Abstract
Serum antibodies induced by seasonal influenza or seasonal influenza vaccination exhibit limited or no cross-reactivity against the 2009 pandemic swine-origin influenza virus of the H1N1 subtype (pH1N1). Ferrets immunized once or twice with MF59-adjuvanted seasonal influenza vaccine exhibited significantly reduced lung virus titers but no substantial clinical protection against pH1N1-associated disease. However, priming with MF59-adjuvanted seasonal influenza vaccine significantly increased the efficacy of a pandemic MF59-adjuvanted influenza vaccine against pH1N1 challenge. Elucidating the mechanism involved in this priming principle will contribute to our understanding of vaccine- and infection-induced correlates of protection. Furthermore, a practical consequence of these findings is that during an emerging pandemic, the implementation of a priming strategy with an available adjuvanted seasonal vaccine to precede the eventual pandemic vaccination campaign may be useful and life-saving.
The first influenza pandemic of the 21st century caused by the swine origin influenza virus of the H1N1 subtype (pH1N1) emerged in Mexico in 2009 and caused an as-yet-unknown number of clinical and fatal cases (28). Due to its rapid spread and the apparent absence of preexisting immunity in especially young people, there was an urgent need for a safe and effective vaccine (6). Early in the pandemic phase it became clear that seasonal influenza virus infection or vaccination with seasonal influenza vaccines did not or only marginally induce antibodies that cross-reacted with pH1N1 (5, 14). The vaccines used against seasonal influenza are so-called conventional nonadjuvanted vaccines that display suboptimal immunogenicity and reduced protection due to periodic antigenic drifts (4, 18). To enhance immunogenicity and/or broaden the immune response, there are several options: the use of alternative routes for antigen delivery, the administration of higher antigen doses, the selection of more conserved vaccine antigens, or the addition of an adjuvant to the vaccine (9). There are several adjuvants under development, most of them based on oil-in-water emulsions.
MF59 is such an adjuvant that has been well characterized and is used in a seasonal influenza vaccine that has been registered in many European and other countries since 1997. The adjuvant is an oil-in-water emulsion that contains 9.75 mg of squalene, 1.175 mg of polysorbate 80, 1.175 mg of sorbitan trioleate, sodium citrate dihydrate, and citric acid monohydrate (19). MF59 has been shown to potentiate the immunogenicity of seasonal and pandemic vaccines at all ages (20). It was the first adjuvant to be shown to successfully allow dose sparing with an H5-based vaccine and to widen the breadth of cross-clade neutralization by anti-HA antibodies (19, 25). In addition, more recently MF59 was shown to expand the repertoire of B-cell epitopes recognized by anti-HA cross-neutralizing antibodies (16). MF59-adjuvanted swine origin H1N1 vaccine has been widely used in many European and other countries during the past pandemic (7) and is now utilized for the trivalent vaccine for the season 2010-2011 which contains the new H1N1 strain. For all of these reasons, it was relevant to ask what contribution MF59 could have given to a potential effect of vaccination of seasonal H1N1 on subsequent vaccination with the swine-origin H1N1 vaccine (8).
In preclinical and clinical studies it thus has been demonstrated that the adjuvant MF59 has an antigen-sparing effect and broadens the intra-subtypic antibody response against influenza viruses upon vaccination (1, 2, 10, 16). Therefore, we investigated the potential of an MF59-adjuvanted trivalent seasonal influenza vaccine to elicit protection against pH1N1 infection in ferrets, since in this vaccine a virus strain is represented that shares an ancestor with pH1N1 (15). Recently, we have shown that immunization with an MF59-adjuvanted seasonal influenza vaccine did prime ferrets for the protective antibody response induced upon a second immunization with the MF59 adjuvanted pH1N1 vaccine (8). To obtain a more detailed understanding of the impact of different vaccination strategies, we analyzed here to what extent thus-vaccinated ferrets would be protected from pH1N1 replication in the upper and lower respiratory tracts and from pH1N1 infection-associated disease by evaluating the gross pathology and histopathological changes of their lungs.
MATERIALS AND METHODS
Vaccines.
In the present study we used commercially available seasonal trivalent vaccine with (sVacMF59) or without (sVac) MF59 as an adjuvant. Both vaccines contained envelope subunits (hemagglutinin [HA] and neuraminidase [NA]) (15 μg of HA) from the influenza viruses A/Brisbane/59/2007 (H1N1), A/Brisbane/10/2007 (H3N2), and B/Brisbane/60/2008. The subunit vaccine based on pandemic influenza virus A/California/4/2009 (H1N1) was used as a prototype pH1N1 vaccine (15 μg of HA), which was also used with (pVacMF59) or without (pVac) MF59 as an adjuvant. The ferrets received 0.5 ml of vaccine containing 0.25 ml of antigen and 0.25 ml of MF59. The adjuvant MF59 and phosphate-buffered saline (PBS) were also used to immunize control animals.
Viruses.
Influenza virus A/Netherlands/602/2009 (A/NL/602/09) (pH1N1) was isolated from a 3-year-old child that was the first laboratory-confirmed case of the pandemic influenza virus in the Netherlands (17). The virus was isolated in embryonated chicken eggs and subsequently passaged once in Madin-Darby canine kidney (MDCK) cells. The infectious virus titer (50% tissue culture infective dose [TCID50]) was determined as described previously (22).
Ferret studies.
Healthy outbred male and female ferrets (Mustela putorius furo) between 6 and 12 months of age and seronegative for antibodies against circulating influenza viruses H1N1, H3N2, and pH1N1 by hemagglutination inhibition (HI) assay were used. Two weeks prior to the start of the experiment, the animals were anesthetized by using a cocktail of ketamine (Alfasan, Woerden, Netherlands) and domitor (Orion Pharma, Espoo, Finland), and a temperature logger (DST Micro-T Ultra small temperature logger; Star-Oddi, Reykjavik, Iceland) was placed in their peritoneal cavities. This device recorded body temperature of the animals every 15 min. The animals were maintained in standard housing and provided with commercial food pellets and water ad libitum. For the challenge inoculation, the animals were placed in BSL-3 isolator units. An independent animal ethics committee of the Erasmus Medical Center (DEC consult) approved the experimental protocol before the start of the experiments.
Immunizations and infection: experiment 1.
