Abstract
AIM: To evaluate the diagnostic values of serum autoantibodies against matrix metalloproteinase-7 (MMP-7) in patients with esophageal squamous cell carcinoma (ESCC).
METHODS: The MMP-7 cDNA was cloned from ESCC tissues, and MMP-7 was expressed and purified from a prokaryotic system. MMP-7 autoantibodies were then measured in sera from 50 patients with primary ESCC and 58 risk-matched controls, using a reverse capture enzyme-linked immunosorbent assay (ELISA) in which autoantibodies to MMP-7 bound to the purified MMP-7 proteins. In addition, MMP-7 autoantibody levels in sera from 38 gastric cancer patients and from control serum samples were also tested.
RESULTS: The optimum conditions for recombinant MMP-7 protein expression were determined as 0.04 mmol/L Isopropyl-β-D-Thiogalactopyranoside (IPTG) induction at 37°C for four hours. The levels of serum autoantibodies against MMP-7 were significantly higher in patients with ESCC than in the matched-control samples (OD450 = 1.69 ± 0.08 vs OD450 = 1.55 ± 0.10, P < 0.001). The area under the receiver operating characteristic (ROC) curve was 0.87. The sensitivity and specificity for detection of ESCC were 78.0% and 81.0%, respectively, when the OD450 value was greater than 1.65. Although the levels of autoantibodies against MMP-7 were also significantly higher in patients with gastric cancer compared to control samples (OD450 = 1.62 ± 0.06 vs OD450 = 1.55 ± 0.10, P < 0.001), the diagnostic accuracy was less significant than in ESCC patients. The area of ROC curve was 0.75, whereas the sensitivity and specificity were 60.5% and 71.7%, respectively, when the cut-off value of OD450 was set at 1.60.
CONCLUSION: Serum autoantibody levels of MMP-7 may be a good diagnostic biomarker for esophageal squamous cell carcinoma.
Keywords: Matrix metalloproteinase-7, Serum autoantibody, Esophageal squamous cell carcinoma, Gastric cancer, Biomarker
INTRODUCTION
Esophageal squamous cell carcinoma (ESCC), the major histological form of esophageal cancer in East Asian countries, is one of the leading causes of cancer death worldwide[1,2]. The high mortality of this disease is largely due to the lack of a screening strategy to detect early stage disease. ESCC survival is highly stage dependent. Patients with localized disease are 12 times more likely to survive five years than those with distant disease[3]. Unfortunately, most cases are diagnosed with ESCC when they have already reached an advanced stage[4]. Thus there is a growing need to identify useful biological markers for early, non-invasive diagnosis of ESCC[5].
The traditional serological tumor markers for ESCC, which are mainly secreted tumor antigens, i.e. CEA, SCCA, CYFRA21-1, and DKK-1, have been found to be useful but not sufficiently sensitive for early detection of the disease[6,7]. Autoantibodies against tumor-associated antigens were recently reported in sera from patients with ESCC and other cancers as a promising approach for early cancer detection[8-10]. Changes in the level of gene expression and aberrant expression of tissue-restricted gene products are factors that lead to humoral immune response in cancer patients, usually at the early stage of cancer development[11,12]. Therefore identifying novel autoantibody biomarkers may lead to early diagnosis or prediction of disease progression in patients with ESCC.
The matrix metalloproteinases (MMPs) are a family of zinc-dependent proteolytic enzymes capable of degrading the extracellular matrix (ECM). MMPs play a key role in the physiological degradation of the ECM in angiogenesis, tissue repair, and tissue morphogenesis[13]. They also regulate cell growth and inflammation by cleaving non-matrix proteins like growth factors, cytokines and chemokines, and their respective receptors[14]. MMP-7, as the smallest molecule of the MMPs, has been found overexpressed in a variety of epithelial and mesenchymal tumors, such as esophagus, colon, liver, renal, and pancreas. Its expression is correlated with unfavorable prognosis[15]. Increased circulating levels of MMP-7 proteins were correlated with the presence of metastatic disease and poor patient survival in colorectal and renal cell cancer[15-17]. However, as one of the early immune responses to cancer development, levels of autoantibodies against the MMP-7 protein have not been studied. This humoral immune response to MMP-7 might be a good early indicator of ESCC.
