Abstract
(See the editorial commentary by Bray, on pages 1037–9.)
The licensed smallpox vaccine, ACAM2000, is a cell culture derivative of Dryvax. Both ACAM2000 and Dryvax are administered by skin scarification and can cause progressive vaccinia, with skin lesions that disseminate to distal sites. We have investigated the immunologic basis of the containment of vaccinia in the skin with the goal to identify safer vaccines for smallpox. Macaques were depleted systemically of T or B cells and vaccinated with either Dryvax or an attenuated vaccinia vaccine, LC16m8. B cell depletion did not affect the size of skin lesions induced by either vaccine. However, while depletion of both CD4+ and CD8+ T cells had no adverse effects on LC16m8-vaccinated animals, it caused progressive vaccinia in macaques immunized with Dryvax. As both Dryvax and LC16m8 vaccines protect healthy macaques from a lethal monkeypox intravenous challenge, our data identify LC16m8 as a safer and effective alternative to ACAM2000 and Dryvax vaccines for immunocompromised individuals.
Variola is a highly transmissible orthopox virus that causes smallpox, a generalized infection fatal in approximately one-third of infected individuals. Dryvax contributed to the worldwide eradication of smallpox and has been one of the most widely used smallpox vaccines [1, 2]. Dryvax, however, can cause fatal complications in individuals with atopic dermatitis/eczema and in immunocompromised patients due to human immunodeficiency virus (HIV) infections, chemotherapy, or conditioning for organ transplantation [3–9].
The importance of the immune system in the containment of vaccinia replication was identified in the 1950s due to cases of progressive vaccinia in infants vaccinated at birth, later identified to have congenital immune deficiencies [3]. Humoral immunity was initially considered protective, and the passive administration of vaccinia immunoglobulins (VIG) was the treatment of choice for progressive vaccinia. This method was pioneered in children by Kempe et al [10] and has been used recently, in a 28 month-old child who developed severe eczema vaccinatum via contact with his vaccinated parent, as well as in a military recruit with progressive vaccina [11, 12]. However, the efficacy of VIG remains uncertain. Indeed, boys with severe X-linked agammaglobulinemia (Bruton's disease) can be vaccinated safely [3], and there is an association of progressive vaccinia with a defect in delayed-type hypersensitivity suggesting the importance of cell-mediated responses. The recent reintroduction of smallpox vaccinations in selected “at risk” groups, such as primary care or military personnel, have again raised the issue of vaccine safety. In 2007, the Food and Drug Administration (FDA) approved ACAM2000 (Acambis), a cell culture-passaged clone of Dryvax, for use in the United States [13–17]. However, similar to Dryvax, ACAM2000 can induce severe adverse events, including myopericarditis vesicular eruptions and, as recently reported, progressive vaccinia [12, 18, 19]. Thus, understanding how vaccinia replication is controlled in the skin is instrumental for the development of a safe vaccine against smallpox [20].
In the 1970s, an attenuated replicating vaccinia virus, LC16m8, was derived from the original Lister strain by passage in primary rabbit kidney cells [21, 22]. LC16m8 contains a deletion in the B5R envelope gene, which may contribute to its attenuation [21, 23, 24]. LC16m8 has demonstrated low neuro-virulence, good protective efficacy in animal models, and its safety profile has been confirmed in more than 100,000 infants and, more recently, in more than 3000 members of the armed forces [22, 25–27].
Monkeypox infection of macaques is an appropriate model to test the immunogenicity and relative efficacy of smallpox vaccine candidates [28]. Using this model, we previously demonstrated that vaccination with Dryvax protects from systemic dissemination of monkeypox, and that antibodies to vaccinia mediate this protection [29]. In this study, we investigated the immune responses that contribute to local containment of vaccinia-induced skin lesions in macaques. We modulated the development of vaccinia specific antibody or T cell responses by depleting CD20+ B cells or both CD4+ and CD8+ T cells during immunization. Our results support the notion that T cells, and not antibodies, are important for the containment of local vaccinia replication. Moreover, our data indicate that the LC16m8 attenuated vaccine is a safer alternative to the nonattenuated ACAM2000 vaccine.
MATERIALS AND METHODS
T cell– or B cell–Depleting Antibody Treatments
To model a compromised immune system, rhesus macaques were treated with either T cell– or B cell–depleting antibodies. Eight rhesus macaques were depleted of CD4+ T cells by intravenous administration of a humanized α-CD4 antibody (huOKT4A) at a dose of 50 mg/kg on day 7. The α-CD4 treated animals were also depleted of CD8+ cells by intravenous administration at day 4 of a recombinant mouse-human chimera α-CD8a antibody (cM-T807) at a dose of 50 mg/kg (provided by Keith Reimann). Six rhesus macaques were depleted of B cells by intravenous administration on days 7 and 6 with a monoclonal mouse-human chimeric anti-human CD20 antibody (Rituxan; IDEC Pharmaceuticals Corp), at a dose of 50 mg/kg.
Vaccination and Exposure to Monkeypox
Eight α-CD4 and α-CD8 antibody treated rhesus macaques, six α-CD20 antibody treated rhesus macaques, and six untreated rhesus macaques were vaccinated with either Dryvax (Wyeth Pharmaceutical Incorporated) or LC16m8 (KAKETSUKEN) (2.5 × 105 PFU, respectively) by scarification between the scapulas.
Twenty -four adult cynomolgus macaques were vaccinated with a single inoculation of Dryvax, LC16m8 (2.5 × 105 PFU), or saline by scarification between the scapulas. Sixty days post-vaccination; the animals were inoculated intravenously with 5× 107 PFU of the monkeypox virus (Zaire 79 strain). Animals with significant weight loss, numerous pock lesions, elevated temperature, anorexia, inability to eat or drink, dehydration, or lethargy were killed Studies were performed in accordance with US FDA guidelines. All animals were cared for in accordance with the standards of the Association for the Assessment and Accreditation of Laboratory Animal Care International.
Flow Cytometry and Imaging of Skin Lesions
Mononuclear cells were isolated from blood, lymph nodes and broncho-alveolar lavage as described elsewhere [30]. Cells were stained with antibodies to CD8 APC (clone DK25) (Dako), CD20 (clone B9E9) (Beckman Coulter), CD4 PE (clone L200), and CD3 (clone SP34-2) (BD Biosciences). CD4, CD8, and CD20 antibodies used for flow cytometry were chosen as they have been shown not to compete with or mask the epitopes of the depleting antibodies [31–34].