Three groups of six ferrets each were immunized intramuscularly in a 3-week interval regimen. Animals received the following immunizations: two doses of MF59, one dose of sVacMF59, or two doses of sVacMF59 (Table 1) . At 4 weeks after the last immunization the animals were challenged intratracheally with pH1N1 at a dose of 106 TCID50 in a volume of 3 ml. On days 0, 2, and 4 after infection, nose and throat swabs were taken from the animals under anesthesia. At 4 days after challenge, the ferrets were euthanized by exsanguination under anesthesia.
TABLE 1.
Clinical parameters, percentage of lung tissue affected, and relative lung weights of ferrets 4 days after infection with pH1N1 in experiment 1
| Immunization | % Wt loss (SD) | Presence of fever | % Affected lung area (SD) | % Relative lung wta (SD) |
|---|---|---|---|---|
| MF59 | 12.9 (4.2) | Yes | 36.7 (10.3) | 1.67 (0.22) |
| sVacMF59 (one dose) | 14.0 (7.8) | Yes | 28.3 (7.5) | 1.59 (0.30) |
| sVacMF59 (two doses) | 11.4 (2.6) | Yes | 18.3 (13.3) | 1.60 (0.38) |
The relative lung weight is expressed as a percentage of the total body weight.
Immunizations and infection: experiment 2.
For the second experiment seven groups of six animals each received two immunizations at an interval of 4 weeks with different combinations of vaccines (Table 2). Animals that were primed with adjuvanted seasonal vaccine (sVacMF59) were boosted with pandemic vaccine without (pVac) or with (pVacMF59) adjuvant (groups 1 and 2). Animals primed with unadjuvanted seasonal vaccine (sVac) were boosted with sVac, pVac, or pVacMF59 (groups 3, 4, and 5). The animals in groups 6 and 7 received a mock vaccination with PBS and subsequently an immunization with pVacMF59 and PBS, respectively. A group that would receive PBS and subsequently sVacMF59 was not included in experiment 2 since results similar to those observed in groups 3 and 7 of experiment 2 could be expected by extrapolation of the results from experiment 1.
TABLE 2.
Vaccination parameters in experiment 2a
| Group | First immunization |
Second immunization |
||
|---|---|---|---|---|
| Antigen | Adjuvant | Antigen | Adjuvant | |
| 1 | sVac | MF59 | pVac | |
| 2 | sVac | MF59 | pVac | MF59 |
| 3 | sVac | sVac | ||
| 4 | sVac | pVac | ||
| 5 | sVac | pVac | MF59 | |
| 6 | PBS | pVac | MF59 | |
| 7 | PBS | PBS | PBS | PBS |
Animals were immunized intramuscularly with an interval of 4 weeks. sVac, seasonal vaccine, subunits (0.25 ml of antigen, 15 μg of HA) from influenza viruses A/Brisbane/59/2007 (H1N1), A/Brisbane/10/2007 (H3N2), and B/Brisbane/60/2008; pVac, pandemic vaccine, subunits (0.25 ml of antigen, 15 μg of HA) from virus strain A/California/04/2009 (H1N1); MF59, 0.25 ml.
At 4 weeks after the second immunization, the animals were challenged intratracheally with pH1N1 at a dose of 106 TCID50. On days 0, 1, 2, 3, and 4 after infection nose and throat swabs were taken from the animals, and on day 4 the animals were euthanized by exsanguination under total anesthesia.
Serology.
Serum samples collected prior to the first and second immunizations and prior to infection were stored at −20°C. They were tested for the presence of anti-HA antibodies by using an HI assay with 1% turkey erythrocytes (21). Subsequently, the sera were tested for the presence of virus neutralizing antibodies by using a micro virus neutralization (VN) assay (11). Sera were tested for the presence of antibodies reactive with influenza viruses A/NL/602/09 (pH1N1), A/Brisbane/59/2007 (H1N1), and A/Uruguay/716/2007 (H3N2) in the HI assay and in the VN assay (experiment 2 sera only). For this purpose, a reverse genetics virus was used with the HA and NA of the 2009 H1N1 virus and the remaining six gene segments of influenza virus A/Puerto Rico/8/34 (A/PR/8/34). The antibody titers obtained with this virus were comparable to those obtained with the wild-type pH1N1 virus (data not shown). The sera of ferrets infected with the homologous strain were used as control sera. These sera were also tested against other swine influenza H1N1 viruses: A/swine/Iowa/15/30, A/swine/Netherlands/25/80, A/Netherlands/386/86 (derived from a zoonotic infection [23]), and influenza H5N1 virus A/Vietnam/1194/04. Postinfection sera from ferrets infected with these viruses were used as positive controls.
Virus replication in the upper and lower respiratory tracts.
Samples of all lobes of the right lung and the accessory lobe were collected and snap-frozen by using a dry ice-ethanol bath and stored at −70°C until further processing. Lung samples were weighed and subsequently homogenized with a FastPrep-24 (MP Biomedicals, Eindhoven, Netherlands) in Hanks balanced salt solution containing 0.5% lactalbumin, 10% glycerol, 200 U of penicillin/ml, 200 μg of streptomycin/ml, 100 U of polymyxin B sulfate/ml, 250 μg of gentamicin/ml, and 50 U of nystatin/ml (ICN Pharmaceuticals, Zoetermeer, Netherlands) and centrifuged briefly before dilution.
After collection, nose and throat swabs were stored at −70°C in the same medium used for the processing of the lung samples. Quadruplicate 10-fold serial dilutions of lung and swab supernatants were used to determine the virus titers in confluent layers of MDCK cells as described previously (22).
Histopathology and immunohistochemistry.
