Abstract
Objectives:
Research increasingly suggests that obesity is an exacerbating factor for migraine. However, it is less clear whether weight loss may help to alleviate migraine in obese individuals. We examined whether weight loss after bariatric surgery is associated with improvements in migraine headaches.
Methods:
In this prospective observational study, 24 patients who had migraine according to the ID-Migraine screener were assessed before and 6 months after bariatric surgery. At both time points, patients had their weight measured and reported on frequency of headache days, average headache pain severity, and headache-related disability over the past 90 days via the Migraine Disability Assessment questionnaire. Changes in headache measures and the relation of weight loss to these changes were assessed using paired-sample t tests and logistic regression, respectively.
Results:
Patients were mostly female (88%), middle-aged (mean age 39.3), and severely obese (mean body mass index 46.6) at baseline. Mean (±SD) number of headache days was reduced from 11.1 ± 10.3 preoperatively to 6.7 ± 8.2 postoperatively (p < 0.05), after a mean percent excess weight loss (%EWL) of 49.4%. The odds of experiencing a ≥50% reduction in headache days was related to greater %EWL, independent of surgery type (p < 0.05). Reductions in severity were also observed (p < 0.05) and the number of patients reporting moderate to severe disability decreased from 12 (50.0%) before surgery to 3 (12.5%) after surgery (p < 0.01).
Conclusions:
Severely obese migraineurs experience marked alleviation of headaches after significant weight reduction via bariatric surgery. Future studies are needed to determine whether more modest, behaviorally produced weight losses can effect similar migraine improvements.
Classification of evidence:
This study provides Class III evidence that bariatric surgery is associated with reduction of migraine headaches in severely obese individuals.
The relationship between migraine and obesity is an emerging area of research interest. Some studies have found that migraineurs who are obese have more frequent and severe headaches compared to those who have normal weight.1,2 Moreover, these associations are strongest in migraineurs with severe obesity, suggesting that greater adiposity contributes to greater exacerbation of headaches.
The notion that obesity contributes to worsening of migraine also has biological plausibility. Proinflammatory molecules such as calcitonin gene-related peptide and cytokines that are increased in obese individuals have been implicated as pain mediators in neurovascular inflammation, which generates migraine pain.3 Despite these potential shared mechanisms and epidemiologic evidence of a migraine–obesity link, no study has examined whether weight loss may help improve headaches in obese migraineurs.
The current study evaluated whether headache frequency, severity, and disability decreased in severely obese migraineurs at 6 months after bariatric surgery. Additionally, we examined if greater postoperative weight loss was related to greater headache improvements.
METHODS
Participants and procedures.
This 2-year prospective observational study was conducted from December 2007 to December 2009. Severely obese (body mass index [BMI] ≥35 kg/m2) adult (21–70 years) patients preparing to undergo Roux-en-Y gastric bypass (RYGB) or laparoscopic adjustable gastric banding (LAGB) were recruited from 3 clinics in Providence, RI. Patients who expressed interest in participating in clinical research studies during a preoperative visit were administered the ID-Migraine (ID-M), a self-administered screening instrument used and validated in the primary care setting to conduct diagnosis of migraine.4 As per standard ID-M procedures, participants who provided an affirmative response to 2 of the 3 questions regarding presence of migraine-related clinical symptoms (nausea, photophobia, and headache-related disability) were classified as migraine-positive. Additionally, in order to examine potential migraine headache improvements, participants had to report ≥1 headache days during the past 90 days to be included in the study. Height and weight, demographics, and headache variables were measured an average of 93 ± 64 days preoperatively. Headache variables and weight were measured again at 6 months (200 ± 43 days) postoperatively.
Standard protocol approvals, registrations, and patient consents.
Written informed consent was obtained from all patients participating in the study. Study procedures were approved by The Miriam Hospital Institutional Review Board, Providence, RI.
Measures.
The Migraine Disability Assessment (MIDAS) questionnaire was used to assess preoperative to postoperative headache changes.5 The MIDAS total score represents the sum of lost days and activity limitations due to headache over the past 90 days. These scores can be grouped into 4 disability grades: I (0–5 = minimal or infrequent disability), II (6–10 = mild or infrequent disability), III (11–20 = moderate disability), and IV (≥21 = severe disability). Two additional questions, not included in the total score, assess frequency of headache days and average headache pain severity (using a 0–10 scale) over the same recall period.5
Weight change was measured as percent excess weight loss (%EWL), according to standards in reporting bariatric surgery outcomes. This measure represents the percentage of excess weight that a patient has lost relative to 1983 Metropolitan Height and Weight Table for a person of medium frame.
Depression symptoms were measured via the Patient Health Questionnaire–9 (PHQ-9), a measure shown to be valid in diagnosing current depression and detecting changes in severity over time.6 Scores range from 0 to 27, with higher scores indicating greater depression severity.
Statistical methods.