Daily imaging of skin lesions and measurement of the size of the lesion was performed as described elsewhere [34].
Immune Responses to Vaccinia and Monkeypox Viruses
Neutralizing antibodies to vaccinia and monkeypox were measured using a plaque reduction neutralization assay. Heat-inactivated serum samples diluted and mixed with 30–50 PFU of vaccinia virus (NYCBH, ATCC No. VR-1536), were incubated at 37°C and inoculated on to duplicate VeroE6 cells overlaid with MEM, supplemented with methylcellulose, and incubated at 37°C for 2 days. Cells were stained and plaques counted. End point titers are the reciprocal of the highest dilution of serum with a mean of 50% plaque reduction. Naive macaque serum or FBS was used as a negative control; 1:10 dilutions of control serum caused minimal reduction in plaque formation. For the anti-monkeypox virus PRN assay, heat inactivated diluted serum samples were mixed with 2 ×103 PFU/mL of monkeypox virus (Zaire 79 strain) overnight at 37°C. The virus/serum mixture was added to VeroE6 cells and incubated for 1 h at 37°C. Methylcellulose was overlaid and the plates incubated for 72 h. The overlay was removed, the plates stained, the plaques enumerated, and the titer determined.
Vaccinia-specific T cells were assessed using an ELISPOT kit (Cell Sciences). Cells were stimulated with 1 × 106 PFU vaccinia virus (Western Reserve strain), concavalin A or left unstimulated and added to interferon γ (IFN-γ) coated plates the plates were developed and the frequency of IFN-γ positive spot-forming cells per 106 peripheral blood mononuclear cells (PBMC) was determined.
Detection of Vaccinia/Monkeypox DNA
DNA was extracted from blood using a DNA mini kit (Qiagen) and monkeypox DNA quantified using the LightCycler Quantitative Pan-orthopox HA polymerase chain reaction (PCR) Assay. The TaqMan MGB probe and PCR primers for the real-time PCR were designed within the hemagglutinin gene sequences (NT 164827-NT165759) in vaccinia virus strain LC16m8 genome (DDBJ sequence number: AY678275). DNA from Dryvax or LC16m8 was used as a positive control.
Statistical Analysis
Comparisons between groups in the numbers of CD4+ and CD8+ T cells and in monkeypox viral loads were performed using the Wilcoxon rank sum test. Depletion of CD20+ cell was assessed using 2-way ANOVA with Dunn's multiple comparisons post-test, and arc-sine transformed CD3+ cell percentages were analyzed using repeated measures analysis of variance. Survival post monkeypox challenge was assessed with Fisher exact test. Associations between the number of lesions and viral DNA were tested by the Spearman rank correlation. Log-transformed neutralizing antibody titers were analyzed in a repeated measures Poisson model using generalized estimating equations. To test for associations between lesion sizes and CD4+, CD8+, and CD20+ cell counts, a Box-Cox power transformation with parameter lambda = 0.33 was applied to the lesion sizes before analysis to normalize their distribution, and repeated measures analysis of variance with adjustment for the changes over time and for the α-CD4 treatment effect was performed. Product-moment correlations were calculated after adjustment for all significant effects other than cell counts.
RESULTS
Treatment with Antibody to CD20 Depletes B cells and Decreases Neutralizing Antibody Titers
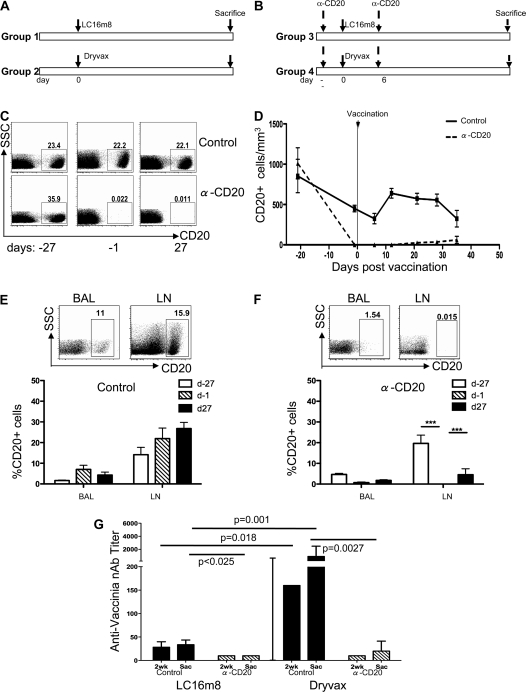
In non-human primates, antibodies to vaccinia are sufficient to protect against systemic exposure to monkeypox [29]. However, the immunologic response that regulates early vaccinia virus replication in the skin is unknown. To address the role of humoral immunity, we experimentally depleted B cells in 6 macaques using a α-CD20 depleting antibody at 6 days prior and 6 days post scarification with either LC16m8 (group 3) or Dryvax (group 4) and compared them to untreated macaques (groups 1 and 2, Figures 1A and 1B). Treatment with the α-CD20 antibody induced a persistent depletion of B cells in blood (Figures 1C and 1D), similar to our previous observations [29]. α-CD20 treatment depleted CD20+ cells in lymph nodes (LN) and in the bronchial alveolar lavage (BAL), (Figures 1E and 1F). The functional effect of B cell depletion was assessed by measuring neutralizing antibodies to vaccinia in the sera of α-CD20 treated and untreated vaccinated animals. Dryvax vaccination induced significantly higher levels of vaccinia neutralizing antibodies compared with LC16m8 at both 2 weeks post vaccination and at death 28-38 days post-vaccination (P = .018 and P = .0001 respectively) (Figure 1G). As expected, α-CD20 treatment significantly decreases the neutralizing antibody titer to vaccinia in both vaccinated groups as compared with the untreated controls (LC16m8 P < .025, Dryvax P = .0027) (Figure 1G).
Figure 1.