In this study, we evaluate the diagnostic values of serum autoantibodies against MMP-7 in ESCC and gastric cancer patients using purified MMP-7 proteins. We further discuss the possibility of the utility of these autoantibodies to MMP-7 as tumor markers in clinical diagnosis.
MATERIALS AND METHODS
Clinical samples
A total of 108 individuals’ serum samples (50 ESCC patients and 58 risk-matched controls) were collected from Baoding Tumor Hospital, Hebei, China. About 10 g of ESCC tumor samples were also collected in parallel. In addition, 38 serum samples were collected from patients with gastric cancer from the same hospital. Detailed information on the serum samples is listed in Table 1. All the clinical samples were collected after informed consents were obtained.
Table 1.
Characteristics of normal and patient serum n (%)
| Control (n = 58) | Patients with esophageal squamous cell carcinoma (n = 50) | Patients withgastric cancer (n = 38) | |
| Age | |||
| ≤ 45 | 5 (8.62) | 3 (6.00) | 4 (10.53) |
| 45-55 | 7 (12.07) | 4 (8.00) | 6 (15.79) |
| 55-65 | 24 (41.38) | 23 (46.00) | 13 (34.21) |
| 65-75 | 17 (29.31) | 19 (38.00) | 12 (31.58) |
| ≥ 75 | 5 (8.62) | 1 (2.00) | 1 (2.63) |
| Sex | |||
| Female | 11 (18.97) | 9 (18.00) | 13 (34.21) |
| Male | 47 (81.03) | 41 (82.00) | 25 (65.79) |
Cloning the MMP-7 cDNA from ESCC tissues
About 10 g of each ESCC tissue sample was snap-frozen in liquid nitrogen. RNA extraction was performed according to procedures described in the TRIzol Reagent manual (Invitrogen, USA). Primers were designed according to the sequence of the MMP-7 mRNA (GenBank, NM_002423.3). The sequence of the forward primer was5’-GGAATTCCATATGTCACTATTTCCAAATAGCCC-3’ and the sequence of reverse primer was 5’-CCCAAGCTTTTATCCATATAGTTTCTGAATGCC-3’. NdeI and Hind III (underlined) restriction sites were introduced into the sequences of forward and reverse primers, respectively.
RT-PCR reactions were carried out under the following conditions. After heating at 94°C for 4 min, the reactions were exposed to 30 cycles of 94°C for 30 s, 63°C for 40 s, and 72°C for 1 min; with a final extension at 72°C for 10 min. The final products were then subjected to electrophoresis on 1% agarose. The amplified inserts were purified using a DNA purification kit (QIAGEN, USA), digested with NdeI and Hind III, and then ligated to a prokaryotic expression vector pET28b(+) (Novagen, USA) that was also digested with the same restriction enzymes. The constructed plasmid was transformed into competent E. coli. DH5α cells and grown in Luria-Bertani (LB) broth supplemented with kanamycin (30 μg/mL). The recombinant plasmid was confirmed by double endonuclease digestion and DNA sequencing.
MMP-7 protein expression and purification
The recombinant plasmid pET-28b/MMP-7 was transformed into expression strain E. coli Rosetta (DE3) cells by heat-shock. One colony was picked and grown in 20 mL LB medium containing 30 μg/mL kanamycin at 37°C until an optical density (OD) at 600 nm of 0.6 was reached. Isopropyl-β-D-Thiogalactopyranoside (IPTG) was then added to induce protein expression at 28°C and 37°C. To determine the optimal condition for MMP-7 expression, DE3 cells were induced at different concentrations (0.4, 0.8, and 1.0 mmol/L) of IPTG for different lengths of time (1, 2, 4, 6 and 7 h). At the end of each condition, cells were harvested by centrifugation, resuspended in 1 mL PBS, and sonicated on ice until the suspension became transparent (5 min). The lysate was centrifuged for 30 min at 12 000 g, and then both the supernatant and the pellets were tested for the MMP-7 protein expression by 15% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE).
