Abstract
Objective:
To design and test an in-expensive air-inflated balloon that is easy to sterilize and use for the control of atonic post partum hemorrhage (APPH).
Outcome measures:
Primary outcome measure: Maternal Mortality (MM).
Secondary outcome measures: Surgical maternal morbidities, amount and doses of drugs, blood transfusion units used for resuscitation, general condition of women on admission and outcome on discharge, the resuscitation time and time for regaining normal uterine tone; hospital stay and ICU admission.
Technical outcomes: Incidence of Balloon rupture, allergic manifestations, and pyrexia.
Methods:
Randomized clinical trail / cross over study
Two hundred and forty women with diagnosis of atonic PPH complicating vaginal deliveries were randomly assigned to be managed either by ecbolics and uterine massage as recommended by the WHO; or by WHO protocol plus El-Menia air inflated balloon.
Results:
No maternal mortality in either group. The maternal morbidities in the form of surgical intervention (uterine and ovarian artery ligation, uterine compression suture, internal iliac artery ligation and abdominal hysterectomy) were observed in five women in controls and none in the studied women. Blood transfusion units, ecobolic drugs, resuscitation time, regaining uterine tone time, hospital stay and ICU admission were significantly less in studied women than controls.
Out of the 19 failures to arrest APPH in the controls; 14 cases responded to secondary application of El-Menia balloon, and only five cases required surgical intervention.
Conclusion :
El-Menia balloon is an inexpensive, easy to apply, effective in controlling APPH with minimal side effects. It is targeted for use on a large scale in developing countries to reduce the maternal mortality and morbidity caused by APPH.
Keywords: atonic pph, el-menia balloon
Introduction
Management of third stage of labor is crucial because its complications may kill the parturient. Severe postpartum hemorrhage (PPH) is the single most important cause of maternal mortality (MM) with an incidence of 5 – 15 % worldwide.(1) Although certain predisposing factors may contribute to PPH development, yet every pregnant woman may face life threatening blood loss at delivery. Uterine atony is the most common cause of PPH, accounting for 80–90 % of PPH. (2)
Maternal mortality is very high in developing te renal failure and loss of future fertility countries. Not only thousands of young productive women die every year, but also millions of young women were left with permenant disability such as anaemia, fatigue, depression, necrosis of anterior pituitary gland and viral infection with HIV, HCV, and HBV and loss of future fertiluty as a result of hysterectomy due to intractable postpartum hemorrhage.(3, 4) Families of affected women were also left to face miserable life, particularly the children. Although active management of third stage of labor and the use of ecobolics after delivery contributed to a reduction of about 60 % of atonic PPH.(5,6) PPH remains still, the major cause of MM especially in developing countries, where, it accounts for more than 30 % of MM. (7) Fortunately, this complication can be prevented, if an immediate and aggressive team management is properly instituted. The aim of this study was to design an in-expensive, air inflated balloon to stop uterine bleeding in cases of atonic PPH and to conduct a study to demonstrate its efficacy.
Methods
In a randomized clinical trial conducted in Beni-Mazar District Hospital, El-Menia, Egypt, in the years 2003 and 2004, two hundred and forty women delivered vaginally either in hospital or at home and were complicated with atonic postpartum hemorrhage admitted to the study. This was after signing an informed consent by their husbands. The study design was approved by El-Menia Faculty of medicine ethical committee.
Following the diagnosis of PPH, these women were assigned to one of two treatment groups. Women were allocated to either the study or the control group according to a computer generated randomization, the study officer handled out a closed opaque envelope containing the orders to manage the patient according to one of the approved treatment plans.
Group I: 120 women treated with uterine massage and ecobolics according to WHO protocol. (7)
Group II: 120 women treated with WHO protocol plus El-Menia balloon application. The inclusion criteria were vaginal delivery, atonic PPH and medical resuscitation approach. Exclusion criteria were cases of PPH due to traumatic, retained placental tissues, other cause and after cesarean delivery.
Intervention procedure in study group:
When APPH was diagnosed (8), manual aortic compression around the umbilicus was carried out immediately to reduce uterine bleeding; this is to allow insertion of the balloon without delay. This balloon has been tested ten times against rigid walls of plastic sac with increasing intra-balloon pressure up to 300 mmHg; this is to test the pressure effect on balloon wall integrity.