The animals were necropsied according to a standard protocol. The trachea was clamped off so that the lungs would not deflate upon opening the pleural cavity. This allowed an accurate visual quantification of the areas of affected lung parenchyma. Samples for histological examination of the left lung and trachea were taken and stored in 10% neutral-buffered formalin (lungs after inflation with formalin), embedded in paraffin, sectioned at 4 μm, and stained with hematoxylin and eosin (H&E) for examination by light microscopy. Samples were taken in a standardized way and not guided by changes observed in the gross pathology. Histopathology was described, and semiquantitative assessment of influenza virus-associated inflammation in the lung was performed as described previously (Table 4) (26). For the extent of alveolitis and alveolar damage we used the following scoring scale: 0, 0%; 1, 25%; 2, 25 to 50%; and 3, >50%. The severity of alveolitis was scored as follows: 0, no inflammatory cells; 1, few inflammatory cells; 2, moderate numbers of inflammatory cells; and 3, many inflammatory cells. We also scored for presence of alveolar edema (no = 0, yes = 1), alveolar hemorrhage (no = 0, yes = 1), and type II pneumocyte hyperplasia (no = 0, yes = 1). For the severity of bronchiolitis, bronchitis, and tracheitis we used the following scale: 0, no inflammatory cells; 1, few inflammatory cells; 2, moderate numbers of inflammatory cells; and 3, many inflammatory cells. Finally, the extent of peribronchial, peribronchiolar, and perivascular infiltrates were scored as follows: 0, none; 1, one to two cells thick; 2, three to ten cells thick; and 3, more than ten cells thick. Slides were examined without knowledge of the identity of the animals. The cumulative scores for size and severity of inflammation provided the total score per animal.
Immunohistochemistry.
For the detection of influenza A virus antigen, sequential slides were stained with a monoclonal antibody (clone HB65 IgG2a [American Type Culture Collection]) against the nucleoprotein of influenza A virus. Goat anti-mouse IgG2a HRP (Southern Biotech, Birmingham, AL) was used as a secondary antibody. Peroxidase was revealed with a diaminobenzidine substrate, resulting in a deep red precipitate in the nuclei of infected cells and a less intense red staining of their cytoplasm. The sections were counterstained with hematoxylin. After determining the cell types expressing viral antigen, semiquantitative assessment of influenza virus antigen expression in the lungs was performed as reported previously (26). For the alveoli, 25 arbitrarily chosen, ×20 objective, fields of lung parenchyma in each lung section were examined by light microscopy for the presence of influenza virus nucleoprotein, without the knowledge of the identity of the animals. The cumulative scores for each animal were presented as number of positive fields per 100 fields. For the bronchi and bronchioles, the percentage of positively staining bronchial and bronchiolar epithelium was determined on every slide, and the average of the four slides was taken to provide the score per animal.
Statistical analysis.
Differences between groups were analyzed statistically using the Student t test. Differences were considered significant at P < 0.05.
RESULTS
Experiment 1: efficacy of MF59-adjuvanted seasonal influenza vaccine.
Ferrets immunized once or twice with sVac-MF59 developed HI antibodies against the seasonal H1N1 strain A/Brisbane/59/07 with a geometric mean titer (GMT) of 45 (standard deviation [SD] = 6) and 968 (SD = 3), respectively. After a single immunization four of six animals developed detectable antibody titers, whereas after two immunizations all animals tested positive. The A/Brisbane/59/07-specific antibodies did not cross-react with pH1N1 in the HI assay.
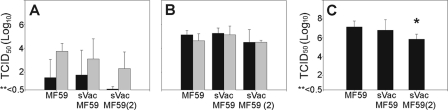
Upon infection with pH1N1 virus animals from both vaccinated and the control MF59 groups developed clinical signs such as lethargy, loss of appetite, and dyspnea from day 2 onward. All animals lost weight after infection ranging from 12.9 (SD = 4.2) to 14.0% (SD = 7.8) and 11.4% (SD = 2.6) for the animals immunized with MF59, sVac, and sVacMF59 (two immunizations), respectively (Table 1). Virus was detected in the nose on day 2 postinfection (p.i.) in at least one of six animals, and by day 4 all animals had detectable virus in the nose with GMTs of 105.6 (SD = 100.6), 104.3 (SD = 101.9), and 104.6 (SD = 100.4) for the three groups, respectively (Fig. 1A). All animals had detectable virus titers in their throats on day 2 and 4 (Fig. 1B). The differences in virus titers in the upper respiratory tract between the respective study groups were not statistically significant. On day 4 p.i. virus titers in the lungs of ferrets that had received two immunizations with sVac-MF59 were significantly lower (P = 0.003) than those in the MF59-immunized group (Fig. 1C). The reduced virus replication correlated with a reduction in gross pathological changes of the lungs (Table 1).
FIG. 1.
Virus replication in the upper and lower respiratory tracts of ferrets. Virus replication was determined in the nose (A) and throat (B) on days 2 (▪) and 4 (░⃞) p.i. and expressed as the TCID50/ml. (C) Lung virus titers were determined on day 4 p.i. and expressed as the TCID50/g of lung. (An asterisk indicates that the mean titer is significantly lower than that in the MF59-immunized group; 0.5 TCID50 is the limit of detection of the assay.)
Experiment 2: efficacy of pandemic vaccine and effects of priming and MF59 usage. (i) Serology.
After primary immunization with seasonal influenza vaccine or PBS, animals received a second immunization with seasonal vaccine, pandemic vaccine, or PBS. Both vaccines were used with or without MF59, and all groups that had received pVac in combination with MF59 developed antibody titers against the homologous strain, as detected in the HI and VN assays.
In the sVacMF59-pVac group and the sVac-pVac animals (groups 1 and 4) the mean HI antibody titers against the pandemic virus were 48.8 (SD = 5.6) and 26.2 (SD = 4.8), and the animals had VN antibody titers of 46.5 (SD = 3.6) and 18.3 (SD = 4.0), respectively. Animals that had received pVac-MF59 as a second immunization appeared to have higher antibody titers, especially when they had first been immunized with sVac-MF59 (group 2). The mean antibody titers in this group were 565.2 (SD = 1.9) compared to 163.2 (SD = 2.3) and 231.6 (SD = 2.4) in the PBS-pVacMF59 (group 6) and sVac-pVacMF59 (group 5) animals, respectively. The VN titers for these groups were 767.1 (SD = 1.6), 97.9 (SD = 4.8), and 229.0 (SD = 2.4), respectively. In the sVac-sVac animals (group 3), only a serological response against the seasonal influenza A/H1N1 virus was detected, whereas no virus-specific antibodies were detected in sera from the PBS-PBS animals (group 7).