To purify this His-tagged MMP-7 recombinant protein, a QIAexpressionist (QIAGEN, USA) kit was used. Briefly, 3 mL of cell culture at the most optimal expression conditions was pelleted and resuspended in 600 μL lysis buffer (8 mol/L Urea, 10 mmol/L NaH2PO4, 10 mmol/L Tris.Cl, pH8.0) at room temperature for 4 h. Cell debris was cleared by centrifugation, and the supernatants were transferred to a fresh tube and incubated with 60 μL of a 50% slurry of Ni-NTA resin (10 μL resin has a capacity for 50-100 μg His-tagged protein) for 60 min at 4°C with agitation. The resin was then pelleted by centrifugation and washed twice with 300 μL wash buffer (8 mol/L Urea, 100 mmol/L NaH2PO4, 10 mmol/L Tris.Cl, pH6.3). The protein was then eluted three times with 30 μL elution buffer (8 mol/L Urea, 100 mmol/L NaH2PO4, 10 mmol/L Tris.Cl, pH4.5). The purification process was tested by 15% SDS-PAGE followed by Coomassie Brilliant Blue staining.
Measurement of serum autoantibodies against MMP-7
Ninety-six-well Costar ELISA plates (Jet Biofil, Beijing, China) were coated with 2 μg/mL of the purified MMP-7 protein and incubated overnight at 4°C. The plates were washed four times with PBST (PBS buffer containing 0.05% Tween 20), and then blocked with PBS containing 1% BSA at 37°C for 1 h, followed by four washes in PBST. Serum samples (ESCC or gastric cancer patients or control) were diluted 1/150 in 1% BSA and incubated in the MMP-7-coated ELISA plates at 37°C for 1 h. After washing four times with PBST, 100 μL of goat anti-human IgG-HRP (1:1000 dilutions) was added to each well for 1h at 37°C. After washing four times with PBST, the color was developed with 3,4,5-trimethoxy benzaldehyde (TMB) for exactly 15 min, and then stopped with 0.5 mol/L H2SO4. The absorbance of each well was read at 450 nm by a plate microplate reader (Beijing’s New Air Electrical Technology, Beijing, China). Each serum sample was tested in triplicate.
Statistical analysis
To analyze the difference of autoantibodies reaction to MMP-7 proteins between cancer and matched control sera, the absorbance of each serum sample in the ELISA plate was averaged from triplicate experiments. Student’s t-test was performed between cancer and matched-control samples. Nonparametric receiver-operating curves (ROCs), in which the value for sensitivity was plotted against false-positive rate (1-specificity), were generated. In addition, an area under the ROC curve (AUC) with 95% confidence intervals (CI) was calculated for each marker. In all tests, a P-value of ≤ 0.05 was considered to be statistically significant. All statistical analysis was done with the SPSS software package version 16.0 (SPSS, Chicago, IL, USA).
RESULTS
MMP-7 expression and purification
The cDNA of MMP-7 was cloned from ESCC tissues and inserted into a prokaryotic expression plasmid, pET-28b. After double endonuclease digestion and PCR confirmation, a single band of 492 bp was obtained (Figure 1) at the expected location. The insert DNA was further purified and sequenced. The sequence was found to be a perfect match to the sequence of MMP-7 deposited in NCBI GenBank.
Figure 1.
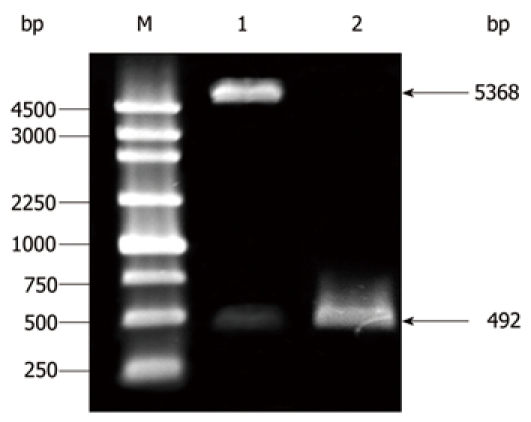
Double endonuclease digestion of the recombinant vector pET-28b/matrix metalloproteinase-7. M: DNA maker; Lane 1: Double digestion with NdeI and HindIII; Lane 2: Positive bacterial clone.