B cell depletion in rhesus macaques. A, Study design: 6 macaques were vaccinated with LC16m8 (n = 3) group1 or Dryvax (n = 3) group 2, in the absence of antibody treatment. B, Six macaques were given α-CD20 antibodies 6 days prior and again 6 days post-vaccination with LC16m8 (n = 3) group 3 or Dryvax (n = 3) group 4. C, Flow cytometric dot plots showing the frequency of CD20 expressing cells at baseline (day−27), day −1, and day 27, in control and antibody treated animals. D, The absolute number of CD20-expressing cells before and after vaccination in antibody-treated and untreated animals. E–F, Flow cytometric dot plots showing the frequency of CD20+ cells in the bronchial alveolar lavage (BAL) and lymph nodes (LN) (top) and the average frequency of CD20+ cells before and after vaccination in controls (E) and α-CD20 treated macaques (***) represents P < .001 (F). G, Dryvax-vaccinated (right) animals had significantly higher neutralizing antibody titers to vaccinia (NYCBH strain) compared with LC16m8-vaccinated (left), assessed at 2 weeks post-vaccination or at time of death (sac) (P = .018 and P = .001, respectively). α-CD20 treatment caused a significant reduction in anti-vaccinia neutralizing antibody titer (P = .0027 and P < .025).
B Cell Depletion Is Not Associated with Dissemination of Vaccinia-induced Skin Lesions
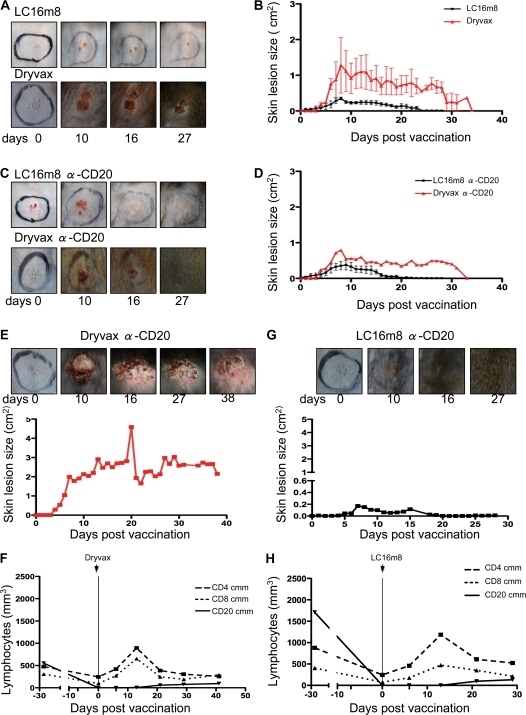
Dryvax vaccination induces a skin papule that progresses to a vesicle, a pustule then a crust, and the skin lesion is resolved typically by 21–28 days post-vaccination [35]. This primary reaction or “take” is a sign of successful vaccination. Vaccination with LC16m8 or Dryvax induced a skin lesion within 3–4 days, which progressed to a vesicle, and reached its maximum size within 2 weeks post-scarification. LC16m8-vaccinated animals had a mean lesion size <0.5 cm2 and resolved the skin lesion by 28 days post-inoculation (Figure 2A). In contrast, Dryvax-vaccinated macaques had larger skin lesions that were slower to resolve (Figure 2B). Macaques from groups 3 and 4 that were depleted of B cells but maintained normal levels of CD4+ and CD8+ T cells, did not differ from untreated macaques in their ability to resolve skin lesions induced by either vaccine (Figures 2C and 2D). An exception was a B cell–depleted, Dryvax-vaccinated macaque, P104. This animal developed a skin lesion that reached 2 cm2 in size in 8 days and had not resolved by 38 days post-scarification (Figure 2E). Analysis of the T cell number before antibody treatment demonstrated low levels of both CD4+ and CD8+ T cells in this animal, and the number of these cells further declined during α-CD20 treatment (Figure 2F). Interestingly, macaque (P102), vaccinated with LC16m8, also experienced a reduction in the number of T cells during B cell depletion but developed an average sized skin lesion that resolved by 28 days post-immunization (Figures 2G and 2H) indicating differences in the virulence of Dryvax and LC16m8.
Figure 2.
LC16m8 and Dryvax induced skin lesions in B cell–depleted animals. A, Photographs of the primary skin lesion after vaccination in two untreated control macaques vaccinated with LC16m8 or Dryvax. B, Mean skin lesion size and time to resolution in untreated LC16m8 and Dryvax vaccinated macaques. C, Photgraphs of the skin lesions after vaccination with LC16m8 or Dryvax in B cell–depleted animals. D, Mean skin lesion size and time to resolution in B cell–depleted macaques vaccinated with LC16m8 and Dryvax. E, G, Photographs of the vaccine induce lesion (top) and the mean size of the skin lesion (bottom) in a Dryvax vaccinated animal P104 (E) and an LC16m8 vaccinated animal P102 (G). F, H, Absolute number of CD4+, CD8+, and CD20+ cells/mm3 in a Dryvax vaccinated animal P104 (F) and a LC16m8 vaccinated animal P102 (H).
Altogether, these data suggest that B cells may not play a key role in the containment of vaccinia replication in the skin. Rather, they suggest that either a decrease in T cell number alone or the combination of B cell and T cell depletion may affect the size of the Dryvax-induced skin lesions.