Postimmunization sera were tested for cross-reactive antibody responses against multiple swine influenza viruses of the H1N1 subtype and H5N1 virus. Cross-reactive antibody titers were detected against two swine influenza H1N1 strains from the Netherlands: A/Netherlands/386/86 (derived from a zoonotic event) and A/swine/Netherlands/25/80 (Table 3). The ranking of GMTs in the HI assay for the different groups was identical to that of the GMTs against the homologous influenza virus. No cross-reactivity was seen with influenza virus A/swine/Iowa/15/30 H1N1 or with A/Vietnam/1194/04 H5N1.
TABLE 3.
HI and VN antibody titers against swine origin influenza A/H1N1 viruses and H5N1 virus
| Group | Immunization |
GMT (SD)a |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Swine origin H1N1 |
H5N1 (A/VN/ 1194/04) |
|||||||||||
| A/NL/602/09b |
A/NL/386/86 |
A/NL/25/80 |
A/Iowa/15/30 |
|||||||||
| First | Second | HI | VN | HI | VN | HI | VN | HI | VN | HI | VN | |
| 1 | sVacMF59 | pVac | ||||||||||
| 2 | sVacMF59 | pVacMF59 | 565 (2) | 767 (2) | 181 (2) | 18 (3) | 80 (2) | 16 (2) | <10 | <10 | <10 | <10 |
| 3 | sVac | sVac | <10 | <10 | <10 | 6 (1) | <10 | <10 | <10 | <10 | <10 | <10 |
| 4 | sVac | pVac | 26 (5) | 18 (4) | <10 | 10 (3) | <10 | 6 (1) | <10 | <10 | <10 | <10 |
| 5 | sVac | pVacMF59 | 232 (2) | 229 (2) | 45 (4) | <10 | 33 (3) | 7 (2) | <10 | <10 | <10 | <10 |
| 6 | PBS | pVacMF59 | 163 (2) | 98 (5) | 28 (3) | <10 | 27 (3) | <10 | <10 | <10 | <10 | <10 |
| 7 | PBS | PBS | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 | <10 |
Antibody titers are expressed as the geometric mean titer (GMT) with the standard deviation in parentheses. A/NL/602/09, A/Netherlands/602/2009; A/NL/386/86, A/Netherlands/386/1986; A/NL/25/80, A/Netherlands/25/1980; A/Iowa/15/30, A/swine/Iowa/15/30; A/VN/1194/04, A/Vietnam/1194/04.
Data were obtained as described by Del Giudice et al. (8).
(ii) Clinical signs.
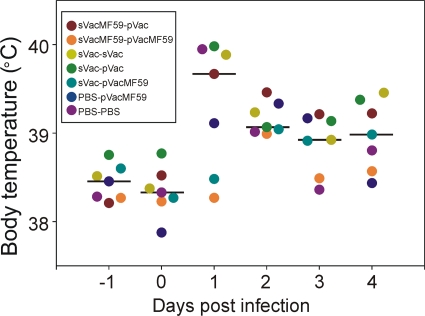
From day 1 p.i. onward, all infected animals developed symptoms including lethargy, loss of appetite, and dyspnea. These symptoms were mild in the sVacMF59-pVacMF59 animals (group 2). To quantify clinical outcome, animals were weight before infection, and on day 4 p.i. and their body temperatures were recorded during the course of the experiment. The greatest weight loss was observed in animals from groups 3, 4, 6, and 7 (12 to 17%), whereas animals from groups 1, 2, and 5 had reduced weight loss with median percentages of 10.8 (range, <0 to 17), 7.5 (2 to 16), and 10.1 (1 to 22), respectively (Table 4). The weight losses in the sVacMF59-pVac or pVacMF59 animals (groups 1 and 2) were lower than those of the other groups. Body temperature rose during day 1 p.i. in all animals (Fig. 2). The sVacMF59-pVacMF59 animals (group 2) displayed a reduced temperature increase and did not develop a sustained fever in contrast to the other groups.
TABLE 4.
Weight loss, percentage of lung tissue affected, relative lung weights, and virus titers in the lungs of ferrets 4 days after infection with pH1N1
| Group | Immunization |
Wt loss (%) |
Affected lung tissue (%) |
Relative lung wt (%) |
Lung virus titers (TCID50/g of lung)a |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| First | Second | Median | Range | Median | Range | Median | Range | Mean (SD) | nb | |
| 1 | sVacMF59 | pVacc | 10.8 | <0-17 | 5.0 | 0-20 | 0.9 | 0.8-1.3 | 2.7 (1.9) | 4 |
| 2 | sVacMF59 | pVacMF59 | 7.5 | 2-16 | 5.0 | 0-5 | 0.8 | 0.7-0.9 | Negd | 0 |
| 3 | sVac | sVac | 15.1 | 7-33 | 15.0 | 5-30 | 1.2 | 0.8-2.0 | 6.0 (0.6) | 6 |
| 4 | sVac | pVac | 15.6 | 8-23 | 7.5 | 0-20 | 1.0 | 0.7-1.3 | 3.1 (1.8) | 4 |
| 5 | sVac | pVacMF59 | 10.1 | 1-22 | 5.0 | 0-20 | 0.9 | 0.6-1.3 | 1.0 (0.0) | 1 |
| 6 | PBS | pVacMF59 | 13.0 | 6-17 | 5.0 | 0-5 | 1.0 | 0.7-1.3 | Neg | 0 |
| 7 | PBS | PBS | 14.3 | 9-30 | 40.0 | 40-80 | 1.2 | 0.8-1.9 | 5.5 (0.8) | 6 |
Data were obtained as described by Del Giudice et al. (8) and are given as a log10 values.
n, The number of animals positive for virus isolation from the lungs of six animals per group.
Weight loss data were available for 5 of 6 animals.
Neg, negative (i.e., all animals tested negative for virus replication in the lungs).
FIG. 2.
Mean body temperature of ferrets. The mean body temperatures in ferrets (n = 6 per group) were measured by a temperature logger (DST Micro-T Ultra small temperature logger; Star-Oddi, Reykjavik, Iceland) placed in the peritoneal cavity. Black bars indicate the median. (In group 3, data from four temperature loggers could be retrieved, and in group 1 and groups 6 and 7 data from five temperature loggers could be retrieved. The data from the other loggers could not be retrieved.)
(iii) Virus replication in the respiratory tract.