Under complete aseptic conditions, the balloon was introduced inside the uterine cavity. This was aided by grasping the anterior lip of the cervix with sponge forceps. Then, the balloon was inflated with air up to 140 mmHg as a maximum pressure; this pressure was chosen because a pressure above this level has led to marked dilatation of uterus causing systemic symptoms such as tachycardia and hypotension, and; cervical tears. To prevent herniation of the inflated balloon through the dilated cervix, a cerclage with silk suture was undertaken under light analgesia. The suture was taken in cervix at 3 and 9 o’clock and was not too tight in order not to obscure uterine blood loss. The time taken to insert the balloon and cerclage ranged from four to five minutes; this time was compensated by the rapid effect of the balloon controlling APPH.
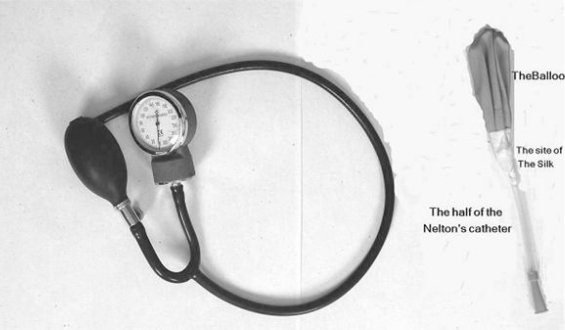
Fig.1 shows El-Menia balloon design. It is composed of a latex balloon (that is commonly used by children on celebrations) this particular brand is manufactured in Italy and has a 0.19 mm wall thickness. And a 15 cm long piece of rigid catheter (Nelton catheter, size 16 f with 5 mm caliber “orange color”), this brand is made in Malaysia. The catheter is introduced inside the balloon and is tied over tightly several times with a silk suture, to prevent air escape.
Fig. (1). shows El-Menia balloon components and the inflation device.
Sterilization of El-Menia balloon was done by emersion of El-Menia balloon design in an activated 2% gluteraldehyde for 20 min. (8) The sterilized balloon is then stored in a sterile box ready for use. The effect of sterilization solution on the strength of the balloon wall was tested by air inflation up to 300 mmHg for at least ten repeated times, it has been found that the sterilization solution has no weakening effect on the balloon wall integrity. Such pressure is very high; never been reached during balloon application.
Inflation Device
The free end of the catheter is attached to a sphygmomanometer inflation device (Fig. 1). This device is attached to a pump with a valve to deflate air when needed.
El-Menia Baloon Deflation
Following stabilization of the women’s condition, arrest of uterine bleeding and the return of normal uterine tone (tested by hand feeling), deflation of one half of balloon pressure was done, keeping close observation on uterine blood loss. If uterine bleeding re-started then, re-inflation to the previous pressure was done. Otherwise, the new pressure was kept for two hours, and then the remaining pressure was deflated over ten min. Re-appearance of uterine bleeding necessitated re-inflation again to the previous pressure.
Prophylactic antibiotics in the form of metronidazole 500 mg, gentamycin 80 mg and ampecillin 500 mg every eight hours were given after insertion of the balloon and for three days thereafter.
Outcomes measured in this study were:
Primary outcome measure: maternal mortality.
Secondary outcome measures: maternal morbidities, surgical interventions e.g. uterine and ovarian arteries ligation, compression suture, internal artery ligation and abdominal hysterectomy), amount and dosage of drugs used for resuscitation, blood transfusion units used, the general condition of women on admission and outcome on discharge, time of resuscitation, time required to regain normal uterine tone, hospital stay and ICU admission. Technical outcome measures: incidence of balloon rupture, allergic manifestations and pyrexia.
The data were analyzed using the SPSS program version 11 for windows. Student t test was used to compare the independent means.
Results
No maternal mortality has been reported in both groups, however, maternal morbidities in the form of surgical intervention i.e. laparotomy, B. Lynch suture and internal iliac artery ligation or peripartum hysterectomy were seen in five of the controls, while, none has been reported in the study group.