Simultaneous Depletion of CD4+ and CD8+ T Cells in Macaques
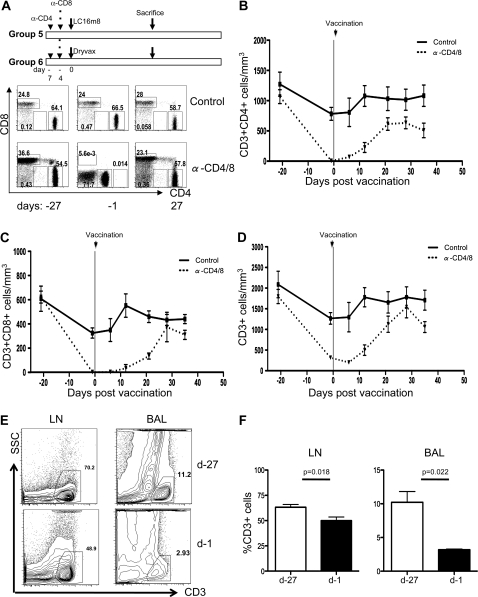
Next, we experimentally compromised the cell-mediated arm of the immune system by the depletion of both CD4+ and CD8+ T cells. Eight rhesus macaques were treated with α-CD4 and α-CD8 depleting antibodies, prior to vaccination, with either LC16m8 (group 5) or Dryvax (group 6), (Figure 3A). Representative dot plots of the frequency of CD4+ and CD8+ cells (pre-gated on CD3) before and after treatment, is shown in Figure 3A. Treatment with α-CD4 and α-CD8 antibodies induced a significant loss in the absolute number of CD4+ T cells (P = .0007) and CD8+ T cells (P = .0003) from blood when compared with untreated controls, (Figures 3B and 3C, respectively). Surprisingly, the decrease in number of CD4+ and CD8+ T cells in blood was transient and by day 28 post-vaccination, the number of CD4+ and CD8+ T cells in blood did not differ significantly in antibody-treated or untreated controls, (Figures 3B and 3C). After antibody treatment, a CD4 dim population was observed; this may be due to a down-regulation of the CD4 molecule or a preferential depletion of CD4+ T cells that express more CD4 molecules on a per cell basis. The remaining CD4+ cells would then have a lower mean florescence intensity of CD4 as observed (Figure 3A). In order to determine the extent of T cell depletion, we examined the absolute number of CD3+ cells; CD3 is expressed on all T cells and is not affected by CD4 or CD8 depleting antibodies (Figure 3D). Prior to antibody treatment, the average number of CD3 cells was 1796 cells/mm3 (day21); following treatment with α-CD4 and α-CD8 antibodies, the CD3 count fell to 314 cells/mm3 before vaccination (day1), and to 202/mm3 by 6 days post-vaccination, representing a depletion of 88.7% of CD3+ T cells (Figure 3D).
Figure 3.
α-CD4 and α-CD8 treatment induces T cell depletion in the blood and tissues of rhesus macaques. A, Study design and antibody administration schedule (top), representative flow cytometric dot plots showing the frequency of CD4+ and CD8+ T cells in blood of control untreated animals and T cell–depleted macaques before and after vaccination. B–D, Mean absolute numbers of CD4+ T cells/mm3 (B) CD8+ T cells/mm3 (C), and CD3+ cells/mm3 (D), in the blood of antibody treated and control macaques before and after vaccination. E, Representative flow cytometric plots showing the frequency of CD3+ cells in the LN and BAL before (day −27) and after (day −1) α-CD4 and -CD8 treatment. F, Mean percentage of CD3+ cells in the LN and BAL. α-CD4 and α-CD8 treatment caused a significant depletion of CD3+ cells from the LN and BAL P = .018 and P = .022.
Treatment with α-CD4 and α-CD8 also caused depletion of T cells from the LN and the BAL, similar to blood a CD4 dim population was observed. Thus, we used the frequency of CD3+ cells to evaluate the levels of T cell depletion in tissues. We found that CD3+ T cells were significantly reduced in both the LN and the BAL (P = .018 and P = .022 respectively) (Figures 3E–3F). However, the extent of the depletion was less severe in lymph nodes as compared with blood or BAL.
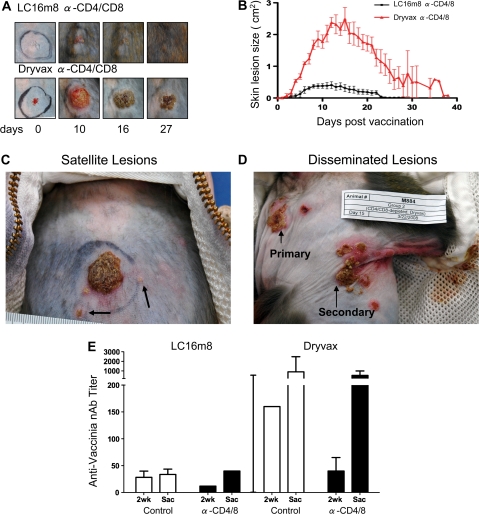
T Cells Are Essential to Prevent Dissemination of Vaccinia to Distal Sites
The role of T cells in the control of vaccinia-induced skin lesions was investigated by vaccinating macaques depleted of both CD4+ and CD8+ T cells. Macaques treated with α-CD4 and α-CD8 antibodies and vaccinated with Dryvax developed larger skin lesions, with a mean size greater than 2 cm2, compared with LC16m8-vaccinated macaques that were similarly treated (Figures 4A and 4B). Skin lesions in Dryvax-vaccinated α-CD4 and α-CD8 treated macaques had an increased resolution time of up to 38 days post-scarification, (Figure 4B). Furthermore, we observed satellite lesions in 2 of the 4 Dryvax-immunized macaques (P100 and M884), (Figures 4C and 4D, respectively). In macaque M884, the skin lesions spread from the primary site of scarification, between the scapulas, to a secondary site (Figure 4D). In contrast, all LC16m8-vaccinated T cell–depleted animals resolved their lesions by day 25 (Figure 4B), and none had satellite or distal lesions (data not shown). Because CD4+ T cell depletion can affect vaccine induced antibody responses [36], we measured the titers of neutralizing antibody to vaccinia in the T cell–depleted macaques. T cell depletion did not significantly affect the neutralizing antibody titers in neither LC16m8 vaccinated animals nor Dryvax vaccinated animals, (Figure 4E).
Figure 4.
T cell depletion favors increased lesion size and disseminating lesions in Dryvax vaccinated animals. A, Photographs of LC16m8 and Dryvax induced primary lesions in α-CD4 and α-CD8 treated macaques. B, Mean lesion size and resolution time following α-CD4 and α-CD8 treatment and vaccination with LC16m8 and Dryvax. C, Satellite lesions (arrows) surrounding the primary Dryvax vaccination site in one CD4 and CD8 depleted macaque P100. D, Lesions disseminating from the primary vaccination site, between the scapulas, to a distal site under the arm in one Dryvax vaccinated CD4 and CD8 depleted macaque M884. E, Anti-vaccinia neutralizing antibody titers in LC16m8-vaccinated (left), and Dryvax-vaccinated (right) animals, assessed at 2 weeks post-vaccination or at time of death (sac). Macaques were either untreated (control) or treated with α-CD4 and α-CD8 depleting antibodies.