This pET-28b/MMP-7 plasmid was transformed into DE3 cells for MMP-7 expression. Optimal IPTG concentration and time course determinations were performed for the kinetics of protein expression in the bacterial culture. The results showed that DE3 cells had the highest MMP-7 protein expression level after 4 h of 0.4 mmol/L IPTG induction at 37°C (Figure 2A and B). The pET-28b/MMP-7 recombinant proteins were mainly observed in the precipitate of the DE3 lysate, which indicated that the expressed protein was mainly in sequestered to inclusion bodies. The expressed proteins were further purified to approximately 95% purity by Ni-NTA resin (Figure 3).
Figure 2.

pET-28b/matrix metalloproteinase-7 protein expression by sodium dodecyl sulfate-polyacrylamide gel electrophoresis. Panel A: Time course analysis of pET-28b/matrix metalloproteinase-7 (MMP-7) protein expression by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE). M: Protein marker; 1-5: Samples for different time points (1, 2, 4, 6, and 7 h) at 37°C after 0.4 mmol/L IPTG induced; 6: Uninduced bacterial lysate. Panel B: SDS-PAGE showing pET-28b/MMP-7 protein expression induced by different amounts of IPTG. 1, 5: Uninduced bacterial lysate; 2-4: Samples induced at different concentrations of IPTG (0.4, 0.8, 1 mmol/L) at 37°C for 4 h; 6-8: Samples induced at different concentrations of IPTG (0.4, 0.8, 1 mmol/L) at 28°C for 4 h.
Figure 3.
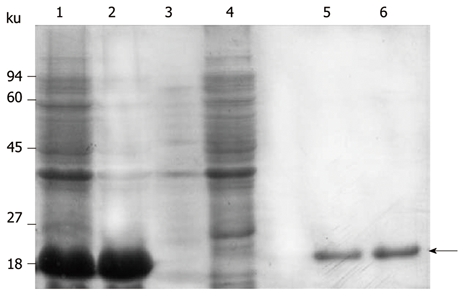
Soluble analysis and purification. 1: Samples induced with IPTG (0.4 mmol/L) for 4 h at 37°C; 2: Precipitate from the lysate of pET-28b/matrix metalloproteinase-7 (MMP-7) induced by IPTG; 3: The lysate supernatant of pET-28b/MMP-7 induced by IPTG; 4: Uninduced bacterial lysate; 5-6: Purified recombinant protein.
Comparison of MMP-7 autoantibodies between cancer and control samples
To test serum autoantibodies against MMP-7 proteins, the purified MMP-7 proteins were coated onto 96-well ELISA plates. Serum samples from 50 patients with ESCC or 38 with gastric cancer were tested, along with 58 control serum samples, using indirect ELISA. The mean OD450 (± SD) of serum autoantibodies against MMP-7 in 50 ESCC patients was 1.69 ± 0.08, and was 1.55 ± 0.10 in 58 control individuals. The mean OD450 (± SD) of serum autoantibodies against MMP-7 in 38 gastric cancer patients was 1.62 ± 0.06. The serum levels of autoantibodies against MMP-7 were significantly higher in ESCC than in healthy donors (P < 0.001, Figure 4A). The difference between healthy individuals and gastric cancer patients was also significant (P < 0.001, Figure 4B).
Figure 4.

Comparison of the specificity and sensitivity of matrix metalloproteinase-7 autoantibodies. A: matrix metalloproteinase-7 (MMP-7) autoantibodies were detected by enzyme-linked immunosorbent assay (ELISA) in sera from patients with esophageal squamous cell carcinoma (ESCC) and control samples (Control); B: MMP-7 autoantibodies were detected by ELISA in sera from patients with gastric cancer (Gastric cancer patients) and controls (Control); C: ROC curve for ESCC serum antibodies against MMP-7; D: ROC curve for gastric cancer serum antibodies against MMP-7.
ROC curves were plotted to identify a cut-off value that would distinguish case from control samples. According to the ROC curve, the optimal cutoff value for ESCC was 1.65, providing a sensitivity of 78.0% and a specificity of 81.0%. The AUC for MMP-7 was 0.87 (95% CI: 0.80-0.93, Figure 4C) in ESCC patients. For gastric cancer, according to the ROC curve, the optimal cutoff value was 1.60, providing a sensitivity of 60.5% and a specificity of 71.7%. The AUC for MMP-7 was 0.75 (95% CI: 0.64-0.84, Figure 4D).