There was no single failure to control APPH in the study group while, there were 19 failures to arrest APPH in control group. Out of these 19 failures, 14 women responded to the secondary application of El-Menia balloon and five required surgical operations to control APPH.
Table (1): shows conditions of studied women and controls on admission to the study and outcome on hospital discharge. It can be seen that 83 of the 120 studied women (69%) were admitted in shock; none of them had surgical intervention. While, 78 of the 120 control women (65%) were in shock on admission, five of them (4.2%) had surgical operations; three of these five had total abdominal hysterectomy.
Resuscitation of the unshocked women has been done in a mean time of less than three hours, the shocked and conscious women in a mean time of five hours and those whom were shocked and unconscious had taken a mean time of eight hours to resuscitate. Regaining the normal uterine tone as palpated by hand followed a similar order as the above.
Tables 2–6 show highly significant differences, in favor of the study group in comparison to controls in the following parameters: hemoglobin and hematocrit values on hospital discharge, drugs, transfused blood units used for resuscitation, time required for resuscitation and regaining normal uterine tone in both groups, and days of hospitalization and ICU admission.
Table (2). Comparison between ergometerine ampoules and syntocinon units used in both groups.
| Groups | Patient No. | Range ergometrine ampoules | Mean ± ST | T | P. value |
|---|---|---|---|---|---|
| Controls | 120 | 3 – 4 | 3.6 ± 0.5 | 12.2 | 0.001 |
| Study | 120 | 2 – 4 | 2.5 ± 0.8 | ||
| Range of syntocinon units | |||||
| Controls | 120 | 40–110 | 639 ± 23.3 | 12.3 | 0.001 |
| Study | 120 | 30–50 | 37 ± 5.6 |
Table (6). Comparison between days stayed in I.C.U. and hospital by women in both groups.
| Groups | Patient No. | Range of days ICU | Mean ± ST | T | P. value |
|---|---|---|---|---|---|
| Controls | 120 | 1–2 | 1.5± 0.5 | 10.9 | 0.001 |
| Study | 120 | 1 | 1 ± 0.0 | ||
| Hospital days | Mean ± ST | T | P. value | ||
| Controls | 120 | 3 – 6 | 3.5± s0.5 | 17.9 | 0.001 |
| Study | 120 | 2–3 | 2.3±0.5 |
There was no balloon rupture in the entire study; nor was any complains by the studied women of pyrexia or allergic symptoms.
Discussion
In case of postpartum uterine atony, in order to arrest the bleeding, either uterine contractions or compression against bleeding sinuses are required. If none were feasible and the bleeding continues the circulating blood volume and the oxygen carrying capacity are significantly diminished leading to a state of tissue hypoxia. Anaerobic metabolisms of uterine muscles as well as other body tissues produce nitric oxide, lipid peroxides and other toxic metabolites that may seriously damage the nucleolus and membrane of uterine smooth muscle cells, rendering them irresponsive to endogenous and/or exogenous ecobolics. The intractable APPH then, may be initiated putting the women’s life in jeopardy.(9)
Among the new modalities introduced to arrest the intractable APPH is the uterine tamponade. It allows adequate time to resuscitate the women and to correct coagulopathy if present. (10, 11)
Anatomically, the gravid uterine cavity is not spherical but egg shaped, not easily fitted with several balloon catheters such as Foley’s catheters.(10) The balloon which we have designed when inflated with air fits the cavity well, compresses the bleeding sinuses and arrest the bleeding. This special criterion is shared with Sangestaken Blakemore(8, 11, 12, 13), Rush catheters (14, 15) and others.(16) However, El-Menia balloon is comparably very inexpensive. El-Menia balloon when inflated can reach large size to fit in well the gravid uterus.
This study is a unique one, because not only air was used instead of fluid, but also it is the largest among tamponade studies, 240 versus 16 and 23 women in Condous et al. (8) and Akhter et al.(17) respectively. The rational behind using air instead of saline to inflate the balloon was that pumping air inside the balloon is quicker, easier to do in such critical emergency, as well as air is always available at all times without cost.