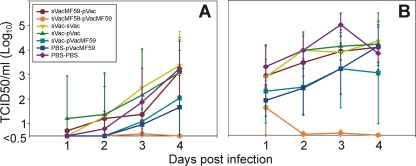
Nose and pharyngeal swabs were collected daily to determine the kinetics of virus replication in the upper respiratory tract. Not all nasal swabs tested positive or animals became positive only after day 3 or 4 p.i. However, those that were positive showed an increase in virus titers in time with maximum titers on day 4 p.i. of 103.1 (SD = 101.4), 103.4 (SD = 101.4), 103.1 (SD = 101.3), and 103.3 (SD = 101.1) for groups 1, 3, 4, and 7, respectively (Fig. 3A). Lower virus titers—102.0 (SD = 102.0) and 101.7 (SD = 101.3), respectively—were found in the ferrets that had been immunized with sVac or PBS and subsequently with pVacMF59 (groups 5 and 6). Except for one ferret with a low titer on day 3 p.i., no virus was detectable in nasal swabs from animals that had been immunized with sVac-MF59, followed by pVacMF59 (group 2). In pharyngeal swabs of virtually all animals of groups 1, 3, 4, 5, 6, and 7 virus was detected from day 1 p.i. onward, with titers increasing until day 4 p.i., resulting in mean titers of 104.1 (SD = 100.9), 104.3 (SD = 100.8), 104.2 (SD = 101.3), 103.0 (SD = 102.1), 104.1 (SD = 100.8), and 103.8 (SD = 100.4), respectively (Fig. 3B). All of the sVacMF59-pVacMF59 animals (group 2) tested negative on day 4 p.i., and most of them also tested negative on day 2 p.i.
FIG. 3.
Virus titer kinetics in the upper respiratory tract of ferrets. Virus titers were determined daily in the noses (A) and throats (B) of the infected animals (n = 6 per group). Nasal and pharyngeal swabs that tested negative were assigned a value of 0.5. (0.5 is the limit of detection of the assay.)
On day 4 p.i. the highest virus titers were found in the lungs of ferrets that had been immunized twice with sVac, 106.0 (SD = 100.6), or PBS, 105.5 (SD = 100.8) (groups 3 and 7; Table 4). Animals that had received sVacMF59 or sVac, followed by pVac (groups 1 and 4) showed lower virus titers of 102.7 (SD = 101.9) and 103.1 (SD = 101.8), respectively. The sVac-pVacMF59-immunized animals (group 6) had significantly lower virus titers—101.0 (SD = 0)—in their lungs than those of the other groups. Moreover, no virus was detected in the lungs of animals that had been immunized with sVacMF59 or PBS, and subsequently received pVacMF59 (groups 2 and 6).
(iv) Pathology.
In all ferrets, the primary macroscopic lesions were found in the lungs and consisted of pulmonary consolidation, characterized by reddening and slightly increased firmness of the lung parenchyma. The extent of pulmonary consolidation was assessed by visual quantification of the affected lung area and the relative lung weight. The average percentage of affected lung tissue was lowest in ferrets first vaccinated with sVac with or without MF59 or with PBS and subsequently with pVac with or without MF59 (groups 1, 2, 4, 5, and 6). The ferrets vaccinated twice with sVac (group 3) and the sham-vaccinated animals (group 7) had the highest percentages of affected lung tissue (Table 4). However, a slightly different pattern was found for the relative lung weights: only animals that had first received sVac with or without MF59 and subsequently pVac with MF59 (groups 2 and 5) had low relative lung weights. Other macroscopic lesions related to challenge with influenza virus were enlargement of the tracheobronchial lymph nodes (lymphadenopathy) and splenomegaly. This was considered to be an effect of the immune response following influenza virus infection of the respiratory tract. No notable lesions were found in other tissues.
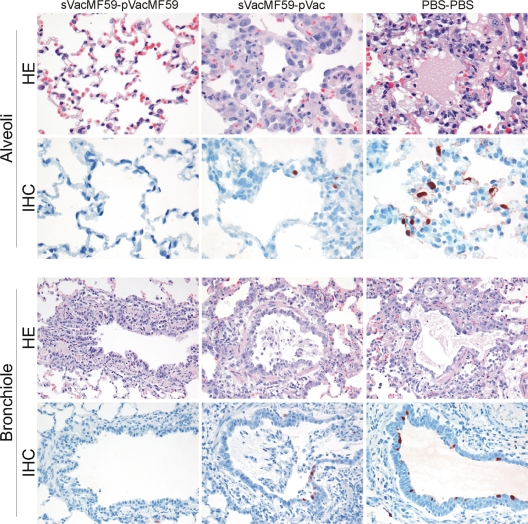
The macroscopically observed pulmonary consolidation corresponded with necrotizing broncho-interstitial pneumonia at microscopic examination (Fig. 4). This broncho-interstitial pneumonia was characterized by the presence of inflammatory cells in alveolar and bronchiolar lumina and walls and necrosis of alveolar and bronchiolar epithelium. The inflammatory cells consisted mainly of neutrophils and macrophages with variable amounts of intraluminal edema fluid, fibrin, and erythrocytes. Type II pneumocyte hyperplasia was observed as a reaction to alveolar epithelial cell damage. Mild to severe interstitial edema was seen in perivascular and peribronchiolar areas. The tracheobronchial submucosal glands in many animals exhibited infiltration of neutrophils and fewer macrophages and lymphocytes with associated epithelial cell necrosis. Less severe inflammation and epithelial necrosis were observed in bronchi and trachea. There were no indications for concurrent infections.
FIG. 4.