Upon resolution of their primary or secondary lesions, the animals from all groups were killed to obtain the spleen, liver, heart, ovaries, jejunum, rectum, cerebrum, cerebellum, brain stem, cerebrospinal fluid, lymph nodes (axillary, inguinal and mesenteric), and blood. Skin from the site of vaccination was also collected. Real-time PCR for vaccinia DNA revealed that half of the animals that were either untreated or treated with CD20 depleting antibodies had vaccinia DNA at the site of vaccination, in contrast 6 of 8 animals that were treated with CD4 depleting antibodies had vaccinia DNA remaining at the site of vaccination at death. In addition, macaque M886 depleted of CD4/CD8 T cells and vaccinated with LC16m8, had vaccinia DNA in the draining axillary lymph node. Interestingly, 2 of the 4 Dryvax-vaccinated macaques had virus at distal sites as well. Macaque M889 had vaccinia DNA in the spleen and M884, which had disseminated vaccinia, also scored positive for viral sequences in the skin, axillary lymph nodes, blood, and the brain, corroborating a diagnosis of progressive vaccinia.
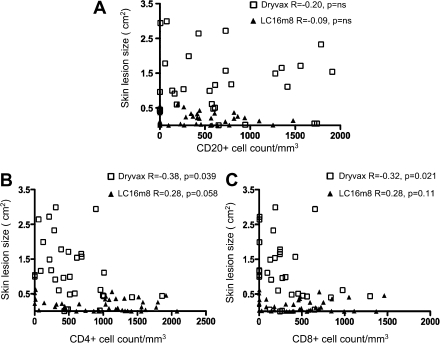
Lesion Size Inversely Correlates with T Cell but Not B Cell Count
Viral dissemination in animals depleted of T cells suggests that T cells rather than B cells contribute to the control of vaccinia replication in the skin. We correlated lesion size with the number of T cells and B cells in blood of the vaccinated macaques and found no correlation between B cell count and the size of the primary lesion regardless of the vaccine used (Figure 5A). In contrast, the number of CD4+ and CD8+ T cells in blood was inversely correlated with lesion size in Dryvax-vaccinated animals (R = −0.38; P = .039 and R = −0.32; P = .021), but not in LC16m8-vaccinated macaques (R = 0.28; P = 0.058, and R = 0.28; P = .11) (Figures 5B and 5C). These data corroborate the results presented above, that an immune system weakened by CD4 and CD8 T cell depletion is able to control the attenuated LC16m8, but not the nonattenuated Dryvax vaccine.
Figure 5.
T cell depletion is a correlate of the size of Dryvax-induced but not LC16m8-induced skin lesions. A–C, Spearman ranked correlations between the number of CD20+ cells (A), CD4+ (B), and CD8+ (C) cells/mm3 and the size of either LC16m8 or Dryvax-induced skin lesions.
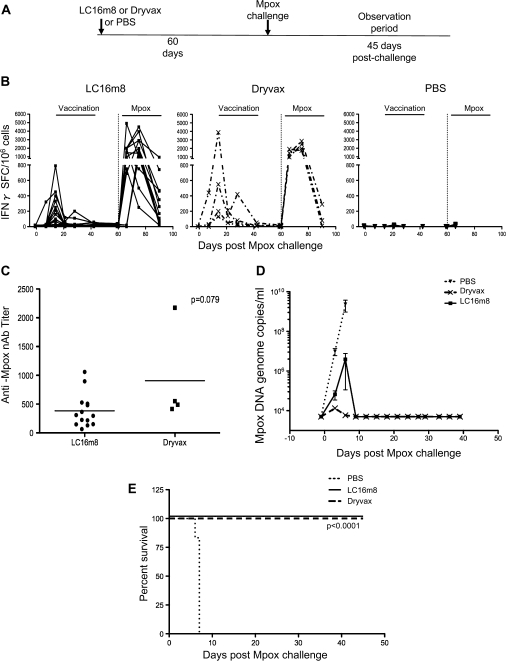
Efficacy of LC16m8 and Dryvax Vaccination Against a Lethal Monkeypox Challenge
Attenuation of live vaccines often results in a decrease in efficacy. We compared the ability of LC16m8 and Dryvax to protect from a lethal monkeypox infection by immunizing 4 cynomolgus macaques with a single inoculation of Dryvax, 14 macaques with a single inoculation of LC16m8, and 6 controls with phosphate-buffered saline (PBS). Sixty days post-vaccination, all animals were challenged intravenously with a lethal dose of monkeypox, Zaire 79 strain, (Figure 6A). Vaccination with LC16m8 or Dryvax induced comparable cell-mediated responses measured in blood by ELISPOT (Figure 6B). The 2 vaccines induced comparable neutralizing antibodies to monkeypox measured 2½ weeks prior to monkeypox exposure (Figure 6C). Intravenous infection with monkeypox induced secondary vaccinia specific T cell responses of similar frequency in Dryvax and LC16m8-vaccinated animals (Figure 6B). In contrast, unvaccinated animals failed to mount a detectable cell-mediated response to monkeypox (Figure 6B). Monkeypox DNA was detected in the blood of all challenged animals within 6 days of infection (Figure 6D). Both LC16m8 and Dryvax-vaccinated macaques had significantly lower levels of virus replication compared with unvaccinated controls (P< .0001 and P = .0095, respectively). Dryvax-vaccinated animals had lower viral loads at 3 and 6 days post-infection when compared with LC16m8-vaccinated animals; however, the difference was not statistically significant (P = .37 and P = .076) and by day 9, viral DNA was undetectable (Figure 6D). Intravenous infection with monkeypox induced characteristic skin lesions in vaccinated and control macaques. LC16m8-vaccinated animals developed varying numbers of lesions, with some animals developing less than 40 skin lesions, similar to the Dryvax-vaccinated animals, and others developing too many lesions to be counted (T), similar to the unvaccinated controls (Table 1). Despite the number of lesions, all vaccinees completely resolved skin lesions and scabs within 12–15 days of infection and fully recovered. In distinct contrast, all unvaccinated animals succumbed to monkeypox-induced disease and were either killed or found dead during morning rounds. A Fisher exact test demonstrated that the survival rates of vaccinated versus unvaccinated animals differed significantly (P < .0001) (Figure 6E). The level of monkeypox DNA in blood at 3 and 6 days post-infection directly correlated to the number of lesions at day 6 (R = 0.61; P = .0086 and R = 0.54; P = .022, respectively). Thus, while the level of early control of monkeypox replication and the resulting lesions varied in LC16m8-vaccinated animals, LC16m8 completely prevented disease progression and death, similar to Dryvax.