Statistical analyses were conducted using SPSS for Windows, version 14.0 (SPSS, Chicago, IL). All continuous headache variables were assessed for normality of distribution. MIDAS disability and frequency variables were log transformed prior to analysis to correct for positive skew. Paired sample t tests were used to assess preoperative to postoperative changes in MIDAS variables. McNemar χ2 test was used to examine differences in the proportion of participants reporting moderate to severe disability across the 2 time points. For this analysis, MIDAS scores were collapsed into a dichotomous variable (grades I, II vs III, IV). Logistic regression was used to assess whether greater %EWL was associated with experiencing a ≥50% improvement in headache variables after adjusting for surgery type given that RYGB produces more rapid and greater weight loss compared to LAGB.7 The 50% threshold for headache improvement is considered the gold standard for treatment outcome.8 Finally, Pearson correlations were used to examine the relationship between changes in depression scores and each of the MIDAS-assessed headache measures.
RESULTS
A total of 274 participants were screened, 57 (20.8%) of whom were identified as having migraine and meeting initial inclusion criteria. Of these 57, only 29 proceeded to surgery. Twenty-four (83%) of these 29 participants completed the 6-month postoperative follow-up measures and 5 were lost to follow-up. At baseline, study completers reported a greater number of headache days compared to study noncompleters (11.1 ± 10.3 vs 2.8 ± 2.0, p = 0.001).
Participants were 39.3 ± 9.4 (range 22–61) years of age and mostly female (88%) and non-Hispanic white (71%). Participants on average reduced from a BMI of 46.6 ± 6.6 at presurgery to a BMI of 34.6 ± 7.0 at 6 months postsurgery (125.6 ± 18.0 kg to 95.4 ± 21.5 kg and 49.4 ± 23.0% EWL), with the majority (58%) having the LAGB operation.
On average, participants at baseline reported having headaches on 11 of the past 90 days (range 2–40) that caused distressing pain and severe disability.5 Separate chart reviews indicated that 5 (21%) participants had been previously diagnosed with migraine, 3 (13%) were taking prescription migraine medications, and no participants had been diagnosed with idiopathic intracranial hypertension or secondary headache disorder.
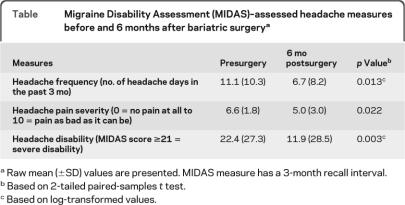
There were marked reductions in frequency of headache days, pain severity, and disability at 6 months postoperatively (table). In addition, the percentage of participants reporting moderate to severe disability decreased from presurgery to postsurgery (50.0% to 12.5%, p = 0.008). Fourteen of the 24 participants (58%) reported a reduction in headache days postoperatively, while 4 (17%) reported no change and 6 (25%) reported an increase. Greater %EWL was independently associated with a greater likelihood of experiencing a ≥50% reduction in number of headache days (odds ratio 1.07; 95% confidence interval 1.01–1.13, p = 0.038), but not with reduction in pain severity or disability.
Table.
Migraine Disability Assessment (MIDAS)–assessed headache measures before and 6 months after bariatric surgerya
Raw mean (±SD) values are presented. MIDAS measure has a 3-month recall interval.
Based on 2-tailed paired-samples t test.
Based on log-transformed values.
Participants on average reported reduced depression scores from presurgery to postsurgery (8.8 ± 6.7 to 4.3 ± 5.1, p = 0.002). However, changes on the PHQ-9 were not associated with improvements in any of the MIDAS-assessed headache measures (p > 0.20).
DISCUSSION
In the present study, we examined whether headache measures were improved in severely obese migraineurs at 6 months after bariatric surgery, the most effective treatment for clinical severe obesity.7 We found that headache frequency was markedly reduced from before to 6 months postoperatively (11.1 to 6.7 headache days), with nearly half (46%) of participants showing at least a 50% reduction, regarded as the gold standard for treatment outcome.8 The odds of experiencing a ≥50% improvement in headache frequency was higher in participants who had greater weight losses, regardless of the type of surgery that was performed. Findings also demonstrated substantial decreases in headache pain severity and related disability. Before surgery, 12 (50%) of the participants reported moderate to severe disability, indicating a high need for medical treatment.5 However, at 6 months after surgery, only 3 (12.5%) of the participants reported this degree of disability. Remarkably, headache improvements occurred postoperatively despite the fact that 70% of participants were still obese, suggesting that weight loss can help alleviate migraine in the absence of resolution of obesity.
Although associations between obesity and increased headache frequency, severity, and disability in migraineurs have been demonstrated in previous investigations,1,2 the present study is the first to prospectively document improvements in these headache measures after weight loss. While large weight losses achieved through bariatric surgery had a positive impact on migraine, it remains unclear whether smaller, behaviorally produced weight losses result in similar improvements.