El-Menia balloon is flexible, soft with non traumatic consistency, does not require long forceps for insertion; this reduces chances of uterine perforation and infection. If it fails to arrest uterine bleeding, this is immediately visible. Because the cervical stitch unlike packed vaginal gauze do not mask the uterine bleeding. The manual external aortic compression was used in this study as a first aid to reduce the uterine bleeding to allow a relatively clear field for insertion of the balloon. (18)
In this study, no maternal mortality in studied women has occurred because of the balloon use; and also none in controls because every woman was attended and aggressively managed by specialist professional as well as the availability of intensive care facilities. However, in the control group there were five non-responders, two required B-Lynch suture and internal iliac artery ligation and the other three had total abdominal hysterectomies.
As a primary intervention the success rate of El-Menia balloon was 100%. However, when the balloon was used as secondary intervention in failed cases in control group, the success rate was only 74%. The 26% failure rate in the secondary intervention subgroup may be due to the prolonged damaging effect of anaerobic metabolites on the uterine muscle rendering these uterine muscle cells irresponsive to ecobolics.(9) The use of El-Menia balloon to treat the resuscitation failures in the control group has disturbed the RCT design of the study, nevertheless, it is unethical to expose woman to serious morbidity, only because of a study design.
The results of our study agree with Akhter et al.(17), they reported 100% success similar to our study. However, they studied only 23 women using condom and packed the vagina with gauze to prevent condom herniation, which may increase the incidence of infection and hide uterine blood loss. The results of our study are better than Condous et al, study (8), where the success rate was 86% in their 16 cases study.
Undesired over inflation of the balloon, has resulted in three complications; two cases of cervical tear treated with surgical repair under general anesthesia. The third one was a rise of uterine size above umbilicus; associated with tachycardia and hypotension, which had returned back to normal after deflation of the balloon bringing the uterine level just below the umbilicus.
In conclusion, the uterine tamponade has proved to be valuable in arresting APPH, particularly, El-Menia balloon because it is flexible, easy to use, air inflated, inexpensive with minimal side effect. It can be used on a massive scale in the developing countries to reduce maternal mortality and morbidity due to APPH.
Table (1). women’s condition on admission and outcome on hospital discharge.
| Woman condition on admission | Control group | Outcome On discharge | Study Group | Outcome On discharge |
|---|---|---|---|---|
| Conscious & unshocked | 42 | Three T.A.H. | 37 | No T.A.H. |
| Conscious & shocked | 53 | 55 | ||
| Unconscious & shocked | 25 | 28 |
T.A.H. = Total Abdominal Hysterectomy
Table (3). comparison between blood units transfused to women in both groups.
| Groups | Patient No | Range of blood units transfused | Mean ± ST | T | P. value |
|---|---|---|---|---|---|
| Controls | 120 | 5– 12 | 7.4 ± 1.8 | 17.9 | 0.001 |
| Study | 120 | 3– 6 | 4.1 ± 0.86 |
Table (4). Comparison between haemoglobin % and haematocrit values of both groups on hospital discharge.
| Groups | Patient No. | Range of Women’ Hb | Mean ± ST | T | P. value |
|---|---|---|---|---|---|
| Controls | 120 | 8.9–10% | 8.78 ± 1.6 | 6 | 0.001 |
| Study | 120 | 9.1 – 10.1% | 9.7 ± 0.2 | ||
| Patients HCT | |||||
| Controls | 120 | 26.7 – 30% | 26.7 ± 4.5 | 5.8 | 0.001 |
| Study | 120 | 27.3 – 30% | 29 ± 0.7 |
Table (5). comparison of time needed (hrs) to resuscitate women and regaining normal uterine tone in both groups.