DISCUSSION
Immune response with antibody production can be elicited due to the overexpression of cellular proteins, such as Her2[18], by the expression of mutated forms of cellular protein, such as mutated p53[19], or by the aberrant expression of tissue-restricted gene products, such as cancer-testis antigens[20] by cancer cells. These autoantibodies are raised against these specific antigens from the cancer cells; therefore, the detection of these antibodies in patients’ sera can be exploited for cancer diagnosis in these patients. Furthermore, the immune system is especially well adapted for the early detection of cancer, because it can respond to low levels of an antigen by mounting a very specific and sensitive antibody response. Autoantibodies against cancer-specific antigens have been identified in cancers of the colon[21], breast[22], lung[23], ovary[24], prostate[25], and head and neck[26].Thus, the use of the immune response as a biosensor for early detection of cancer through serum-based assays holds great potential as an ideal screening and diagnostic tool[27,28].
MMP-7 is closely related to tumor invasion and metastasis: many studies have shown MMP-7 to be overexpressed in colorectal cancer[29], esophagus[30], stomach[31], pancreatic cancer[32], breast cancer[33], prostate cancer[34], and renal cell carcinoma[35]. In addition, recent studies have shown that MMP-7 could be detected in the serum of cancer patients, including patients with ovarian[36] and colorectal cancer[17]. However, there has been no report regarding the diagnostic values of the serum autoantibodies against MMP-7 for any kind of cancers. In this study, we chose ESCC and gastric cancer as two typical gastrological cancers to evaluate the diagnostic values of autoantibodies against MMP-7. Our results clearly suggested that serum autoantibodies against MMP-7 have the potential to be a tumor marker for ESCC and gastric cancer. MMP-7 is overexpressed in many cancers; therefore, elevated levels of autoantibodies against MMP-7 may also be present in other cancers as a nonspecific cancer biomarker. The samples in this study were mostly late stage serum samples; therefore, it is necessary to further validate these results using a large cohort of well-characterized patient samples, especially with early stage patient samples. It might be also a good approach to further analyze the MMP-7 autoantibody diagnostic values in combination with the current tumor markers in ESCC and gastric cancer.
In conclusion, the results in this study are encouraging, even though further investigations are needed to evaluate its usefulness in population screening for ESCC. Moreover, the assay is easy to set up, because the recombinant proteins expressed and purified from E. coli are cost-effective and easy-to-standardize as serological reagents[37].
COMMENTS
Background
Early diagnosis of esophageal squamous cell carcinoma (ESCC) has resulted in a significant reduction in morbidity and mortality, and new diagnostic markers could improve the results of screening. Matrix metalloproteinase-7 (MMP-7) is closely related to tumor invasion and metastasis. Increased MMP-7 levels have been found in ESCC. The present study aims to determine whether serum autoantibodies against MMP-7 in patients with ESCC could be used as biomarkers for diagnosis of the disease.
Research frontiers
New serum-based markers that could improve the accuracy of early detection of cancer are being sought. Recent findings suggested that MMP-7 is aberrantly expressed in ESCC. However, a prospective consecutive study of the evaluation of serum autoantibodies against MMP-7 as a diagnostic marker for ESCC has not been established.
Innovations and breakthroughs
Autoantibodies as biomarkers for early cancer detection have been recently studied in other cancers. This is the first report to show that autoantibodies against MMP-7 could be a potential biomarker for ESCC diagnosis.
Applications
Serum autoantibodies against MMP-7 could become an important biomarker for ESCC early detection in clinics if this observation is further validated with a large cohort of patient samples.
Terminology
The Humoral Immune Response: is the aspect of immunity that is mediated by secreted antibodies (as opposed to cell-mediated immunity, which involves T lymphocytes) produced in the cells of the B lymphocyte lineage (B cell). B Cells (with co-stimulation) transform into plasma cells that secrete antibodies. Humoral immunity is so named because it involves substances found in the humors, or body fluids. Autoantibody: antibody that reacts with antigens found on the cells and tissues of an individual’s own body. Autoantibodies can cause autoimmune diseases.
Peer review
The research described is very interesting. The manuscript is well written.