Figure 6.
LC16m8 and Dryvax protect cynomologus macaques from a lethal monkeypox intravenous challenge. A, Study design: 60 days post-scarification with LC16m8, Dryvax or PBS, macaques were challenged with monkeypox and monitored for 45 days. B, Monkeypox specific T cell responses after vaccination and monkeypox challenge in LC16m8 vaccinated (n = 14, left) Dryvax vaccinated (n = 4, middle) and unvaccinated macaques (n = 6, right) measured by IFN-γ-specific ELISPOTs. C, Monkeypox neutralizing antibody titers measured in vaccinated animals 2½ weeks prior to monkeypox challenge, ie, 42 days post-vaccination. D, Monkeypox DNA measured by quantitative PCR in the blood of LC16m8 or Dryvax vaccinated and unvaccinated macaques. E, Percentage of animals surviving after monkeypox challenge. A Fisher exact test demonstrated that the difference in survival between vaccinated and unvaccinated animals was statistically significant P < .0001(E).
Table 1.
Number of Skin Lesions Following Monkeypox Challenge
| Vaccine | Animal no. | 0 | 3 | 6 | 9 | 12 | 15 | 18 | 21 | 24 |
| LC16m8 | 3955 | 0 | 0 | 15 | s | 0 | 0 | 0 | 0 | 0 |
| LC16m8 | 3956 | 0 | 0 | 125 | s | 0 | 0 | 0 | 0 | 0 |
| LC16m8 | 3957 | 0 | 0 | 146 | s | 0 | 0 | 0 | 0 | 0 |
| LC16m8 | 3959 | 0 | 0 | 94 | s | 0 | 0 | 0 | 0 | 0 |
| LC16m8 | 3960 | 0 | 0 | 42 | s | 0 | 0 | 0 | 0 | 0 |
| LC16m8 | 3962 | 0 | 0 | 22 | 22 | s | 0 | 0 | 0 | 0 |
| LC16m8 | 3963 | 0 | 0 | 12 | 11 | s | 0 | 0 | 0 | 0 |
| LC16m8 | 3965 | 0 | 0 | T | 195 | s | 0 | 0 | 0 | 0 |
| LC16m8 | 3967 | 0 | 94 | T | s | 0 | 0 | 0 | 0 | 0 |
| LC16m8 | 3968 | 0 | 6 | 93 | 88 | s | 0 | 0 | 0 | 0 |
| LC16m8 | 3969 | 0 | T | T | s | 0 | 0 | 0 | 0 | 0 |
| LC16m8 | 3970 | 0 | 0 | 75 | s | 0 | 0 | 0 | 0 | 0 |
| LC16m8 | 3971 | 0 | 0 | 54 | s | 0 | 0 | 0 | 0 | 0 |
| LC16m8 | 3976 | 0 | 0 | 64 | s | 0 | 0 | 0 | 0 | 0 |
| Dryvax | 3958 | 0 | 0 | 39 | s | 0 | 0 | 0 | 0 | 0 |
| Dryvax | 3961 | 0 | 0 | 31 | s | 0 | 0 | 0 | 0 | 0 |
| Dryvax | 3972 | 0 | 0 | 23 | s | 0 | 0 | 0 | 0 | 0 |
| Dryvax | 3973 | 0 | 0 | 1 | s | 0 | 0 | 0 | 0 | 0 |
| PBS | 3964 | 0 | 7 | T | x | |||||
| PBS | 3966 | 0 | 0 | T | x | |||||
| PBS | 3974 | 0 | 10 | T | d | |||||
| PBS | 3975 | 0 | 4 | T | T | d | ||||
| PBS | 3977 | 0 | 0 | T | d | |||||
| PBS | 3978 | 0 | 0 | T | d |
NOTE. T = too many to be counted, x=killed, d=found dead during morning rounds, s=scabs.
DISCUSSION
Following the cessation of smallpox vaccination, there has been a decline in population immunity as evidenced, in part, by the 2003 outbreak of monkeypox that affected both vaccinated and unvaccinated individuals [37]. The potential release of smallpox as a biological weapon has highlighted the need for a vaccine that confers protection from disease. However, the safety of Dryvax and its derivative ACAM2000, remains a concern, especially because of the HIV-1 pandemic, the large proportion of the population affected by atopic dermatitis/eczema, and the increased practice of iatrogenic immune suppression in cancer treatment and organ transplantation [35, 38]. Indeed, progressive vaccinia has occurred in Dryvax and ACAM2000 vaccinees [3, 12, 14–18], and the first case of severe eczema vaccinatum since 1972 was recently reported in a child whose father had been vaccinated [11]. Our data in non-human primates confirm data in mice that suggest LC16m8 may be a safe alternative for populations at risk for vaccinia- associated adverse effects [39]. Our study assessed the safety of LC16m8 and Dryvax in immunocompromised non-human primates, modeled by pharmacological depletion of CD4+ and CD8+ T cells or B cells. Our novel findings include the importance of T cells for the prevention of progressive vaccinia and the safety of LC16m8 in immunocompromised non-human primates.
Our study does not, however, identify which cell(s) mediate the containment of vaccinia replication in the skin, since our experimental approach depleted CD8+ cells that include NK cells in macaques and CD4+T cells including T regulatory cells (Tregs). The lack or dysfunction of NK cells and T regulatory cells has been independently described to worsen the severity of eczema vaccinatum in mouse models [40, 41], and both are decreased in patients in atopic dermatitis [42–45]. Furthermore, rhesus macaques are susceptible to atopic dermatitis [46]; thus, with some manipulation, this model of CD4 and CD8 depletion could elucidate the immunologic basis of the susceptibility of patients with atopic dermatitis to eczema vaccinatum. In conclusion, our data suggest that LC16m8 may be a safer vaccine not only for HIV-infected individuals but also for patients with atopic dermatitis/eczema.
Funding
This research was partially funded by the intramural budget of Dr. Franchini at the National Institute of Health and through a Collaborative Research and Development Agreement by the Chemo-Sero-Therapeutic Research Institute.