Lung pathology and virus replication on day 4 p.i. Histopathology and immunohistochemistry analyses were performed 4 days after infection with pH1N1. Representative slides were selected for the protected animals from group 2 (immunized with sVacMF59 and pVacMF59). For intermediate protection, representative slides were chosen from group 1 (immunized with sVacMF59 and pVac) and represent group 1 and groups 3 to 6. The unprotected animals were from group 7; these were immunized twice with PBS and developed severe pneumonia upon challenge infection. Based on the histopathology of the alveoli (first row, H&E stained) there was only mild inflammation in the sVacMF59-pVacMF59-immunized animals (group 2) with few inflammatory cells. The inflammation was intermediate in animals of group 1 and groups 3 to 6, with thickening of the septa with moderate infiltration of neutrophils, pneumocyte type II hyperplasia, and mild necrosis, and a severe pneumonia was seen in the PBS control group with severe necrosis and intra-alveolar flooding with edema fluid and inflammatory cells. Based on immunohistochemistry of the alveoli (second row), there was no antigen expression in sVacMF59-pVacMF59-immunized animals, intermediate expression of predominantly pneumocytes type II in group 1 and groups 3 to 6, and abundant expression in the PBS control group. In the bronchioles (third row) there was a mild to moderate bronchiolitis with neutrophils and macrophages and necrosis in sVacMF59-pVacMF59-immunized animals and in the animals in group 1 and groups 3 to 6, and there was severe bronchiolitis with severe necrosis in the animals in group 7. Based upon immunohistochemistry (fourth row), there was no antigen expression in sVacMF59-pVacMF59-immunized animals, mild expression in bronchiolar epithelial cells in group 1 and groups 3 to 6, and moderate expression in the PBS control group. Magnifications: ×400, alveoli; ×200, bronchioles.
The histological parameters that were scored are summarized in Table 5. For all parameters but one, the sVacMF59-pVacMF59 animals (group 2) had the lowest scores for alveolar lesions. The most severe lesions were found in the sham-vaccinated animals (group 7). Again, the sVacMF59-pVacMF59 animals (group 2) had the lowest scores for bronchiolitis and bronchitis. These scores were lower in the PBS-pVacMF59 and control animals (groups 6 and 7) than in the other groups (groups 1, 3, 4, and 5). The colocalization of perivascular and peribronchiolar cuffing with lymphocytes at areas of alveolar inflammation in lung sections suggests that the lymphocytic infiltration was a response to the alveolar inflammation.
TABLE 5.
Semiquantitative scoring for histopathology in lungs of ferrets 4 days after infection with pH1N1
| Group | Immunization |
Avga |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Score (1 to 3) |
% Positive slides |
Score (1 to 3) |
||||||||
| First | Second | Extent of alveolitis/alveolar damage | Severity of alveolitis | Alveolar edema | Alveolar hemorrhage | Type II pneumocyte hyperplasia | Severity of bronchitis/bronchiolitis | Degree of perivascular/peribronchial cuffing | Severity of tracheitis | |
| 1 | sVacMF59 | pVac | 1.92 | 1.13 | 17 | 0 | 100 | 2.21 | 2.13 | 1.17 |
| 2 | sVacMF59 | pVacMF59 | 1.58 | 0.96 | 4 | 0 | 100 | 1.13 | 1.58 | 1.17 |
| 3 | sVac | sVac | 2.85 | 1.55 | 65 | 35 | 95 | 2.00 | 2.05 | 0.17 |
| 4 | sVac | pVac | 2.29 | 1.33 | 50 | 8 | 100 | 2.04 | 2.08 | 0.50 |
| 5 | sVac | pVacMF59 | 1.92 | 1.25 | 17 | 0 | 100 | 2.00 | 1.79 | 0.80 |
| 6 | PBS | pVacMF59 | 2.50 | 1.29 | 13 | 0 | 100 | 1.96 | 2.04 | 1.30 |
| 7 | PBS | PBS | 2.75 | 1.79 | 88 | 17 | 100 | 1.67 | 1.63 | 0.50 |
Scores and values were determined as follows. Extent of alveolitis and alveolar damage: 0, 0%; 1, 25%; 2, 25 to 50%; and 3, >50%. Severity of alveolitis: 0, no inflammatory cells; 1, few inflammatory cells; 2, moderate numbers of inflammatory cells; 3, many inflammatory cells. Alveolar edema: 0, no; 1, yes. Alveolar hemorrhage: 0, no; 1, yes. Type II pneumocyte hyperplasia: 0, no; 1, yes. Severity of bronchiolitis, bronchitis, and tracheitis: 0, no inflammatory cells; 1, few inflammatory cells; 2, moderate numbers of inflammatory cells; 3, many inflammatory cells. Extent of peribronchial, peribronchiolar, and perivascular infiltrates: 0, none; 1, one to two cells thick; 2, three to ten cells thick; 3, more than 10 cells thick.
(v) Immunohistochemistry.
By immunohistochemistry, influenza virus antigen expression was visible as diffuse to granular red staining, most often stronger in the nucleus than in the cytoplasm (Fig. 4). Influenza virus antigen expression was closely associated with the presence of histological lesions at different levels of the lower respiratory tract. Antigen expression was seen predominantly in type I and II pneumocytes, alveolar macrophages, bronchiolar epithelial cells, bronchial epithelial cells, and tracheal and bronchial epithelial cells of submucosal glands. Semiquantitative scoring showed that there was no influenza virus antigen expression in the alveoli and bronchi and expression in only few cells in the bronchioles of the sVacMF59-pVacMF59 animals (group 2) (Table 6). The highest expression at all levels of the respiratory tract was seen in the control animals (group 7), followed by the PBS-pVacMF59 animals (group 6), as well as the sVac-sVac and sVac-pVac animals (groups 3 and 4).
TABLE 6.
Semiquantitative assessment of influenza virus antigen expression in the lungs of ferrets 4 days after infection with pH1N1
| Group | Immunization |
Scorea |
||||||
|---|---|---|---|---|---|---|---|---|
| Alveoli |
Bronchioles |
Bronchi |
||||||
| Median | Range | Median | Range | Median | Range | |||
| 1 | sVacMF59 | pVac | 4.5 | 0-8 | 4.5 | 0.5-6.3 | 0.5 | 0-2.8 |
| 2 | sVacMF59 | pVacMF59 | 0 | NA | 0 | 0-1.3 | 0 | NA |
| 3 | sVac | sVac | 10.5 | 5-84 | 4.5 | 1.8-6.3 | 4.5 | 1.3-8.8 |
| 4 | sVac | pVac | 7 | 1-56 | 2.13 | 1.5-7.5 | 1.75 | 0-2.8 |
| 5 | sVac | pVacMF59 | 2.5 | 0-5 | 2.5 | 0-5 | 0.25 | 0-0.3 |
| 6 | PBS | pVacMF59 | 4.5 | 1-10 | 8.75 | 2.5-20 | 1.88 | 0-15 |
| 7 | PBS | PBS | 66 | 14-96 | 5.63 | 5-6.3 | 5.75 | 5-16.3 |
For the alveoli, 25 arbitrarily chosen, ×20 objective fields of lung parenchyma in each lung section were examined by light microscopy for the presence of influenza viral nucleoprotein, without the knowledge of the identity of the animals. The cumulative scores for each animal are presented as the number of positive fields per 100 fields. For the bronchi and bronchioles, the percentages of positively staining bronchial and bronchiolar epithelium were estimated on every slide, and the average of the four slides was taken to provide the score per animal.