Footnotes
Supported by Science and Technology Projects of Hebei Province, #10396107D and NIH Grant CA137570 (Zhong L)
Peer reviewer: Mario M D’Elios, Professor, University of Florence, viale Morgagni 85, Florence, 50134, Italy
S- Editor Sun H L- Editor Stewart GJ E- Editor Ma WH
References
- 1.Muto M, Minashi K, Yano T, Saito Y, Oda I, Nonaka S, Omori T, Sugiura H, Goda K, Kaise M, et al. Early detection of superficial squamous cell carcinoma in the head and neck region and esophagus by narrow band imaging: a multicenter randomized controlled trial. J Clin Oncol. 2010;28:1566–1572. doi: 10.1200/JCO.2009.25.4680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jemal A, Center MM, DeSantis C, Ward EM. Global patterns of cancer incidence and mortality rates and trends. Cancer Epidemiol Biomarkers Prev. 2010;19:1893–1907. doi: 10.1158/1055-9965.EPI-10-0437. [DOI] [PubMed] [Google Scholar]
- 3.Takikita M, Hu N, Shou JZ, Wang QH, Giffen C, Taylor PR, Hewitt SM. Biomarkers of apoptosis and survival in esophageal squamous cell carcinoma. BMC Cancer. 2009;9:310. doi: 10.1186/1471-2407-9-310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shimada H, Nabeya Y, Okazumi S, Matsubara H, Shiratori T, Gunji Y, Kobayashi S, Hayashi H, Ochiai T. Prediction of survival with squamous cell carcinoma antigen in patients with resectable esophageal squamous cell carcinoma. Surgery. 2003;133:486–494. doi: 10.1067/msy.2003.139. [DOI] [PubMed] [Google Scholar]
- 5.Sobin LH, Fleming ID. TNM Classification of Malignant Tumors, fifth edition (1997). Union Internationale Contre le Cancer and the American Joint Committee on Cancer. Cancer. 1997;80:1803–1804. doi: 10.1002/(sici)1097-0142(19971101)80:9<1803::aid-cncr16>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 6.Mealy K, Feely J, Reid I, McSweeney J, Walsh T, Hennessy TP. Tumour marker detection in oesophageal carcinoma. Eur J Surg Oncol. 1996;22:505–507. doi: 10.1016/s0748-7983(96)92998-4. [DOI] [PubMed] [Google Scholar]
- 7. Yamabuki T, Takano A, Hayama S, Ishikawa N, Kato T, Miyamoto M, Ito T, Ito H, Miyagi Y, Nakayama H, Fujita M, Hosokawa M, Tsuchiya E, Kohno N, Kondo S, Nakamura Y, Daigo Y. Dikkopf-1 as a novel serologic and prognostic biomarker for lung and esophageal carcinomas. Cancer Res 2007; 67: 2517-2525. doi: 10.1158/0008-5472.CAN-06-3369. [DOI] [PubMed] [Google Scholar]
- 8.Dong J, Zeng BH, Xu LH, Wang JY, Li MZ, Zeng MS, Liu WL. Anti-CDC25B autoantibody predicts poor prognosis in patients with advanced esophageal squamous cell carcinoma. J Transl Med. 2010;8:818. doi: 10.1186/1479-5876-8-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Long M, Luo J, Li Y, Zeng FY, Li M. Detection and evaluation of antibodies against neutrophil-activating protein of Helicobacter pylori in patients with gastric cancer. World J Gastroenterol. 2009;15:2381–2388. doi: 10.3748/wjg.15.2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang XJ. Autoantibody Biomarkers in Prostate Cancer. LabMedicine. 2008;39:165–171. [Google Scholar]
- 11.Hanash SM, Pitteri SJ, Faca VM. Mining the plasma proteome for cancer biomarkers. Nature. 2008;452:571–579. doi: 10.1038/nature06916. [DOI] [PubMed] [Google Scholar]
- 12.Finn OJ. Immune response as a biomarker for cancer detection and a lot more. N Engl J Med. 2005;353:1288–1290. doi: 10.1056/NEJMe058157. [DOI] [PubMed] [Google Scholar]
- 13.Bosman FT, Stamenkovic I. Functional structure and composition of the extracellular matrix. J Pathol. 2003;200:423–428. doi: 10.1002/path.1437. [DOI] [PubMed] [Google Scholar]