Acknowledgments
We would like to thank A.Weissman for critical reading of the manuscript and T.Habina for editorial assistance, K. McKinnon for her help in flow cytometry, and S. Orndorf, J. Treece, Dr. D. Weiss, Dr. P. Markham, Dr. C. Empig, and Mr. K. Higgins for the coordination and execution of the animal handling.
References
- 1.Fenner F, Henderson DA, Arita I, Jezek Z, Ladnyi I. Smallpox and its eradication. Geneva: World Health Organization; 1988. [Google Scholar]
- 2.Henderson DA. The looming threat of bioterrorism. Science. 1999;283:1279–82. doi: 10.1126/science.283.5406.1279. [DOI] [PubMed] [Google Scholar]
- 3.Bray M, Wright ME. Progressive vaccinia. Clin Infect Dis. 2003;36:766–74. doi: 10.1086/374244. [DOI] [PubMed] [Google Scholar]
- 4.Chen RT, Lane JM. Myocarditis: the unexpected return of smallpox vaccine adverse events. Lancet. 2003;362:1345–6. doi: 10.1016/S0140-6736(03)14674-0. [DOI] [PubMed] [Google Scholar]
- 5.Fulginiti VA, Papier A, Lane JM, Neff JM, Henderson DA. Smallpox vaccination: a review, part II. Adverse events. Clin Infect Dis. 2003;37:251–71. doi: 10.1086/375825. [DOI] [PubMed] [Google Scholar]
- 6.Lane JM, Ruben FL, Neff JM, Millar JD. Complications of smallpox vaccination, 1968. N Engl J Med. 969;281:1201–8. doi: 10.1056/NEJM196911272812201. [DOI] [PubMed] [Google Scholar]
- 7.Bray M. Pathogenesis of potential antiviral therapy of complications of smallpox vaccination. Antivir Res. 2003 doi: 10.1016/s0166-3542(03)00008-1. In press. [DOI] [PubMed] [Google Scholar]
- 8.Goldstein JA, Neff JM, Lane JM, Koplan JP. Smallpox vaccination reactions, prophylaxis, and therapy of complications. Pediatrics. 1975;55:342–7. [PubMed] [Google Scholar]
- 9.Redfield RR, Wright DC, James WD, Jones TS, Brown C, Burke DS. Disseminated vaccinia in a military recruit with human immunodeficiency virus (HIV) disease. N Engl J Med. 1987;316:673–6. doi: 10.1056/NEJM198703123161106. [DOI] [PubMed] [Google Scholar]
- 10.Kempe CH. Studies smallpox and complications of smallpox vaccination. Pediatrics. 1960;26:176–89. [PubMed] [Google Scholar]
- 11.Vora S, Damon I, Fulginiti V, et al. Severe eczema vaccinatum in a household contact of a smallpox vaccinee. Clin Infect Dis. 2008;46:1555–61. doi: 10.1086/587668. [DOI] [PubMed] [Google Scholar]
- 12.Progressive vaccinia in a military smallpox vaccinee - United States, 2009. MMWR Morb Mortal Wkly Rep. 009;58:532–6. [PubMed] [Google Scholar]
- 13.Greenberg RN, Kennedy JS. ACAM2000: a newly licensed cell culture-based live vaccinia smallpox vaccine. Expert Opin Investig Drugs. 2008;17:555–64. doi: 10.1517/13543784.17.4.555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Handley L, Buller RM, Frey SE, Bellone C, Parker S. The new ACAM2000 vaccine and other therapies to control orthopoxvirus outbreaks and bioterror attacks. Expert Rev Vaccines. 2009;8:841–50. doi: 10.1586/erv.09.55. [DOI] [PubMed] [Google Scholar]
- 15.Nalca A, Zumbrun EE. ACAM2000: the new smallpox vaccine for United States Strategic National Stockpile. Drug Des Devel Ther. 2010;4:71–9. doi: 10.2147/dddt.s3687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frey SE, Newman FK, Kennedy JS, et al. Comparison of the safety and immunogenicity of ACAM1000, ACAM2000 and Dryvax in healthy vaccinia-naive adults. Vaccine. 2009;27:1637–44. doi: 10.1016/j.vaccine.2008.11.079. [DOI] [PubMed] [Google Scholar]
- 17.Marriott KA, Parkinson CV, Morefield SI, Davenport R, Nichols R, Monath TP. Clonal vaccinia virus grown in cell culture fully protects monkeys from lethal monkeypox challenge. Vaccine. 2008;26:581–8. doi: 10.1016/j.vaccine.2007.10.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beachkofsky TM, Carrizales SC, Bidinger JJ, Hrncir DE, Whittemore DE, Hivnor CM. Adverse events following smallpox vaccination with ACAM2000 in a military population. Arch Dermatol. 2010;146:656–61. doi: 10.1001/archdermatol.2010.46. [DOI] [PubMed] [Google Scholar]
- 19.Artenstein AW, Johnson C, Marbury TC, et al. A novel, cell culture-derived smallpox vaccine in vaccinia-naive adults. Vaccine. 2005;23:3301–9. doi: 10.1016/j.vaccine.2005.01.079. [DOI] [PubMed] [Google Scholar]
- 20.Slifka MK. The Future of smallpox vaccination: is MVA the key? Med Immunol. 2005;4:2. doi: 10.1186/1476-9433-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kenner J, Cameron F, Empig C, Jobes DV, Gurwith M. LC16m8: an attenuated smallpox vaccine. Vaccine. 2006;24:7009–22. doi: 10.1016/j.vaccine.2006.03.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hashizume S, Yoshizawa H, Morita M, Suzuki K. Proceedings of the Workshop on vaccinia Viruses as Vectors for vaccine Antigens. 1984. pp. 87–8. [Google Scholar]
- 23.Morikawa S, Sakiyama T, Hasegawa H, et al. An attenuated LC16m8 smallpox vaccine: analysis of full-genome sequence and induction of immune protection. J Virol. 2005;79:11873–91. doi: 10.1128/JVI.79.18.11873-11891.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Saijo M, Ami Y, Suzaki Y, et al. LC16m8, a highly attenuated vaccinia virus vaccine lacking expression of the membrane protein B5R, protects monkeys from monkeypox. J Virol. 2006;80:5179–88. doi: 10.1128/JVI.02642-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Empig C, Kenner JR, Perret-Gentil M, et al. Highly attenuated smallpox vaccine protects rabbits and mice against pathogenic orthopoxvirus challenge. Vaccine. 2006;24:3686–94. doi: 10.1016/j.vaccine.2005.03.029. [DOI] [PubMed] [Google Scholar]