DISCUSSION
The primary aim of vaccination against pH1N1 influenza virus is the reduction of virus replication and the associated spread of the virus, as well as prevention of the disease and pathological changes in the respiratory tract. In the present study we have carefully described these parameters in ferrets after different vaccination regimes using combinations of MF59-adjuvanted and nonadjuvanted seasonal and pandemic influenza vaccines. The most striking finding was that prevaccination with sVacMF59 not only induced a strong priming effect on the antibody response elicited by pVacMF59 vaccination but also a strong priming effect on the protection induced with this vaccine against virus replication, associated disease, and pathological changes in the respiratory tract.
First, we showed that immunization with sVacMF59 alone, administered either once or twice, failed to induce pH1N1 influenza virus-specific antibodies and, at best, afforded modest protection. These findings are in agreement with the failure to induce antibodies cross-reactive with pH1N1 influenza virus in humans with adjuvanted and nonadjuvanted seasonal influenza vaccines (14). Apparently, the HAs of the seasonal and pandemic H1N1 strains are antigenically quite distinct, as had already been shown by using postinfection ferret serum against both strains (13).
Although sVacMF59 failed to induce cross-reactive antibodies, it did have a significant priming effect on the induction of both specific antibodies and protective responses induced by pVacMF59 against pH1N1 influenza virus. It may be speculated that this priming effect, which apparently should be attributed to the adjuvant, is caused by eliciting cross-reactive T-cell and memory B-cell responses (12, 16). Such responses may indeed contribute to protective and cross-reactive immunological memory, which may be an additional correlate of protection against influenza virus besides specific HI or VN antibodies.
Cross-reactive antibody titers against two swine influenza viruses of the H1N1 subtype indicate broadening of the antibody response by MF59 adjuvanted vaccines when used for prime and boost immunizations. This, as well as the absence of intersubtypic cross-reactive antibodies upon vaccination with adjuvanted influenza vaccines, is in line with previous data from studies using different adjuvant systems (3, 16).
In the control ferrets (group 7) and those not protected after vaccination, the character of the macroscopic and microscopic lung lesions with associated antigen expression was consistent with that described previously in pH1N1 influenza virus-infected ferrets and humans (26, 27). Immunization with sVacMF59, followed by administration of pVacMF59 (group 2), resulted in the strongest reduction of alveolar, bronchiolar, and bronchial lesions, as well as the extent of inflammation. Leaving out the adjuvant in the priming seasonal or the boosting pandemic vaccine strongly reduced the protective efficacy of vaccination against the development of alveolar lesions (groups 1 and 5). Omitting the priming vaccination reduced this protective efficacy of pVacMF59 vaccination even further (group 6). The substantial alveolar damage observed in these animals was apparently not paralleled by the levels of weight loss and increased lung weight. This could probably be explained by the delay between viral clearance and the resolution of histopathological changes. The extent of lymphocytic cuffing and the severity of bronchitis and bronchiolitis were more pronounced in the ferrets of group 1 (sVacMF59-pVac) and in those primed with sVac regardless the vaccine used for boosting (groups 3, 4, and 5) than in the ferrets of groups 2, 6, and 7. It may be speculated that this finding is related to a phenomenon recently described in Canada suggesting that subjects vaccinated with seasonal vaccine would be more at risk to develop severe pH1N1 influenza (24). However, the mechanism underlying this phenomenon is poorly understood, and more research is required to elucidate its postulated immunological basis.
Collectively, it may be concluded that the MF59-adjuvanted pandemic influenza vaccine used afforded strong protection against the development of severe pH1N1 influenza-associated lesions and disease in the ferret model. This vaccine-induced protective immunity could further be enhanced by prior vaccination with an MF59-adjuvanted seasonal vaccine. Further studies into the mechanism involved in this priming immune response will yield understanding of novel correlates of infection and vaccine-induced protection. This understanding will especially be important for future quality assessment of novel generations of adjuvanted, vectored, and live influenza virus vaccines that are expected to induce broader protection than the currently used classical seasonal vaccines. Finally, a practical consequence of these findings is that during an emerging pandemic, the implementation of a priming strategy with an available adjuvanted seasonal vaccine that precedes the eventual pandemic vaccination campaign, may be useful and life saving.
Acknowledgments
We thank P. van Run, L. Leijten, R. van Lavieren, C. W. I. Verhagen, W. van Aert, and R. C. A. Boom for technical assistance and S. van Trierum and W. Vos for biotechnical assistance.
This study was supported in part by EU FP7 EMPERIE project 223498, VIRGO (NGI), and EU FP6 FLUVAC grant 044407.
Potential conflicts of interest are as follows. K.J.S. and J.S. are full-time employed and G.V.A., G.F.R., and A.D.M.E.O. are partly employed by ViroClinics-Biosciences BV. G.D.G. and R.R. are full-time employed by Novartis Vaccines and Diagnostics. A.D.M.E.O. is CSO of ViroClinics-Biosciences BV, an affiliate of Erasmus Medical Center that collaborates with pharmaceutical companies. Novartis Vaccines and Diagnostics is financially supported by ViroClinics-Biosciences BV.
Footnotes
Published ahead of print on 5 January 2011.