- 14.Luukkaa H, Klemi P, Hirsimäki P, Vahlberg T, Kivisaari A, Kähäri VM, Grénman R. Matrix metalloproteinase (MMP)-7 in salivary gland cancer. Acta Oncol. 2010;49:85–90. doi: 10.3109/02841860903287197. [DOI] [PubMed] [Google Scholar]
- 15.Szarvas T, Becker M, vom Dorp F, Gethmann C, Tötsch M, Bánkfalvi A, Schmid KW, Romics I, Rübben H, Ergün S. Matrix metalloproteinase-7 as a marker of metastasis and predictor of poor survival in bladder cancer. Cancer Sci. 2010;101:1300–1308. doi: 10.1111/j.1349-7006.2010.01506.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ramankulov A, Lein M, Johannsen M, Schrader M, Miller K, Jung K. Plasma matrix metalloproteinase-7 as a metastatic marker and survival predictor in patients with renal cell carcinomas. Cancer Sci. 2008;99:1188–1194. doi: 10.1111/j.1349-7006.2008.00802.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maurel J, Nadal C, Garcia-Albeniz X, Gallego R, Carcereny E, Almendro V, Mármol M, Gallardo E, Maria Augé J, Longarón R, et al. Serum matrix metalloproteinase 7 levels identifies poor prognosis advanced colorectal cancer patients. Int J Cancer. 2007;121:1066–1071. doi: 10.1002/ijc.22799. [DOI] [PubMed] [Google Scholar]
- 18.Disis ML, Bernhard H, Gralow JR, Hand SL, Emery SR, Calenoff E, Cheever MA. Immunity to the HER-2/neu oncogenic protein. Ciba Found Symp. 1994;187:198–207; discussion 207-211. doi: 10.1002/9780470514672.ch13. [DOI] [PubMed] [Google Scholar]
- 19.Soussi T. p53 Antibodies in the sera of patients with various types of cancer: a review. Cancer Res. 2000;60:1777–1788. [PubMed] [Google Scholar]
- 20.Chen YT, Scanlan MJ, Sahin U, Türeci O, Gure AO, Tsang S, Williamson B, Stockert E, Pfreundschuh M, Old LJ. A testicular antigen aberrantly expressed in human cancers detected by autologous antibody screening. Proc Natl Acad Sci USA. 1997;94:1914–1918. doi: 10.1073/pnas.94.5.1914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scanlan MJ, Chen YT, Williamson B, Gure AO, Stockert E, Gordan JD, Türeci O, Sahin U, Pfreundschuh M, Old LJ. Characterization of human colon cancer antigens recognized by autologous antibodies. Int J Cancer. 1998;76:652–658. doi: 10.1002/(sici)1097-0215(19980529)76:5<652::aid-ijc7>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 22.Disis ML, Calenoff E, McLaughlin G, Murphy AE, Chen W, Groner B, Jeschke M, Lydon N, McGlynn E, Livingston RB. Existent T-cell and antibody immunity to HER-2/neu protein in patients with breast cancer. Cancer Res. 1994;54:16–20. [PubMed] [Google Scholar]
- 23.Zhong L, Peng X, Hidalgo GE, Doherty DE, Stromberg AJ, Hirschowitz EA. Identification of circulating antibodies to tumor-associated proteins for combined use as markers of non-small cell lung cancer. Proteomics. 2004;4:1216–1225. doi: 10.1002/pmic.200200679. [DOI] [PubMed] [Google Scholar]
- 24.Chatterjee M, Mohapatra S, Ionan A, Bawa G, Ali-Fehmi R, Wang X, Nowak J, Ye B, Nahhas FA, Lu K, et al. Diagnostic markers of ovarian cancer by high-throughput antigen cloning and detection on arrays. Cancer Res. 2006;66:1181–1190. doi: 10.1158/0008-5472.CAN-04-2962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang X, Yu J, Sreekumar A, Varambally S, Shen R, Giacherio D, Mehra R, Montie JE, Pienta KJ, Sanda MG, et al. Autoantibody signatures in prostate cancer. N Engl J Med. 2005;353:1224–1235. doi: 10.1056/NEJMoa051931. [DOI] [PubMed] [Google Scholar]