- 26.Saito T, Fujii T, Kanatani Y, et al. Clinical and immunological response to attenuated tissue-cultured smallpox vaccine LC16m8. JAMA. 2009;301:1025–33. doi: 10.1001/jama.2009.289. [DOI] [PubMed] [Google Scholar]
- 27.Meseda CA, Mayer AE, Kumar A, et al. Comparative evaluation of the immune response and protection engendered by LC16m8 and Dryvax smallpox vaccines in a mouse model. Clin Vaccine Immunol. 2009 doi: 10.1128/CVI.00040-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zaucha GM, Jahrling PB, Geisbert TW, Swearengen JR, Hensley L. The pathology of experimental aerosolized monkeypox virus infection in cynomolgus monkeys (Macaca fascicularis) Lab Invest. 2001;81:1581–600. doi: 10.1038/labinvest.3780373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Edghill-Smith Y, Golding H, Manischewitz J, et al. Smallpox vaccine-induced antibodies are necessary and sufficient for protection against monkeypox virus. Nat Med. 2005;11:740–7. doi: 10.1038/nm1261. [DOI] [PubMed] [Google Scholar]
- 30.Gordon SN, Weissman AR, Cecchinato V, et al. Preexisting infection with human T-cell lymphotropic virus type 2 neither exacerbates nor attenuates simian immunodeficiency virus SIVmac251 infection in macaques. J Virol. 2010;84:3043–58. doi: 10.1128/JVI.01655-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schmitz JE, Simon MA, Kuroda MJ, et al. A nonhuman primate model for the selective elimination of CD8+ lymphocytes using a mouse-human chimeric monoclonal antibody. Am J Pathol. 1999;154:1923–32. doi: 10.1016/S0002-9440(10)65450-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schroder C, Azimzadeh AM, Wu G, Price JO, Atkinson JB, Pierson RN. Anti-CD20 treatment depletes B-cells in blood and lymphatic tissue of cynomolgus monkeys. Transpl Immunol. 2003;12:19–28. doi: 10.1016/S0966-3274(03)00059-5. [DOI] [PubMed] [Google Scholar]
- 33.Engram JC, Cervasi B, Borghans JA, et al. Lineage-specific T-cell reconstitution following in vivo CD4+ and CD8+ lymphocyte depletion in nonhuman primates. Blood. 2010;116:748–58. doi: 10.1182/blood-2010-01-263814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Edghill-Smith Y, Venzon D, Karpova T, et al. Modeling a safer smallpox vaccination regimen, for human immunodeficiency virus type 1-infected patients, in immunocompromised macaques. J Infect Dis. 2003;188:1181–91. doi: 10.1086/378518. [DOI] [PubMed] [Google Scholar]
- 35.Rotz LD, Dotson DA, Damon IK, Becher JA. Vaccinia (smallpox) vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2001. MMWR Recomm Rep. 001;50(RR-10):1–25. [PubMed] [Google Scholar]
- 36.Vaccari M, Mattapallil J, Song K, et al. Reduced protection from simian immunodeficiency virus SIVmac251 infection afforded by memory CD8+ T cells induced by vaccination during CD4+ T-cell deficiency. J Virol. 2008;82:9629–38. doi: 10.1128/JVI.00893-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Karem KL, Reynolds M, Hughes C, et al. Monkeypox-induced immunity and failure of childhood smallpox vaccination to provide complete protection. Clin Vaccine Immunol. 2007;14:1318–27. doi: 10.1128/CVI.00148-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Aragon TJ, Ulrich S, Fernyak S, Rutherford GW. Risks of serious complications and death from smallpox vaccination: a systematic review of the United States experience, 1963-1968. MC Public Health. 2003;3:26. doi: 10.1186/1471-2458-3-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kidokoro M, Tashiro M, Shida H. Genetically stable and fully effective smallpox vaccine strain constructed from highly attenuated vaccinia LC16m8. Proc Natl Acad Sci U S A. 2005;102:4152–7. doi: 10.1073/pnas.0406671102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Freyschmidt EJ, Mathias CB, Diaz N, et al. Skin inflammation arising from cutaneous regulatory T cell deficiency leads to impaired viral immune responses. J Immunol. 2010;185:1295–302. doi: 10.4049/jimmunol.0903144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kawakami Y, Tomimori Y, Yumoto K, et al. Inhibition of NK cell activity by IL-17 allows vaccinia virus to induce severe skin lesions in a mouse model of eczema vaccinatum. J Exp Med. 2009;206:1219–25. doi: 10.1084/jem.20082835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jensen JR, Sand TT, Jorgensen AS, Thestrup-Pedersen K. Modulation of natural killer cell activity in patients with atopic dermatitis. J Invest Dermatol. 1984;82:30–4. doi: 10.1111/1523-1747.ep12259055. [DOI] [PubMed] [Google Scholar]
- 43.Lever RS, Lesko MJ, Mackie RM, Parrott DM. Natural-killer-cell activity in atopic dermatitis. Clin Allergy. 1984;14:483–90. doi: 10.1111/j.1365-2222.1984.tb02232.x. [DOI] [PubMed] [Google Scholar]
- 44.Verhagen J, Akdis M, Traidl-Hoffmann C, et al. Absence of T-regulatory cell expression and function in atopic dermatitis skin. J Allergy Clin Immunol. 2006;117:176–83. doi: 10.1016/j.jaci.2005.10.040. [DOI] [PubMed] [Google Scholar]
- 45.Orihara K, Narita M, Tobe T, et al. Circulating Foxp3+CD4+ cell numbers in atopic patients and healthy control subjects. J Allergy Clin Immunol. 2007;120:960–2. doi: 10.1016/j.jaci.2007.05.036. [DOI] [PubMed] [Google Scholar]
- 46.Torreilles SL, Luong RH, Felt SA, McClure DE. Tacrolimus ointment: a novel and effective topical treatment of localized atopic dermatitis in a rhesus macaque (Macaca mulatta) J Am Assoc Lab Anim Sci. 2009;48:307–11. [PMC free article] [PubMed] [Google Scholar]