W. Studier, and B. Moss. 1986. Eukaryotic transient-expression system based on recombinant vaccinia virus that synthesizes bacteriophage T7 RNA polymerase. Proc. Natl. Acad. Sci. U. S. A. 83:8122-8126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Geisbert, T. W., et al. 2006. Postexposure protection of guinea pigs against a lethal Ebola virus challenge is conferred by RNA interference. J. Infect. Dis. 193:1650-1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guillaume, V., et al. 2004. Nipah virus: vaccination and passive protection studies in a hamster model. J. Virol. 78:834-840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gurley, E. S., et al. 2007. Person-to-person transmission of Nipah virus in a Bangladeshi community. Emerg. Infect. Dis. 13:1031-1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Halpin, K., and B. A. Mungall. 2007. Recent progress in henipavirus research. Comp. Immunol. Microbiol. Infect. Dis. 30:287-307. [DOI] [PubMed] [Google Scholar]
- 14.Hsu, V. P., et al. 2004. Nipah virus encephalitis reemergence, Bangladesh. Emerg. Infect. Dis. 10:2082-2087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones, S. M., et al. 2005. Live attenuated recombinant vaccine protects nonhuman primates against Ebola and Marburg viruses. Nat. Med. 11:786-790. [DOI] [PubMed] [Google Scholar]
- 16.Kahn, J. S., A. Roberts, C. Weibel, L. Buonocore, and J. K. Rose. 2001. Replication-competent or attenuated, nonpropagating vesicular stomatitis viruses expressing respiratory syncytial virus (RSV) antigens protect mice against RSV challenge. J. Virol. 75:11079-11087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kaku, Y., et al. 2009. A neutralization test for specific detection of Nipah virus antibodies using pseudotyped vesicular stomatitis virus expressing green fluorescent protein. J. Virol. Methods 160:7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kapadia, S. U., et al. 2005. Long-term protection from SARS coronavirus infection conferred by a single immunization with an attenuated VSV-based vaccine. Virology 340:174-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kapadia, S. U., I. D. Simon, and J. K. Rose. 2008. SARS vaccine based on a replication-defective recombinant vesicular stomatitis virus is more potent than one based on a replication-competent vector. Virology 376:165-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lamb, R. A., and D. Kolakofsky. 1996. Paramyxoviridae: the viruses and their replication, p. 1177-1204. In D. M. Knipe et al. (ed.), Fields virology, 3rd ed. Lippincott Raven Publishers, Philadelphia, PA.
- 21.Lawson, N. D., E. A. Stillman, M. A. Whitt, and J. K. Rose. 1995. Recombinant vesicular stomatitis viruses from DNA. Proc. Natl. Acad. Sci. U. S. A. 92:4477-4481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lefrancois, L., and D. S. Lyles. 1982. The interaction of antibody with the major surface glycoprotein of vesicular stomatitis virus. I. Analysis of neutralizing epitopes with monoclonal antibodies. Virology 121:157-167. [PubMed] [Google Scholar]
- 23.Mungall, B. A., et al. 2006. Feline model of acute Nipah virus infection and protection with a soluble glycoprotein-based subunit vaccine. J. Virol. 80:12293-12302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Niwa, H., K. Yamamura, and J. Miyazaki. 1991. Efficient selection for high-expression transfectants with a novel eukaryotic vector. Gene 108:193-199. [DOI] [PubMed] [Google Scholar]
- 25.Okuma, K., et al. 2001. Analysis of the molecules involved in human T-cell leukaemia virus type 1 entry by a vesicular stomatitis virus pseudotype bearing its envelope glycoproteins. J. Gen. Virol. 82:821-830. [DOI] [PubMed] [Google Scholar]
- 26.Publicover, J., E. Ramsburg, and J. K. Rose. 2005. A single-cycle vaccine vector based on vesicular stomatitis virus can induce immune responses comparable to those generated by a replication-competent vector. J. Virol. 79:13231-13238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Roberts, A., L. Buonocore, R. Price, J. Forman, and J. K. Rose. 1999. Attenuated vesicular stomatitis viruses as vaccine vectors. J. Virol. 73:3723-3732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roberts, A., et al. 1998. Vaccination with a recombinant vesicular stomatitis virus expressing an influenza virus hemagglutinin provides complete protection from influenza virus challenge. J. Virol. 72:4704-4711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rose, N. F., et al. 2001. An effective AIDS vaccine based on live attenuated vesicular stomatitis virus recombinants. Cell 106:539-549. [DOI] [PubMed] [Google Scholar]
- 30.Schnell, M. J., L. Buonocore, M. A. Whitt, and J. K. Rose. 1996. The minimal conserved transcription stop-start signal promotes stable expression of a foreign gene in vesicular stomatitis virus. J. Virol. 70:2318-2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schnell, M. J., J. E. Johnson, L. Buonocore, and J. K. Rose. 1997. Construction of a novel virus that targets HIV-1-infected cells and controls HIV-1 infection. Cell 90:849-857. [DOI] [PubMed] [Google Scholar]
- 32.Schwartz, J. A., et al. 2007. Vesicular stomatitis virus vectors expressing avian influenza H5 HA induce cross-neutralizing antibodies and long-term protection. Virology 366:166-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tamin, A., et al. 2002. Functional properties of the fusion and attachment glycoproteins of Nipah virus. Virology 296:190-200. [DOI] [PubMed] [Google Scholar]
- 34.Tamin, A., et al. 2009. Development of a neutralization assay for Nipah virus using pseudotype particles. J. Virol. Methods 160:1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weingartl, H. M., et al. 2006. Recombinant Nipah virus vaccines protect pigs against challenge. J. Virol. 80:7929-7938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Witko, S. E., et al. 2010. Refined methods for propagating vesicular stomatitis virus vectors that are defective for G protein expression. J. Virol. Methods 164:43-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wong, P. K. Y., A. F. Holloway, and D. V. Cormack. 1971. A search for recombination between temperature-sensitive mutants of vesicular stomatitis virus. J. Gen. Virol. 13:477-479. [DOI] [PubMed] [Google Scholar]