- 26.Lin HS, Talwar HS, Tarca AL, Ionan A, Chatterjee M, Ye B, Wojciechowski J, Mohapatra S, Basson MD, Yoo GH, et al. Autoantibody approach for serum-based detection of head and neck cancer. Cancer Epidemiol Biomarkers Prev. 2007;16:2396–2405. doi: 10.1158/1055-9965.EPI-07-0318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tan EM, Zhang J. Autoantibodies to tumor-associated antigens: reporters from the immune system. Immunol Rev. 2008;222:328–340. doi: 10.1111/j.1600-065X.2008.00611.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lu H, Goodell V, Disis ML. Humoral immunity directed against tumor-associated antigens as potential biomarkers for the early diagnosis of cancer. J Proteome Res. 2008;7:1388–1394. doi: 10.1021/pr700818f. [DOI] [PubMed] [Google Scholar]
- 29.Leeman MF, Curran S, Murray GI. New insights into the roles of matrix metalloproteinases in colorectal cancer development and progression. J Pathol. 2003;201:528–534. doi: 10.1002/path.1466. [DOI] [PubMed] [Google Scholar]
- 30.Zhang J, Jin X, Fang S, Wang R, Li Y, Wang N, Guo W, Wang Y, Wen D, Wei L, et al. The functional polymorphism in the matrix metalloproteinase-7 promoter increases susceptibility to esophageal squamous cell carcinoma, gastric cardiac adenocarcinoma and non-small cell lung carcinoma. Carcinogenesis. 2005;26:1748–1753. doi: 10.1093/carcin/bgi144. [DOI] [PubMed] [Google Scholar]
- 31.McCaig C, Duval C, Hemers E, Steele I, Pritchard DM, Przemeck S, Dimaline R, Ahmed S, Bodger K, Kerrigan DD, et al. The role of matrix metalloproteinase-7 in redefining the gastric microenvironment in response to Helicobacter pylori. Gastroenterology. 2006;130:1754–1763. doi: 10.1053/j.gastro.2006.02.031. [DOI] [PubMed] [Google Scholar]
- 32.Jones LE, Humphreys MJ, Campbell F, Neoptolemos JP, Boyd MT. Comprehensive analysis of matrix metalloproteinase and tissue inhibitor expression in pancreatic cancer: increased expression of matrix metalloproteinase-7 predicts poor survival. Clin Cancer Res. 2004;10:2832–2845. doi: 10.1158/1078-0432.ccr-1157-03. [DOI] [PubMed] [Google Scholar]
- 33.Wang F, Reierstad S, Fishman DA. Matrilysin over-expression in MCF-7 cells enhances cellular invasiveness and pro-gelatinase activation. Cancer Lett. 2006;236:292–301. doi: 10.1016/j.canlet.2005.05.042. [DOI] [PubMed] [Google Scholar]
- 34.Lynch CC, Hikosaka A, Acuff HB, Martin MD, Kawai N, Singh RK, Vargo-Gogola TC, Begtrup JL, Peterson TE, Fingleton B, et al. MMP-7 promotes prostate cancer-induced osteolysis via the solubilization of RANKL. Cancer Cell. 2005;7:485–496. doi: 10.1016/j.ccr.2005.04.013. [DOI] [PubMed] [Google Scholar]
- 35.Miyata Y, Iwata T, Ohba K, Kanda S, Nishikido M, Kanetake H. Expression of matrix metalloproteinase-7 on cancer cells and tissue endothelial cells in renal cell carcinoma: prognostic implications and clinical significance for invasion and metastasis. Clin Cancer Res. 2006;12:6998–7003. doi: 10.1158/1078-0432.CCR-06-1626. [DOI] [PubMed] [Google Scholar]
- 36.Palmer C, Duan X, Hawley S, Scholler N, Thorpe JD, Sahota RA, Wong MQ, Wray A, Bergan LA, Drescher CW, et al. Systematic evaluation of candidate blood markers for detecting ovarian cancer. PLoS One. 2008;3:e2633. doi: 10.1371/journal.pone.0002633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carattoli A, Di Bonito P, Grasso F, Giorgi C, Blasi F, Niedrig M, Cassone A. Recombinant protein-based ELISA and immuno-cytochemical assay for the diagnosis of SARS. J Med Virol. 2005;76:137–142. doi: 10.1002/jmv.20338. [DOI] [PMC free article] [PubMed] [Google Scholar]