Strengths of this study include the use of the validated MIDAS questionnaire and objective weight measurement. A limitation of this study is the absence of a control group, and the inability to rule out the potential influence of participant expectancy effects on reported migraine improvements. Considering the small sample size and preliminary nature of the findings, more definitive future studies should include neurologist examination to confirm ID-M screening, examination of headache changes by surgery type, and use of daily headache monitoring to optimize valid assessment of migraine headache frequency. Although in this study, improvements in depression symptoms after bariatric surgery were not related to alleviation of migraine headaches, additional research is needed to explore the importance of changes in other factors such as medication usage, physical functioning, and mental health.
The current study demonstrated marked alleviation of migraine headaches in severely obese individuals after large weight losses via bariatric surgery. Moreover, patients who had greater weight loss were more likely to experience a 50% or greater reduction in headache frequency. These findings support the recently proposed concept that weight loss may be an important part of a migraine treatment plan for obese individuals.9 Although large weight losses produced by bariatric surgery appear to positively affect migraine, future clinical trials are needed to examine whether more modest weight losses achieved through behavioral treatments can produce similar improvements. These investigations may provide a useful treatment model for gaining insight into physiologic, psychological, and behavioral mechanisms through which weight loss impacts migraine.10
ACKNOWLEDGMENT
The authors thank Jennifer Trautvetter, BA, The Miriam Hospital Weight Control and Diabetes Research Center, Providence, RI, for assistance with data collection, and the following surgeons who contributed patients to this study: Beth A. Ryder, MD, and G. Dean Roye, MD, Rhode Island Hospital/Department of Surgery, Warren Alpert Medical School of Brown University, Providence, RI; Dieter Pohl, MD, Roger Williams Hospital, Providence, RI; and Harry C. Sax, MD, Department of Surgery, Warren Alpert Medical School of Brown University, Providence, RI.
See page 1189
- %EWL
- percent excess weight loss
- BMI
- body mass index
- ID-M
- ID-Migraine
- LAGB
- laparoscopic adjustable gastric banding
- MIDAS
- Migraine Disability Assessment
- PHQ-9
- Patient Health Questionnaire–9
- RYGB
- Roux-en-Y gastric bypass.
DISCLOSURE
Dr. Bond serves on the editorial boards of Surgery for Obesity and Related Diseases and American Journal of Health Behavior and receives research support from the NIH (NIDDK/ NCI). Dr. Vithiananthan reports no disclosures. Dr. Nash serves as an Associate Editor for Annals of Behavioral Medicine and served as an Associated Editor for Journal of Behavioral Medicine; receives publishing royalties for Doing Data Analysis with SPSS version 16 (Cengage Publishing, 2009); and receives research support from the NIH/NCI. Dr. Thomas serves as a consultant for the University of Pennsylvania, School of Medicine, Center for Weight and Eating Disorders; and receives research support from the NIH, the American Diabetes Association, and The Obesity Society. Dr. Wing receives research support from the NIH (NIDDK/NHLBI/NCI).
REFERENCES
- 1. Bigal ME, Liberman JN, Lipton RB. Obesity and migraine: a population study. Neurology 2006;66:545–550 [DOI] [PubMed] [Google Scholar]
- 2. Bigal ME, Tsang A, Loder E, Serrano D, Reed ML, Lipton RB. Body mass index and episodic headaches: a population-based study. Arch Intern Med 2007;167:1964–1970 [DOI] [PubMed] [Google Scholar]
- 3. Bigal ME, Lipton RB, Holland PR, Goadsby PJ. Obesity, migraine, and chronic migraine: possible mechanisms of interaction. Neurology 2007;68:1851–1861 [DOI] [PubMed] [Google Scholar]
- 4. Lipton RB, Dodick D, Sadovsky R, et al. A self-administered screener for migraine in primary care: The ID Migraine validation study. Neurology 2003;61:375–382 [DOI] [PubMed] [Google Scholar]
- 5. Stewart WF, Lipton RB, Dowson AJ, Sawyer J. Development and testing of the Migraine Disability Assessment (MIDAS) Questionnaire to assess headache-related disability. Neurology 2001;56:S20–S28 [DOI] [PubMed] [Google Scholar]
- 6. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606–613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Maggard MA, Shugarman LR, Suttorp M, et al. Meta-analysis: surgical treatment of obesity. Ann Intern Med 2005;142:547–549 [DOI] [PubMed] [Google Scholar]
- 8. Subcommittee IHSCT Guidelines for controlled trials of drugs in migraine: second edition. Cephalalgia 2000;20:765–786 [DOI] [PubMed] [Google Scholar]
- 9. Nicholson R, Bigal M. Screening and behavioral management: obesity and weight management. Headache 2008;48:51–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bond DS, Roth J, Nash JM, Wing RR. Migraine and obesity: epidemiology, possible mechanisms, and the potential role of weight loss treatment. Obes Rev Epub 2010 July 28 [DOI] [PMC free article] [PubMed] [Google Scholar]