REFERENCES
- 1.Ansaldi, F., et al. 2008. Cross-protection by MF59-adjuvanted influenza vaccine: neutralizing and haemagglutination-inhibiting antibody activity against A(H3N2) drifted influenza viruses. Vaccine 26:1525-1529. [DOI] [PubMed] [Google Scholar]
- 2.Ansaldi, F., et al. 2010. Antibody response against heterogeneous circulating influenza virus strains elicited by MF59- and non-adjuvanted vaccines during seasons with good or partial matching between vaccine strain and clinical isolates. Vaccine 28:4123-4129. [DOI] [PubMed] [Google Scholar]
- 3.Bosch, B. J., et al. 2010. Recombinant soluble, multimeric HA and NA exhibit distinctive types of protection against pandemic swine-origin 2009 A(H1N1) influenza virus infection in ferrets. J. Virol. 84:10366-10374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carrat, F., and A. Flahault. 2007. Influenza vaccine: the challenge of antigenic drift. Vaccine 25:6852-6862. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. 2009. Serum cross-reactive antibody response to a novel influenza A (H1N1) virus after vaccination with seasonal influenza vaccine. MMWR Morb. Mortal. Wkly. Rep. 58:521-524. [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. 2009. Prevention and control of seasonal influenza with vaccines, recommendations of the Advisory Committee on Immunization Practices (ACIP), 2009. MMWR Morb. Mortal. Wkly. Rep. 58:1-52.19145219 [Google Scholar]
- 7.Clark, T. W., et al. 2009. Trial of 2009 influenza A (H1N1) monovalent MF59-adjuvanted vaccine. N. Engl. J. Med. 361:2424-2435. [DOI] [PubMed] [Google Scholar]
- 8.Del Giudice, G., et al. 2009. Seasonal influenza vaccine provides priming for A/H1N1 immunization. Sci. Transl. Med. 1:12re1. [DOI] [PubMed] [Google Scholar]
- 9.Durando, P., G. Icardi, and F. Ansaldi. 2010. MF59-adjuvanted vaccine: a safe and useful tool to enhance and broaden protection against seasonal influenza viruses in subjects at risk. Expert Opin. Biol. Ther. 10:639-651. [DOI] [PubMed] [Google Scholar]
- 10.Forrest, H. L., et al. 2009. Single- and multiple-clade influenza A H5N1 vaccines induce cross protection in ferrets. Vaccine 27:4187-4195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Frank, A. L., J. Puck, B. J. Hughes, and T. R. Cate. 1980. Microneutralization test for influenza A and B and parainfluenza 1 and 2 viruses that uses continuous cell lines and fresh serum enhancement. J. Clin. Microbiol. 12:426-432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Galli, G., et al. 2009. Fast rise of broadly cross-reactive antibodies after boosting long-lived human memory B cells primed by an MF59 adjuvanted prepandemic vaccine. Proc. Natl. Acad. Sci. U. S. A. 106:7962-7967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garten, R. J., et al. 2009. Antigenic and genetic characteristics of swine-origin 2009 A(H1N1) influenza viruses circulating in humans. Science 325:197-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hancock, K., et al. 2009. Cross-reactive antibody responses to the 2009 pandemic H1N1 influenza virus. N. Engl. J. Med. 361:1945-1952. [DOI] [PubMed] [Google Scholar]
- 15.Igarashi, M., et al. 2010. Predicting the antigenic structure of the pandemic (H1N1) 2009 influenza virus hemagglutinin. PLoS One 5:e8553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khurana, S., et al. 2010. Vaccines with MF59 adjuvant expand the antibody repertoire to target protective sites of pandemic avian H5N1 influenza virus. Sci. Transl. Med. 2:15ra5. [DOI] [PubMed] [Google Scholar]
- 17.Munster, V. J., et al. 2009. Pathogenesis and transmission of swine-origin 2009 A (H1N1) influenza virus in ferrets. Science 325:481-483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nichol, K. L. 2003. The efficacy, effectiveness, and cost-effectiveness of inactivated influenza virus vaccines. Vaccine 21:1769-1775. [DOI] [PubMed] [Google Scholar]
- 19.Nicholson, K. G., et al. 2001. Safety and antigenicity of non-adjuvanted and MF59-adjuvanted influenza A/Duck/Singapore/97 (H5N3) vaccine: a randomised trial of two potential vaccines against H5N1 influenza. Lancet 357:1937-1943. [DOI] [PubMed] [Google Scholar]
- 20.O'Hagan, D. T., A. Wack, and A. Podda. 2007. MF59 is a safe and potent vaccine adjuvant for flu vaccines in humans: what did we learn during its development? Clin. Pharmacol. Ther. 82:740-744. [DOI] [PubMed] [Google Scholar]
- 21.Palmer, D., W. Dowle, M. Coleman, and G. Schild. 1975. Hemagglutination inhibition test, p. 25-62. In Advanced laboratory techniques for influenza diagnosis: procedural guide. U.S. Department of Health Education, Atlanta, GA.
- 22.Rimmelzwaan, G. F., M. Baars, E. C. Claas, and A. D. Osterhaus. 1998. Comparison of RNA hybridization, hemagglutination assay, titration of infectious virus, and immunofluorescence as methods for monitoring influenza virus replication in vitro. J. Virol. Methods 74:57-66. [DOI] [PubMed] [Google Scholar]
- 23.Rimmelzwaan, G. F., et al. 2001. Antigenic and genetic characterization of swine influenza A (H1N1) viruses isolated from pneumonia patients in The Netherlands. Virology 282:301-306. [DOI] [PubMed] [Google Scholar]
- 24.Skowronski, D. M., et al. 2010. Association between the 2008-09 seasonal influenza vaccine and pandemic H1N1 illness during Spring-Summer 2009: four observational studies from Canada. PLoS Med. 7:e1000258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stephenson, I., et al. 2005. Cross-reactivity to highly pathogenic avian influenza H5N1 viruses after vaccination with nonadjuvanted and MF59-adjuvanted influenza A/duck/Singapore/97 (H5N3) vaccine: a potential priming strategy. J. Infect. Dis. 191:1210-1215. [DOI] [PubMed] [Google Scholar]
- 26.van den Brand, J. M., et al. 2010. Severity of pneumonia due to new H1N1 influenza virus in ferrets is intermediate between that due to seasonal H1N1 virus and highly pathogenic avian influenza H5N1 virus. J. Infect. Dis. 201:993-999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Webb, S. A., I. M. Seppelt, and A. I. Investigators. 2009. Pandemic (H1N1) 2009 influenza (“swine flu”) in Australian and New Zealand intensive care. Crit. Care Resusc. 11:170-172. [PubMed] [Google Scholar]
- 28.World Health Organization. 2010. Pandemic (H1N1) 2009-update 97. World Health Organization, Geneva, Switzerland. http://www.who.int/csr/don/2010_04_23a/en/index.html.