| Groups | Patient No. | Range time resuscitation | Mean ± ST | T | P. value |
|---|---|---|---|---|---|
| Controls | 120 | 5 – 22.13 | 13.3 ± 4.9 | 16.1 | 0.001 |
| Study | 120 | 2.52 – 12.11 | 5.9 ± 1.7 | ||
| Range time normal tone | |||||
| Controls | 120 | 3 – 13.41 | 9.4 ± 5.5 | 12.5 | 0.001 |
| Study | 120 | 1.14 – 10.18 | 5.9 ± 1.4 |
References
- 1.SOGC, Prevention and management of postpartum hemorrhage, SOGC Clinical practice guidelines No 88. J Soc Obstet gynecol Can. 2000;22(4):271–81. [Google Scholar]
- 2.Ripley DL. Uterine emergencies: atony inversion, and rupture. Obstetrics and Gynecology clinics of North America. 1999;26:419–434. doi: 10.1016/s0889-8545(05)70087-5. [DOI] [PubMed] [Google Scholar]
- 3.Arulkumaran S. Maternal mortality: the need for global participation. International Federation of Gynecology and Obstetrics and the International Confederation of Midwives. Curr opin Obstet gynecol. 2004;16:107–109. doi: 10.1097/00001703-200404000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Alexander D, Alioune G, Patricia M, Marie BH. Emergency obstetric care in developing countries: impact of guidelines implementation in community hospital in Senegal. BJOG. 2005;112:1262–1269. doi: 10.1111/j.1471-0528.2005.00604.x. [DOI] [PubMed] [Google Scholar]
- 5.Elbourne DR, Prendiville WJ, Corrdi G, et al. 3. Oxford: update software; 2003. Prophylactic use of oxytocin in the third stage of labor. In the Cochrane library. [Google Scholar]
- 6.Prendiville WJ, Elbourne DR, McDonald S. the Cochrane library. 3. oxford: update software; 2003. Active vs. expectant management in the third stage of labor. [Google Scholar]
- 7.World Health Organization, Mother Baby Package. Geneva: WHO; 1994c. Implementing safe motherhood in countries. Published document FHE/MSM/94.11. [Google Scholar]
- 8.Condous G, Arulkumaran S, Symonds I, Chapman R, Sinha A, Razvi K. “ the tamponade test” in the management of massive postpartum hemorrhage. Obstet Gynecol. 2003;101:767–72. doi: 10.1016/s0029-7844(03)00046-2. [DOI] [PubMed] [Google Scholar]
- 9.Soltan MH, Ibrahim IY, Ibrahim MH. Clinical outcome and biochemical changes in intractable atonic postpartum hemorrhage. IHSJ, submitted for publication. [Google Scholar]
- 10.Marcovici I, Sococcio B. Postpartum hemorrhage and intrauterine balloon tamponade. A Report of three cases. J Reprod Med. 1999;44:122–24. [PubMed] [Google Scholar]
- 11.Edwin C. Management algorithm for atonic postpartum hemorrhage. JPOD. 2005 May–Jun; [Google Scholar]
- 12.De loor J, Van Dam P. Foley catheter for uncontrollable obstetric or gynecologic hemorrhage. Obstet Gyncol. 1996;88:737. doi: 10.1016/0029-7844(96)00158-5. [DOI] [PubMed] [Google Scholar]
- 13.Chan C, Razvi K, Tham K. The use of Sangstaken-blackmore tube to control postpartum hemorrhage. Int J Gynecol Obstet. 1997;58:251–2. doi: 10.1016/s0020-7292(97)00090-8. [DOI] [PubMed] [Google Scholar]
- 14.Ibrahim A, Mekkawy S, Harara R. Use of Sangstaken-Blackmore tube to control intractable postpartum hemorrhage. ASJOG. 2004;3:132–7. [Google Scholar]
- 15.Johanson R, Kurmar M, Obharia M, Young P. Management of massive post partum hemorrhage; use of hydrostatic balloon to avoid laparotomy. BJOG. 2002;108:420–2. doi: 10.1111/j.1471-0528.2001.00102.x. [DOI] [PubMed] [Google Scholar]
- 16.Bakri YN, Amri A, Abdul Jaber F. Tamponade balloon for obstetric bleeding. Int J Gynecol Obstet. 1992;37:302–3. [Google Scholar]
- 17.Akhter S, Begum MR, Kabir Z, Rashid M, Laila TR, Zabeen Z. Use of condom to control Massive postpartum hemorrhage. Medscape General medicine. 2003;5(3) [PubMed] [Google Scholar]
- 18.Soltan MH, Mosabah MH, Al-Adawy AR, Faragallah MF. External Aortic Compression, The First Aid for Postpartum Control. BJOG. doi: 10.1111/j.1447-0756.2008.00975.x. (In press) [DOI] [PubMed] [Google Scholar]